Abstract
Background and Aim:
Postoperative urinary retention (POUR) is defined as a disability in urinary excision after surgery. There are several strategies to prevent POUR, such as tamsulosin, which is a selective antagonist at alpha-1A and alpha-1B-adrenoceptors which reduces the bladder outlet resistance. The aim of this study was to investigate the efficacy of prophylactic tamsulosin in preventing acute urinary retention and other obstructive urinary symptoms following colporrhaphy surgery.
Materials and Methods:
This study was a randomized, double-blind clinical trial. A total of 130 patients who were candidates for colporrhaphy were divided into two groups: the intervention group (65 subjects received 0.4 mg tamsulosin in a single dose at the time of sleeping) and the control group (65 subjects received placebo at the same time as the intervention group). The incidence of acute urinary retention and other obstructive urethral symptoms and the mean urination volume after catheterization were recorded 24 h after operation. Patients’ demographic and clinical data were analyzed using SPSS version 20 software using Chi-square and Fisher's tests.
Results:
There was a significant difference in the incidence of acute urinary retention, decrease in urine flow diameter, and the mean residual urine volume Post Void Residual (PVR) in the bladder, and the incidence of these symptoms decreased in the tamsulosin recipient group. The incidence of other symptoms of acute urinary retention was not significantly different when compared between both the groups.
Conclusion:
It seems that the use of prophylactic tamsulosin is more effective in decreasing the incidence of acute urinary retention, decreasing the PVR in the bladder, and decreasing the diameter of the urine flow in patients after colporrhaphy.
Keywords: Acute urinary retention, colporrhaphy, tamsulosin
Introduction
Colporrhaphy is a kind of aesthetic and restorative surgery in the birth canal that is performed following pelvic organ prolapse including rectocele and cystocele. Pelvic organs prolapse and its symptoms are common (about 50%).[1] The high prevalence requires a restorative surgery, where about 300,000 restorative surgeries have been reported annually in the United States.[2] Demographic studies have reported a prevalence of 11%–19% for reconstructive surgery of female pelvic floor prolapse over a lifetime.[3] Pelvic organ prolapse is associated with poor sexual satisfaction of couples, and colporrhaphy is recommended in women who suffer from distressing symptoms such as dyspareunia and sexual problems, where they do not respond to other supportive therapies.[4]
Ultimately, colporrhaphy surgery can improve sexual function.[5] One of the common complications associated with surgery of pelvic organ prolapse is an inadequate bladder discharge and acute urinary retention,[6] with an estimated rate of about 2.5%–43% reported.[7] Postoperative urinary retention (POUR) is defined as a disability in urinary excision after surgery.[2]
Urinary retention is defined to be the inability to pass urine following surgery. This disorder is present in both sexes and in all age groups, following urinary tract surgery and perineal and anorectal surgery.[8] The cause of POUR is not completely clear; however, the cause of this disorder appears to be multifactorial.[2] Ample evidence suggests that POUR is associated with some factors such as spinal anesthesia, age, the presence of obstructive urogenital disease, the type and duration of surgical procedures, and fluid and analgesia.[9]
According to studies, POUR imposes significant health and financial costs on patients,[10,11] which is associated with urinary tract infections in many cases, and also results in a need for catheterization of the bladder, obstructed urethra (urea), increased duration of admission to the hospital, and additional surgeries. Therefore, surgery is useful to reduce this complication. There are several strategies to prevent POUR, such as limitation of fluid intake during surgery, use of sympathomic and alpha-adrenergic blocking agents,[12] pain control,[13] sitz bath,[14] use of local anesthesia,[15] and early movement after surgery.[2] In this regard, alpha-adrenergic blockers have been used as a prophylaxis for POUR treatment, where favorable results have been obtained.[10] As previously indicated by Neimark et al. (2012), the use of tamsulosin (alpha-blocker) reduces the duration of urination in increasing the maximum urine flow rate and can improve the quality of life in patients by improving the urinary obstruction disorders.[16] Tamsulosin is a selective alpha-1 receptor blocker that reduces bladder output and thus reduces resistance to urine flow.[17] There are few studies on the use of tamsulosin in the prevention of acute urinary retention after surgery. The aim of this study was to evaluate the efficacy of tamsulosin prophylaxis in preventing acute urinary retention and other symptoms of urinary obstruction following colporrhaphy surgery, as well as to evaluate the efficacy of tamsulosin single dose, which may be used as a low-risk treatment.
