Abstract
Background: Volar locking plate fixation may offer several advantages over headless screw fixation for scaphoid nonunion, or segmental or comminuted fractures: (1) increased surface area for bony healing; (2) preserved vascularity; and (3) maintenance of a gap for graft insertion. The purpose of this study is to compare headless screw and locking plate fixation of segmental scaphoid fractures and to determine whether either fixation provides a greater mechanical advantage in osteoporotic versus nonosteoporotic bone. Methods: Sixteen matched-pair cadaver scaphoids were dissected from a range of osteoporotic and nonosteoporotic specimens. Scaphoids from each matched pair were randomly assigned to either volar locking plate or compression screw fixation. A 3-mm segment of bone was circumferentially excised from each scaphoid waist to simulate a segmental defect. Implants were applied, and each specimen was then loaded in axial compression. Load to failure was defined as the load required to achieve gap closure. Mechanism of failure, load to failure, and percent gap recovery were recorded for each trial. Results: Gap closure occurred in all trials. Difference in load to failure was not statistically significant between plate and screw fixation in either nonosteoporotic or osteoporotic cadaver specimens. However, percent gap recovery was significantly higher for plate fixation than for screw fixation. Conclusions: In scaphoid fractures with segmental defect, plate and screw fixation demonstrate similar loads to failure, but plate fixation performs superiorly to screw fixation for gap recovery after an applied load to failure.
Keywords: scaphoid, nonunion, biomechanical, plate
Introduction
Scaphoid nonunion after a fracture can occur secondary to undiagnosed fractures, fracture displacement, rotational instability, ischemia, or in up to 10% of fractures treated acutely with a headless compression screw.12,14,15,20 Treatment of scaphoid nonunion is paramount to preventing carpal collapse and wrist osteoarthritis.24,25,29
Surgical management of scaphoid nonunion is recommended to prevent pain, disability, and arthritis.1,23,24 Operative treatment for scaphoid nonunion is an evolving technique, but the current gold standard is headless compression screw fixation, typically with some form of bone grafting.12,20
Using a volar scaphoid locking plate is a newly described technique that may have some advantages over screw fixation in specific circumstances.8,9,15 The plate provides rotational stability, greater surface area contact for bone graft insertion, and may be more useful when there is a paucity of structurally sound bone to compress with a screw, especially in cases of segmental defect.5,7,10 The volar plate may improve scaphoid fracture fixation by resisting axial compression, rotation, and shear.8 Current proposed indications for plate fixation include revision scaphoid nonunion repair after screw fixation, chronic nonunion delayed greater than 2 years, and in cases of bone loss or where screw purchase is suboptimal with segmental bone defect.8
Bone quality has also been implicated as a potential determinant in strength of fixation.2 Disuse osteoporosis is common in chronic scaphoid nonunion, increases the difficulty of fixation, and merits consideration when selecting choice of fixation.17,28
The optimal nonvascularized bone graft in scaphoid nonunion is cancellous graft due to its superior biologic properties.11 However, cancellous graft lacks the structural integrity that cortical or corticocancellous graft provides. Therefore, fixation for scaphoid nonunion will need to be structurally resilient if cancellous graft is to be used without cortical support when needed. The aim of this article is to determine whether plate or screw fixation provides a greater mechanical advantage in a simulated scaphoid nonunion with segmental defect.
Methods and Materials
Study Design
Using previous biomechanical cadaveric studies as a reference, the investigators used a power analysis with an alpha error of 0.05 and 80% power to estimate that a minimum of 7 specimens per group would be necessary to have sufficient statistical power, with a difference of 20 N between specimens.13,18
In total, 32 scaphoids were dissected from forearms of 16 matched cadaver pairs. Cadavers were specifically obtained in 2 different groups in an effort to acquire osteoporotic and nonosteoporotic density specimens. Specimens were either males less than 60 years old or females greater than 60 years of age. No cadavers had any history of wrist trauma or surgery.
All forearm specimens were scanned with dual-energy X-ray absorptiometry, using the distal radius for measurement.17 The average T score for left wrist specimens was −2.13 ± 2.20, versus −2.18 ± 2.32 for the right wrist specimens (P = .95). To differentiate between densities, scaphoids were classified as either osteoporotic (T score ≤ –2.5, n = 13) or nonosteoporotic (T score > –2.5, n = 19). Ten scaphoids were osteopenic (T score between −1 and −2.5), and these were included in the nonosteoporotic group to generate a sample size great enough for comparison with the osteoporotic group.
