Abstract
Aim:
To assess the association between maternal dental anxiety and its effect on the oral health status of their child, in Murad nagar –An institutional cross-sectional study.
Materials and Methods:
Among the randomly selected 200 mother-child pairs, a cross-sectional study was done. The children of 2–5 years were selected for the study. A five-level Modified Dental Anxiety Scale (MDAS), Hindi edition, was used to assess dental anxiety among the mothers. Clinical examination of the wards was finished by using a modified gingival record and WHO dentition status (2013). The SPSS software version 20 was used for statistical analysis.
Results:
Approximately, 61% of the children were males, and 39% were females. The modified gingival index (MGI) score was high, if there should arise an occurrence of high MDAS values. The mean MGI score was most astounding in phobic class of MDAS and least in the not anxious classification. The MGI score expanded on increment in maternal anxiety. Dental caries expanded in kids, if there should be an occurrence of high maternal dental uneasiness. The MDAS demonstrated a critical association with clinical oral health results of the child. The children whose mothers were “extremely anxious” (phobic) had the highest mean decayed, missing, or filled teeth.
Conclusion:
Maternal dental anxiety significantly affects the oral health status of their ward.
Keywords: Behavior, dental caries, Modified Dental Anxiety Scale, Modified Gingival Index
Introduction
Anxiety has been defined as a “state of unpleasantness with associated fear of danger from within or a learned process of one's own environment. ”[1] Anxiety and fear toward dental treatment are common problems frequently experienced by patients worldwide. Dental anxiety is ranked fourth among common fears and ninth among intense fears.[2]
Most children are affected by dental caries in their early childhood. Pain and fear due to dental caries and its treatment do not let a child seek preventive and curative treatment in an early stage. Family income also plays a crucial role in taking dental treatment. Dental caries affects the self-confidence of children along with affecting their chewing, smiling, speaking, etc., Dental caries in primary dentition also affects the permanent dentition. Dental caries is multi-factorial in nature. According to Keyes triad,[3] environmental factors also play an important role in dental caries development.
The families of young children and their own mindset toward seeking dental treatment also affect the oral health of their child. Usually, mothers spend most of their times with the child in early age, and the behavior of the child get influenced by maternal beliefs including their child's dental health. It was found in a study done by Niji R et al.[4] that maternal age at birth of their child also affects the oral health of the child. Children born from mothers younger than 23 years had the highest prevalence of caries and decayed, missing, or filled teeth (dmft).[4] Child's negative behavior was also attributed to fearful and anxious parents. Children with negative behavior for dental treatment were really difficult to treat. Sometimes it leads to symptomatic treatment by the dentist rather than an ideal treatment plan. These children also have high dental morbidity and oral health issues.
This study was done to assess the association between maternal dental anxiety and its effect on the oral health status of their child.
Materials and Methods
A cross-sectional examination was directed in the outpatient department of Department of Public Health Dentistry of ITS Dental College, Murad nagar, Ghaziabad, India. The investigation was done on the relationship between maternal dental anxiety and its impact on the oral health status of their ward. Before starting the study, ethical clearance was obtained from the ethical committee of ITS - Centre for Dental Studies and Research (ITS-CDSR) Murad nagar. Written consent from guardians of wards was taken before their cooperation and clinical examination of their wards in the investigation. Two hundred mother-child pairs were arbitrarily chosen for the investigation. The study period was 6 months from June 2017 to December 2017. The calibration of the principal investigator was done in the Department of Public Health Dentistry ITS CDSR Murad nagar, Ghaziabad to limit the examiner variability.
Inclusion criteria
Mother-child pairs, attending for dental treatment
Child's age between 2 and 5 years.
Exclusion criterion
Children with special health needs.
Statistical analysis
The statistical analysis was finished by utilizing Statistical Package for Social Sciences (SPSS) version 20.0. The results were found statistical significant with P value equal or less than 0.05. Data were statistically compiled, and the master table was prepared on a computer after conversion of data from a pre-coded proforma to the computer. Significant dispersion and introduction of information were done in tables and graphs.
