Abstract
Setting:
A northern province in Thailand.
Objectives:
To explore experiences and perspectives on tuberculosis (TB) contact investigations in non-household contacts.
Design:
Focus group discussions and in-depth interviews with eight groups: three groups of former TB patients (teachers, students and hospital staff) and five groups of representatives from congregate settings such as schools and workplaces. Data were analysed using the modified grounded theory.
Result:
Annual health check-ups at the workplace contributed to the early detection of active TB in teachers. Former TB patients were highly exposed to non-household contacts, but contact investigations were limited to household contacts only. Barriers and facilitators for non-household contact investigations are associated with five factors, including information, awareness and knowledge about TB; stigma; empathy; health system response and informing non-household contacts about TB exposure. Stigma may be the main barrier to investigations among non-household contacts because TB patients tend to withhold information about their diagnosis from colleagues. Lack of knowledge and misperceptions regarding TB transmission contributed to stigma. Empathy with other people encouraged TB patients to inform non-household contacts.
Conclusion:
Non-household contact investigations are not performed despite the risk of TB transmission. To promote contact investigations in congregate settings, interventions to overcome TB stigma and improve public knowledge about TB transmission are required.
Keywords: TB; contact investigation; stigma, qualitative research; non-household
Abstract
Contexte :
Une province du nord de la Thaïlande.
Objectif :
Explorer les expériences et les perspectives relatives à la recherche des contacts de tuberculose (TB) en ce qui concerne les contacts hors domicile.
Schéma :
Des discussions en groupe focal et des entretiens approfondis avec huit groupes : trois groupes d’anciens patients TB (enseignants, étudiants et personnel de l’hôpital) et cinq groupes de représentants de collectivités comme des écoles et des lieux de travail. Les données ont été analysées par la méthode de la théorisation ancrée.
Résultats :
Des bilans de santé annuels sur le lieu de travail ont contribué à la détection précoce de la TB active parmi les enseignants. Les anciens patients tuberculeux ont été très exposés à des contacts hors domicile, mais les procédures de recherche des contacts ont été limitées aux contacts domiciliaires. Les contraintes et les facilitateurs de recherche de contacts hors domicile sont associés à cinq catégories incluant l’information, la sensibilisation et les connaissances relatives à la TB, la stigmatisation, l’empathie, la réponse du système de santé et l’information des contacts relative à l’exposition à la TB. La stigmatisation peut être un obstacle majeur au dépistage des contacts hors domicile parce que les patients TB ont tendance à dissimuler leur diagnostic à leurs collègues. Le manque de connaissances et des perceptions erronées de la transmission de la TB ont contribué à la stigmatisation. Ressentir de l’empathie vis-à-vis de la maladie des autres personnes a encouragé les patients TB à informer leurs contacts hors domicile.
Conclusion :
La recherche de contacts hors domicile n’est pas mise en œuvre bien qu’il y ait un risque de transmission de la TB. La promotion de la recherche de contacts dans des collectivités, des interventions visant à vaincre la stigmatisation de la TB et l’amélioration des connaissances du public relatives à la transmission de la TB sont requises.
Abstract
Marco de Referencia:
Una provincia al norte de Tailandia.
Objetivos:
Examinar las experiencias y las perspectivas sobre la investigación de los contactos de pacientes con tuberculosis (TB) que no son contactos domiciliarios.
Método:
Se llevaron a cabo sesiones de grupos de opinión y entrevistas exhaustivas con ocho grupos: tres grupos de antiguos pacientes con TB (profesores, estudiantes y personal hospitalario) y cinco grupos de representantes de entornos colectivos como escuelas y lugares de trabajo). Los datos se analizaron mediante una estrategia modificada de muestreo teórico.
Resultado:
Los reconocimientos médicos anuales en el lugar de trabajo contribuyeron a la detección temprana de la TB activa en los profesores. Los antiguos pacientes con TB exhibieron una exposición alta a contactos no domiciliarios, pero las investigaciones de contactos se limitaban a los contactos en los hogares. Los obstáculos y los factores facilitadores de la investigación de contactos no domiciliarios se asociaron con cinco categorías que incluían la información, la sensibilización y los conocimientos sobre la TB, la estigmatización, la empatía, la respuesta del sistema de salud y el hecho de informar a los contactos no domiciliarios sobre la exposición a la TB. La estigmatización puede constituir el mayor obstáculo a la investigación de los contactos no domiciliarios, pues los pacientes con TB tienden a ocultar el diagnóstico a sus colegas. La falta de conocimientos y las percepciones erradas sobre la transmisión de la TB contribuyen a la estigmatización. El sentimiento de empatía frente a la enfermedad de otras personas estimula a los pacientes con TB a informar a sus contactos fuera del domicilio.
Conclusión:
La investigación de los contactos no domiciliarios no se practica, pese a que existe el riesgo de transmisión de la TB. Con el fin de promover esta investigación en los ambientes colectivos, es preciso realizar intervenciones que contribuyan a superar la estigmatización y mejoren los conocimientos que tiene el público sobre la transmisión de esta enfermedad.
Tuberculosis (TB) is a global public health problem. Although Thailand is ranked as a high middle-income country and has achieved universal health coverage for over a decade,1 it is listed as one of 14 countries with the highest burdens of TB, TB and human immunodeficiency virus (HIV) co-infection and multi-drug-resistant TB (MDR-TB). Although TB is curable, every year TB kills more than 10 000 people in Thailand.2 Contact investigation is an important strategy to lower TB mortality and the risk of TB transmission in the community because close contacts are assessed for TB early and provided with timely access to care and prevention.3 However, the implementation of contact investigation is limited.4 Barriers to low coverage of contact investigation include stigma, low accessibility to health services and poor knowledge and attitude among health staff.5–8 Contact investigations should cover both household and non-household contacts. Several studies have shown that TB transmission occurs in nurseries, schools, hospitals, workplaces and other settings.9–12 However, most published studies from high-burden countries mainly report contact investigation in household contacts. Little is known about the barriers to TB investigation among non-household contacts. Because there are no guidelines on contact investigation in Thailand, we conducted operational research to obtain information to develop guidelines. These guidelines should advise health workers on how to recognise household and non-household contacts and manage barriers to contact investigation.
