Abstract
Background:
In India, gutkha is popular among all socioeconomic groups, since it is available easily and is of less cost. Various investigations have demonstrated the relationship of gutkha biting with periodontal status and oral hygiene.
Aim:
The aim of this study is to assess the effect of gutkha chewing on periodontal health and oral hygiene of patients attending the dental department in India.
Materials and Methods:
A cross-sectional investigation was directed among 200 patients going to dental camps. Among them, 100 were gutkha chewers and 100 were smokers. The oral hygiene status of selected patients was determined by using the Simplified Oral Hygiene Index. Various periodontal parameters like a gingival recession, clinical attachment loss, mobility, and furcation were used to evaluate the periodontal status. Data were collected and analyzed with the help of SPSS software version 20.
Result:
Among the 200 subjects, 102 were males and 78 were females. In 100 gutkha chewers, 67% were male and 33% were females. About 68% gutkha chewers showed poor oral hygiene as compared to nonchewers (41%). The values of all the periodontal parameters were significantly higher in gutkha smokers compared to nonchewers.
Conclusion:
Gutkha chewing has a strong effect on oral hygiene. The findings can contribute to the evidence of smokeless tobacco (gutkha) as a risk factor for periodontal disease.
Keywords: Clinical Attachment Loss, Gutkha, Oral Hygiene Index, Periodontal Status, Probing Pocket Depth, Smokeless Tobacco
Introduction
In India, tobacco utilization has been viewed as a noteworthy contributor to the aggregate death rate, and in 1990, 1.5% of aggregate deaths were tobacco related. Tobacco utilization is evolving at the rate of 2–3% per annum. World Health Organization (WHO) appraisal evaluated that by 2020, tobacco-related demise may surpass 1.5 million yearly or 13% of death in India. India is a developing nation and tobacco smoking is turning into the well-known type of tobacco utilization in rural and urban populace. Out of 930 million worldwide tobacco buyers, 1.1 billion smokers live in developing nations, in which India alone has 182 million smokers.[1]
The most well-known kind of smokeless tobacco consumed is gutkha. Gutkha, a sort of smoked tobacco (ST), comprises of tobacco, areca nut, and catechu combined with a few different fixings accepted to be exceedingly addictive, enhanced, and sweetened and has a high concentration of nicotine and other addictive. Thus falling prey to the double destructive impacts of areca nut and tobacco.[2] Smokeless tobacco is known to cause malignancies of the mouth, lip, tongue, and pancreas. Users likewise might be in danger for cancer of the voice box, throat, colon, and bladder, since they swallow a portion of the poisons in the juice made by utilizing smokeless tobacco.[3] Smokeless tobacco can trouble gum tissue, causing periodontal disease. Sugar is routinely added to update the sort of smokeless tobacco, growing the danger for tooth cavitation. Smokeless tobacco also routinely contains sand and coarseness, which can further harm the teeth.[4] Periodontal illnesses are one of the fundamental wellsprings of tooth loss, particularly among all the more elderly individuals. Tobacco smoking is a champion among the most fundamental characteristic peril factors for periodontal sicknesses. Enormous amount of studies have been led to comprehend the job of smoking in the etiology of periodontal diseases and the accessible information demonstrates that smoking is related with expanded pervasiveness and seriousness of periodontal ailment, which might be because of the unfavorable impacts of tobacco smoking on the physiology, immunology, and microbiology of the oral condition. Dissimilar to smoking, the job of oral smokeless tobacco (SLT) in the etiology of the periodontal ailment has gotten extensively less attention.[5]
Thus, the present investigation was conducted to assess the impact of chewing gutkha on oral hygiene and periodontal status.
Materials and Methods
An investigation was directed among 200 patients going to dental camps. Among them, 100 were gutkha chewers and 100 were smokers. The study was led for a half-year length. Before beginning, the investigation ethical clearance was acquired from the ethical advisory group of the doctor's facility. Composed assent from subjects was taken before their investment and clinical examination of the individuals in the investigation.
The population aged between 15–60 years; with at least 20 permanent teeth, utilizing smokeless tobacco for over a half year and at least two packets every day, and those with no history of any periodontal treatment for at least 6 months were incorporated into the investigation. Exclusion criteria enveloped the following: patients taking tobacco in any frame other than gutkha biting (smoking, snuff, the container with tobacco, and biting tobacco leaf), liquor utilization, fundamental infections, pregnant or lactating females, and patients utilizing any drug which influences the well-being of the periodontium.