Data collection
A pretested, organized survey was filled by a solitary calibrated interviewer to inspect maternal demographic factors, and clinical examination of the wards was finished by the inspector by using modified gingival index[5] (MGI) and WHO dentition status 2013.[6] Modified Dental Anxiety Scale (MDAS) {Hindi version} was used to evaluate the maternal dental anxiety. The MDAS is an exceedingly steady and solid measure, which has great discriminant and simultaneous legitimacy. The 5-item MDAS has been created by the adjustment of Corah's Dental Anxiety Scale.[7] The MDAS survey makes inquiries beginning from the sentiment of having a meeting with the dental practitioner to having a tooth being bored and in conclusion having a local anesthesia injection being infused into the gums. This Likert scale has a score range from 5 to 25, with each item's response ranging from 1 to 5 as follows: Not anxious (1), Slightly anxious (2), Fairly anxious (3), Very anxious (4), and Phobic (5). The data entry was made around the same time with a specific end goal to amend any disparity.
Results
Two hundred pairs of mother-child were included in our investigation. Approximately, 39% of children were females and 61% were males [Graph 1]. The percentage of children in each age group [Graph 2] was as follows: 19% were of 2 to 3 years, 35% were of 3 to 4 years, and 46% were of 4 to 5 years old.
Graph 1.
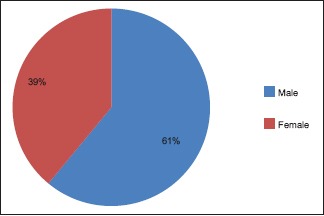
Distribution of children on the basis of gender
Graph 2.
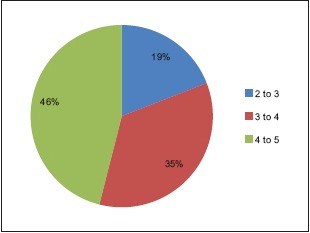
Distribution of study population on the basis of age (years)
In our study, the participants belong to a different socio-economic class: the maximum number of participants belong to lower/upper lower class and minimum belong to upper class [Graph 3].
Graph 3.
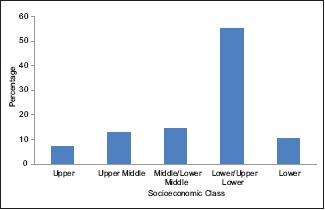
Distribution of study population on the basis of socioeconomic class
The MDAS was used for maternal anxiety assessment in the present study. Approximately, 39% belongs to fairly anxious, 34.8% to slightly anxious, 11.7% to not anxious, 10.7% to very anxious, and 3.7% to a phobic category of the anxiety scale [Graph 4]. The maximum participants belong to the fairly anxious category and minimum number belong to phobic category of the MDAS. Children's gingival health was assessed by using MGI. Clinical findings of children were directly proportional to MDAS. The MGI score was high in case of high MDAS values [Graph 5]. The mean MGI score was highest in phobic category of MDAS and lowest in the not anxious category. The MGI score increased on increment in maternal anxiety level and gingival well-being of child get decayed on increment in maternal dental anxiety level. Dental caries expanded in children in the event of high maternal dental anxiety. The caries experience of children with highly anxious mothers was fundamentally higher than those with less anxious and non-anxious mothers. The children whose mothers were “extremely anxious” (phobic) had the highest mean dmft [Table 1].
Graph 4.
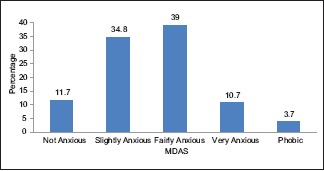
Distribution of study population according to Modified Dental Anxiety Scale (MDAS)
Graph 5.
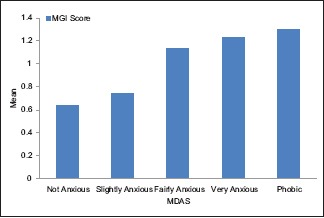
Comparison between Modified Dental Anxiety Scale (MDAS) and Modified Gingival Index Score (MGI)
Table 1.