The present qualitative study investigates the experiences and perspectives of persons without TB and former TB patients from settings where TB transmission may occur outside of the household setting. The research questions were as follows: what is the possibility of TB transmission in congregate settings such as schools and workplaces? What are the barriers and facilitators for contact investigations in these settings?
STUDY POPULATION, DESIGN AND METHODS
Study area and tuberculosis service
We conducted the study in a province in northern Thailand. In 2017, the provincial TB statistics showed a TB notification rate of 143 per 100 000 population, a death rate of 11.4% and a TB-HIV co-infection rate of 15.5%, which are higher than the national figures. TB patients receive free TB diagnosis and treatment at government hospitals. However, some patients pay for care at private hospitals. In practice, contact investigation for TB is mostly limited to household contacts. Upon diagnosis, TB clinic staff verbally ask TB patients to bring everyone living in the same house to be screened for TB at the hospital. However, no data exist as to whether this advice is rigorously followed and as such, there is no systematic evaluation of contact investigation coverage.
Participants and sampling procedure
We conducted focus group discussions (FGDs) and in-depth interviews with eight different groups. These included three groups of former TB patients whose lifestyle and jobs exposed them to non-household contacts (teachers, students and hospital staff) and five groups including business and industry, boarding schools, kindergarten schools, pre-schools and a group of students’ parents. Table 1 describes the study participants, sampling procedure and some characteristics of the participants selected.
TABLE 1.
Recruitment of study participants and sampling procedure *
| Groups of participants | Methods of identifying the participants (sampling) | Number of invited participants and result of the invitation | Number and characteristic of participants in each FGD and individual in-depth interviews |
|---|---|---|---|
| Former TB patients teachers | TB register 2015–2016 | Invited (n = 12) | Three in-depth interviews (1 male computer teacher, 1 female elementary school teacher and 1 female university lecturer; age: 28–45 years) |
| Declined (n = 2) | |||
| Moved to other provinces (n = 3) | |||
| No reply (n = 4) | |||
| Former TB patients students | TB register 2015–2016 most recent cases | Invited (n = 13 | FGD with 3 participants: 1 female primary school student, who came with her father, and 1 female university student |
| Declined (n = 2) | |||
| No reply (n = 9) | |||
| Former TB patients hospital staff | TB register 2007–2016 (selected all cases) | Invited (n = 14) | FGD with 7 participants (4 males, 3 females; age: 30–55 years): 2 medical doctors, 2 nurses and 3 non-medical staff |
| Declined (n = 4) | |||
| No reply (n = 3) | |||
| Representatives from kindergarten schools | Simple random sampling of 14 PESAO schools | Invited (n = 14) | FGD with 5 female participants (age: 30–45 years): 3 from private schools and 2 from public schools |
| Declined (n = 2) | |||
| No reply (n = 7) | |||
| Representatives from pre-schools | Local administrative offices and municipality office (simple random sampling for 14 nurseries) | Invited (n = 14) | FGD with 8 participants (7 females, 1 male; age: 25–50 years): 2 nursery heads and 6 nursery care givers |
| Refused (n = 3) | |||
| No reply (n = 1) | |||
| Representatives of boarding schools | List of boarding schools from PESAO; simple random sampling of 14 schools | Invited (n = 14) | FGD with 5 female participants (age: 25–40 years): all from public boarding schools, including 4 elementary schools and 1 junior/senior high school with 5–720 students each) |
| Declined (n = 8) | |||
| No reply (n = 1) | |||
| Students’ parents | List of schools from PESAO (simple random sampling for 14 schools) | Invited (n = 14) | FGD with 7 participants (age: 30–50 years): 2 fathers and 5 mothers of students from 2 kindergarten schools, 4 elementary schools and 1 high school) |
| Declined (n = 7) | |||
| Representatives from business sector | Obtained a list from Department of Occupational Health of a tertiary hospital (all selected) | Invited (n = 11) | FGD with 9 participants (age: 28–50 years; 3 males, 6 females): 1 manager and 8 heads of human resources from 5 food industries, 2 hotel and spas, 1 construction company and 1 department store |
| Declined (n = 2) |
* After identifying the participants, the project sent official invitation letters with an information sheet for research participants and a reply form, which were approved by the ethical research committee (institutional review board). It was clearly indicated that participants have right to refuse participation in the FGD without justification. Most participants had a mobile telephone although several participants changed their telephone numbers and could not be contacted.
FGD = focus group discussion; TB = tuberculosis; PESAO = Primary Educational Service Area Office.
METHODS
Between April and June 2017, a single moderator (JN; 20 years of experience in TB and qualitative research) conducted all FGD sessions. Two researchers (JN and SL) conducted individual in-depth interviews with teachers who were former TB patients. Each FGD lasted 2–3 h; the individual in-depth interviews lasted 50–90 min. All FGD sessions were organised in a hotel meeting room, except for the former TB patient hospital staff group, which was held in a hospital meeting room. A note-taker observed and detailed the participants’ body language during the discussions. All discussions were recorded using a digital voice recorder. During FGDs with former TB patients, questions were used to prompt participants to share their experiences with TB illness, TB stigma and disclosure about their TB to others. They also shared experiences of contact investigations among their household and non-household contacts. The questions for the FGDs with representatives from congregate settings addressed the perception of TB, stigma against TB and current policy and practice for communicable diseases. A hypothetical question asking how they would react if doctors informed them that they had TB was also included. Moreover, topics encompassing contact investigation at schools and workplace with regards to potential barriers were discussed. The moderator incorporated findings from the previous FGD sessions to explore and triangulate the data with the subsequent sessions. At the end of each FGD session, the moderator responded to questions raised by participants and displayed short video clips relating to TB and the importance of contact investigation. The participants received 500 Thai baht (US$15) for travel and compensation. After finishing the FGD sessions, the participants were invited for lunch, which sometimes provided an opportunity to collect further information.