Materials and Methods
This study was conducted as a randomized, double-blind clinical trial using placebo. The target population was female patients less than 60 years of age who were candidates for colporrhaphy surgery at Taleghani hospital in Arak, Iran. The data collection tool was a checklist (questionnaire). Placebo capsules similar to tamsulosin (in terms of shape, size, color, and other features) were provided by the hospital pharmacy staff, both of which were in the same container (in appearance), with codes A and B. Drug prescriptions were performed for all patients who satisfied the inclusion criteria, and the questionnaire was completed by the resident of hospital. In addition, the indication of surgery in patients was determined based on the conditions of the disease, the surgeon's opinion, and the conditions of each patient. The resident had completed the checklist for demographic and clinical data and also the task of assessing the incidence of urinary retention and other clinical variables. The resident evaluated the urinary retention rate and other clinical variables related to patients. Accordingly, the researcher, anesthesiologist, and patients were blind to the type of treatment. Convenience sampling was performed using inclusion and exclusion criteria.
Inclusion criteria:
-
1)
Patients 18–60 years of age
-
2)
Patients with colporrhaphy surgery indications
-
3)
Informed consent to participate in research
-
4)
No active urinary tract infection
-
5)
No history of neurological disorders
-
6)
Not having malignancy
-
7)
Not having urinary incontinence
-
8)
Lack of use of drugs affecting voiding function, such as cholinergic drugs
-
9)
Not having a history of urologic diseases such as urethral or bladder stricture
-
10)
No history of urinary stone or urinary tract obstruction
-
11)
No history of urological surgery
-
12)
No fixed urinary catheter
-
13)
Not having significant associated disorders, especially chronic renal disease and cardiopulmonary disorders
-
14)
No history of allergy for tamsulosin
-
15)
No history of treatment or recent use of tamsulosin for any cause.
Exclusion criteria:
-
1)
Failure to reach the patient for any reason during the first 24 h after surgery
-
2)
Patient dissatisfaction.
All patients had undergone a clinical examination and blood and urine analysis before surgery. Then, eligible patients were entered into the study based on clinical, laboratory, and exclusion and inclusion criteria.
After receiving the demographic data, the patients were randomly assigned (ratio 1:1) into two groups of intervention (65 subjects, administered 0.4 mg tamsulosin, one single dose, 12 nights after the operation during sleep) and control (65 subjects received placebo at similar times in the intervention group).
The surgery was performed by a surgeon for less than an hour. For all patients, Ringer's lactate (1.5 mL/kg/h) was prescribed in the operating room, before the anesthesia and after operation during the NPO period (nil per os) (4–6 h).
Anesthesia was performed after short-term spinal anesthesia (lidocaine 5%). For postoperative pain control, morphine and nonsteroidal anti-inflammatory drugs (NSAIDs) were used. Patients in the two groups were matched in terms of age, duration of operation, type of anesthesia, and NSAIDs. The age of patients less than 60 years was considered not to be biologically studied due to the higher prevalence of acute urinary retention in elderly people. It was considered to prevent bias from the high incidence of urinary retention in the elderly.
All patients were examined for 24 h after surgery (from the time of removal of the catheter) in terms of difficulty in urinating or the appearance of administrative retention. Urinary retention is defined based on the presence of palpable mass in the suprapubic region, discomfort and inability to urinate, a feeling of decreased urinary flow, a feeling of caliber reduction in the urine flow, a feeling of urine left in the bladder since the removal of the catheter, despite the intake of fluids, and when the conservative attempts for warming up the suprapubic region and encouraging patients to move for urination are unsuccessful and catheterization of the bladder is inevitable.
Bladder catheterization was performed using Foley catheter with xylocaine 2%. Finally, the incidence of acute urinary retention and other obstructive urethral symptoms based on the above definition and the mean of urinary volume discharged after postoperative catheterization were compared in patients with acute urinary retention as the main variables between the two groups.