Showing maternal anxiety level and their child’s caries experience
| MDAS | Mean±SD | |||
|---|---|---|---|---|
| Decayed teeth | Missing teeth | Filled teeth | Mean dmft | |
| Not Anxious | 0.53±0.24 | 0.30±0.21 | 0.83±0.17 | 1.66±0.62 |
| Slightly Anxious | 0.85±0.07 | 0.12±0.5 | 0.11±0.03 | 1.08±0.60 |
| Fairly Anxious | 0.93±0.35 | 0.25±0.09 | 0.24±0.05 | 1.42±0.49 |
| Very Anxious | 1.75±0.26 | 0.45±0.21 | 0.80±0.31 | 3.0±0.78 |
| Phobic | 2.00±0.75 | 0.73±0.36 | 0.84±0.47 | 3.57±1.58 |
| Total | 1.00±0.64 | 0.24±0.11 | 0.33±0.20 | 1.57±0.95 |
| P | 0.001 | 0.001 | 0.00 | 0.00 |
Discussion
Dental anxiety demonstrated a dynamic and clear effect on the oral health of individuals. Parent's dental fear influences the youngster's oral health result. Guardians with high-anxiety level maintain a strategic distance from dental treatment themselves and do not take their ward to the dental practitioner. Moms of low-financial class demonstrated high-tension level. These outcomes are like the investigations done by Kramer PF et al.[8] and Ardenghi TM et al.[9]
Studies were done by Khawja SG et al.,[10] Eitner S et al.,[11] and Pramila M et al.[12] had done comparative examinations and found a significant relationship between maternal anxiety and high caries involvement in their kids. These outcomes were like the discoveries of the present investigation. Milsom KM et al.,[13] in an investigation of five-year-old youngsters, found that dental tension in these kids was nearly connected with unpredictable dental visits, history of extraction, and having a dentally anxious parent. Maternal education level assumed an essential role in child's oral health. Mothers of high-education level were more concerned for their child's oral health. In a study done by Tyagi U et al.,[14] the maternal proficiency level is straightforwardly relative to the oral health status of their kids. In our study, 11.7% of mothers were not anxious and rest showed some level of dental anxiety. These results were similar to study done by Ain TS et al.[15] in which 13% were not anxious.
The mean dmft was highest in mothers with high dental anxiety level. These results were found similar in many previous studies.[11,16] However, Taani DQ et al.[16] showed no relationship between “general dental fear” and dental caries or gingival disease in youngsters. Dental caries demonstrated a strong association with parental factor and its similar discoveries of an investigation done by Menon I et al.[17]
Very few studies were done on the relationship between maternal dental anxiety and their child's gingival status. In the present investigation, the gingival status of the child declined in highly tensed mothers. These outcomes were similar to investigation done by Pramila M et al.[12]
To offer more humanized dental care, the prevalence of dental anxiety should not be overlooked in clinical practice, especially in pediatric dentistry. Strategies for the assessment, prevention, and control of dental anxiety should be implemented to allow better treatment for children, adolescents, and their parents. It is possible to conduct a simple, efficient evaluation of anxiety in the routine of a pediatric dental clinic with the use of validated tools. An adequate approach regarding children and adolescents with dental anxiety can assist in establishing a good dental experience and a trusting relationship between pediatric dentists, patients, and parents.[18]
A few constraints are additionally present in the investigation. The MDAS did not consider the past dental experience of the mothers. The sample size was small.
Maternal oral health was significantly associated with dental health of their children; not only did maternal dental anxiety influence oral health of mothers but also a concomitant factor in the development of children's dental anxiety. The education program on mothers’ oral health-related knowledge can be a target for improvement of the oral health of mothers and children.[19] Proper dental education and awareness programs must be organized by dental professionals to improve the oral health knowledge and awareness of mothers and to reduce their fear for dental treatments, so that their psychological factors do not affect their child's health.