Scaphoids from each matched pair were randomly assigned to receive either plate or screw fixation. Wrist pairs were randomized to determine type of fixation for the right or left hand.
Implant Application and Osteotomy
For the scaphoids receiving screw fixation, the scaphoid was dissected from the wrist and all soft tissue was removed. Each scaphoid was measured, specifically noting the midpoint of the scaphoid between proximal and distal poles. This point was marked, and 1.5-mm on either side of the point was also marked, to create a boundary for the osteotomy. The 3-mm osteotomy represents the segmental defect frequently encountered in scaphoid nonunion along the scaphoid waist, and also represents the site typically filled with bone graft. Using a custom-made guide, a 1.1-mm Kirschner wire (K-wire) was then inserted through the central axis of the scaphoid from distal to proximal.18 A 3-mm osteotomy was made using a fine precision saw along the previously marked boundaries. A 3-mm polyurethane spacer was inserted temporarily into the osteotomy site to preserve the height of the scaphoid during screw insertion. A 2.1-mm cannulated drill bit was used to predrill along the axis of the K-wire, according to manufacturer guidelines. A depth gauge was used to select appropriate screw length. A 3.0-mm headless screw (Medartis, AG, Austrasse, Basel, Switzerland) of either 18, 20, or 22 mm was inserted on power until the screw was flush with the near cortex. A hand screw driver was used to provide 3 further full turns, to 2-finger tightness, by the same investigator. The 3-mm spacer was removed after hardware installation.
For the scaphoids receiving plate fixation, a standard volar approach radial to flexor carpi radialis was used to dissect down to the scaphoid. Once the nonarticular volar portion of the scaphoid was fully visualized, the plate (Medartis, AG) was temporarily placed and the proximal- and distal-most screw holes of the plate were predrilled with a 1.1-mm K-wire. These predrilled holes served as landmarks for plate fixation after the scaphoid was dissected. These steps were performed to assure proper placement of the plate on the scaphoid with all anatomic landmarks still present. All soft tissue was dissected off of the scaphoid. The scaphoid was measured, the midpoint between proximal and distal poles noted, and a 3-mm segment was marked for the osteotomy as previously described. The plate was then placed on the volar aspect of the scaphoid and contoured, with attention to predrilled holes. The osteotomy was then made with a fine precision saw, and the 3-mm spacer was inserted. Afterward, the proximal and distal holes were predrilled with a 1.2-mm drill bit though the holes previously used, and the plate was secured to the scaphoid through those holes using 1.5-mm nonlocking screws. The other 4 holes were predrilled with the 1.2-mm drill bit, and then four 1.5-mm locking screws were inserted. The proximal and distal nonlocking screws were then traded for locking screws. All screws holes were measured with a depth gauge to appropriate length, using screws measuring between 9 and 15 mm.
Loading Configuration
Once fixation was installed and spacers were removed, the scaphoids were potted in cement to facilitate mounting on the load frame (TestResources, Inc, Shakopee, Minnesota). A 1.1-mm K-wire was first inserted in the proximal pole of the scaphoid, parallel to the osteotomy and perpendicular to the plane of rotational inertia experienced with cantilever bending, to serve as additional fixation in the cement. Polymethylmethacrylate (The Bosworth Company, Skokie, Illinois) was then poured into a custom-made collapsible wooden box, and the scaphoid was inserted, taking care to embed as much of the proximal pole as possible without allowing the cement to enter the osteotomized gap.
The scaphoids were mounted on the load frame and tested in axial compression in the technique previously described by other published studies (Figure 1).13,18 This mechanism represents the most frequent cause of scaphoid collapse, due to decreased cortical opposition with a segmental defect, which is commonly encountered in nonunion.9,21 Scaphoids were oriented in 45° of flexion to recreate the dorsal to volar cantilever force that is thought to cause the humpback deformity of a collapsed scaphoid.25 In vivo, this oblique loading is transmitted to the scaphoid by the trapezium, trapezoid, and capitate.6,16,22 Each model was loaded in compression at 0.125 mm/s until failure.
Figure 1.

Scaphoid cadaver with plate fixation mounted on load frame.