Data analysis
Immediately after each FGD session, the moderator and the note-taker summarised the key findings and observations. The note-taker then transcribed the recordings verbatim using the Thai Microsoft Office Word (MicroSoft, Redmond, WA, USA). Short notes on the participants’ body language, tone of voice and atmosphere observed during the session were inserted into the transcribed texts.13 The moderator then carefully reviewed the material and analysed the data using the modified grounded theory.14,15 We performed open coding, listed all codes and grouped them into categories and identified properties and dimensions. Based on the research question, a model of barriers and facilitators for TB contact investigation for non-household contacts was then developed.
Ethical consideration
The study was approved by the Ethical Research Committee of Chiang Rai Prachanukroh Hospital, Chiang Rai, Thailand (CR 0032.102/8398). All participants provided written informed consent before starting the discussions and interviews. To prevent negative consequences to the participants and institutions, the names of the study settings and participants’ gender are not reported.
RESULTS
All participants actively participated in the FGDs and interviews. Table 2 summarises the participants’ behaviour and the atmosphere of each group. Despite different social, economic and working backgrounds, every group reported similar findings regarding stigma against TB, misperceptions about modes of TB transmission and the use of the internet as the primary source of TB information seeking.
TABLE 2.
Atmosphere and participants’ manners observed during the FGDs and the individual in-depth interviews
| Group of participants | Atmosphere and behaviour observed during the session |
|---|---|
| Individual interviews: former TB patients, school teachers and a university lecturer | Teacher 1: active participation in the interview, looked sensitive with shaky voice when discussing how she was seated in a hospital’s isolation area designated for persons with communicable disease |
| Teacher 2: active participation in the interview. No visible emotional facial expressions or change of voice throughout the interview | |
| Teacher 3: telephone interview. Lively and active in the discussion. Sounded calm throughout the interview | |
| FGD (3 participants): former TB patients; school and university students | Student 1 (Grade 4 primary school): very shy and quiet, frequently nodding or shaking her head instead of speaking, frequently holding her father’s arm |
| Father of Student 1: active participation in the discussion, asked several questions | |
| Student 2: active participation in the discussion. No visible emotional facial expressions or change of throughout the discussion | |
| FGD (7 participants): former TB patients, hospital staff | Doctors and nurses were very active in the discussion. Encouragement from the moderator was needed to encourage non-medical staff to talk. One doctor talked in a high tone of voice and was emotional when he explained how he felt when he discovered he had TB |
| FGD (5 participants): head/representatives from kindergarten schools | All participants were very active in the discussion and asked questions from the beginning of the session |
| FGD (9 participants): head/representatives of pre-schools | Most participants were very active in the discussion. There was a heated debate on the issue of disclosing their hypothetical TB diagnosis to their colleagues |
| FGD (5 participants): head/representatives of boarding schools | Three participants were very active in the discussion, while the other two participants joined mainly when the moderator encouraged them to share their opinion and experiences |
| FGD (7 participants): parents of students | Male participants talked in loud voices and were more active in the discussion than female participants. One mother looked worried after learning that small children are at risk of contracting TB because her father in-law recently passed away due to TB. She often visited him with her son aged <5 years. One male participant insisted during the discussion that if he had TB, he would not tell anyone, even his family. His face looked worried but he appeared to be relieved after obtaining more information about TB |
| FGD (9 participants): managers and heads of human resources from the business sector | All participants were active in the discussion, particularly a male participant and a female participant, who recently had a worker with TB. They shared their experience and described how their boss was fearful of the worker with TB |
FGD = focus group discussion; TB = tuberculosis.
Possibility of tuberculosis transmission to non-household contacts
Among the former TB patient groups, only doctors and nurses knew they were at risk for TB due to their working conditions. The other former TB patients, including teachers, students and non-medical staff, were surprised to learn that that they were exposed to TB although their family and the people around them did not have TB. However, a university student suspected her friend with serious cough might spread TB to her. We found that the number of non-household contacts was likely to vary between 20 and 100 persons with 1–8 h of daily contact. None of the non-household contacts of the former TB patients had undergone TB screening. Results from the non-TB group FGD in terms of the number of contacts and the duration of exposure were similar. However, physical proximity is particularly high in cases with small children and teachers or care givers. Due to high temperatures, particularly in the city, classrooms of several kindergartens, pre-schools, universities and office workplaces are equipped with air conditioning. Although the ordinary classrooms of some schools do not have air conditioning, every computer classroom is equipped with air conditioning. A computer class lasts 1–2 h for 30–40 students from kindergarten level to high school.
I teach Grade 1 students. Only one teacher teaches every subject and stays with children for 6 h. They are small kids and several times they cried. I have to hug or put them on my lap. (In-depth interview with former TB patient, teacher #1. Similar views were expressed in the other two FGDs with pre-school and kindergarten teachers)
Some subjects I studied with the same group of students in the same (air-conditioned room) from morning to evening. Some subjects I studied only 1 h with one hundred students in a big hall. (FGD; former TB patient, university student #1)
Children are with us from 7.30 am to 4.30 pm, sometimes until 5 pm. Sometimes parents do not pick them up. Mothers always put their children with us. They often just bring a bag of medicine and ask us to take care of their sick child. (FGD pre-school; care giver #1, confirmed by other care givers)
An annual health check-up, which included a mobile chest X-ray (CXR) available at the schools, contributed to the early detection of active TB in three teachers who were former TB patients. Conversely, not participating in the annual health check of three hospital staff who were former TB patients (two doctors and one nurse) may have contributed to an increased risk of TB transmission to their colleagues and patients due to delayed diagnosis and treatment. Teachers and care givers who are government civil servants are eligible for annual health check-ups. However, staff working in private schools or with the local government administration have neither health insurance nor access to annual health check-ups. Despite the availability of mobile CXR services in schools, only 60–70% of individuals underwent CXR, which is less than testing for diabetes and cholesterol. The reasons for low CXR coverage included the inconvenience of female teachers having to change clothing and being unable to cope with the CXR result if the examination showed TB.
