Abstract
Background
Over a 14‐year period, age‐adjusted high total cholesterol (≥240 mg/dL) in the United States declined from 18.3% in 1999 to 2000 to 11.0% in 2013 to 2014, coinciding with the 2001 National Cholesterol Education Program Adult Treatment Panel (ATP)‐III guidelines that endorsed low‐density lipoprotein (LDL)‐cholesterol blood value goals. Statin treatment recommendations were revised by the American College of Cardiology and the American Heart Association (ACC/AHA) in November 2013 to a “risk‐based prescription” approach that did not utilize blood cholesterol values. This increased dosage and expanded the statin‐eligible population by an estimated 12.8 million US adults. These changes should further lower total and LDL cholesterol concentrations nationally.
Methods
We examined data from 507 752 patients nationally aged ≥16 years whose fasting bloods were sent to Boston Heart Diagnostics for direct LDL‐cholesterol measurements. Between 2012 and 2017, age‐adjusted concentrations were examined by analysis of covariance and LDL‐cholesterol ≥160 mg/dL by logistic regression.
Results
Contrary to expectations, age‐adjusted mean LDL‐cholesterol concentrations (±SE, mg/dL) increased significantly (P < 10−16) in men (2012:113.8 ± 0.3; 2013:115.3 ± 0.2; 2014:114.7 ± 0.2; 2015:116.0 ± 0.2; 2016:117.6 ± 0.2; and 2017:117.1 ± 0.2 mg/dL) and women (2012:119.5 ± 0.3; 2013:120.7 ± 0.2; 2014:119.8 ± 0.02; 2015:120.8 ± 0.2; 2016:122.7 ± 0.1; and 2017:123.8 ± 0.2 mg/dL). The percentage with LDL‐cholesterol ≥160 mg/dL also increased significantly (P < 10−9) in men and women. Similar results were obtained for ages 40 to 75 years olds (corresponding to ACC/AHA guidelines).
Conclusion
These results provide additional evidence that declining blood LDL‐cholesterol levels observed following the ATP‐III recommendations, did not further decline (actually increased) following the 2013 ACC/AHA recommendations.
Keywords: cholesterol, guidelines, heart disease prevention, low density lipoprotein cholesterol
1. INTRODUCTION
In 2001, the National Cholesterol Education Program Adult Treatment Panel (ATP)‐III guidelines provided a comprehensive guide to lipid management, namely, the use of drug therapy in persons with coronary heart disease (CHD) or CHD risk equivalents (10 year risk >20%) to obtain a low‐density lipoprotein (LDL)‐cholesterol goal <100 mg/dL (2.59 mmol/L), considered optimal for primary prevention and <70 mg/dL (1.81 mmol/L) for secondary prevention.1 In patients with two or more risk factors and moderate 10‐year CHD risk (10%‐20%) the proposed goal was <130 mg/dL, and for those with a <10% risk or zero or one risk factor the proposed goal was <160 mg/dL). In 2004, the guidelines were updated to recommend treatment an option for achieving LDL‐cholesterol <70 mg/dL in very high‐risk patients as defined by the Framingham 10‐year CHD risk equation for fatal CHD and nonfatal myocardial infarction.2 These recommendations likely contributed strongly to the increase in use of antihyperlipidemic agents in the United States from 6.5% in 1999 to 2002 to 14.3% in 2011 to 2014.3 This increase coincided with a decline in the percent of the US adult population with total cholesterol ≥240 mg/dL of 18.3% in 1999 to 2000 to 11.0% by 2013 to 2014,4 and a decline in the age adjusted death rate due to heart disease from 257.6 to 167.0 per 100 000 population between 2000 and 2014.4 Data from nearly 105 million adults show that mean LDL‐cholesterol levels declined from 120 mg/dL in 2001 to 105 mg/dL in 2008, plateauing thereafter through 2011.5
In November 2013, the American College of Cardiology (ACC) and the American Heart Association (AHA) changed statin recommendations from a “titration to cholesterol goal” to a “risk benefit”‐based approach with reduced emphasis on individual blood LDL‐cholesterol values as a goal of treatment.6 The recommendations were based exclusively on evidence of statin benefit from randomized controlled trials. Specifically, statin treatment was recommended for adult patients with: (a) atherosclerotic cardiovascular disease (ASCVD); (b) LDL‐cholesterol ≥190 mg/dL, (c) diabetes between the ages of 40 and 75 years and LDL‐cholesterol between 70 and 189 mg/dL; and (d) 7.5% or greater 10‐year ASCVD risk and LDL‐cholesterol between 70 and 189.6 Low‐intensity statin therapy (expected LDL‐cholesterol lowering <30%) was only recommended for patients who did not tolerate higher intensity statin therapy. Moderate intensity statins (expected LDL‐C lowering of 30% to 50%) was generally recommended for primary prevention in subjects with LDL‐cholesterol <190 mg/dL. High intensity statins (expected LDL‐C lowering ≥50%) was recommended for patients aged 75 and younger with ASCVD or LDL‐cholesterol ≥190 mg/dL without safety concerns, and could be considered for individuals with or without diabetes who had a 10‐year ASCVD risk ≥7.5%. Additional factors that may suggest statin therapy include family history of premature ASCVD, lifetime ASCVD risk, an abnormal coronary artery calcium (CAC) or ankle‐brachial index (ABI) score, or elevated high‐sensitivity C‐reactive protein concentrations.6 New to the 2013 ACC/AHA guidelines is the concept of shared decision making between the physician and patient.