Data Analysis
Load to failure was defined as the load required to cause complete gap closure. For each trial, we recorded axial load and position. To determine the point of failure, video recordings were analyzed to identify the time interval that starts just before the gap begins to close and ends with the scaphoid poles making contact (complete gap closure). Within that time interval, the load to failure is the highest load that occurs just before the gap begins closing and well before a rapid increase in load capacity upon complete gap closure.
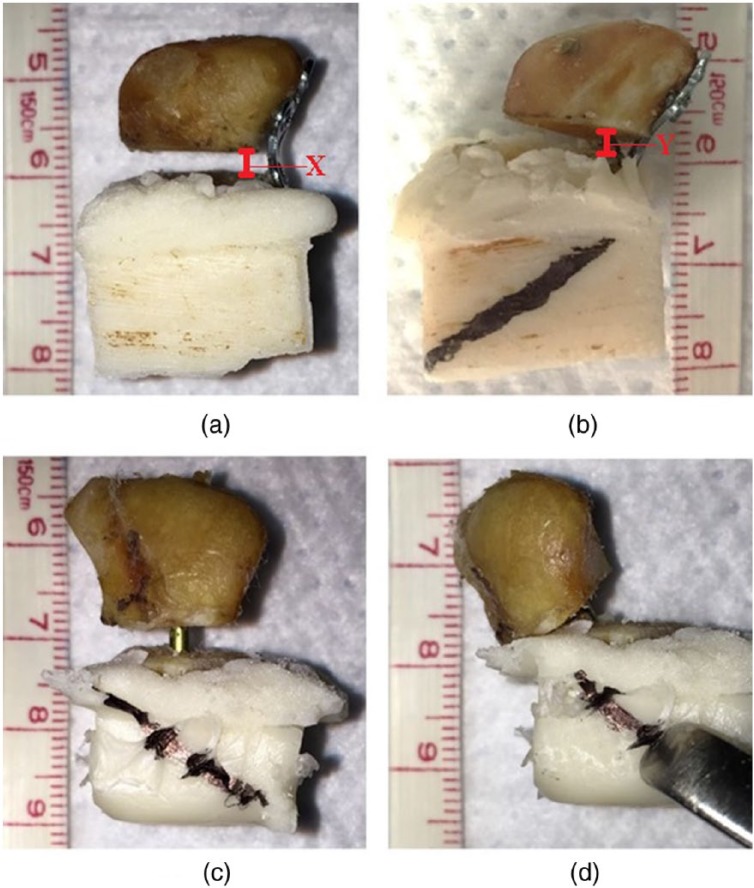
The amount of gap restoration after unloading, or percent gap recovery, was also recorded for each specimen to define to what extent, if any, the segmental gap was reestablished after gap closure. To normalize gap recovery for each specimen, this was calculated as the ratio: postload gap height / preload gap height. Gap measurements were recorded before and after loading for each specimen using high resolution photography (Figure 2). When measuring the gap, the smallest longitudinal dimension between the poles was recorded.
Figure 2.
Scaphoid cadavers with plate fixation (a, preloading, and b, postloading) and screw fixation (c, preloading, and d, postloading) representing typical mechanism of failure and gap recovery.
Note. Percent gap recovery is represented by the space remaining between the scaphoid poles after a load to failure and is represented by the distance Y/X. This gap represents the space in a scaphoid nonunion model that is without structural support after bone grafting.
Two-way independent analysis of variance was used to determine which groups, if any, were statistically different in load to failure.
Results
Load to failure was recorded as the mean for each group, including osteoporotic and nonosteoporotic plate and screw fixation (Table 1).
Table 1.
Mean Load to Failure With Standard Deviation for Each Density/Fixation Group.
| n | Average T score | Load to failure (N) | |
|---|---|---|---|
| Osteoporotic plate fixation | 5 | −4.2 ± 1.7 | 118.9 ± 40.6 |
| Osteoporotic screw fixation | 6 | −3.8 ± 1.6 | 114.1 ± 51.3 |
| Nonosteoporotic plate fixation | 9 | −1.1 ± 1.2 | 185.0 ± 87.5 |
| Nonosteoporotic screw fixation | 8 | −0.9 ± 1.2 | 131.5 ± 59.8 |
Four of the 32 scaphoid trials were excluded from data analysis due to errors in testing: In 2 normal density trials (1 plate and 1 screw), the scaphoids separated from the cement during testing, and in 2 osteoporotic trials (1 plate and 1 screw), gap closure failed to occur secondary to translation of the scaphoid poles. Complete gap closure occurred in all other trials.