Sample size
The sample size was based on α = 0.05 and generalizable ratio to population (=0.03); 65 patients were considered for each group (130 patients) using the following formula:
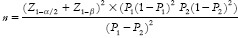
≈65 individual in each grops
→ overall: 300
Z1−α/2=1.96
Z1−β=2.33
P1= 0.25
P2= 0.03
Data analysis
Data obtained from the checklist and demographic and clinical data were analyzed using SPSS version 20 software based on Chi-square and Fisher's exact tests. Descriptive statistics were used for quantitative variables using central and distribution indices, and for qualitative variables using frequency and percentages. Inferential statistics were used for quantitative variables, and analysis of variance and post hoc tests or its nonparametric equivalents were applied. For qualitative variables, Chi-square test or Fisher's exact test was used.
Ethical considerations
The introduction letter was received from the university's staff for introducing patients to the research centers
The letter was received from the authorities of the selected researcher centers
The purpose of the study was explained to all research units, and written consent was obtained from participants.
The information of all patients was kept confidential by the presenter. The Declaration of Helsinki and ethics committees of Arak University of Medical Sciences were considered in this study.
This article is obtained from a dissertation with ethic code of IR.ARAK.MU.REC.381.
Results
In this study, 130 patients were enrolled in the study and divided into intervention and control groups. The mean ± standard deviation of patients’ age in the group receiving tamsulosin was 45.95 ± 7.55 years, and in the placebo group was 42.83 ± 8.84 years. Independent T-test revealed that this difference was not statistically significant between the two groups (P > 0.05) and it was shown that the two groups were similar in age [Table 1].
Table 1.
Mean and standard deviation of patients’ age in the two groups
| Group | No. | The least | The most | Mean | Standard deviation | t | P |
|---|---|---|---|---|---|---|---|
| Tamsulosin | 65 | 28 | 60 | 42/95 | 7/85 | 0/084 | 0/933 |
| Placebo | 65 | 27 | 57 | 42/83 | 8/84 |
The frequency of urinary retention in the group receiving tamsulosin was 78.5% and in the placebo group was 63.1%, where this difference was not found to be statistically significant (P = 0.054). Therefore, tamsulosin use has not had a positive effect on patients; 51 patients with tamsulosin use had no urinary retention, whereas this figure was reduced to 41 patients in the placebo group [Table 2].
Table 2.
Frequency of urinary retention in patients receiving tamsulosin and placebo
| Study group | Feeling the fever under the abdomen and inability to urinate | P | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. | % | No. | % | ||
| Tamsulosin | 14 | 21/5 | 51 | 78/5 | 0/054 |
| Placebo | 24 | 36/9 | 41 | 63/1 | |
| All participants | 38 | 29/2 | 92 | 70/8 | |
The feeling of remaining urine in the bladder was 76.9% higher in the tamsulosin group than the placebo group (63.1%). Chi-square test showed that this difference was not statistically significant between the two groups (P > 0.05) and indicates that the urine remaining in the bladder was not affected by tamsulosin. In other words, 50 patients did not feel the urine to remain in the bladder in the tamsulosin group, whereas the number decreased to 41 patients in the placebo group [Table 3].
Table 3.
The feeling of remaining urine in the bladder in the two groups receiving tamsulosin and placebo
| Study group | The feeling of remaining urine in the bladder | P | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. | % | No. | % | ||
| Tamsulosin | 15 | 23/1 | 50 | 76/9 | 0/085 |
| Placebo | 24 | 36/9 | 41 | 63/1 | |
| All participants | 39 | 30 | 91 | 70 | |
The decrease in urinary flow rate was 73.8% in patients receiving tamsulosin and 63.1% in the placebo group. Chi-square test showed that this difference was not statistically significant between the two groups (P = 0.05) indicating that tamsulosin has no effect on the reduction of urinary flow; 48 patients did not show a decrease in urinary flow rate for those taking tamsulosin, whereas there were 41 patients with this disorder in the placebo group [Table 4].
Table 4.
