Abstract
Objectives/Hypothesis
Reduction of vocal effort is a therapeutic goal in resonant voice therapy and the treatment of a variety of voice disorders. The Borg CR10 is a perceived effort scale that is widely accepted across a wide variety of disciplines. The purpose of the present study was to examine 1) the utility of an anchored, adapted Borg CR10 in observing treatment-related vocal effort reduction 2) the convergent validity of the Borg CR10 in its relation to VHI item 14.
Study Design
Pretest-Posttest Experimental Design.
Methods
36 individuals with phonotraumatic hyperfunctional voice disorders completed the VHI item 14 and Borg CR10 at the start and completion of 4 sessions of resonant voice therapy treatment.
Results
Borg CR10 scores significantly differentiated pre- from post-therapy perceived effort levels. Convergent validity was demonstrated through significant associations with VHI item 14 scores.
Conclusion
The anchored Borg CR10 is an easy-to-use clinical tool to capture treatment-related vocal effort reduction. Whereas VHI item 14 indicates how frequently increased perceived effort is experienced, the Borg CR 10 captures the severity of perceived effort used. Thus, the two measures complement each other
Keywords: voice therapy, voice disorders, vocal effort, Borg CR 10, Voice outcome measurement
INTRODUCTION
One of the common and characteristic symptoms of a voice disorder is the patient’s perception of increased effort or strain in voicing1 otherwise known as perceived phonatory effort or exertion2,3. Numerous medical conditions can theoretically contribute to the need to increase exertion in the phonatory system. Vocal fold edema or mass lesions require increased respiratory drive, as does glottal incompetence associated with unilateral vocal fold paralysis4–7 These can therefore translate into the patient’s perception of increased effort. Increased vocal effort or strain can also be behavioral in nature and potentially result in trauma as a result of excessive adductory collisions forces observed in some behaviorally acquired voice disorders termed “adducted hyperfunction7” or synonymously, “phonotraumatic hyperfunction.8” Because of this, the reduction of vocal effort is often targeted through behavioral voice therapy.9–13 Unfortunately, physiological measurement such as phonation threshold pressure or visual observation of the vocal folds do not comprehensively capture this common complaint and attempts to measure patients’ perception of vocal effort have remained incomplete2,3. Thus, a meaningful measurement tool of perceived vocal effort has not been established for clinical use.
One measure of vocal effort that has been investigated for clinical utility is the Borg CR1014–15. Given that the Borg CR10 scale has effectively tracked vocal effort in past research protocols3,16–18, it may be a promising tool to employ clinically. Additionally, this scale is of interest because of its extensive and successful measurement of perceived exertion or effort in the kinesiology, medical, and ergonomic fields19–26. Particular strengths include its usability for the lay person, its response format, and its construction as a numeric ratio with standard intervals and true zero point3, as well as categorical verbal descriptors of each numeric point (e.g. “light” “moderate” “heavy” exertion).
The Borg CR10 also proved promising in differentiating a voice disordered population from a healthy population in an investigation of its clinical utility completed by Baldner et al (2015)3. Voice-disordered individuals rated their vocal effort level higher than vocally healthy individuals for a variety of quiet and normal-loudness vocal tasks. In conversation, the average score for perceived effort was in voice disordered participants was 1.48 (SD 1.81) (SD = .95), whereas it was 1.41 (SD=.95) for healthy controls. However, this difference was not statistically significant. Because the voice-disordered participants in this study were known to have significantly elevated vocal effort (i.e. strain, phonotraumatic voice use, complaint of effortful voice production) compared to vocally-healthy participants, the study represented a “known groups27 validity test” of the Borg CR10. A valid measure of vocal effort should be able to detect known group differences. The authors considered that the instrument’s verbal descriptors ranging from “very, very light” effort to “maximal” effort may not have been meaningful without links to concrete tasks such as quiet confidential conversation versus yelling over noise at a ballgame. The authors suggested that more investigation into varying the elicitation tasks, anchoring the responses, and standardizing the instructions could improve the clinical utility of the Borg CR10. Therefore, a study involving clinical application of the Borg CR10 should involve methods (i.e., elicitation tasks, anchors, and instruction) that improve the ability to detect known differences.
