Abstract
Introduction:
The co-occurrence of bipolar disorder (BD) and obsessive-compulsive disorder (OCD) seemed to be a poor prognostic factor associated with greater disability, lower social and occupational functioning, poorer treatment response, and higher suicidal ideas and attempts compared to BD patients.
Materials and Methods:
A systematic review was conducted on the risk of suicide in BD-OCD patients compared to BD patients. Relevant papers published through August 2018 were identified searching the electronic databases MEDLINE, EMBASE, PsycINFO, and the Cochrane Library.
Results:
In all cases, diagnoses were according to the standard Diagnostic and Statistical Manual criteria and were established using validated assessment scales. More than 80% of the selected studies presented higher rates of history of suicide attempts and lifetime depressive episodes in BD-OCD patients compared to non-comorbid patients.
Conclusions:
Osler's view that medicine should be a treatment of diseases, not of symptoms, is consistent with the approach of mood stabilization as the first objective in apparent BD-OCD patients, as opposed to immediate treatment with antidepressants. In line with that, especially in comorbid patients, lithium may be preferred because of its proven anti-suicidal effect.
Keywords: Bipolar, comorbidity, obsessive-compulsive, suicide
INTRODUCTION
The co-occurrence of bipolar disorder (BD) and obsessive-compulsive disorder (OCD) was noted 150 years ago by the French psychiatrist Morel,[1] but the significance of this comorbidity has not been sufficiently clarified yet.[2]
Our previous meta-analysis revealed higher comorbidity rates in youths than adults,[3] with the majority of patients experiencing the onset of OCD prior to the onset of BD.[4] Compared to non-BD-OCD patients, BD-OCD patients had a higher prevalence of family history for mood disorders and lower prevalence of family history for OCD.[5] Obsessive-compulsive (OC) symptoms in comorbid patients appeared more often - and sometimes exclusively - during depressive episodes, and comorbid BD and OCD cycled together, with the OC symptoms often remitting during manic/hypomanic episodes.[6] In other words, OC symptoms would initially coexist with BD symptoms, even cycling together, and they would gradually tend to decrease in the adulthood, supporting the hypothesis that OC symptoms in childhood and adolescence are an expression of vulnerability to a later BD diagnosis.[7]
Moreover, BD-OCD comorbidity seemed to be a poor prognostic factor associated with greater disability, lower social and occupational functioning, poorer treatment response, and higher suicidal ideas and attempts compared to BD patients.[8]
Although recent studies have investigated the co-occurrence of anxiety and BDs, the topic is insufficiently studied, and the relationship between BD and OCD remains unclear. To address this unanswered question, we updated our systematic review to investigate specifically the risk of suicide in BD-OCD patients.
MATERIALS AND METHODS
As done before,[9,10] this review was conducted according to methods recommended by the Cochrane Collaboration and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.[11,12]
Information sources and search strategy
Studies were identified by searching the electronic databases MEDLINE, EMBASE, PsycINFO, and the Cochrane Library. We combined the search strategy of free text terms and exploded MESH headings for the topics of bipolar disorder and obsessive-compulsive disorder combined as following: ((((((((“Bipolar Disorder” [Mesh]) OR Bipolar disorder) OR BD) OR Bipolar) OR Manic depressive disorder) OR Manic depressive) OR Manic)) AND (((((“Obsessive-Compulsive Disorder” [Mesh]) OR OCD) OR Obsessive-compulsive) OR Obsessive-compulsive disorder)). The strategy was first developed in MEDLINE and then adapted for use in the other databases. Studies that compared BD patients and BD-OCD patients, published in English, through August 31st, 2018 were included [Figure 1].
Figure 1.
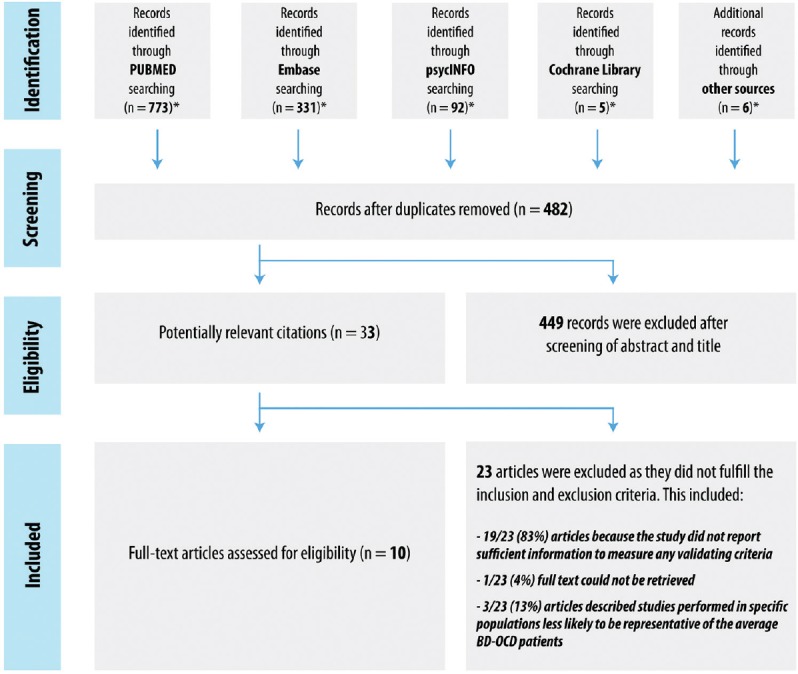
Flow diagram of selected studies
Inclusion criteria
Study population and study design
We considered studies that compared BD patients and BD-OCD patients. BD and OCD were considered if diagnostic criteria used were specified. Among hospital-based studies, inpatients, day-hospital, and outpatient subjects were included, whereas emergency care records were excluded as non-representative. All experimental and observational study designs were included apart from case reports and case series. Narrative and systematic reviews, letters to the editor, and book chapters were excluded.