Comparison of the feeling of decreased urinary flow among patients receiving tamsulosin and placebo
| Study group | Feeling of decreased urine flow | P | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. | % | No. | % | ||
| Tamsulosin | 17 | 26/2 | 48 | 73/8 | 0/186 |
| Placebo | 24 | 36/9 | 41 | 63/1 | |
| All participants | 41 | 31/5 | 89 | 68/5 | |
Based on data presented in Table 5, the decrease in the diameter of the urine stream was determined to be 16.9% in patients receiving tamsulosin and 36.9% in the placebo group. Chi-square test depicted that this difference was statistically significant between the two groups (P < 0.05), indicating the acceptable effect of tamsulosin on the frequency of decreasing the diameter of the urine stream. In fact, 11 people exhibited a decrease in the diameter of the urine stream in those taking tamsulosin, whereas this was reported in 24 subjects in placebo users.
Table 5.
Comparison of the sensation of decreasing diameter of the urine stream in patients receiving tamsulosin and placebo
| Study group | Feeling reduced urine flow diameter | P | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. | % | No. | % | ||
| Tamsulosin | 11 | 16/9 | 54 | 83/1 | 0/010 |
| Placebo | 24 | 36/9 | 41 | 63/1 | |
| All participants | 35 | 26/9 | 95 | 73/1 | |
The frequency of acute urinary retention in patients receiving tamsulosin (20%) was lower than the placebo group (36.9%). Chi-square test revealed that this difference was statistically significant between the two groups (P < 0.05) and it indicates that the effect of tamsulosin on urinary retention is positive, leading to a decrease in urinary retention. In other words, among tamsulosin users, 13 have urinary retention, whereas 24 were in the placebo group [Table 6].
Table 6.
Frequency of acute urinary retention in patients receiving tamsulosin and placebo
| Study group | Acute urinary retention | P | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No. | % | No. | % | ||
| Tamsulosin | 13 | 20 | 52 | 80 | 0/044 |
| Placebo | 24 | 36/9 | 41 | 63/1 | |
| All participants | 37 | 28/5 | 93 | 71/5 | |
The mean residual urine volume in patients receiving tamsulosin was lower (58.61) than the placebo group (110.15). It is noteworthy that this difference was statistically significant between the two groups (P < 0.05) by Mann–Whitney U test, indicating that tamsulosin causes a further reduction in residual urine volume of bladder compared with placebo [Table 7].
Table 7.
Comparison of mean and standard deviation of residual urine volume in the two groups
| Variable | Group | Mean | Standard deviation | Average rating | Total rank | Middle | Mann–Whitney U | P |
|---|---|---|---|---|---|---|---|---|
| Volume of urine remaining in the bladder (cm3) | Tamsulosin | 58/61 | 122/2 | 59/86 | 3891 | 00/00 | 1746 | 0/032 |
| Placebo | 110/15 | 150 | 71/14 | 4624 | 00/00 |
Discussion
Colporrhaphy is the oldest surgical procedure for the treatment of pelvic organ prolapse.[18] Colporrhaphy results in edema and tenderness of the povococytic muscles, which may interfere with bladder function and excessive dilation of the bladder, resulting in acute urinary retention.[19] Urinary retention is a disorder in the urinary system, which means the inability to completely or partially empty the bladder, which causes specific physical and mental consequences for the individual. This complication is one of the main causes of prostatic hyperplasia in men. Other complications of urinary retention include infections, neurological problems, and constipation.[20] In acute urinary retention, bladder muscle and bladder sphincter are not released which makes directing the stream difficult, resulting in incomplete bladder emptying. Inserting a urinary catheter or installing a stent can temporarily help urinate.[21] For ultimate treatment, the cause of retention should first be identified and then the use of alpha-blockers such as tamsulosin can be an appropriate treatment.[22]
In this study, the efficacy of prophylactic tamsulosin in preventing the occurrence of acute urinary retention was studied, and 130 patients satisfying the inclusion criteria were included in the intervention and control groups.
In this study, there was no difference in age between the two groups of tamsulosin and placebo (P = 0.933). There was no significant difference in the sensation of urinary retention between the two groups of tamsulosin and placebo (P = 0.054), which can be due to low sample size.
In addition, no significant difference was found regarding residual urine in the bladder between the two groups (P = 0.085). However, a significant difference was found between the two groups in terms of decreasing the diameter of the urinary flow (P = 0.110). Furthermore, the decrease in the diameter of the urinary flow in the intervention group (16.9%) was significantly lower than the control group (36.9%). There was a significant difference in urinary retention between tamsulosin and placebo groups (P = 0.44), in which the incidence of urinary retention was significantly lower in the tamsulosin group (20%) when compared with the placebo group (36.9%). The mean volume of residual urine in the tamsulosin group was lower than the placebo group and there was a significant difference between the two groups (P = 0.032).