In the present study, we investigate the Borg CR10’s potential as outcome measure of perceived vocal effort in voice therapy. The instrument’s validity is examined by 1) testing its ability to detect known pre and post-therapy vocal effort differences and 2) quantifying its association with another measure of perceived vocal effort: Voice Handicap Index28 item 14 (“I feel as though I have to strain to produce voice.”). The former approach can be considered a variation on known-groups validity testing, while the latter exemplifies convergent validity 27 testing. Given the aim to examine the Borg CR10’s appropriateness as outcome measure, the investigation is entirely in the context of voice treatment and the within-group differences that represent progress in therapy.
The study population, and the implementation of resonant voice therapy, are particularly appropriate to the aim because phonotraumatic voice production is characterized by increased vocal effort7 2) resonant voice therapy directly reduces hyperfunctional adduction and associated perceived vocal effort 29,30 and 3) post-therapy improvement signifies at least in part, a reduction in vocal effort.29,31,32 Data were collected as part of a larger treatment-research study of patient adherence (i.e. compliance), such that extensive outcome measures documented pre and post therapy differences.33
Convergent validity testing was possible through participants’ completion of the Voice Handicap Index item 14: “I feel as though I have to strain to produce voice.” As both this item and the Borg CR10 assess perceived vocal effort, the two measures should yield a significant statistical association. However, because VHI item 14 asks users to rate the frequency of effortful voice use, whereas the Borg CR10 measures the severity of effort, the association is unlikely to be perfect.
In the present study, implementation of the Borg CR10 scale differs from its use in the previous two studies by incorporating experiential anchoring to clarify scale endpoints. The ecological validity of effort scales can be improved by using experiential anchoring of the scale endpoints: zero effort and maximal effort.34 Specifically, experiential anchoring methods can include exercise and memory anchoring34. When employing exercise anchoring, the user completes a given exercise that is indicative of the end-point effort level on the scale, thus experientially anchoring that point. In the present study, the 0 end point (i.e. no perceived vocal effort) was anchored with the exercise of effortless resonant voice production. To anchor the maximum scale endpoint (10) we used memory rather than exercises anchoring in order to avoid phonotrauma that could be associated with maximal vocal effort production. Memory anchoring is achieved by asking the user to recall a specific effort level experienced in the past, then tying this experience to an endpoint. Recollection of attempting to talk during severe laryngitis was used to anchor the maximal effort endpoint of “10.”
Purpose of the Study
The purpose of this study was twofold: 1) to examine whether an experientially-anchored Borg CR10 scale values could detect treatment-related changes in patient-perceived vocal effort We hypothesized Borg CR10 scores would be significantly higher at the start of treatment than at the completion of 4 sessions2) to examine convergent validity of the Borg CR-10 by quantifying the relationship between the Borg CR-10 and an easily recognized clinical effort rating: VHI item 14 (“I feel as though I have to strain to produce voice”). We hypothesized that the two instruments would be significantly, but not perfectly, associated both pre and post therapy.
To accomplish these goals, we examined pre- and post-therapy Borg CR10 and VHI item 14 scores in a clinical population of individuals with phonotraumatic hyperfunction who had successfully completed 4 sessions of voice therapy with significant improvements on traditional outcome measures. Pre- and post- therapy data collection included completion of the Borg CR10 and the VHI, yielding the data set analyzed in the present study.
METHODS
Participants
Thirty six adults ages 21–64 participated in a larger IRB-approved treatment study at the University of Wisconsin Voice and Swallow Clinic24. The group included twenty-six women ages 21–62 (M=40.08, SD=13.43) and ten men ages 21 to 64 years of age (M=45.3, SD=14.59). Vocal fold status and vocal function were determined via team approach evaluation by the providing speech-language pathologist and laryngologist. A complete patient demographics and vocal fold pathologies for 35 of the participants can be found in van Leer & Connor, 201535. All participants presented with visual confirmation of increase medial compression on stroboscopy. Additionally, participants demonstrated initial success in diagnostic therapy probes for resonant voice therapy. In all cases treatment was rated as successful to some degree, as indicated by significant improvement in outcome measures including significant reduction in VHI scores and CAPE-V ratings, significant increase in self-reported use of resonant voice, and significant increase in self-efficacy for resonant voice production.