Outcomes
Studies that investigate the risk of suicide in BD patients and BD-OCD patients were considered.
Study selection and data extraction
Identified studies were independently reviewed for eligibility by two authors in a two-step process: a first screening was performed according to the title and abstract, and then full texts were retrieved for a second screening. At both stages, disagreements by reviewers were resolved by consensus. Data were extracted by two authors and supervised by a third author using an ad-hoc developed data extraction spreadsheet. The data extraction spreadsheet was piloted on three randomly selected papers and modified accordingly.
RESULTS
Ten studies were selected [Table 1]. In all cases, diagnoses were according to the standard Diagnostic and Statistical Manual (DSM) criteria and were established using validated assessment scales. More than 80% of the selected studies presented higher rates of history of suicide attempts and lifetime depressive episodes in BD-OCD patients compared to non-comorbid patients.[13,14,15,16,17] In the Epidemiologic Catchment Area (ECA) database, BD-OCD patients had statistically significant higher lifetime rates of “thoughts of suicide,” “thoughts of death,” “suicide attempts,” and “wanting to die” versus non-comorbid patients.[18] These features were also confirmed in a case-control study conducted in the USA in the adolescent population. OCD was associated with a 2.4-fold increase in the odds of suicidal ideation among BD adolescents as compared to non-comorbid adolescents.[19] Less than 20% of the selected studies did not report a statistically significant difference in terms of suicide attempts between comorbid and non-comorbid patients.[20,21,22]
Table 1.
Studies that met inclusion/exclusion criteria for systematic review
| References | Study design | Country | Study population | Diagnosis assessment | Results | Quality* |
|---|---|---|---|---|---|---|
| Chen et al. 1995[18] | Cross-sectional study | USA | Pt. with BD, unipolar disorder or any Axis I disorder other than bipolar or unipolar disorder (n=6622, age >18): BD (n=167) | DIS; DSM-III | Higher lifetime rates of “thoughts of suicide”, “suicide attempts”, “thoughts of death” and “wanting to die” in BD-OCD pt. vs BD pt. | 25/31 |
| Dilsaver et al. 2006[19] | Case-control study | USA | Latino adolescents (n=313): BD (n=115, mean age=14.6±1.5) | SCID; DSM-IV | BD-OCD pt. associated with a 2.4 fold increase in the odds of suicidal ideation vs BD pt. (95% CI=1.0-5.8). | 18/31 |
| Goes et al. 2012[13] | Cross-sectional study | USA | BD (n=1416, mean age=42.0), first-degree relatives with BD (n=850) | DIGS; DSM-IV | Higher rates of history of suicide attempts in BD-OCD pt. vs BD pt. (48.3 vs. 29.6%). | 23/31 |
| Jeon et al. 2018[20] | Case-control study | Korea | BD (n=264, mean age=35.5), BD-OCD (n=50, mean age=31.8) | SCID; DSM-IV | No statistically significant differences between BD-OCD patients and BD patients in terms of a history of suicidal attempts. | 23/31 |
| Kazhungil et al. 2017[14] | Case-control study | India | BD-I (n=90, mean age=21.69) | SCID; DSM-IV | Higher rates of suicide attempts in BD-OCD pt. vs BD pt. (0.29±0.59 vs. 1.19±0.93). | 23/31 |
| Koyuncu et al. 2010[21] | Case-control study | Turkey | BD (n=214, mean age: BD=34.8±10.3, BD-OCD=36.2±15.9) | SCID; DSM-IV | No statistically significant differences between BD-OCD pt. and BD pt. in terms of lifetime suicide attempts. | 20/31 |
| Kruger et al. 2000[15] | Case-control study | Germany | BD-I or BD-II (n=143, mean age=44) | SCID; DSM-III-R | Higher incidence of prior suicide attempts in BD-OCD pt. vs BD pt. (90% vs. 38%). | 22/31 |
| Magalhaes et al. 2010[16] | Case-control study | Brazil | BD (n=259, mean age=41) | SCID; DSM-IV | Higher rates of history of suicide attempts in BD-OCD pt. vs BD pt. (70% vs. 35%). | 23/31 |
| Shashidhara et al. 2015[22] | Case-control study | India | BD-I (n=396, mean age=22.55) | MINI-BIPOLAR; DSM-IV | No statistically significant differences between BD-OCD pt. and BD pt. in terms of current suicide risk. | 23/31 |
| Simon et al. 2004[17] | Cross-sectional study | USA | BD (n=475, mean age=41.7±12.8) | MINI; DSM-IV | Higher rates of history of suicide attempts in BD-OCD pt. vs BD pt. | 23/31 |
