Abstract
Fungal rhinosinusitis is not very uncommon in diabetic patients, but Scedosporium apiospermum as a cause of this infection is rare. We report a case of fungal rhinosinusitis by Scedosporium spp. in a diabetic male along with literature review. The patient is on voriconazole, with adequate therapeutic response after 6 months of follow up.
Keywords: Diabetes, rhinosinusitis, Scedosporium apiospermum
Introduction
Scedosporium apiospermum is a ubiquitous fungus. The clinical importance of this fungus is mostly seen with immunocompromised host and rarely in immunocompetent patients.[1] It can present with wide variety of clinical spectrum. Hereby, we report a case of Scedosporium apiospermum infection causing rhinosinusitis a rare clinical entity in a diabetic male.
Case Report
A 79-year-old gentleman resident of Delhi, known case of diabetes mellitus with well controlled sugar on oral hypoglycemic medication presented with complaints of progressive painless diminished vision in right eye for last 4 years. There was no history of fever, swelling, redness, or watering from eye, headache, altered behavior, vomiting, facial deviation, seizures, or any other neurological deficits. He consulted ophthalmologist for decreasing vision at outside hospital who initially attributed it to diabetes retinopathy but due to progressive unexplained vision loss to the level of loss of perception of light in right eye and 6/6 in left eye (with refractive error correction) a computed tomography (CT) scan of head was done which showed poorly defined soft tissue mass in posterior part of the orbit along with involvement of right paranasal sinuses. He was started on oral steroids and referred to a higher center. Patient presented to our center with loss of perception of light in his right eye. He complained of easy fatigability and generalized tiredness. His glycemic control on steroids was very poor. Because of unilateral eye involvement, with a soft tissue mass in CT scan orbit, magnetic resonance imaging (MRI) head along with brain was done. The MRI showed the involvement of maxillary sinus, ethmoid sinus, sphenoid sinus, and orbit at right side [Figure 1]. The patient was referred to Department of ENT and transnasal maxillary and ethmoid sinus biopsy was taken. The biopsy revealed in KOH mounts hyaline thin septate hyphae. A multidisciplinary approach by ophthalmologist, ENT specialist, radiologist, microbiologist, and infectious disease specialist worked up further. Routine laboratory examination was normal. There was no history of trauma, travel, drowning, or near drowning or swimming or religious water dips. Steroids were tapered and stopped. Based upon the finding of thin septate hyphae in KOH mount, he was empirically started on itraconazole. Patient did not show any improvement. Subsequently, the fungal culture of sinus tissue biopsy showed Scedosporium apiospermum. After the culture report came, the treatment was modified. He was started on intravenous voriconazole 300 mg for two doses followed by 200 mg twice a day. Therapeutic drug monitoring with serum trough levels was checked on day 5 of starting voriconazole. Patient was shifted on oral voriconazole and discharged tested again at 1 month follow up. On 1 and 3 month follow-up drug levels of voriconazole were maintained in therapeutic range, along with symptomatic improvement. Radiologically, on repeat MRI significant resolution was appreciated [Figure 2].
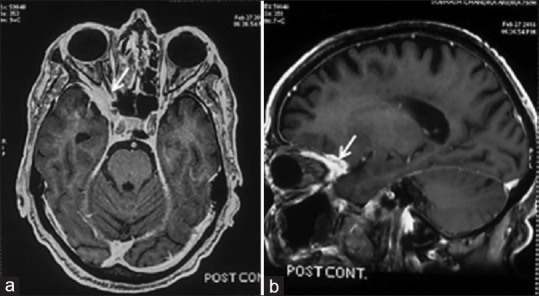
Figure 1.

Baseline Contrast enhancement magnetic resonance imaging Head. CEMRI Head A shows enhancing lesions in the right sphenoid sinus and right orbit (arrow in a) and right orbit, right ethmoid sinus and right maxillary sinus (arrow in b). Findings are suggestive of infective etiology (rhinosinusitis with orbit involvement)
Figure 2.
Follow-up Scan on treatment (Contrast enhancement magnetic resonance imaging Head. CEMRI after six months). CECT Head (a and b) shows significant resolution of the disease involving the sinuses. Right orbit apex still shows enhancement but significantly improved (arrow in a and b). Findings are suggestive of good treatment response
Discussion
The genus Scedosporium is ubiquitous in nature found in soil and water. An increase in incidence of scedosporiosis in recent years could be because of increased use of immunosppressive drugs and antifungals that lacks adequate activity against Scedosporium spp. leading to selective pressure and contributing to the increasing incidence of Scedosporium infections.[2]
The involvement of Central nervous system (CNS) can be through direct inoculation, by direct extension from the adjacent area, or by hematogenous spread from distant infection like skin or lungs. Many reports of CNS scedosporiosis have been reported due to aspiration of polluted water or because of near drowning infecting sinuses leading to direct CNS invasion. In the present case, there was no such history of the patient, which still makes it difficult to assess the route of infection of this rare pathogen.[3]
Rhinosinusitis is also an uncommon presentation of scedosporium infections. Till date five cases of rhinosinusitis caused by Scedosporium species are reported in English literature[Table 1].[4,5,6,7,8] In present case, the patient is a known diabetic on oral hypoglycemic drugs with adequate blood sugar control who is doing well on 6 months follow up.