Information will be collected by using a pretested questionnaire, which contains the information about the sociodemographic profile and oral cleanliness survey (aids use, frequency, and duration). The intraoral study was done to assess oral cleanliness, gingival bleeding, and periodontal status (probing depth, clinical attachment loss (CAL), recession, furcation involvement). The oral hygiene status of selected patients was determined using Simplified Oral Hygiene Index (OHI-S), introduced by Greene and Vermilion in 1964, which comprises the Simplified Debris Index and Simplified Calculus Index. Each of these indices is based on numerical determinations, representing the amount of debris or calculus on six preselected tooth surfaces.
Probing pocket depth (PPD) was measured by inserting calibrated UNC 15 probe parallel to the long axis of the tooth to measure the distance from the gingival margin to base of sulcus or pocket to the nearest millimeter, at four sites of a tooth, namely, mesiobuccal, buccal, distobuccal, and mid-lingual, around all teeth. Deepest pocket in millimeter was considered amongst all PPD measurements.
Gingival recession was scored as “present” if the gingival margin was located apical to cementoenamel junction (CEJ) at the buccal aspect of all the teeth. CAL was determined by calculating the distance from a fixed reference point, CEJ, to the base of pocket or sulcus. Mobility was scored using the following criteria: no mobility (score 0), slight mobility to touch (score 1), a mobility of 1–2 mm (score 2), and obvious looseness with mobility >2 mm (score 3). Furcation involvement was detected using Naber's probe and scored according to criteria modified from Loesche et al. as follows: no furcation involvement (score 0), slight indentation (score 1), pronounced indentation (score 2), through-and-through penetration but filled with soft tissue and might not be visible (score 3), through-and through-penetration and furcation was clinically visible (score 4).
The data obtained were compiled systematically, transformed from a precodedproforma to a computer, and a master table was prepared in Microsoft Excel SPSS software version 20. Chi-square test/Fisher exact test has been used. Statistically significant figure was set for the study when P < 0.05, 95% confidence interval.
Result
A total number of 100 gutkha chewers and 100 nonchewers participated in the study. Among the 200 subjects, 102 were males and 78 were females. In 100 gutkha chewers, 67% were male and 33% were females [Graph 1]. Mean age for gutkha chewers was 34.5 years and 30.3 years for nonchewers (range 25–60 years).
Graph 1.
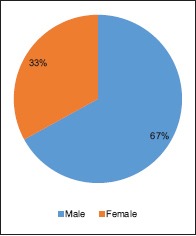
Distribution of gender among gutka chewers
Graphs 2 and 3 depict the oral hygiene practices among the study population. About 61% nongutkha chewers used a toothbrush with toothpaste and 42% gutkha chewers used finger with toothpaste for cleaning their oral cavity [Graph 2].
Graph 2.
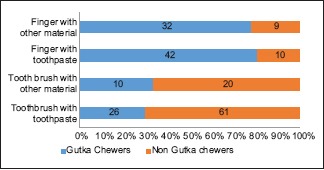
Distribution of material used for oral hygiene practices among study population
Graph 3.
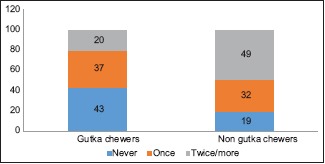
Distribution of Frequency of tooth brushing among the study population
About 68% subjects indicated poor oral cleanliness when contrasted with nonchewers (41%) [Table 1]. Various subjects with great oral cleanliness (32%) were altogether higher among nonchewers when contrasted with gutkha chewers where none of the subjects had great oral cleanliness. Greater part of gutkha chewers never brushes their teeth [Graph 3].
Table 1.
Distribution of oral hygiene status among the study population
| OHI-S | Gutkha chewers n=100 | Nongutkha chewers n=100 | |
|---|---|---|---|
| Good | 0 | 32 | Chi-square value 39.1118 |
| Fair | 32 | 27 | P<0.00001* |
| Poor | 68 | 41 |
*P<0.05 is significant
Table 2 depicts the periodontal status among the study population. Gingival recession was found to be more in gutkha chewers (62%) as compared to nongutkha chewers (25%). CAL was found with >5 mm of attachment loss to be 41% in gutkha chewers as compared to 21% in nongutkha chewers. About 1–2 mm attachment loss was more in nongutkha chewers, that is, 43% as compared to 27% in gutkha chewers.