The findings of previous studies were consistent with the results of our study. For instance, Ghuman et al. examined the use of an alpha-1 adrenergic blocker to prevent urinary retention. They reported that the use of alpha-1 adrenergic blocker reduces the risk of postoperative urinary retention (P < 0.0001). The use of alpha-1 adrenergic blocker reduced the risk of POUR after spinal anesthesia,[23] which is consistent with the results of our study. In both studies, urinary retention in the intervention group was lower. Moreover, Ahmad et al., in 2014, conducted a study to investigate the effect of tamsulosin on prevention of urinary retention in anorectal surgeries. The results showed that 56 (17.9%) patients in the control group exhibited inability to pass urine and required catheterization and 8 (2.5%) in the case group needed catheterization following POUR, which was statistically significant (P < 0.0001). Patients in the case group received 0.4 mg of tamsulosin only 6 h preoperatively and 6–8 h postoperatively.[2] However, in our study, 0.4 mg of tamsulosin was administered in a single dose of 12 nights after surgery. The findings of the aforementioned study were consistent with our study.
A study by Mohammadi-Fallah and Tayyebi-Azarin 2012 was conducted to investigate the prophylactic effects of tamsulosin on the incidence of acute urinary retention in neurosurgical patients. Based on the results, 15% and 2.5% of the patients in the control and intervention groups suffered from urinary retention, respectively, where a significant difference was found (P = 0.04).
In addition, the results exhibited that the type of surgical technique, type of anesthesia, and duration of operation did not have a significant effect on the frequency of urinary retention.[10] In our study, despite the lack of use of tamsulosin before surgery, the results were consistent with the aforementioned study. According to the aforementioned study, male gender has been reported to be a risk factor for urinary retention (P = 0.023). Tamsulosin in general cannot be a good prophylactic drug for urinary retention after rectal cancer surgery.[24] Their study results were not in agreement with our study. In this study, not only urine volume but also the incidence of urinary retention and diarrhea in the thymus group were lower. It seems that the cause of this difference is due to the type of patients in the two groups.
Because Jang et al.'s study evaluated the efficacy of tamsulosin in preventing acute voiding difficulty after rectal cancer surgery where all patients were male, all of our patients were female and underwent colporrhaphy surgery. Therefore, our results were consistent with most of the studies in POUR and confirm the results of other studies.
Conclusion
It seems that the use of prophylactic tamsulosin is effective in reducing the incidence of urinary retention, reducing the residual volume of bladder, and decreasing the diameter of the urinary flow in patients after colporrhaphy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Thom DH, Ragins AI. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175:259. doi: 10.1016/S0022-5347(05)00039-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmad MM, Jeelani A, Thakur S, Waseem M, Nazir I. Preventive effect of tamsulosin on postoperative urinary retention in benign anorectal surgeries. Saudi Surg J. 2014;11:27–33. [Google Scholar]
- 3.Asante WM, Kulkarni A. Elective oophorectomy in the United States: Trends and in-hospital complications, 1998-2006. Obstet Gynecol. 2010;32:24–9. doi: 10.1097/AOG.0b013e3181f5ec9d. [DOI] [PubMed] [Google Scholar]
- 4.Jones KA. Trends in inpatient prolapse procedures in the United States, 1979-2006. Am J Obstet Gynecol. 2010;2:202–9. doi: 10.1016/j.ajog.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feldner PC, Martins SB, Castro RA, Sartori MG, Girão MJ. Sexual function after anterior vaginal wall prolapse surgery. Clinics (Sao Paulo) 2012;67:871–5. doi: 10.6061/clinics/2012(08)03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lemack GE. Pressure flow analysis may aid in identifying women with outflow obstruction. J Urol. 2000;163:1823–8. [PubMed] [Google Scholar]
