Abstract
Fungal rhino-orbital sinusitis due to mucormycetes is a rapidly progressive condition with high mortality, rarely seen in immunocompetent individuals. A 26-year-old immunocompetent male presented with rhino-orbital mucormycosis after a history of dental manipulation. The patient was successfully managed with a combination of surgery, amphotericin B, and posaconazole. Here, we highlight the delay in diagnosis and challenges faced in the management.
Keywords: Amphotericin B, Mucormycosis, Posaconazole
Introduction
Mucormycosis is a potentially fatal angioinvasive fungal infection with high prevalence in India owing to the high endemicity of diabetes and the hot and humid climatic conditions conducive to the growth of the fungi.[1] Reports of mucormycosis in apparently immunocompetent individuals is increasing in recent times.[2] In immunocompetent patients with rhino-orbital mucormycosis, it is postulated that previous infection or trauma of the upper respiratory tract may predispose the individual to the omnipresent spores of the fungi.[3] We present a rare case of rhino-orbital mucormycosis after oral injections in a young immunocompetent male.
Case History
A 26-year-old male teacher, resident of Uttar Pradesh (state in northern part of India) presented to a dentist with right-sided dental pain for 3 days. He was injected locally at the site of pain. One week later, he presented to a local hospital with fever, headache, and gradually progressive swelling and redness of right side of the face. The swelling progressed to involve the right eye. He was prescribed multiple antibiotics without any improvement. He continued to have high-grade fever and headache. His right eye started to swell and protrude from the orbit to an extent that he was not able to open his eye. A right eye enucleation was performed. Culture from corneal scrapings revealed Aspergillus flavus and methicillin-resistant coagulase negative Staphylococcus spp. The culture from the representative tissues and fluids from other parts of the eye were sterile. He received ceftriaxone and vancomycin for 7 days. The cheek swelling continued to increase in the right side and started to appear on the left side later. A contrast-enhanced computed axial tomography (CECT) of the face revealed bilateral rhinosinusitis [Figure 1]. With a suspicion of invasive fungal rhinosinusitis, endoscopic debridement of right maxillary sinus was done which showed no hyphae. He was continued on intravenous antibiotics but did not respond. A serum galactomannan was done which turned out to be positive with an optical density (OD) value of 0.75. Voriconazole was added at this point. The patient was referred with nonresolving symptoms. A new onset collection was noted in the left cheek below the eye. This was aspirated and an emergency gram stain and a KOH mount was performed. The gram stain revealed gram negative bacilli and KOH showed few aseptate hyphae [Figures 2 and 3]. With an impression of invasive mucormycosis and secondary gram negative infection, voriconazole was changed to intravenous liposomal amphotericin B and imipenem was added empirically. The bacterial culture was positive for Escherichia coli sensitive to beta lactam/beta lactamase inhibitor and carbapenem but the fungal culture was negative. An extensive debridement and right maxillary exenteration was done after 3 days which showed field full of aseptate hyphae. Patient was improving postoperatively on imipenem and amphotericin. He was advised maxillary exenteration in the left side but he refused. Amphotericin B (250 mg) was given for a total of 1 month in the inpatient setting. There was a considerable decrease in cheek swelling. Posaconazole was arranged for the patient under government health scheme for poor patients. Follow-up after 2 months of discharge showed considerable decrease in the swelling both clinically and radiologically [Figure 4].
Figure 1.
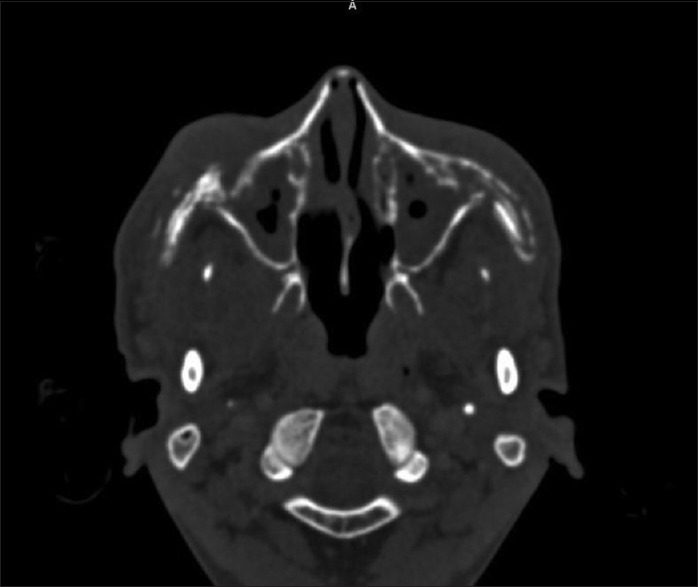
Axial contrast tomography section at the level of maxillary sinus showing soft tissue in bilateral maxillary sinuses and nasal cavity with destruction of bilateral maxilla and medial wall of maxillary sinuses
Figure 2.