Treatment
As part of a larger study on therapy compliance, participants received four hour-long treatment sessions of resonant voice therapy each spaced 1 week apart. Although some participants continued to receive therapy service after the study completion, pre-and post-therapy measures were taken before and after four sessions to maximize the consistency of the temporal course of therapy. In this manuscript, the term “post therapy” is used to denote “after 4 sessions of therapy.” The therapy protocol was based on Lessac-Madsen Resonant Voice Therapy30,31,36 (LMRVT) and provided by clinicians who had completed an LMRVT workshop by Dr. Verdolini. The aim of this program is to develop “resonant” voice, defined as voice production associated with patient-perceived lack of effort at the laryngeal level (“ease”) and a sensation of vibration in the oral cavity30,36; resonant voice production is associated with reduce laryngeal adduction29.
Measures
The VHI and Borg CR10 were administered at the first and fourth (i.e. final) therapy session associated with the study. Participants were asked to rate their habitual vocal effort by referring to their “typical voice use in the past week” to complete both scales.
VHI
The Voice Handicap Scale is a 30-item self-report measure that represents the patient’s perspective of the voice disorder and its handicapping effects. The VHI employs a 5-point ordinal response format ranging from 0 (never) to 4 (always) to rate the frequency of occurrence of each scale item. For the present study, only item 14 was analyzed: “I feel as though I have to strain to produce voice.”
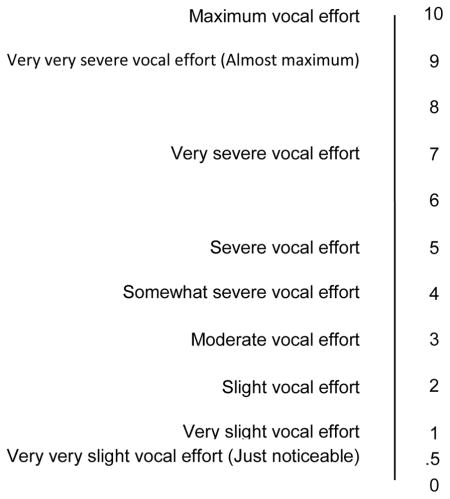
Borg CR10
The Borg CR1013 is a category-ratio scale that asks the user to rate their perception of physical effort or exertion in relation to a task. As noted in the appendix, the scale was adapted to refer to “vocal effort” in voice production rather than “exertion.” The scale, provided in appendix A, employs a response format that ranges from a value of 0 to 10, including both 0 and 10, for a total of 11 points. In addition, decimals (e.g. .5) are permitted although only the “.5” decimal point is printed on the scale. The numeric points are anchored by (categorical) verbal expressions including, for example, “very, very slight effort” commensurate with a numeric score of .5, severe vocal effort for a score of 5. Given the nature and instructions for the Borg CR10 rating there was no concern of learning effects as a result of the multiple presentations of either of these scales.
Procedure
VHI Completion
The VHI, a paper and pencil administered self-report questionnaire, was administered either at the start or end of session 1 and at the completion of session 4. Clarification of items was provided at the participants’ requests as needed.
Borg CR10 Completion
The Borg CR10 was completed at the end of session one so that the participant could refer to the preceding voice therapy session as an exercise anchor, and again at the end of session four. Patients were provided with two experiential anchors to operationalize the endpoints of the scale. To anchor the zero point on the scale, the investigator and patient discussed occasions in the immediately preceding therapy session in which effortless voice production was elicited, such as on humming or production of voiced fricatives. As such, zero effort was described to the patient as “The absence of vocal effort you felt here (pointing to the larynx) when you practiced that (i.e. the resonant voice strategy) with your therapist.” If the patient was unsure of this experience, easy resonant voice production was re-established with the investigator through resonant voice approaches. Thus, anchoring of zero effort exemplified exercise anchoring. Also, to prevent confusion with cognitive effort to produce resonant voice, the participant was told to “think only of vocal effort (clinician pointing to the larynx), not the mental effort or concentration it took to produce effortless voice” in reference to the zero point.
A value of “10” was described to the patient as “the amount of vocal effort or strain your feel here (pointing to the larynx) when you have laryngitis and can barely get sound out, even with a lot of strain.” All patients verbalized that they had experienced this level of effort in their life. This approach exemplified a memory-based experiential anchor. With these anchors, patients were asked to rate their habitual vocal effort level or “typical voice use in the past week” on the Borg CR10 by circling a value on the form or adding a .5 increment (e.g. a score of 4.5 instead of 4).