My dad had TB when I was at elementary school. I did not have a chest X-ray at my school. I cannot get over if the result shows I have TB. I dare not …my dad had (TB). I just wait until I have symptoms. I’m afraid I can’t cope. (FGD for boarding school staff; computer teacher in primary school. Similar expressions were also reported in FGD by a kindergarten teacher)
I think I am a doctor. I am healthy. I have never had an annual health check. I did not have any symptoms. A nurse encouraged me to have an annual chest X-ray and I decided to do one. When I looked my chest film (sound of deep breath), I was so shocked and immediately felt down. There was a cavity in the lung. I did not have any symptoms but suddenly I found a lung cavity!! (FGD; former TB patient hospital staff, physician #1, confirmed by physician #2 regarding not having an annual health check-up)
All boarding schools reported that students with communicable diseases are sent back to their homes. Only one out of five boarding school had a designated isolation room in the dormitory, and acknowledged that some parents living in other provinces cannot pick up their children immediately. All groups reported that there were no school guidelines for the management of communicable diseases. Instructions for the management of teachers and students/children with infectious diseases including TB were therefore not available.
Before employing staff members, labour laws require employers to screen for five critical diseases and health conditions, including active TB. In practice, physician-issued medical certificates based on only verbal screenings are accepted in many workplaces. However, participants from food industries consistently reported that all newly recruited workers had to submit medical certificates, together with health examination results, including CXR. The workers are responsible for paying for pre-employment medical check-up costs themselves. Given that food industries export to Europe and require high quality control of food products, they cannot afford to be negligent of disease screening and good hygiene practices.
Barriers and facilitators for non-household tuberculosis contact investigation
This study created a model of barriers and facilitators for non-household contact investigation comprising five categories and one core category. The properties and dimensions of these categories were also identified (Figure 1 and Table 3). The first category ‘Information, awareness and knowledge about TB’ is further subdivided into three subcategories—stigma, empathy and health system response. These three categories are related to the category ‘Informing non-household contacts about TB exposure’. For example, if stigma is high, TB patients are less concerned about other people’s health, and health services do not carry out contact investigation in non-household contacts. In such cases, non-household contacts are not screened for TB because, either the TB patients or the health care system do not inform non-household contacts about the need for TB screening. Contact investigation in non-household contacts is thus poor. Each category is described below:
FIGURE.
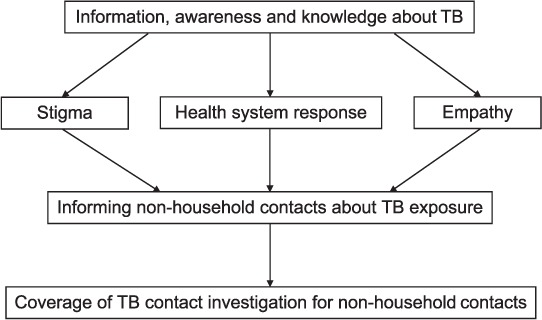
Model of barriers to and facilitators for TB contact investigation among non-household contacts. TB = tuberculosis.
TABLE 3.
Categories leading to investigation among non-household contacts for TB
| Categories | Open codes | Properties and dimension |
|---|---|---|
| Non-household contact investigation | TB screening, annual health check-up, no X-ray, enforcement | Degree (none, some, all) |
| Information, awareness and knowledge about TB | TB cause, TB prevention, TB transmission, doctor’s advice, family with TB, Google, internet, reject chest X-ray, wait until having symptoms, no symptoms, no TB screening, using mask, peer education at workplace, parents’ knowledge, knowing but not changing | Type (medical, lay), source (self, friends, health staff, internet, school, workplace), accuracy (correct, incorrect), level (low, moderate, high) |
| Stigma | Disgusting, crying, shock, fear, keeping distance, confidential, isolation room, wearing mask, cannot cope with TB, cannot get over, forgetting TB by travelling, fired from work, reject sick leave, perceived incurable, awful word ‘communicable disease’ | Type (felt, enacted), source (self, family, friend, colleagues, community) degree (none, some, high, extremely high), ethnicity (Thai, hill tribe), impact (none, depression, loss job, loss clients, bad organization, reputation) |
| Health system response | Doctor advice, ignorance of patient’s occupation, only household contacts, no recognition of non-household contacts, infection control policy in school and workplace | Magnitude (none, some), level (none, low) |
| Empathy | Must prevent others, consideration, public minded, selfish business, love but fearful of contagion, concerned about other persons’ health | Relation (student-teacher, boss-colleagues, care givers-clients, friend-friend), magnitude (none, low, high) |
| Informing non-household contacts about TB exposure | Keep TB secret, no friends know, telling others disease not TB, no secret in the world, openly disclosed, must inform | Method (self-report, observations, rumour) magnitude (none, some, all), time (immediately, later, not at all), relation (close, distant) |
TB = tuberculosis
Information, awareness and knowledge about tuberculosis
Almost all participants of all the groups had heard about TB from several sources, such as at school at a young age, due to TB among family members with TB and on television. Despite differing social, financial and work backgrounds, all of the groups mentioned the internet as the primary source of TB information seeking.
From the participants’ perspectives, TB is caused by smoking, poor living conditions in unhealthy environments, poor nutrition and sharing opium pipes with TB patients. Most participants considered TB to be a serious disease because it was infectious. In Thailand, employers are barred from recruiting persons with TB. Participants knew that TB is a communicable disease that can be easily transmitted to other people. Except for the physicians and nurses who were former TB patients, most participants believed that TB was transmitted by air through breath and saliva. As a result, all participants in all of the groups said TB prevention should include avoiding eating with TB patients, as TB is also transmitted through eating and drinking. In the FGD group comprising parents of students, one father firmly believed that a person eating healthy food and performing regular exercise such as himself could never have TB.