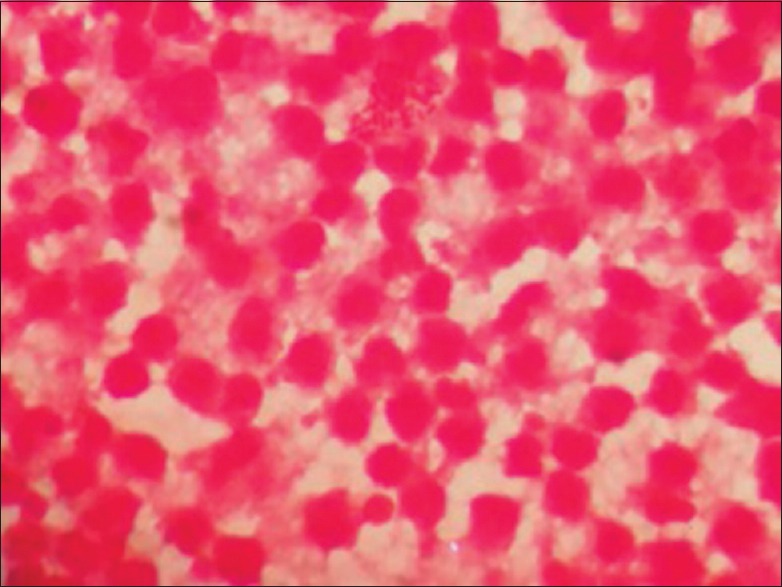
Gram stain of the aspirated pus shows field full of pus cells along with few gram negative bacilli
Figure 3.
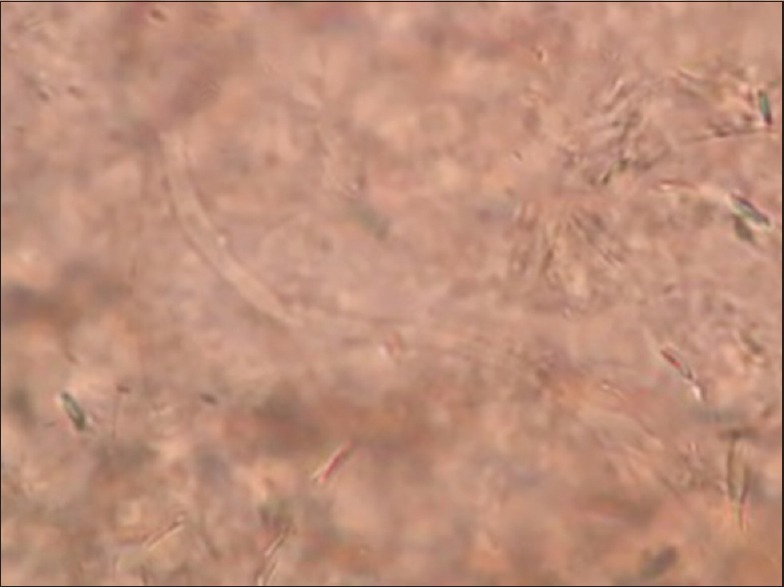
KOH mount from the aspirated pus shows aseptate hyphae
Figure 4.
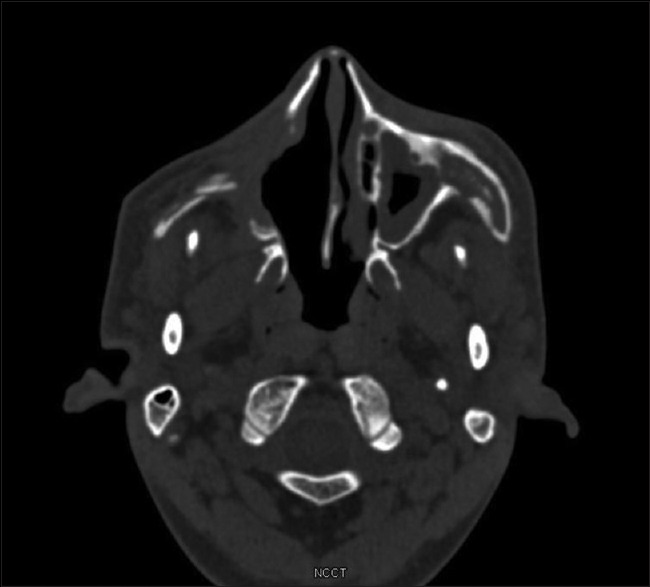
Post exenteration and post treatment scan showing persistent soft tissue in left maxillary sinus with associated bony destruction but on the right side there is no residual soft tissue with post exenteration changes suggesting partial response
Discussion
Mucormycosis is caused by an angioinvasive aggressive fungi, the spores of which are commonly found in the environment. It colonizes the upper airway of the individuals and utilizes the depressed function of innate immune cells in the immunosuppressed to invade the deeper tissues.[4] However, in immunocompetent patients, prior history of infection or trauma may predispose the individual to the disease. Very few reports of mucormycosis post-dental manipulation has been published in the literature.[3]
The disease is acutely invasive and progresses to involve the sinus, orbits and eventually the brain. Mucormycosis should always be the kept in the differential in a progressive lesion involving the cheek and eyes. Although Aspergillus spp. and other fungi can present in a similar fashion but their course is more indolent.[5] In cases where mucormycosis is a suspicion, broad-spectrum antifungals like amphotericin B should be initiated. Voriconazole, even though, is the drug of choice for aspergillosis, has no activity against mucormycosis.[6] Our patient was initially started on broad-spectrum antibiotics and voriconazole in view of the positive serum galactomannan and the positive Aspergillus spp. culture. In hindsight, it was most likely a contaminant as other parts of the eyeball were sterile. It has to be kept in mind that a heavy reliance on serum galactomannan test in clinically incompatible situations may also be misleading.[7]
The ultimate treatment for mucormycosis is surgical debridement. Amphotericin B is the drug of choice for mucormycosis, but unfortunately, the duration of amphotericin B is not standardized and patients may require months of amphotericin B therapy depending on the extent of the disease.[8] Although posaconazole is an attractive oral alternative for switch therapy once the patient is stable, the currently available suspension form in India is expensive and has erratic pharmacokinetics.[9,10] Patients have to be monitored closely for compliance and recurrence of symptoms.