Statistical analysis
Purpose 1
To determine treatment-related effort reduction could be observed with the Borg CR10, the Matched-Pair Wilcoxon Signed Rank was performed for both Borg CR10 and VHI item 14 to calculate significance of treatment-related score reductions. This test was chosen over a repeated-measures t-test because VHI scores were ordinal. The same procedure was followed for VHI item 14 as a reference.
Purpose 2
Goodman and Kruskal’s Gamma was calculated to quantify the association between Borg CR10 and VHI item 14 scores for both pre- and post- therapy ratings. This non-parametric ordinal measure of correlation was chosen to accommodate the categorical response format of the Voice Handicap Index.
RESULTS
Purpose 1: did the Borg CR10 capture treatment-related change?
The Borg CR10 and the VHI item 14 both captured treatment related changes. The Wilcoxon Signed-Rank Test indicated that Borg CR10 scores at session 1 were significantly higher (M= 4.69, SD=1.57, range 2–8) than at session 4 (M=1.99, SD=1.23, range 0–5) of therapy, Z=−5.57, p< .001. Likewise, VHI item 14 scores reduced significantly from session 1 (M=2.28, SD=1.1, range 0–4) to session 4 (M=1.11, SD =.89, range 0–3) of therapy: the sign test shows Z=−4.118, p<001.
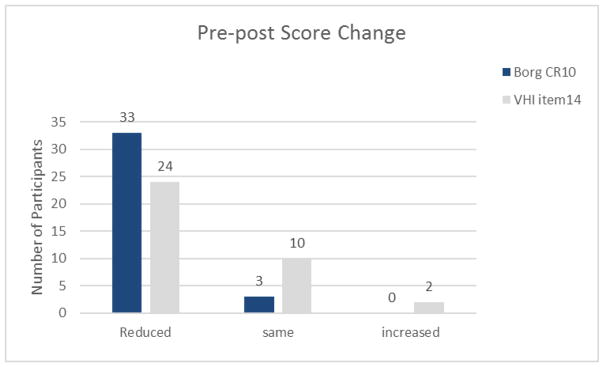
Although significant mean score reductions were found for both measures, not all participants reported a reduction in vocal effort. Score reduction was observed for 33 (92%) of participants on the Borg CR10, with the remaining 3 participants reporting no change in effort on this measure. Alternatively, 24 (67%) of participants rated the frequency of effortful voice use as reduced on VHI item 14, with 10 (27%) of 12 participants reporting no change, and 2(5%) indicating an increase.
Eleven participants scored change differently by instrument. Specifically, nine participants rated their pre to post-therapy vocal effort as reduced in severity on the Borg CR10 but unchanged in frequency of strained voice use on VHI item 14. Two individuals rated frequency of strained voice use as elevated at the end of therapy on VHI item 14, but unchanged in the severity of effort on the Borg CR10 (see Figure 1).
Figure 1.
The number of participants who rated their vocal effort as reduced, unchanged (same), and increased from pre- to post-therapy.
Purpose 2
There was a weak but significant correlation between pre-therapy Borg CR10 and VHI item 14 scores; Gamma=.345, Asymptotic Standard Error (ASE)=.154, p=.037. For both measures post-therapy, this correlation was moderate; Gamma= .686, ASE=.082, p=.001.
DISCUSSION
The overarching purpose of this study was to assess the clinical utility of the experientially anchored Borg CR10 as a vocal effort scale. To this end, vocal effort was assessed with both the Borg CR10 and VHI item 14 at treatment onset and completion of 4 resonant voice therapy sessions in 36 patients who presented with behaviorally acquired phono-traumatic voice disorders. There were two major findings commensurate to the study purposes. First, as hypothesized, Borg CR10 scores significantly reduced with treatment, as were VHI item 14 scores. Second, significant associations were found between Borg CR10 and VHI item 14 scores both pre- and post-therapy, supporting concurrent validity of the Borg CR10 as a measure of vocal effort.
Vocal effort reduction is of principal importance in the treatment of many behaviorally acquired voice disorders. In our study, individuals with phonotraumatic hyperfunction who had made significant outcome gains in 4 sessions of resonant voice therapy, were found to have significant pre- to post therapy vocal effort reductions on both the Borg CR10 and VHI item 14. This finding supports the scale’s construct validity in observing a known treatment-related improvement in this defining characteristic of vocal hyperfunction.