Conclusion
Maternal dental anxiety was firmly identified with their child's oral health and dental caries encounter. Improvement in maternal factors such as education, income, etc., may improve the oral health of their children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. Basic Books. 2005 [Google Scholar]
- 2.Kvale G, Berg E, Raadal M. The ability of Corah's dental anxiety scale and Spielberger's state inventory to distinguish between fearful and regular Norwegian dental patients. Acta Odontol Scand. 1998;56:105–9. doi: 10.1080/00016359850136076. [DOI] [PubMed] [Google Scholar]
- 3.Fejerskov O. Changing paradigms in concepts on dental caries: Consequencesfor oral health care. Caries Res. 2004;38:182–91. doi: 10.1159/000077753. [DOI] [PubMed] [Google Scholar]
- 4.Niji R, Arita K, Abe Y, Lucas ME, Nishino M, Mitome M. Maternal ageat birth and other risk factors in early childhood caries. Pediatr Dent. 2010;32:493–8. [PubMed] [Google Scholar]
- 5.Wyne AH, Chohan AN, Al-Owaisi MM, Al-Ahmari MS. Oral hygiene and gingival health status of preschool children attending a university dental hospital. Pak Oral Dent J. 2003;23:35–8. [Google Scholar]
- 6.World Health Organisation. Oral Health Surveys, Basic Methods. 5th ed. Geneva: WHO; 2013. [Google Scholar]
- 7.Newton JT, Edwards JC. Psychometric properties of the modified dental anxiety scale: An independent replication. Community Dent Health. 2005;22:40–2. [PubMed] [Google Scholar]
- 8.Kramer PF, Ardenghi TM, Ferreira S, FischerLde A, Cardoso L, Feldens CA. Use of dental services by preschool children in Canela, Rio Grande do Sul State, Brazil. Cad Saude Publica. 2008;24:150–6. doi: 10.1590/s0102-311x2008000100015. [DOI] [PubMed] [Google Scholar]
- 9.Ardenghi TM, Vargas-Ferreira F, Piovesan C, Mendes FM. Age of first dental visit and predictors for oral healthcare utilisation in preschool children. Oral Health Prev Dent. 2012;10:17–27. [PubMed] [Google Scholar]
- 10.Khawja SG, Arora R, Shah AH, Wyne AH, Sharma A. Maternal dental anxiety and its effect on caries experience among children in Udaipur, India. J Clin Diagn Res. 2015;9:42–5. doi: 10.7860/JCDR/2015/13647.6103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eitner S, Wichmann M, Paulsen A, Holst S. Dental anxiety--an epidemiological study on its clinical correlation and effects on oral health. J Oral Rehabil. 2006;33:588–93. doi: 10.1111/j.1365-2842.2005.01589.x. [DOI] [PubMed] [Google Scholar]
- 12.Pramila M, Murthy AK, Chandrakala B, Ranganath S. Dental fear in children and its relation to dental caries and gingival condition - A cross sectional study in Bangalore city, India. Int J Clin Dent Sci. 2010;1:1–5. [Google Scholar]
- 13.Milsom KM, Tickle M, Humphris GM, Blinkhorn AS. The relationship between anxiety and dental treatment experience in 5-year-old children. Br Dent J. 2003;194:503–6. doi: 10.1038/sj.bdj.4810070. [DOI] [PubMed] [Google Scholar]
- 14.Tyagi U, Menon I, Tomar D, Singh A, Goyal J. Association between maternal oral health literacy and their preschoolers’ oral health outcomes in Muradnagar -a cross-sectional study. J Dent Specialities. 2017;5:98–101. [Google Scholar]
- 15.Ain TS, Sultan S, Gowhar O, Ravishankar TL. Maternal dental anxiety as a risk factor for dental caries in children: A cross-sectional study. Int J Res Med Sci. 2016;4:4867–72. [Google Scholar]
- 16.Taani DQ, El–QaderiSS, Abu Alhaija ES. Dental anxiety in children and its relationship to dental caries and gingival condition. Int J Dent Hyg. 2005;3:83–7. doi: 10.1111/j.1601-5037.2005.00127.x. [DOI] [PubMed] [Google Scholar]
- 17.Menon I, Nagarajappa R, Ramesh G, Tak M. Parental stress as a predictor of early childhood caries among preschool children in India. Int J Paediatr Dent. 2013;23:160–5. doi: 10.1111/j.1365-263X.2012.01238.x. [DOI] [PubMed] [Google Scholar]
- 18.Assuncão CM, Losso EM, Andreatini R, de Menezes JV. The relationshipbetweendental anxiety in children, adolescents and their parents at dentalenvironment. J Indian Soc Pedod Prev Dent. 2013;31:175–9. doi: 10.4103/0970-4388.117977. [DOI] [PubMed] [Google Scholar]
- 19.Olak J, Nguyen MS, Nguyen TT, Nguyen BBT, Saag M. The influence of mothers’oralhealth behavior and perception there of on the dental health of their children. EPMA J. 2018;9:187–93. doi: 10.1007/s13167-018-0134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