- 7.Buchkobl RL. An evidence-based approach to decrease early postoperative urinary retention following urogynecologic surgery. Urol Nurs. 2012;32:260–4. [PubMed] [Google Scholar]
- 8.Asante WM, Kulkarni A. Elective oophorectomy in the United States: Trends and in-hospital complications. Obstet Gynecol. 2006;11:108–11. doi: 10.1097/AOG.0b013e3181f5ec9d. [DOI] [PubMed] [Google Scholar]
- 9.Klutke SS, Carlin B, Paszkiewicz E, Kirkemo A, Klutke J. Urinary retention after tension-free vaginal tape procedure: Incidence and treatment. Urology. 2001;58:697–701. doi: 10.1016/s0090-4295(01)01366-8. [DOI] [PubMed] [Google Scholar]
- 10.Mohammadi-Fallah HS, Tayyebi-Azar A. Preventive effect of tamsulosin on postoperative urinary retention. Korean J Urol. 2012;53:419–23. doi: 10.4111/kju.2012.53.6.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holte SN, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth. 2002;8:622–32. doi: 10.1093/bja/aef220. [DOI] [PubMed] [Google Scholar]
- 12.Mason SA, Mayer E, Purkayastha S. Patient-related risk factors for urinary retention following ambulatory general surgery: A systematic review and meta-analysis. Am J Surg. 2016;211:1126–34. doi: 10.1016/j.amjsurg.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Winacoo MJ. Operative anesthesia and pain control. Clin Colon Rectal Surg. 2009;22:41–6. doi: 10.1055/s-0029-1202885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pidoj G. Effects of warm water sitz bath on symptoms in post-anal sphincterotomy in chronic anal fissure – A randomized and controlled study. World J Surg. 2007;3:1480–4. doi: 10.1007/s00268-007-9096-1. [DOI] [PubMed] [Google Scholar]
- 15.Gudaityte MI, Pavalkis D. Anesthesia for ambulatory anorectal surgery. Medicina (Kaunas) 2004;40:101–11. [PubMed] [Google Scholar]
- 16.Neimark RM, Kondrat’eva IS, Muzalevskaia NI. Urologiia. Correction of urodynamic disorders in women with obstructive urination. Russian. 2012;5:34–7. [PubMed] [Google Scholar]
- 17.Jang KS, Lee SM, Park JS, Kim DW, Ahn S. Randomized controlled trial of tamsulosin for prevention of acute voiding difficulty after rectal cancer surgery. World J Surg. 2012;36:2730–7. doi: 10.1007/s00268-012-1712-z. [DOI] [PubMed] [Google Scholar]
- 18.Berek JS. 13th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. Novak's Gynecology; pp. 19pp. 685–92. [Google Scholar]
- 19.Pant PR. An effective short duration postoperative catheterization after vaginal hysterectomy and pelvic floor repair. J Institute Med. 2006;28:33–5. [Google Scholar]
- 20.Hakvoort RA, Dijkgraaf MG, Burger MP, Emanuel MH. Predicting short-term urinary retention after vaginal prolapse surgery. Neurourol Urodyn. 2009;28:225–8. doi: 10.1002/nau.20636. [DOI] [PubMed] [Google Scholar]
- 21.Glavind K, Morup L, Madsen H, Glavind J. A prospective, randomized, controlled trial comparing 3 hour and 24 hour postoperative removal of bladder catheter and vaginal pack following vaginal prolapse surgery. Acta Obstet Gynecol Scand. 2007;86:1122–5. doi: 10.1080/00016340701505317. [DOI] [PubMed] [Google Scholar]
- 22.Sekhavat L, Farajkhoda T, Davar R. The effect of early removal of indwelling urinary catheter on postperative urinary complications in anterior colporrhaphy surgery. Aust N J Obstet Gynecol. 2008;48:348–52. doi: 10.1111/j.1479-828X.2008.00842.x. [DOI] [PubMed] [Google Scholar]
- 23.Ghuman A, Jonge S, Simion D, Feeney T. Prophylactic use of alpha-1 adrenergic blocking agents for prevention of postoperative urinary retention: A review & meta-analysis of randomized clinical trials. Am J Surg. 2018;215:973–9. doi: 10.1016/j.amjsurg.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 24.Jang JH, Lee SM, Park JS, Kim DW, Ahn S. Randomized controlled trial of tamsulosin for prevention of acute voiding difficulty after rectal cancer surgery. World J Surg. 2012;36:2730–7. doi: 10.1007/s00268-012-1712-z. [DOI] [PubMed] [Google Scholar]