BD: bipolar disorder; OCD: obsessive-compulsive disorder; DSM: Diagnostic and Statistical Manual of Mental Disorders; SCID: Structured Clinical Interview; DIS: Diagnostic Interview Schedule; DIGS: Diagnostic Instrument for Genetic Studies; MINI: Mini International Neuropsychiatric Interview; MINI-BIPOLAR: MINI: Mini International Neuropsychiatric Interview for Bipolar Disorders Studies. *Checklist for measuring study quality developed by Downs and Black
DISCUSSION
The main limitation of this systematic review is linked to the study design and analysis strategy of the included studies, as documented by the quality assessment scale used. Most studies are observational, according to the retrospective assessments, and do not include a control group. Small sample size and enrollment of subjects mainly from BD-OCD outpatient units may limit the generalizability of these results. Potential confounding factors, such as demographic and clinical variables and phase of illness, often were not appropriately analyzed through multivariate modeling. Moreover, suicide outcomes were assessed by structured interview in only a minority of the studies. The strength of the selected studies is that the diagnosis of BD, OCD, and comorbid psychiatric disorders were consistently according to the DSM criteria and were established by trained investigators mainly using validated assessment scales, with good interrater reliability. The main strength of this review is its being systematic and its inclusion of the entire scientific evidence published so far on the main medical databases.
It is of crucial importance to identify effective and safe maintenance therapy for BD-OCD comorbidity so as to reduce patients’ mood instability, hospitalization rates, and the risk of suicide and to improve their quality of life. Osler's view that medicine should be a treatment of diseases, not of symptoms, is consistent with the approach of mood stabilization as the first objective in apparent BD-OCD patients, as opposed to immediate treatment with antidepressants.[23] In line with that, especially in comorbid patients, lithium may be preferred because of its proven anti-suicidal effect.
Considering the important nosological, clinical, and therapeutic implications, prospective controlled studies with long-term follow-up data collected are needed to confirm or refute our findings and consequent clinical recommendations. In particular, further research is required to investigate several risk factors such as severity of illness, other comorbid disorders, or treatment resistance that might be associated with elevated risk of suicidal behavior among BD-OCD patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Morel BA. Traité des Maladies Mentales. 2nd ed. Paris: Masson; 1860. [Google Scholar]
- 2.Tonna M, Amerio A, Ottoni R, Paglia F, Odone A, Ossola P, et al. The clinical meaning of obsessive-compulsive symptoms in bipolar disorder and schizophrenia. Aust N Z J Psychiatry. 2015;49:578–9. doi: 10.1177/0004867415572010. [DOI] [PubMed] [Google Scholar]
- 3.Amerio A, Stubbs B, Odone A, Tonna M, Marchesi C, Ghaemi SN. The prevalence and predictors of comorbid bipolar disorder and obsessive-compulsive disorder: A systematic review and meta-analysis. J Affect Disord. 2015;186:99–109. doi: 10.1016/j.jad.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 4.Tonna M, Amerio A, Odone A, Stubbs B, Ghaemi SN. Comorbid bipolar disorder and obsessive-compulsive disorder: Which came first? Aust N J Psychiatry. 2016;50:695–8. doi: 10.1177/0004867415621395. [DOI] [PubMed] [Google Scholar]
- 5.Amerio A, Tonna M, Odone A, Stubbs B, Ghaemi SN. Heredity in comorbid bipolar disorder and obsessive-compulsive disorder patients. Shanghai Arch Psychiatry. 2015;27:307–10. doi: 10.11919/j.issn.1002-0829.215123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amerio A, Tonna M, Odone A, Stubbs B, Ghaemi SN. Course of illness in comorbid bipolar disorder and obsessive-compulsive disorder patients. Asian J Psychiatr. 2016;20:12–4. doi: 10.1016/j.ajp.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Tonna M, Amerio A, Odone A, Ossola P, Marchesi C, Ghaemi SN. Are obsessive-compulsive symptoms expression of vulnerability to bipolar disorder? Acta Psychiatr Scand. 2015;132:411–2. doi: 10.1111/acps.12481. [DOI] [PubMed] [Google Scholar]