I will never get sick with TB. Even if the doctor told me that I had TB, I would not believe him. I am sure …nobody in my family or people I know have had TB. I eat healthy food, I exercise every day. I don’t have any risk-associated behaviour…I am not exposed to TB patients… how could I get TB? I don’t believe it’s possible. (FGD; student’s parent group; Participant #1, father of a high school student, said in a loud voice)
Despite these strong beliefs, it is worth noting that Participant #1 entirely changed his perception of how TB occurs after watching a video showing how persons with TB can go undetected in everyday life. He realised that people can be unintentionally exposed to TB patients for long periods of time and be infected without knowing.
Stigma
Participants of all the study groups agreed that public stigma against TB was high. Although some teachers, students and physicians who were former TB patients experienced both felt and enacted stigma, a few former TB patients reported experiencing neither type of stigma. Most of the stigma surrounding TB was related to the perceived risk of infection. The words ‘communicable disease’ (rok-tid-tor in Thai) are culturally considered alarming and frightening. People think that being in close proximity to TB patients would cause them to easily contract TB. Nevertheless, several FGD sessions consistently reported that stigma against TB seems to be less among hill tribe communities. The reason for this is unclear as these observations were made by participants in FGD sessions who did not belong to hill tribes.
Reactions to enacted stigma in this study included keeping one’s distance, avoiding communication with TB patients, wearing masks when TB patients shared the same office and designating a special area in the hospital for TB patients. Reactions to felt stigma included crying, stress, depression, feeling down, telling people they had other diseases and travelling. Physicians generally granted 2 weeks of sick leave to newly diagnosed pulmonary TB patients to prevent TB transmission in the workplace. However, due to the high levels of stigma, some patients coped with stress by travelling. A former TB patient, a teacher, drove a private car with her parents to her mother’s hometown (5 h of driving). She opened the car’s windows and wore a mask throughout the trip. Another former TB patient who was a doctor took two hour-long flights to a famous sea resort in the south. He wore a surgical mask on top of an N-95 mask. He did not eat or drink on the airplane.
I broke down…I cried…I did not want to tell my family…I wanted to avoid examining TB patients. I don’t know how to explain. I don’t know how people surrounding me think about my TB. It was TB with a cavity! Every time I treated TB patients in the past, I tried to keep a good distance from them. Once I had TB, I could not help thinking how other people may treat me the way I thought about and behaved towards TB patients. (FGD, former TB patient, hospital staff, physician #1, said in a continuous high-pitched voice)
My boss noticeably changed her manner. She avoided direct communication with Mr A (staff member with TB). She avoided him physically. Every colleague wore face masks when Mr A was in the office. When he returned home, everyone removed their face masks. Staff were really frightened of TB. No one stayed close to Mr A. I was so sorry for him that all workers including the boss shunned him so. (FGD; private business; Male Participant #1, Head of Human Resources in a departmental store)
Participants reported that TB stigma may result in losing job opportunities or losing a job. If parents know that the teachers or care givers of private pre-schools or kindergartens have TB, they may withdraw their children from the schools. Schools can lose their reputation, which in turn, reduced the number of new applicants. A former TB patient who was a physician reported that he could not go to study in the United States due to TB with cavitation.
All the children would definitely be taken out of pre-school if parents knew a teacher (or care giver) had TB, they would push the pre-school head to take action. (FGD; pre-school: Care giver #7)
Empathy
Due to TB stigma, most participants belonging to non-TB groups reported that if they had TB, they would not inform non-household contacts because they would be disgusted and their employers would face serious consequences. Nevertheless, some of the former TB patients informed their colleagues at the university and the hospital. This issue was hotly debated during the pre-school group discussion. Half of the participants would inform their colleagues because they were concerned about TB transmission to children. They felt their contacts should seek timely TB screening and prevent TB transmission. By contrast, the remaining participants felt that informing others about the TB diagnosis would be risky because parents could panic, create rumours and push the school to take aggressive action against care givers with TB. Although they did not tell non-household contacts about their TB, teachers who were former TB patients wore masks all the time when giving lectures or when in the classroom with students. However, a former TB patient who was a student wore a mask in the classroom, not for the sake of preventing TB transmission to others, but to avoid exposure to additional germs from her friends.
After I knew that I had TB, I immediately sent a message to my Line group (an instant communication on smartphones that can reach a large number of people) to inform them that I have TB. I asked the group to avoid visiting me because they will be exposed to TB. (FGD; former TB patient hospital staff, Physician #2)
If it is me. I have to consult my supervisor how to manage. I must know myself that I have a disease that can spread to children. I must stay away from them. It is not right that we continue working with children. (FGD; pre-schools: Male Participant #1, confirmed by four other participants)
Well…Do you remember? At the time of the AIDS crisis, persons having AIDS were not allowed to sit and eat with others. TB is worse because just breathing and being close to the person could result in TB. If our colleagues know that we have TB, the community will also know. It will be very difficult living in the community if people know. (FGD pre-school; Participant #2, confirmed by three other participants).
Health system response
All former TB patient groups reported that TB physicians and staff advised patients to inform and to bring their household contacts in for TB screening. However, they did not instruct patients to inform or to bring in non-household contacts at school or in the workplace for TB investigations. None of the non-TB patient groups had ever received TB training or TB education. By contrast, there were several educational programmes on HIV infection in schools and workplaces. Participants from pre-schools, kindergartens and boarding schools reported that they had received sufficient information and guidance about hand, foot and mouth disease, but they had never learned about TB. There were no school guidelines for infection control. As a result, the schools do not know how to manage a student or teacher with TB.