Table 1.
Cases of Scedosporium apiospermum rhinosinusitis previously reported in English literature
| Year of reporting | Place | Age/sex | Site involvement/spectrum of disease | Comorbity/significant history | Outcome |
|---|---|---|---|---|---|
| 1998[4] | Brazil | 40 years/Male | Sinusitis with pneumonia | Bone marrow transplant | Died |
| 1999[5] | USA | 21 years/Male | Sinusitis | Hemophilia, AIDS | Died |
| 2009[6] | Chile | 47 years/Female | Rhinosinusitis | Previous nasal surgery | Improved |
| 2013[7] | India | 67 years/Female | Sinusitis with squamous cell carcinoma (Pterygopalatine fossa) | IgA nephropathy, hypertension, hypothyroidism | Lost to follow up |
| 2015[8] | India | 35 years/Female | Sinusitis with nasal polyp | None | Improved |
| Present Case | India | 79 years/Male | Rhinosinusitis along with orbit involvement | Diabetes mellitus | Improving |
Diagnosis of these infections caused by Scedosporium spp. is made using radiological and microbiological tools. In microscopy, the appearance of this fungus is similar to common hyaline hyphomycetes. So, the final diagnosis of scedoporiosis is based on isolation of the fungus in culture.[9] As, in present case the final confirmation of this infection was on the basis of tissue biopsy culture growing Scedosporium apiospermum.
The management of this infection is by surgical debridement and antifungals. The choice of antifungals is voriconazole. Both single as well as combination therapy based on voriconazole is recommended. Most recommended combination is with terbinafine. The serum trough concentration of voriconazole is required to be monitored to be kept between 1 and 5 mcg/mL. In present case, the patient was started on voriconazole based on diagnosis of scedosporiosis.
The case highlighted the fact that everything that looks same can still be different, and the physicians should keep Scedosporium spp. as a close differential of rhinosinusitis, as antifungals that are active in Aspergillus spp. may not always be effective against Scedosporium spp. Also with rising incidence of immunosuppressive disorders and diabetes the Scedoporium spp. causing such infections should always be kept in mind and as such looked for the same. As in present case, a diabetic patient without any history of drowning or swimming, or any surgical intervention suffered fungal rhinosinusitis caused by this rare pathogen, though with the timely diagnosis and adequate management he has improved clinically with significant radiological resolution.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Goldman C, Akiyama MJ, Torres J, Louie E, Meehan SA. Scedosporium apiospermum infections and the role of combination antifungal therapy and GM-CSF: A case report and review of the literature. Med Mycol Case Rep. 2016;11:40–3. doi: 10.1016/j.mmcr.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamaris GA, Chamilos G, Lewis RE, Safdar A, Raad II, Kontoyiannis DP. Scedosporium infection in a tertiary care cancer center: A review of 25 cases from 1989 to 2006. Clin Infect Dis. 2006;43:1580–4. doi: 10.1086/509579. [DOI] [PubMed] [Google Scholar]
- 3.Kantarcioglu AS, Guarro J, de Hoog GS. Central nervous system infections by members of the Pseudallescheria boydii species complex in healthy and immunocompromised hosts: Epidemiology, clinical characteristics and outcome. Mycoses. 2008;51:275–90. doi: 10.1111/j.1439-0507.2008.01489.x. [DOI] [PubMed] [Google Scholar]
- 4.Machado CM, Martins MA, Heins-Vaccari EM, Lacaz Cda S, Macedo MC, Castelli JB, et al. Scedosporium apiospermum sinusitis after bone marrow transplantation: Report of a case. Rev Inst Med Trop Sao Paulo. 1998;40:321–3. doi: 10.1590/s0036-46651998000500010. [DOI] [PubMed] [Google Scholar]
- 5.Eckburg PB, Zolopa AR, Montoya JG. Invasive fungal sinusitis due to Scedosporium apiospermum in a patient with AIDS. Clin Infect Dis. 1999;29:212–3. doi: 10.1086/520164. [DOI] [PubMed] [Google Scholar]
- 6.Chanqueo L, Gutiérrez C, Tapia C, Silva V, Razeto L, Misad C, et al. Scedosporium apiospermum rhinosinusal infection in an immunocompetent host. Rev Chilena Infectol. 2009;26:453–6. [PubMed] [Google Scholar]
- 7.Giri S, Kindo AJ, Rao S, Kumar AR. Unusual causes of fungal rhinosinusitis: A study from a tertiary care centre in South India. Indian J Med Microbiol. 2013;31:379–84. doi: 10.4103/0255-0857.118901. [DOI] [PubMed] [Google Scholar]
- 8.Rynga D, Capoor MR, Varshney S, Naik M, Gupta V. Scedosporium apiospermum an emerging pathogen in India: Case series and review of literature. Indian J Pathol Microbiol. 2017;60:550–5. doi: 10.4103/IJPM.IJPM_742_16. [DOI] [PubMed] [Google Scholar]
- 9.Kwon Chung KJ, Bennett JE. Infections due to miscellaneous molds. In: Kwon Chung KJ, Bennett JE, editors. Medical Mycology. Philadelphia: Lea and Febiger; 1992. pp. 733–67. [Google Scholar]