In relation to previous literature, it is interesting to note that significant within-group differences in Borg CR10 scores were observed in the present study, whereas (between-) group differences were not significant in the Baldner et al study. This is thought due to a measurement limitation of the undefined anchors in the scale employed in this prior study, rather than an absence of actual vocal effort differences between normal and disordered voices. Because voice-disordered participants in both studies had grossly similar outcome measure scores. When we examine a closely related reference experiences- “habitual” voice use in the present study, and the “conversation” task of the Baldner et al study, voice-disordered patients in the Baldner et al study rated their effort level over 3 points lower (M=1.48, SD=1.81) than our untreated voice-disordered participants (M=4.69, SD=1.57), while Baldner et al’s vocally healthy participants rated their vocal effort (M=1.41, SD= ) similar to our participants after treatment (M=1.99, SD 1.23). Thus, it is plausible that that the voice-disordered participants did not utilize the full range of the scale in rating their experience because of poorly defined anchors, thus yielding lower mean scores.
The method of experiential anchoring most likely explains this difference between studies. Experiential anchoring appears to have improved participants’ ability to scale their perceived vocal effort, and thus allow differences in effort level to be captured. This suggests that participants in the prior study used only a limited range of the scale. The zero effort level that was anchored via resonant voice probes (i.e. an exercise anchor) provided a benchmark against which our patients could judge their own habitually elevated typical vocal effort. Additionally, the memory anchor of laryngitis-related maximum vocal effort was familiar to all participants, thus anchoring the 10 value. Taken together, experiential anchoring likely improved ecological validity of the scale and thus, ability to detect known differences. Therefore, with use of experiential anchoring, the Borg CR10 may hold potential as clinical outcome measure.
In addition to experiential anchors, elicitation task may have affected participants’ Borg CR10 ratings. In the present research, reference to “your typical voice use in the past week” was chosen because it was identical to the vocal reference point employed by the Voice Handicap Index, and not for experimental reasons. In the previous research participants were asked to rate their vocal effort in reference to vowel production, sentence reading, conversation, and PTP tasks with normal pitch and loudness levels. A week’s typical voice use may have provided more opportunities for effortful voice, for example, in recalling speaking over noise during the week. However, such retrospective ratings are not typical effort scaling and would expose the rater to memory bias that would degrade the ratings. However, future research is needed to investigate elicitation techniques and anchoring approaches.
Compared to VHI item 14, the Borg CR10 offers unique information. While both the Borg CR10 and VHI item 14 provide an indicator of perceived vocal effort, the two instruments capture different aspects of vocal effort use. Where the Borg CR10 scale asks individuals to rate the severity of their vocal effort for habitual typical voice use, VHI item 14 captured the frequency at which increased effort is used (e.g. sometimes, always). It is therefore not surprising that almost a third of participants (n=11) demonstrated different pre-post therapy trajectories on these measures. When participants reported an improvement on the Borg CR10 but no difference on VHI item 14, frequency of strained voice use may have, for example, remained “often,” but the severity of effort involved was reduced from, for example, moderate to only light effort. VHI item 14 scores in isolation would suggest that the patient has not made any improvements. Therefore, the two measures complement each other. For the purpose of capturing outcomes, the Borg CR10 may be more useful in documenting fine treatment-related change in voice production technique, whereas VHI item14 might be more adept at measuring the functional result of those treatment changes.
A substantially greater number of participants (33 as opposed to 24) reported a reduction of vocal effort on the Borg CR10 scale compared to VHI item 14. These difference may not only be due to the different aspects of effort measured by each instrument, but also by their response format. The finer response format and greater range of (0–10 and decimal points) of the Borg CR10 may have allowed this instrument to detect effort changes that could not be identified on the VHI’s categorical 5-point response format of the VHI (0–4). Indeed, participants used a larger range of scores in completing the Borg CR10 (a range of 6 points pre-therapy, and 5 points post-therapy, respectively), than on the VHI, for which the majority of participants used only a range of 3 scores both pre- and post-therapy. Fine changes in frequency of effortful voice use are not reportable on the VHI, making it difficult to move from one value to another (e.g. from “often” to “sometimes”. For example, a notable change of 2.5 points on the Borg CR10 (from a score of 3.5 to 1) could reflect no change and remain within one category on the VHI (e.g. a score of 3 or “sometimes”). Therefore, the Borg CR10 may hold clinical utility for therapeutically discussing and developing awareness of vocal effort during the course of therapy, which might be helpful in training them to identify vocal changes earlier in the course of the day.