Table 2.
Relationship of periodontal status among the study participation
| Parameters | Gutkha chewers n=100 | Nongutkha chewers n=100 | Chi-square value | P |
|---|---|---|---|---|
| Recession | ||||
| Present | 62 | 25 | 27.8507 | P<0.00001* |
| Absent | 38 | 75 | ||
| CAL | ||||
| 1-2 mm | 27 | 43 | 10.344 | P=0.005673* |
| 3-4 mm | 32 | 36 | ||
| >5 mm | 41 | 21 | ||
| Mobility | ||||
| 0 | 44 | 62 | 8.7098 | P=0.033408* |
| 1 | 25 | 23 | ||
| 2 | 21 | 10 | ||
| 3 | 10 | 5 | ||
| Furcation | ||||
| 0 | 2 | 65 | 90.0274 | P<0.00001* |
| 1 | 42 | 15 | ||
| 2 | 34 | 10 | ||
| 3 | 15 | 8 | ||
| 4 | 7 | 2 | ||
CAL: Clinical attachment loss. *P<0.05 is significant
Table 2 reveals that mobility and furcation involvement were significantly high in gutkha chewers as compare to nongutkha chewers. Mobility with score 2 was 21% in gutkha chewers as compare to 10% in nongutkha chewers. Mobility with score 3 was 10% in gutkha chewers and 5% in nongutkha chewers. Fraction with score 1 was 42% in gutkha chewers and 15% in nongutkha chewers.
Discussion
The connection between tobacco utilization and its malicious consequences for oral health is outstanding. The utilization of gutkha (smokeless tobacco) has found to relate with periodontitis and bone misfortune. The fundamental driver of periodontal disorders is poor oral cleanliness and tobacco utilization. Serious periodontal disease, which may result in tooth misfortune, was the 11th most predominant infection in 2016.[6]
Indian tobacco feature has seen an exponential move in the gutkha bargain during the time in all the socioeconomic level. This is a result of the convenience of usage, easy availability, and insignificant expense of gutkha packets.[7] The expansive promoting of gutkha has incited no matter how you look at its reliance among youthful age group, especially in low-income-related status people.[7]
In this study, it was discovered that lion's share of male chewers had a propensity for chewing gutkha pursued as compared with females. Finding was found in the study coordinated by Hazarey et al.,[8] Sinha et al.,[9] and Bala et al.[10] In our study, mean age was seen to be on more younger side. This resembles Kumar et al.,[11] in which significant smokeless tobacco users (60%) started having tobacco before 21 years of age.
The present study demonstrated that the nonchewers have better oral cleanliness contrasted with chewers. Comparable outcomes were found in the investigation by Parmar et al.[12] and Al-Kholani.[13] In their investigation, oral hygiene status essentially disintegrated in people having deleterious oral propensities contrasted with controls.
The gingival recession is significantly higher among gutkha chewers in our study. This was in affirmation with the investigation by Amarasena et al.[14] The relationship of smokeless tobacco (ST) and gingival recession may be expected to exacerbate incendiary reactions prompted by ST, which adds to quickened periodontal breakdown and gingival recession at the site of situation. Mechanical injury because of the rough idea of the ST being held in closeness to thin gingival tissues could likewise be contributory to subsidence.[15] The nicotine present in gutkha (smokeless tobacco) items has been accounted to actuate hyperemia in gingival veins and, furthermore, assumes a job in upgrading gingival retreat and clinical connection loss.[16]
Blood nicotine levels appearing due to gutkha biting are drastically higher than that appearing from cigarette smoking. Along these lines, the utilization of tobacco items may intensify periodontal disease. This clarifies the huge high score of versatility and furcation inclusion in ghutka chewers.[16] In an in-vitro study by Billman et al[17] and a study by Chang et al[18] stated that the areca nut containing arecoline restrain the development and connection of proteins and periodontal fibroblasts. This showed that gutkha that contains betel nut may be another hazard factor in the pathogenesis of periodontal diseases.[18]
Encourage broad investigations with bigger sample size will be expected to sum up the outcome with more grounded proof. The discoveries of this study will likewise assist us in deciding whether to do guidance or nicotine substitution treatment as a method of de-addiction administration.