Informing non-household contacts about tuberculosis
Almost all former TB patients immediately informed their household contacts about TB, most of whom underwent TB screening. However, one physician, who could not cope with TB stigma, informed his family 1 week later. By contrast, the former TB patients did not inform or minimally informed their non-household contacts about their illness. For example, none of the teachers who were former TB patients informed their students about their TB. When some students asked one teacher why she put on a mask, she only said that she did not feel well. All teachers informed their supervisors about TB as they were allowed a 2-week sick leave. Only one teacher informed her colleagues sharing the same office that she had TB and stopped having lunch with them. As all her colleagues had just undergone CXR during the annual health check-up, none of them underwent TB screening. The remaining two teachers did not inform their colleagues, fearing TB stigma. None of the students who were former TB patients informed their classmates about their TB, as they feared being shunned by friends.
The five non-TB groups were asked a hypothetical question about whether they would inform non-household contacts if they had TB. The common and immediate response from almost all the groups was ‘no’, accompanied by shaking of heads, except for the pre-school FGD session, which ended in a lack of consensus. Although approximately half of the participants stated that they would not inform non-household contacts about their TB, the other half argued that they should inform non-household contacts to prevent other people from contracting TB.
To increase the acceptance of contact investigation in non-household settings such as schools and workplaces, participants suggested that health systems should consider the following strategies to overcome stigma: avoid naming TB patients to protect confidentiality, offering peer education at the workplace and organising meetings with students, teachers and parents to educate them about TB.
The best way is to have a doctor in a meeting with parents and explain to them about the need for TB screening in children who contract TB. Doctors should make parents understand TB and accept to live with children with TB. Parents should not shun children with TB and withdraw their children from school. (Kindergarten FGD: a director, female participant #1)
DISCUSSION
To our knowledge, this is the first qualitative study of TB from a high-burden country to explore non-household contact investigation from the perspective of former TB patients and professionals from congregate settings. To ensure theoretical sensitivity, consistency of data collection and of data analysis, the same moderator conducted all FGDs.15 Despite efforts to ensure the trustworthiness of qualitative research, some limitations prevail. By strictly adhering to ethical research guidelines, the participants are free to decline participation in research without providing a justification. The reasons why some invited former TB patients and selected organisations declined to participate in the research thus remain unknown. The study cannot therefore identify whether those who declined to participate have different opinions on TB, specifically concerning stigma, or differing experience with non-household contacts.
The current study has three important implications for non-household contact investigation and TB control in Thailand. First, former TB patients who are teachers, students and health workers are highly exposed to contacts at school and in the hospital, but contact investigations were limited to household contacts. Annual health check-ups contributed to the early detection of active TB in teachers, which can reduce the duration of TB transmission in the school. Second, stigma against TB is generally high due to fear of infection. Stigma may be a major barrier to investigation among non-household contacts because TB patients tend to withhold their diagnosis from their colleagues or may not provide actual information about non-household contacts to health staff. However, experiencing less stigma and concern for other people’s health motivated TB patients to inform their non-household contacts. Third, the lack of knowledge about TB and misconceptions about TB transmission led to the experience of felt and enacted stigma. Using the internet to search for information about TB is highly prevalent, but the reliability of such information is uncertain.
Health workers can both be exposed to and transmit TB in the hospital. A recent systematic review and meta-analysis on TB transmission from health workers to patients and other colleagues reveals that health workers with TB have lower TB transmission to their contacts than TB transmission by non-health worker index cases in households, schools and congregate and community settings.16 However, all studies were performed in high-income and low TB burden countries, namely, the United States, the United Kingdom and France. The risk of TB transmission from health workers to contacts in this study may not be comparable to those reported previously. The study hospital provides daily out-patient services to 800–1000 clients. Each in-patient ward has 30 beds, which are always fully occupied, and sometimes an additional 20–30 beds are used. Contact investigation in the current hospital would be complicated due to overcrowding. Furthermore, inadequate isolation rooms for TB patients is a common problem in Thailand.17 Measures to prevent nosocomial TB transmission should be strictly implemented. Health workers with active TB should adhere to anti-tuberculosis treatment, and staff contacts should undergo TB screening. The occupational health programme should ensure that the coverage of annual CXR, particularly among doctors and nurses working with patients who are at high risk of contracting TB such as those working in the neonatal unit, the HIV clinic and the dialysis unit.10,11
Although one study reported that annual CXR for the Thai population is not cost-effective,18 our study shows that annual health check-ups contributed to the early detection of active TB in teachers. Our study findings highlight the need to promote CXR among health care workers and kindergarten and nursery school teachers who work closely with high-risk groups.10 Newly recruited staff should submit health check results as proof of being free from communicable diseases such as TB before starting work in congregate settings.
Parents are often concerned about temperature rather than air quality in the classroom.19 Teachers and parents both cited high temperature as the main reason for installing air conditioning in kindergarten and pre-schools. Given the enclosed environment, spending long hours in air-conditioned rooms is likely to increase the risk of TB transmission to contacts if the teacher or one of the students have active TB. Boarding schools are particularly high-risk due to overcrowding and longer periods of contact.20 To enhance ventilation in classrooms and dormitories, schools should follow a regular schedule for cleaning and maintenance of all air conditioning units. Furthermore, daily opening of windows and doors for natural ventilation and exposure to sunlight can reduce the number of airborne particles, including TB droplet nuclei.21 Teachers and students should practice cough etiquette and promote the use of face masks in case of respiratory symptoms.