Difference in load to failure was not statistically significant between plate and screw fixation in either nonosteoporotic or osteoporotic cadaver specimens (μ = 118.9, 114.1, 185.0, and 131.5 N for osteoporotic plate and screw fixation, and nonosteoporotic plate and screw fixation, respectively; P = .47).
All of the constructs fixed with plates failed by the plate initially bending, followed by gradual volar translation of the distal pole relative to the proximal pole (Figure 2). All of the screw constructs failed by screw cut-out and subsequent volar translation of the distal pole.
Percent gap recovery was higher for plate fixation than for screw fixation (μ = 40% ± 6% vs 4% ± 1% gap recovery for plate and screw fixation, respectively; P < .01). The mean preloading gap for the plate fixation group was 2.97 ± 0.29 mm, and the mean postloading gap was 1.21 ± 0.77 mm. The mean preloading gap for the screw fixation group was 2.95 ± 0.26 mm, and the mean postloading gap was 0.25 ± 0.59 mm.
Discussion
While plate and screw fixation demonstrate similar loads to failure in scaphoid fractures with segmental defects, plate fixation performs superiorly to screw fixation for gap recovery. This difference is important, because recovery of scaphoid height in a nonunion scenario is critical to preventing subsequent scaphoid collapse and secondary radiocarpal and periscaphoid arthrosis.12,20,24
The advantage of the locking plate in gap recovery is thought to be due to the locking plate’s quality as a fixed-angle construct and due to the amount of elastic deformation that the plate will tolerate. Because the plate is able to partially return to its original shape after loading, this is likely due to the plate acting within its elastic modulus of 105 GPa. This biomechanical study stresses different aspects of each fixation method due to their unique attributes: The plate’s mechanical properties are tested, while the screw trials specifically stress the screw-bone interface.
In consideration of the plate’s ability to superiorly recover scaphoid gaps after a load to failure, the authors advocate for plate fixation of “complicated” scaphoid fractures and nonunions, especially those with large segmental defects, disuse osteoporosis, delayed presentation, or failed screw fixation.
The segmental defect or collapsed deformity often encountered in scaphoid nonunion may be due to fibrous nonunion, comminution, avascular necrosis, or a chronic defect in bone. Cancellous bone is the ideal graft choice for scaphoid nonunion because of its superior osteoconductive and osteoinductive properties, and because it incorporates faster than corticocancellous grafts.11 However, purely cancellous grafts do not offer structural support, and so the ideal fixation device if cancellous graft is to be used must provide both structural support and space for the graft. The segmental gap, bridged by either a plate or a screw in this study, simulates the scaphoid waist gap that would be without structural support from a graft postoperatively. This study demonstrates that the plate performs superiorly to the screw in recovery of that gap after a load. Furthermore, the plate creates and stabilizes a gap, while the screw crosses and disrupts that gap, or potential space for grafting. The screw may also threaten graft space by displacing bone graft during screw insertion or by compressing across the segmental gap when there is limited bone. Last, when inserted, screws are more likely to allow the gap to collapse. These clinical scenarios suggest that plates may be a superior choice in nonunion with segmental defect.
To date, there are 3 published case series that provide clinical outcome data for plate fixation of scaphoid nonunion, including 31 cases using either vascularized or iliac crest bone graft. The authors report union at 2 to 7 months, and 1 failed union among the 31 cases.8,9,15 It is notable that none of these series used purely cancellous graft but rather corticocancellous. Even pedicled corticocancellous vascularized bone graft has been unpredictable for this indication.4,19,26
The authors expected to find a statistically significant difference in load to failure between osteoporotic and nonosteoporotic groups. This lack of significant difference is likely due to the large variance of the data and suggests that specific scaphoid morphology and microarchitecture may be more significant in determining load to failure than density alone.