Conclusion
The present study demonstrates a strong connection between gutkha smoking and periodontal status. In light of the outcomes, it was reasoned that gutkha sly affects the periodontium. Thus, gutkha is one of the essential hazard factors for the periodontal ailment. More dental health camps and programs should be directed in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vellappally S, Jacob V, Smejkalová J, Shriharsha P, Kumar V, Fiala Z. Tobacco habits and oral health status in selected Indian population. Cent Eur J Public Health. 2008;16:77–84. doi: 10.21101/cejph.a3448. [DOI] [PubMed] [Google Scholar]
- 2.Arun MS, Mythri S, Hegde S, Rajesh KS. Effect of chewing gutkha on oral hygiene, gingival and periodontal status. J Oral Health Res. 2012;3:26–31. [Google Scholar]
- 3.Shah RS, Cole JW. Smoking and stroke: The more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8:917–32. doi: 10.1586/erc.10.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaffee BW, Couch ET, Ryder MI. The tobacco-using periodontal patient: Role of the dental practitioner in tobacco cessation and periodontal disease management. Periodontol 2000. 2016;71:52–64. doi: 10.1111/prd.12120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ravishankar PL, Nadkerney P, Pramod V, Soni A, Jaiswal R, Kumar A, et al. Effect of Gudakhu (Smokeless Tobacco) on periodontal health: A case-control study. Int J Oral Care Res. 2017;5:1–4. [Google Scholar]
- 6.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1211–59. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukherjee K, Hadaye RS. Gutkha its determinants among secondary school male students. Indian J Community Med. 2006;31:177. [Google Scholar]
- 8.Hazarey VK, Erlewad DM, Mundhe KA, Ughade SN. Oral submucous fibrosis: Study of 1000 cases from central India. J Oral Pathol Med. 2007;36:12–7. doi: 10.1111/j.1600-0714.2006.00485.x. [DOI] [PubMed] [Google Scholar]
- 9.Sinha DN, Gupta PC, Pednekar MS. Tobacco use in a rural area of Bihar, India. Indian J Community Med. 2003;27:167–70. [Google Scholar]
- 10.Bala DV, Bodhiwala IN, Patel DD, Shah PM. Epidemiological determinants of tobacco use in Gujarat state, India. Indian J Comm Med. 2006;31:173–6. [Google Scholar]
- 11.Kumar S, Prabu D, Kulkarni S, Dagli RJ. Tobacco as risk factor for periodontal disease in green marble mine laborers of Rajasthan, India. Brazilian J Oral Sci. 2008;7:1641–7. [Google Scholar]
- 12.Parmar G, Sangwan P, Vashi P, Kulkarni P, Kumar S. Effect of chewing a mixture of areca nut and tobacco on periodontal tissues and oral hygiene status. J Oral Sci. 2008;50:57–62. doi: 10.2334/josnusd.50.57. [DOI] [PubMed] [Google Scholar]
- 13.Al-Kholani AI. Influence of khat chewing on periodontal tissues and oral hygiene status among Yemenis. Dent Res J (Isfahan) 2010;7:1–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Amarasena N, Ekanayaka AN, Herath L, Miyazaki H. Association between smoking, and gingival bleeding in rural Sri Lanka. J Clin Periodontol. 2003;30:403–8. doi: 10.1034/j.1600-051x.2003.20010.x. [DOI] [PubMed] [Google Scholar]
- 15.Mavropoulos A, Aars H, Brodin P. The acute effects of smokeless tobacco on gingival blood flow in man. J Periodontal Res. 2001;36:221–6. doi: 10.1034/j.1600-0765.2001.036004221.x. [DOI] [PubMed] [Google Scholar]
- 16.Vikneshan M, Ankola AV, Hiremath A, Hebbal M, Suganya M. Smokeless tobacco and its adverse effects on oral cavity- An overview. Ann Dent Specialty. 2014;2:64–9. [Google Scholar]
- 17.Billman MA, Caughman G, Lewis J, Snyder HB, Schuster G. Nicotine modulation of in vitro human gingival fibroblast beta 1 integrin expression. J Periodontol. 2002;73:505–10. doi: 10.1902/jop.2002.73.5.505. [DOI] [PubMed] [Google Scholar]
- 18.Chang YC, Lii CK, Tai KW, Chou MY. Adverse effects of arecoline and nicotine on human periodontal ligament fibroblasts in vitro . J Clin Periodontol. 2001;28:277–82. doi: 10.1034/j.1600-051x.2001.028003277.x. [DOI] [PubMed] [Google Scholar]