Stigma against TB is one of the barriers to global TB elimination.22 Stigma leads to delay in health-seeking behaviour for TB diagnosis,23 and non-adherence to anti-tuberculosis treatment24 and hinders contact investigation. This study shows that both types of stigma exist, i.e., enacted stigma (actual discrimination) and felt stigma (fearing to be discriminated).25 Although several of our findings are consistent with findings from previous international and Thai studies, some differences were observed. For example, health workers in South Africa refused to undergo TB screening provided by occupational health units, fearing that other health staff would be informed of their diagnosis and that they would be stigmatised.26 In contrast, this study found no stigma reactions from contacts of health staff. A study in Thailand reported that a TB outbreak investigation in a high school was delayed due to a disagreement with the TB patient’s mother.27 The mother would not allow her son to take leave from school and prohibited him from wearing a mask in the classroom. She defended her position stating that she was afraid of other students’ attitudes towards him should they find out he had TB. TB stigma negatively affects both student patients and their parents. Parents taking care of their high school children with active TB were observed to lack knowledge about TB, experienced psychological stress and be negatively impacted by their child’s TB. Stigma resulted in self-isolation and loss of assistance from their relatives.28 Several studies report TB transmission in schools by teachers, but there are no reports about TB stigma in teachers.12,29 Our results show that there is a risk of transmission in schools because employees and students hide their TB diagnosis from students, parents and teachers or colleagues. To remedy this situation, some studies report that effective training and communication can reduce stigma in health workers30 and in the general population.31 To enhance contact investigation among non-household contacts, TB clinic staff and public health workers involved in TB outbreak investigations should receive training to improve their interview skills. This could help them to adequately convey the importance of disclosing a TB diagnosis to non-household contacts to avoid transmitting the disease.32
This study confirms previous findings that a lack of knowledge about TB and misconceptions of TB transmission are common in teachers, parents and industry workers.27,33 Using the internet as a resource to access knowledge about TB was prevalent. However, when we used internet search engines such as Google and type ‘TB’ (wanna rok in Thai), the top 10 websites that appear concern private businesses and hospitals. It is a challenge to make reliable and culturally sensitive TB information, provided by the National TB Programme or from academic institutions, available on the first page of search results. Because most people concerned with TB use internet searches to acquire information, it would be desirable that the information available should not only highlight clinical information on TB but also provide strategies and knowledge for reducing stigma against TB.
Although this study mostly examines the barriers to contact investigation in non-household settings, some facilitators to overcome the barriers were also found. Notably, one of the parents in this study entirely changed his attitude concerning the risks of TB transmission after understanding that TB patients are not identifiable by sight and that it is possible to be unknowingly exposed to TB. This message could possibly reduce stigma against TB patients. This study discovered a category of ‘empathy’, indicating that although stigma was experienced in the pre-school group, half of the participants felt strongly about the need to inform their contacts in pre-schools about their TB. They empathised with children or colleagues who developed TB from them. Several studies refer to empathy as an important concept for training nurses and health care professionals.34,36 Training health staff about empathy plays a role in reducing TB stigma among health workers.35 TB education programme should integrate the notion of empathy into TB education for TB patients and the general public.
Acknowledgments
The study is a part of the research project entitled, ‘Development of an operations manual and tools for enhancing the coverage of TB contact investigations and reducing their social burden and stigma’, funded by Thailand Health System Research Institute (HSRI; Nonthaburi, Thailand; grant number HSRI60-033). The authors thank all participants for their active participation in the study and the anonymous reviewers for their critical review and helpful comments.
Footnotes
Conflicts of interest: none declared.
References
- 1.Tangcharoensathien V, Limwattananon S, Patcharanarumol W, Thammatacharee J, Jongudomsuk P, Sirilak S. Achieving universal health coverage goals in Thailand: the vital role of strategic purchasing. Health Policy Plan. 2015;30:1152–1161. doi: 10.1093/heapol/czu120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Global tuberculosis report, 2017. Geneva, Switzerland: WHO; 2017. WHO/HTM/TB/2017.23. [Google Scholar]
- 3.World Health Organization Systematic screening for active tuberculosis: an operational guide. Geneva, Switzerland: WHO; 2015. WHO/HTM/TB/2015.16. [Google Scholar]
- 4.Hwang T J, Ottmani S, Uplekar M. A rapid assessment of prevailing policies on tuberculosis contact investigation. Int J Tuberc Lung Dis. 2011;15:1620–1623. doi: 10.5588/ijtld.11.0222. [DOI] [PubMed] [Google Scholar]
- 5.Chiang S S, Roche S, Contreras C et al. Barriers to the diagnosis of childhood tuberculosis: a qualitative study. Int J Tuberc Lung Dis. 2015;19:1144–1152. doi: 10.5588/ijtld.15.0178. [DOI] [PubMed] [Google Scholar]
- 6.Faccini M, Cantoni S, Ciconali G et al. Tuberculosis-related stigma leading to an incomplete contact investigation in a low-incidence country. Epidemiol Infect. 2015;143:2841–2848. doi: 10.1017/S095026881400394X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox G J, Loan le P, Nhung N V et al. Barriers to adherence with tuberculosis contact investigation in six provinces of Viet Nam: a nested case-control study. BMC Infect Dis. 2015;15:103. doi: 10.1186/s12879-015-0816-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tlale B L, Masupe T, Molefi M, Tshikuka J G. Knowledge, attitudes and practices of health care workers’ towards tuberculosis contact tracing in a TB/HIV prevalent setting. Int J Int Med Res. 2015;2:16–22. [Google Scholar]