As hypothesized for the second study purpose, there was indeed a significant association between the Borg CR10 and VHI item 14. Concurrent validity of the Borg CR10 as measure of vocal effort is supported by its significant association with another effort measure: VHI item 14. Although significant, the relationship between the two measures was weak at treatment onset, and moderate at study completion. The weaker association noted at treatment onset could be related to the fact that not all patients had experienced the first session of voice therapy when they completed the initial VHI. Thus, without knowledge of effortless voice acquired in session 1 (necessary to anchor the Borg CR10), some individuals may not have scaled their VHI as accurately. The anchoring procedure, then, may be useful as a validity tool for both completion of the Borg CR10 as well as the VHI.
Furthermore, initial association between measures may have been sub-optimal because of patients’ limited experience in understanding and estimating their vocal effort at that time. In the resonant voice therapy provided to these patients, awareness, monitoring and eliminating vocal effort are core elements of therapy. Thus, patients learn to identify and reduce vocal effort over the course of treatment. They are therefore likely to have had greater accuracy in estimating their vocal effort by completion of the study. In fact, several participants verbalized at study completion that their initial Borg CR10 scores had been “too low.” In retrospect, these patients realized that their initial vocal effort was higher than they were aware of at that time.33 Both VHI item 14 and Borg CR10 effort ratings may have been more accurate at study completion, yielding a stronger association between the two measures at that time. Greater awareness of effort may also explain why many participants rated their effort as unchanged on either measure, or even increased in frequency. Future studies may focus on changes in perception of initial effort as greater vocal awareness and skill are achieved over the course of treatment.
Limitation and Future Directions
This study was limited in evaluating self-perceived effort alone, without utilizing physiological measures of effort such as Phonation Threshold Pressure. Furthermore, additional testing is required for validation of the Borg CR10. For example, given the use of anchors in the present study, a future study may seek to differentiate vocally normal from voice disordered populations. In addition, our current study was limited to individuals with phonotraumatic, adducted hyperfunction. The results cannot necessarily be generalized to other voice disorders, in particular if these are not characterized by elevated vocal effort. These require dedicated study.
Future directions may also explore the effect of anchoring. In the present study, we used a memory-based anchor (“talking through laryngitis”) to indicate the upper scale limit. Given that individuals’ experiences with laryngitis may have varied from, for example, moderate vocal effort with some dysphonia, to complete voice loss and severe vocal effort- the “memory anchor” approach may cause inherent variability across patients, making it difficult to compare individuals. One of the important aspects of the category portion of the Borg CR10 scale is the attempt to standardize levels within the scale to improve comparisons between individuals. This feature would enable the Borg CR10 to accurately compare levels of effort across patient populations, which could assist differential diagnostics. Future studies might employ an exercise anchor for both the zero and the maximum point, and could even consider a mid-level anchor to improve scale validity and reliability across patients. However, development of an exercise anchor for the maximum point would need to consider the risk of phonotrauma such as vocal fold hemorrhaging, in particular in a voice-disordered population. Despite this concern, other exercise domains have achieved maximum effort anchors without undue damage to the systems of study. These concerns will require considerable, systematic study.
For development of the Borg CR10 as research measure, further study of elicitation procedure is needed. Where reference to the past week of voice use may be clinically meaningful, effort scaling in specified, controlled conditions (e.g. high, quiet voice, loud reading, sustained vocalizations, etc.) is more commensurate with perceptual effort elicitation methods (Eston & Lamb, 2000). Using specific elicitation tasks across various individual can help us understand vocal effort better. Specifically, vocal effort may play a greater role in patient’s perceived severity, as would be expected in phonotraumatic hyperfunctional voice disorders. This can only be determined if the elicitation methods employed remained constant between individuals.
Conclusion
This study provides support for the utility and validity of the Borg CR10 in measuring severity of perceived vocal effort in the clinical setting. Results are limited to individuals with phonotraumatic hyperfunction. With use of experiential anchors, significant treatment-related changes were captured, even for only 4 sessions of therapy. Furthermore, the scale showed a significant relationship to VHI item 14, supporting its construct validity. In capturing severity of vocal effort use, the measure compliment’s VHI item 14’s assessment of frequency. The scale may hold utility for outcome measurement, weekly progress, therapeutic development of awareness, and screening.