The results of this study are similar to results of other published work. Compared with biomechanical studies using polyurethane models, cadaver studies have higher variance in load to failure.6,13,18 The load to failure data from our study are similar to that over other scaphoid biomechanical studies.6,13,18,27 While a similar cadaveric biomechanical study by McCallister et al describes loads to failure of 712 ± 412 and 513 ± 354 N for central and eccentric screw placement, respectively, our study’s setup differs dramatically in that we used a scaphoid osteotomy to simulate a nonunion scenario.18 In general, lower loads to failure are expected from a construct with a gap or with multiple osteotomies, as was the case in Koh et al, another cadaveric biomechanical study, where mean loads to failure were 123.95, 142.21, and 170.62 N for different types of headless screws in simulated nonunion fixation using osteotomized cadavers.13 This is the first study to our knowledge to test scaphoid fixation with a segmental gap, as opposed to a simple osteotomy with remaining bony contact.3
There are limitations to this study. Power analysis and funding supported the examination of 32 wrist cadavers, but the large variance between trials yielded a study that is likely underpowered. The authors believe that the variance is due mainly to inconsistency in scaphoid morphology, especially because such variance is not encountered in polyurethane studies using similar methods.6 A power analysis was done with the updated specimen variability, and 7 additional specimens per group would be required to evaluate a 65-N difference between fixation and density groups with 80% power. In addition, because this is a biomechanical study, the clinical implications of the results cannot be definitively determined. The design of our study is validated in previous literature and is consistent with the accepted method of scaphoid loading.13,18,25
From a biomechanical standpoint, the authors propose that locking plate fixation be considered at least equivalent to screw fixation for scaphoid nonunion and that locking plate fixation is superior to screw fixation for gap recovery. Given the results of this study, and the authors’ experience, we recommend considering plate fixation in circumstances where there is concern for delayed healing or the presence of a large defect such as scaphoid nonunion after failed screw fixation, scaphoid fracture or nonunion with substantial bone loss or segmental defect, and scaphoid comminution. Furthermore, potential clinical benefits of volar locking plates are beyond the scope of this particular study but are being investigated by the authors.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Scott G. Edwards is a consultant for Medartis. The other authors declare that they have no conflicts of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Testing materials for this study were provided by Medartis. Medartis had no role in the study design, data collection, analysis, or interpretation of this study, nor did Medartis have any role in manuscript preparation or the decision to submit the manuscript for publication.
References
- 1. Amadio PC, Berquist TH, Smith DK, et al. Scaphoid malunion. J Hand Surg Am. 1989;14:679-687. [DOI] [PubMed] [Google Scholar]
- 2. Augat P, Iida H, Jiang Y, et al. Distal radius fractures: mechanisms of injury and strength prediction by bone mineral assessment. J Orthop Res. 1998;16:629-635. [DOI] [PubMed] [Google Scholar]
- 3. Beutel BG, Melamed E, Hinds RM, et al. Mechanical evaluation of four internal fixation constructs for scaphoid fractures. Hand (N Y). 2016;11:72-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chang MA, Bishop AT, Moran SL, et al. The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg Am. 2006;31:387-396. [DOI] [PubMed] [Google Scholar]
- 5. Cooney WP, Linscheid RL, Dobyns JH, et al. Scaphoid nonunion: role of anterior interpositional bone grafts. J Hand Surg Am. 1988;13:635-650. [DOI] [PubMed] [Google Scholar]
- 6. Crawford LA, Powell ES, Trail IA. The fixation strength of scaphoid bone screws: an in vitro investigation using polyurethane foam. J Hand Surg Am. 2012;37:255-260. [DOI] [PubMed] [Google Scholar]
- 7. Daly K, Gill P, Magnussen PA, et al. Established nonunion of the scaphoid treated by volar wedge grafting and Herbert screw fixation. J Bone Joint Surg Br. 1996;78:530-534. [PubMed] [Google Scholar]