The new guideline substantially increased the number of US adults to whom moderate‐ or intense‐statin therapy was indicated. Approximately 33 million people have a high 10‐year ASCVD risk that would qualify them for a high‐intensity statin therapy, and an additional 13 million people have a moderate risk for which statins could be considered.6, 7 Based on the National Health and Nutrition Examination Survey (NHANES) data from 2005 to 2010, an additional 12.8 million people over the previous recommendation would be eligible for statin therapy, with the increase seen mostly among older adults without cardiovascular disease.8 Thus, almost one‐half (56 million) of all people in the United States between the ages of 40 and 75 years without cardiovascular disease became eligible for therapy.8 It is estimated that as many as 475 000 future cardiovascular events could be prevented if statins were assigned to all those who exceeded the ≥7.5% cutoff in 10‐year ASCVD risk in the 40 to 75 years range.8
Several reports on statin prescriptions (behavioral change3, 9, 10, 11) and total or LDL‐cholesterol (physiological responses to the behavioral change3, 4) trends proximal to the ACC/AHA guideline release suggest the recommendations have had less impact than anticipated. Although improved LDL‐cholesterol levels are no longer the clinical goal following the “treat to ASCVD risk” from the “treat to LDL‐cholesterol target” paradigm change, the substantial expansion of the eligible population and shift to moderate‐ and high‐intensity statin therapy should have reduced LDL‐cholesterol concentrations nationally. This should be especially true for newly eligible patients who were heretofore untargeted in the ATP‐III treatment guidelines. However, an important limitation of these and earlier analyses of LDL trends that could affect their sensitivity to change include: (a) uncertainty on whether blood was collected in the fasting state,5, 12 and (b) use of the Friedewald equation to estimate LDL‐cholesterol, which is subject to inaccuracy in the presence of high triglycerides and other conditions. In addition, previously reported trends in statin prescriptions11 and LDL levels include only a year or two of post‐guideline data which could miss delayed acceptance.
We therefore analyzed direct measurements of LDL‐cholesterol levels from 507 752 fasting patients obtained nationally in a large anonymized clinical laboratory data set between 2012 and 2017, to test whether LDL‐cholesterol dropped following the 2013 recommendation for wider, more intense statin therapy.
2. METHODS
The analyses of this report were performed in a large anonymized clinical laboratory (Boston Heart Diagnostics, Framingham, Massachusetts). Due to the anonymized nature of the data analysis, no individual informed consent was required. Initial first visit fasting blood samples from 507 752 patients were measured for LDL‐cholesterol between January 1, 2012 and October 31, 2017 from 50 states and the District of Columbia. The observations were confirmed using the first and second follow‐up patient samples for analysis. This population sample reflects patients likely assessed for CVD risk and may not reflect the general population.
Age, gender, height, and weight were obtained from the sample submission form. Total cholesterol and LDL‐cholesterol were run at the time of collection in a College of American Pathologist (CAP) and Clinical Laboratory Improvement Amendments (CLIA) accredited laboratory (Boston Heart Diagnostics, Framingham, Massachusetts). Enzymatic colorimetric analyses were used for the measurement of total cholesterol and triglycerides13 and direct measurement of LDL‐cholesterol,14 and immunoturbidimetric analyses for apo B concentrations Indirect LDL‐cholesterol was obtained from the Friedewald equation: total cholesterol ‐triglycerides/5 for triglycerides ≤400 mg/dL and direct LDL‐cholesterol for triglycerides >400.15
2.1. Statistical analyses
Statistical analyses were performed using JMP version 13.2 (SAS Institute, Cary, North Carolina). Mean concentrations and percentages by categories are presented with their SE (±SE). The effects of time since January 1, 2012 as a continuous variable (fraction of years) were determined by regression analysis with or without adjustment for age. Analysis of covariance was used to estimate the average age‐adjusted total and LDL‐cholesterol concentrations by year with or without adjustment. Logistic regression analyses was used to estimate trends for the percent of the sample having borderline to high (≥200 mg/dL) and high total cholesterol (≥240 mg/dL), and borderline to very‐high (≥130 mg/dL), high to very‐high (≥160 mg/dL), and very‐high LDL‐cholesterol (≥190 mg/dL) with and without adjustment for age. Results are presented for patients' first (denoted as baseline), second (1st follow‐up), and third cholesterol samples (2nd follow‐up).