Acknowledgments
The work was supported in part by the National Institute on Deafness and Other Communication Disorders (Grant F31DC009526). The authors are indebted to Robert Hendrick for statistical support. The second author would like to thank Kimberly Steinhauer on her suggestion and guidance on using the Borg CR10 as a tool to employ in voice research.
Appendix A. ADAPTED BORG CR-10 FOR VOCAL EFFORT RATINGS
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eva van Leer, Department of Education Psychology, Special Education and Communication Disorders, Georgia State University, Atlanta, GA.
Miriam van Mersbergen, Department of Speech-Language Pathology, Division of Allied Health and Communicative Disorders, Northern Illinois University, DeKalb, IL.
References
- 1.Jiang JJ, Titze IR. Measurement of vocal fold intraglottal pressure and impact stress. J Voice. 1994;8:132–144. doi: 10.1016/s0892-1997(05)80305-4. [DOI] [PubMed] [Google Scholar]
- 2.Chang A, Karnell MP. Perceived phonatory effort and phonation threshold pressure across a prolonged voice loading task: a study of vocal fatigue. J Voice. 2004;18:454–466. doi: 10.1016/j.jvoice.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Baldner EF, Doll E, Van Mersbergen MR. A review of measures of vocal effort with a preliminary study on the establishment of a vocal effort measure. J Voice. 2015;29:530–541. doi: 10.1016/j.jvoice.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 4.Hartl DM, Hans S, Vaissière J, Riquet M, Brasnu DF. Objective voice quality analysis before and after onset of unilateral vocal fold paralysis. J Voice. 2001;15:351–361. doi: 10.1016/S0892-1997(01)00037-6. [DOI] [PubMed] [Google Scholar]
- 5.Inagi K, Khidr AA, Ford CN, Bless DM, Heisey DM. Correlation between vocal functions and glottal measurements in patients with unilateral vocal fold paralysis. The Laryngoscope. 1997;107:782–791. doi: 10.1097/00005537-199706000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Schindler A, et al. Vocal improvement after voice therapy in unilateral vocal fold paralysis. J Voice. 2008;22:113–118. doi: 10.1016/j.jvoice.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Hillman RE, Holmberg EB, Perkell JS, Walsh M, Vaughan C. Objective Assessment of Vocal Hyperfunction An Experimental Framework and Initial Results. J Speech Lang Hear Res. 1989;32:373–392. doi: 10.1044/jshr.3202.373. [DOI] [PubMed] [Google Scholar]
- 8.Mehta DD, et al. Using ambulatory voice monitoring to investigate common voice disorders: research update. Front Bioeng Biotechnol. 2015;3 doi: 10.3389/fbioe.2015.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verdolini-Marston K, Burke MK, Lessac A, Glaze L, Caldwell E. Preliminary study of two methods of treatment for laryngeal nodules. J Voice. 1995;9:74–85. doi: 10.1016/s0892-1997(05)80225-5. [DOI] [PubMed] [Google Scholar]
- 10.Gartner-Schmidt J. Flow phonation. In: Stemple JC, Hapner ER, editors. Voice Therapy- Clinical Case. Studies. Plural Publishing; San Diego, CA: 2010. pp. 84–92. [Google Scholar]
- 11.Stemple JC, Lee L, D’Amico B, Pickup B. Efficacy of vocal function exercises as a method of improving voice production. J Voice. 1994;8:271–278. doi: 10.1016/s0892-1997(05)80299-1. [DOI] [PubMed] [Google Scholar]
- 12.Boone DR. Chapter 7: Voice Facilitating Approaches. In: Boone DR, McFarlane SC, Von Berg SL, Zraick RI, editors. The Voice and Voice Therapy. Pearson; Boston, MA: 2014. pp. 185–242. [Google Scholar]
- 13.Kotby MN, El-Sady SR, Basiouny SE, Abou-Rass YA, Hegazi MA. Efficacy of the accent method of voice therapy. J Voice. 1991;5:316–320. [Google Scholar]
- 14.Borg G. A category scale with ratio properties for intermodal and interindividual comparisons. Psychophys Judgm Process Percept. 1982:25–34. [Google Scholar]