- 8.Amerio A, Odone A, Liapis CC, Ghaemi SN. Diagnostic validity of comorbid bipolar disorder and obsessive-compulsive disorder: A systematic review. Acta Psychiatr Scand. 2014;129:343–58. doi: 10.1111/acps.12250. [DOI] [PubMed] [Google Scholar]
- 9.Amerio A, Galvéz JF, Odone A, Dalley SA, Ghaemi SN. Carcinogenicity of psychotropic drugs: A systematic review of US Food and Drug Administration-required preclinical in vivo studies. Aust N Z J Psychiatry. 2015;49:686–96. doi: 10.1177/0004867415582231. [DOI] [PubMed] [Google Scholar]
- 10.Marchesi C, Ossola P, Amerio A, Daniel BD, Tonna M, De Panfilis C. Clinical management of perinatal anxiety disorders: A systematic review. J Affect Disord. 2015;190:543–50. doi: 10.1016/j.jad.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Higgins J, Green S, editors Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1. The Cochrane Collaboration. 2001 [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goes FS, McCusker MG, Bienvenu OJ, Mackinnon DF, Mondimore FM, Schweizer B, et al. Co-morbid anxiety disorders in bipolar disorder and major depression: Familial aggregation and clinical characteristics of co-morbid panic disorder, social phobia, specific phobia and obsessive-compulsive disorder. Psychol Med. 2012;42:1449–59. doi: 10.1017/S0033291711002637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kazhungil F, Cholakottil A, Kattukulathil S, Kottelassal A, Vazhakalayil R. Clinical and familial profile of bipolar disorder with and without obsessive-compulsive disorder: An Indian study. Trends Psychiatry Psychother. 2017;39:270–5. doi: 10.1590/2237-6089-2017-0061. [DOI] [PubMed] [Google Scholar]
- 15.Kruger S, Braunig P, Cooke RG. Comorbidity of obsessive-compulsive disorder in recovered inpatients with bipolar disorder. Bipolar Disord. 2000;2:71–4. doi: 10.1034/j.1399-5618.2000.020111.x. [DOI] [PubMed] [Google Scholar]
- 16.Magalhaes PV, Kapczinski NS, Kapczinski F. Correlates and impact of obsessive-compulsive comorbidity in bipolar disorder. Compr Psychiatry. 2010;51:353–6. doi: 10.1016/j.comppsych.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Simon NM, Otto MW, Wisniewski SR, Fossey M, Sagduyu K, Frank E, et al. Anxiety disorder comorbidity in bipolar disorder patients: Data from the first 500 participants in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) Am J Psychiatry. 2004;161:2222–9. doi: 10.1176/appi.ajp.161.12.2222. [DOI] [PubMed] [Google Scholar]
- 18.Chen YW, Dilsaver SC. Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. 1995;59:57–64. doi: 10.1016/0165-1781(95)02752-1. [DOI] [PubMed] [Google Scholar]
- 19.Dilsaver SC, Akiskal HS, Akiskal KK, Benazzi F. Dose-response relationship between number of comorbid anxiety disorders in adolescent bipolar/unipolar disorders, and psychosis, suicidality, substance abuse and familiality. J Affect Disord. 2006;96:249–58. doi: 10.1016/j.jad.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Jeon S, Baek JH, Yang SY, Choi Y, Ahn SW, Ha K, et al. Exploration of comorbid obsessive-compulsive disorder in patients with bipolar disorder: The clinic-based prevalence rate, symptoms nature and clinical correlates. J Affect Disord. 2018;225:227–33. doi: 10.1016/j.jad.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 21.Koyuncu A, Tukel R, Ozyildirim I, Meteris H, Yazici O. Impact of obsessive-compulsive disorder comorbidity on the sociodemographic and clinical features of patients with bipolar disorder. Compr Psychiatry. 2010;51:293–7. doi: 10.1016/j.comppsych.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 22.Shashidhara M, Sushma BR, Viswanath B, Math SB, Janardhan Reddy YC. Comorbid obsessive compulsive disorder in patients with bipolar-I disorder. J Affect Disord. 2015;174:367–71. doi: 10.1016/j.jad.2014.12.019. [DOI] [PubMed] [Google Scholar]
- 23.Amerio A, Odone A, Marchesi C, Ghaemi SN. Do antidepressant-induced manic episodes in obsessive-compulsive disorder patients represent the clinical expression of an underlying bipolarity? Aust N Z J Psychiatry. 2014;48:957–63. doi: 10.1177/0004867414530006. [DOI] [PubMed] [Google Scholar]