There is a need for increased awareness among the primary care physicians regarding the possibility of mucormycosis in immunocompetent individuals as delay in diagnosis may lead to significant morbidity and mortality. Early diagnosis, aggressive surgery, and adequate duration of therapy are the keys for successful management of an otherwise fatal disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chakrabarti A, Singh R. Mucormycosis in India: Unique features. Mycoses. 2014;57(Suppl 3):85–90. doi: 10.1111/myc.12243. [DOI] [PubMed] [Google Scholar]
- 2.Prakash H, Ghosh AK, Rudramurthy SM, Singh P, Xess I, Savio J, et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med Mycol. 2018 doi: 10.1093/mmy/myy060. doi: 10.1093/mmy/myy060. [DOI] [PubMed] [Google Scholar]
- 3.Venkatesh D, Dandagi S, Chandrappa PR, Hema KN. Mucormycosis in immunocompetent patient resulting in extensive maxillary sequestration. J Oral Maxillofac Pathol. 2018;22(Suppl 1):S112–6. doi: 10.4103/jomfp.JOMFP_163_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ibrahim AS, Voelz K. The mucormycete-host interface. Curr Opin Microbiol. 2017;40:40–5. doi: 10.1016/j.mib.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trief D, Gray ST, Jakobiec FA, Durand ML, Fay A, Freitag SK, et al. Invasive fungal disease of the sinus and orbit: A comparison between mucormycosis and Aspergillus. Br J Ophthalmol. 2016;100:184–8. doi: 10.1136/bjophthalmol-2015-306945. [DOI] [PubMed] [Google Scholar]
- 6.Gupta N, Kumar A, Singh G, Ratnakar G, Vinod KS, Wig N. Breakthrough mucormycosis after voriconazole use in a case of invasive fungal rhinosinusitis due to Curvularia lunata. Drug Discov Ther. 2017;11:349–52. doi: 10.5582/ddt.2017.01060. [DOI] [PubMed] [Google Scholar]
- 7.Kostamo K, Richardson M, Eerola E, Rantakokko-Jalava K, Meri T, Malmberg H, et al. Negative impact of Aspergillus galactomannan and DNA detection in the diagnosis of fungal rhinosinusitis. J Med Microbiol. 2007;56:1322–7. doi: 10.1099/jmm.0.47101-0. [DOI] [PubMed] [Google Scholar]
- 8.Pilmis B, Alanio A, Lortholary O, Lanternier F. Recent advances in the understanding and management of mucormycosis. F1000Res. 2018:7. doi: 10.12688/f1000research.15081.1. pii: F1000Faculty Rev.1429. doi: 10.12688/f1000research. 15081.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manesh A, John AO, Mathew B, Varghese L, Rupa V, Zachariah A, et al. Posaconazole: An emerging therapeutic option for invasive rhino-orbito-cerebral mucormycosis. Mycoses. 2016;59:765–72. doi: 10.1111/myc.12529. [DOI] [PubMed] [Google Scholar]
- 10.Kendall J, Papich MG. Posaconazole pharmacokinetics after administration of an intravenous solution, oral suspension, and delayed-release tablet to dogs. Am J Vet Res. 2015;76:454–9. doi: 10.2460/ajvr.76.5.454. [DOI] [PubMed] [Google Scholar]