- 15.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 16.Vinney LA, van Mersbergen M, Connor NP, Turkstra LS. Vocal Control: Is It Susceptible to the Negative Effects of Self-Regulatory Depletion? J Voice. 2016 doi: 10.1016/j.jvoice.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 17.Van Mersbergen M, Patrick C, Glaze L. Functional dysphonia during mental imagery: Testing the trait theory of voice disorders. J Speech Lang Hear Res. 2008;51:1405–1423. doi: 10.1044/1092-4388(2008/06-0216). [DOI] [PubMed] [Google Scholar]
- 18.Van Mersbergen M, Lyons P, Riegler D. Vocal Responses in Heighted States of Arousal. J Voice. 2016 doi: 10.1016/j.jvoice.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Borg G, Hassmén P, Lagerström M. Perceived exertion related to heart rate and blood lactate during arm and leg exercise. Eur J Appl Physiol. 1987;56:679–685. doi: 10.1007/BF00424810. [DOI] [PubMed] [Google Scholar]
- 20.Borg G, Ljunggren G, Ceci R. The increase of perceived exertion, aches and pain in the legs, heart rate and blood lactate during exercise on a bicycle ergometer. Eur J Appl Physiol. 1985;54:343–349. doi: 10.1007/BF02337176. [DOI] [PubMed] [Google Scholar]
- 21.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990:55–58. doi: 10.5271/sjweh.1815. [DOI] [PubMed] [Google Scholar]
- 22.Chiu M-C, Wang M-J. The effect of gait speed and gender on perceived exertion, muscle activity, joint motion of lower extremity, ground reaction force and heart rate during normal walking. Gait Posture. 2007;25:385–392. doi: 10.1016/j.gaitpost.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Finsen L, Søgaard K, Jensen C, Borg V, Christensen H. Muscle activity and cardiovascular response during computer-mouse work with and without memory demands. Ergonomics. 2001;44:1312–1329. doi: 10.1080/00140130110099065. [DOI] [PubMed] [Google Scholar]
- 24.Jensen C, et al. Job demands, muscle activity and musculoskeletal symptoms in relation to work with the computer mouse. Scand J Work Environ Health. 1998:418–424. [PubMed] [Google Scholar]
- 25.Shen W, Parsons KC. Validity and reliability of rating scales for seated pressure discomfort. Int J Ind Ergon. 1997;20:441–461. [Google Scholar]
- 26.Razon S, Hutchinson J, Tenenbaum G. Effort Perception. In: Tenenbaum G, Eklund RC, Kamata A, editors. Measurement in Sport and Exercise Psychology. Human Kinetics; 2012. pp. 265–277. [Google Scholar]
- 27.DiIorio CK. Measurement in health behavior: Methods for research and evaluation. John Wiley & Sons; 2006. Validity; p. 1. [Google Scholar]
- 28.Jacobson BH, et al. The voice handicap index (VHI) development and validation. Am J Speech Lang Pathol. 1997;6:66–70. [Google Scholar]
- 29.Verdolini K, Druker DG, Palmer PM, Samawi H. Laryngeal adduction in resonant voice. J Voice. 1998;12:315–327. doi: 10.1016/s0892-1997(98)80021-0. [DOI] [PubMed] [Google Scholar]
- 30.Abbott KV. Lessac-Madsen Resonant Voice Therapy: Clinician Manual. Clinician Manual. Plural Pub; 2008. [Google Scholar]
- 31.Verdolini-Marston K, Burke MK, Lessac A, Glaze L, Caldwell E. Preliminary study of two methods of treatment for laryngeal nodules. J Voice. 1995;9:74–85. doi: 10.1016/s0892-1997(05)80225-5. [DOI] [PubMed] [Google Scholar]
- 32.Speyer R, Wieneke GH, Dejonckere PH. Documentation of progress in voice therapy: perceptual, acoustic, and laryngostroboscopic findings pretherapy and posttherapy. J Voice. 2004;18:325–340. doi: 10.1016/j.jvoice.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Van Leer E, Connor NP. Patient perceptions of voice therapy adherence. J Voice. 2010;24:458–469. doi: 10.1016/j.jvoice.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eston R, Lamb KL. Effort perception. Paediatr Exerc Sci Med. 2000:85–91. [Google Scholar]
- 35.Van Leer E, Connor NP. Predicting and influencing voice therapy adherence using social-cognitive factors and mobile video. Am J Speech Lang Pathol. 2015;24:164–176. doi: 10.1044/2015_AJSLP-12-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abbott KV. Lessac-Madsen Resonant Voice Therapy: Overview. Plural Pub; 2008. [Google Scholar]