- 9.Davidow A L, Mangura B T, Wolman M S et al. Workplace contact investigations in the United States. Int J Tuberc Lung Dis. 2003;7(Suppl 3):S446–S452. [PubMed] [Google Scholar]
- 10.Drobniewski F A, Ferguson J, Barritt K et al. Follow up of an immunocompromised contact group of a case of open pulmonary tuberculosis on a renal unit. Thorax. 1995;50:863–868. doi: 10.1136/thx.50.8.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC) Mycobacterium tuberculosis transmission in a newborn nursery and maternity ward—New York City, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:1280–1283. [PubMed] [Google Scholar]
- 12.Roberts J R, Mason B W, Paranjothy S, Palmer S R. The transmission of tuberculosis in schools involving children 3 to 11 years of age. Pediatr Infect Dis J. 2012;31:82–84. doi: 10.1097/INF.0b013e31823378c9. [DOI] [PubMed] [Google Scholar]
- 13.Krueger R A. Focus group: a practical guide for applied research. 2nd ed. Newbury Park, CA, USA: Sage Publications; 1994. [Google Scholar]
- 14.Strauss A, Corbin J. Basic of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA, USA: Sage; 1998. [Google Scholar]
- 15.Cresswell J W. Qualitative inquiry and research design: choosing among five traditions. Thousand Oaks, CA, USA: Sage; 1998. [Google Scholar]
- 16.Schepisi M S, Sotgiu G, Contini S, Puro V, Ippolito G, Girardi E. Tuberculosis transmission from healthcare workers to patients and co-workers: a systematic literature review and meta-analysis. PLOS ONE. 2015;10 doi: 10.1371/journal.pone.0121639. e0121639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unahalekhaka A, Lueang-a-papong S, Chitreecheur J. Status of nosocomial tuberculosis transmission prevention in hospitals in Thailand. Am J Infect Control. 2014;42:340–343. doi: 10.1016/j.ajic.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 18.Srisuwan P, Koopitakkajorn T, Kingkaew P, Youngkong S, Tantivess S, Teerawattananon S. Population-based screening for tuberculosis in Thailand. J Health Syst Res. 2013;7:433–439. [Google Scholar]
- 19.Fisk W J. The ventilation problem in schools: literature review. Indoor Air. 2017;27:1039–1051. doi: 10.1111/ina.12403. [DOI] [PubMed] [Google Scholar]
- 20.Stein-Zamir C, Volovik I, Rishpon S, Atamna A, Lavy A, Weiler-Ravell D. Tuberculosis outbreak among students in a boarding school. Eur Respir J. 2006;28:986–991. doi: 10.1183/09031936.06.00002506. [DOI] [PubMed] [Google Scholar]
- 21.Curry International Tuberculosis Center Tuberculosis infection control: a practical manual for preventing TB. San Francisco, CA, USA: Curry International Tuberculosis Center; 2011. www.currytbcenter.ucsf.edu/sites/default/files/ic_book_2011.pdf Accessed February 2019. [Google Scholar]
- 22.Jaramillo E, Sahu S, Van Weezenbeek C. Ending TB-related stigma and discrimination. Int J Tuberc Lung Dis. 2017;21:2–3. doi: 10.5588/ijtld.17.0229. [DOI] [PubMed] [Google Scholar]
- 23.Skinner D, Claassens M. It’s complicated: why do tuberculosis patients not initiate or stay adherent to treatment? A qualitative study from South Africa. BMC Infect Dis. 2016;16:712. doi: 10.1186/s12879-016-2054-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Munro S A, Lewin S A, Smith H J, Engel M E, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLOS Med. 2007;4:e238. doi: 10.1371/journal.pmed.0040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scambler G. Stigma and disease: changing paradigms. Lancet. 1998;352:1054–1055. doi: 10.1016/S0140-6736(98)08068-4. [DOI] [PubMed] [Google Scholar]
- 26.Sommerland N, Wouters E, Mitchell E M H et al. Evidence-based interventions to reduce tuberculosis stigma: a systematic review. Int J Tuberc Lung Dis. 2017;21:81–86. doi: 10.5588/ijtld.16.0788. [DOI] [PubMed] [Google Scholar]
- 27.Poopakdee N. Tuberculosis contact investigation among students of a high school in Yanyao sub-district, Sawankhalok district, Sukhothai Province between 14 September–22 December 2011. Wkly Epidemiol Surveill Rep. 2013;44:S57–S63. [Thai] [Google Scholar]
- 28.Zhang S, Ruan W, Li Y, Wang X, Wang X. Experiences of the parents caring for their children during a tuberculosis outbreak in high school: a qualitative study. BMC Public Health. 2014;14:132. doi: 10.1186/1471-2458-14-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Filia A, Ciarrocchi G, Belfiglio R et al. Tuberculosis in kindergarten and primary school, Italy, 2008–2009. Emerg Infect Dis. 2011;17:514–516. doi: 10.3201/eid1703.101440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu P S, Chou P, Chang N T, Sun W J, Kuo H S. Assessment of changes in knowledge and stigmatisation following tuberculosis training workshops in taiwan. J Formos Med Assoc. 2009;108:377–385. doi: 10.1016/S0929-6646(09)60081-4. [DOI] [PubMed] [Google Scholar]
- 31.Waisbord S. Beyond the medical-informational model: recasting the role of communication in tuberculosis control. Soc Sci Med. 2007;65:2130–2134. doi: 10.1016/j.socscimed.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 32.Shrestha-Kuwahara R, Wilce M, DeLuca N, Taylor Z. Factors associated with identifying tuberculosis contacts. Int J Tuberc Lung Dis. 2003;7(Suppl 3):S510–S516. [PubMed] [Google Scholar]
- 33.Upshur R E, Deadman L, Howorth P et al. The effect of tuberculosis and tuberculosis contact tracing on school function: an Exploratory Focus Group Study. Can J Public Health. 1999;90:389–391. doi: 10.1007/BF03404141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thu A, Ohnmar, Win H, Nyunt M T, Lwin T. Knowledge, attitudes and practice concerning tuberculosis in a growing industrialised area in Myanmar. Int J Tuberc Lung Dis. 2012;16:330–335. doi: 10.5588/ijtld.10.0754. [DOI] [PubMed] [Google Scholar]
- 35.Singer T, Klimecki O M. Empathy and compassion. Curr Biol. 2014;24:R875–R878. doi: 10.1016/j.cub.2014.06.054. [DOI] [PubMed] [Google Scholar]
- 36.Tadesse S. Stigma against tuberculosis patients in Addis Ababa, Ethiopia. PLOS ONE. 2016;11 doi: 10.1371/journal.pone.0152900. e0152900. [DOI] [PMC free article] [PubMed] [Google Scholar]