- 8. Dodds SD, Patterson JT, Halim A. Volar plate fixation of recalcitrant scaphoid nonunions with volar carpal artery vascularized bone graft. Tech Hand Up Extrem Surg. 2014;18:2-7. [DOI] [PubMed] [Google Scholar]
- 9. Ghoneim A. The unstable nonunited scaphoid waist fracture: results of treatment by open reduction, anterior wedge grafting, and internal fixation by volar buttress plate. J Hand Surg Am. 2011;36:17-24. [DOI] [PubMed] [Google Scholar]
- 10. Jurkowitsch J, Dall’Ara E, Quadlbauer S, et al. Rotational stability in screw-fixed scaphoid fractures compared to plate-fixed scaphoid fractures. Arch Orthop Trauma Surg. 2016;136:1623-1628. [DOI] [PubMed] [Google Scholar]
- 11. Kakar S, Einhorn T. Biology and enhancement of skeletal repair. In: Skeletal Trauma, 4th ed. Philadelphia, PA: Saunders; 2009:33-50. [Google Scholar]
- 12. Kawamura K, Chung KC. Treatment of scaphoid fractures and nonunions. J Hand Surg Am. 2008;33:988-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koh I-H, Kang H-J, Kim J-S, et al. A central threadless shaft screw is better than a fully threaded variable pitch screw for unstable scaphoid nonunion: a biomechanical study. Injury. 2015;46:638-642. [DOI] [PubMed] [Google Scholar]
- 14. Ledoux P, Lamblin D, Targowski R. Modifications to the mechanical behavior of the wrist after fracture of the scaphoid. Modeling by finite element analysis. Acta Orthop Belg. 2001;67:236-241. [PubMed] [Google Scholar]
- 15. Leixnering M, Pezzei C, Weninger P, et al. First experiences with a new adjustable plate for osteosynthesis of scaphoid nonunions. J Trauma. 2011;71:933-938. [DOI] [PubMed] [Google Scholar]
- 16. Li B, Aspden RM. Composition and mechanical properties of cancellous bone from the femoral head of patients with osteoporosis or osteoarthritis. J Bone Miner Res. 1997;12:641-651. [DOI] [PubMed] [Google Scholar]
- 17. Madeley NJ, Stephen AB, Downing ND, Davis TRC. Changes in scaphoid bone density after acute fracture. J Hand Surg Br. 2006;31:368-370. [DOI] [PubMed] [Google Scholar]
- 18. McCallister WV, Knight J, Kaliappan R, et al. Central placement of the screw in simulated fractures of the scaphoid waist: a biomechanical study. J Bone Joint Surg Am. 2003;85-A:72-77. [DOI] [PubMed] [Google Scholar]
- 19. Merrell GA, Wolfe SW, Slade JF. Treatment of scaphoid nonunions: quantitative meta-analysis of the literature. J Hand Surg Am. 2002;27:685-691. [DOI] [PubMed] [Google Scholar]
- 20. Moon ES, Dy CJ, Derman P, et al. Management of nonunion following surgical management of scaphoid fractures: current concepts. J Am Acad Orthop Surg. 2013;21:548-557. [DOI] [PubMed] [Google Scholar]
- 21. Muller M, Allgower M, Schneider R. Buttress Plate Manual of Internal Fixation. 3rd ed. Heidelberg, Germany: Springer-Verlag; 1991. [Google Scholar]
- 22. Patel PSD, Shepherd DET, Hukins DWL. Compressive properties of commercially available polyurethane foams as mechanical models for osteoporotic human cancellous bone. BMC Musculoskelet Disord. 2008;9:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reigstad O, Grimsgaard C, Thorkildsen R, et al. Long-term results of scaphoid nonunion surgery: 50 patients reviewed after 8 to 18 years. J Orthop Trauma. 2012;26:241-245. [DOI] [PubMed] [Google Scholar]
- 24. Ruby LK, Stinson J, Belsky MR. The natural history of scaphoid non-union. A review of fifty-five cases. J Bone Joint Surg Am. 1985;67:428-432. [PubMed] [Google Scholar]
- 25. Smith DK, Cooney WP, An KN, et al. The effects of simulated unstable scaphoid fractures on carpal motion. J Hand Surg Am. 1989;14:283-291. [DOI] [PubMed] [Google Scholar]
- 26. Straw RG, Davis TRC, Dias JJ. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1,2 intercompartmental supraretinacular branch of the radial artery. J Hand Surg Br. 2002;27:413. [DOI] [PubMed] [Google Scholar]
- 27. Sugathan HK, Kilpatrick M, Joyce TJ, et al. A biomechanical study on variation of compressive force along the Acutrak 2 screw. Injury. 2012;43:205-208. [DOI] [PubMed] [Google Scholar]
- 28. Wagner MA, Frigg R. Locking plates: development, biomechanics and clinical application. In: Skeletal Trauma, 4th ed. Philadelphia, PA: Saunders; 2009:143-176. [Google Scholar]
- 29. Watanabe K. Analysis of carpal malalignment caused by scaphoid nonunion and evaluation of corrective bone graft on carpal alignment. J Hand Surg Am. 2011;36:10-16. [DOI] [PubMed] [Google Scholar]