3. RESULTS
Table 1 displays the sample characteristics. The proportion of males and average age decreased over time, suggesting a declining prevalence of higher risk individuals in later years. Table 1 shows that the significant decrease in baseline age was primarily because of its decline between 2012 and 2015.
Table 1.
Fasting low‐density lipoprotein (LDL) cholesterol concentrations (mg/dL) by year
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Trend (P) | |
|---|---|---|---|---|---|---|---|
| Baseline Sample | |||||||
| Female (N) | 15 970 | 35 716 | 47 294 | 61 504 | 78 936 | 41 620 | — |
| Male (N) | 16 370 | 32 631 | 38 933 | 48 313 | 60 957 | 29 508 | — |
| Male (%) | 50.6 | 47.7 | 45.2 | 44.0 | 43.6 | 41.5 | — |
| Age (years) | |||||||
| Female | 59.3 ± 0.1 | 57.3 ± 0.1 | 55.6 ± 0.1 | 54.5 ± 0.1 | 54.3 ± 0.1 | 54.4 ± 0.1 | <10−16 |
| Male | 58.3 ± 0.1 | 56.4 ± 0.1 | 55.5 ± 0.1 | 55.4 ± 0.1 | 55.1 ± 0.1 | 55.5 ± 0.1 | <10−16 |
| Mean LDL‐cholesterol (mg/dL) | |||||||
| Female | 119.8 ± 0.3 | 120.8 ± 0.2 | 119.8 ± 0.2 | 120.8 ± 0.2 | 122.7 ± 0.1 | 123.7 ± 0.2 | <10−16 |
| Male | 112.1 ± 0.3 | 114.8 ± 0.2 | 114.9 ± 0.2 | 116.2 ± 0.2 | 118.0 ± 0.2 | 117.3 ± 0.2 | <10−16 |
| Age‐adjusted LDL‐cholesterol (mg/dL) | |||||||
| Female | 119.5 ± 0.3 | 120.7 ± 0.2 | 119.8 ± 0.2 | 120.8 ± 0.2 | 122.7 ± 0.1 | 123.8 ± 0.2 | <10−16 |
| Male | 113.8 ± 0.3 | 115.3 ± 0.2 | 114.7 ± 0.2 | 116.0 ± 0.2 | 117.6 ± 0.2 | 117.1 ± 0.2 | <10−16 |
| Borderline to very‐high LDL (%) | |||||||
| Female | 36.2 ± 0.4 | 37.5 ± 0.3 | 36.7 ± 0.2 | 37.3 ± 0.2 | 39.0 ± 0.2 | 40.6 ± 0.2 | <10−16 |
| Male | 30.3 ± 0.4 | 32.7 ± 0.3 | 33.2 ± 0.2 | 34.5 ± 0.2 | 36.7 ± 0.2 | 35.7 ± 0.3 | <10−16 |
| High to very‐high LDL (%) | |||||||
| Female | 14.9 ± 0.3 | 15.4 ± 0.2 | 14.6 ± 0.2 | 14.8 ± 0.1 | 16.2 ± 0.1 | 16.9 ± 0.2 | 5.5x10−10 |
| Male | 11.5 ± 0.2 | 12.6 ± 0.2 | 12.5 ± 0.2 | 13.4 ± 0.2 | 14.9 ± 0.1 | 14.8 ± 0.2 | <10−16 |
| Very‐high LDL (%) | |||||||
| Female | 5.2 ± 0.2 | 5.2 ± 0.1 | 4.6 ± 0.1 | 4.7 ± 0.1 | 5.5 ± 0.1 | 5.6 ± 0.1 | 1.3x10−11 |
| Male | 3.2 ± 0.1 | 3.5 ± 0.1 | 3.5 ± 0.1 | 4.0 ± 0.1 | 4.6 ± 0.1 | 4.8 ± 0.1 | <10−16 |
| 1st follow‐up sample (N) | |||||||
| Female (N) | 3437 | 6418 | 12 423 | 15 937 | 21 783 | 15 798 | |
| Male (N) | 3552 | 6454 | 11 633 | 13 064 | 18 747 | 13 283 | |
| Male (%) | 50.8 | 50.1 | 48.4 | 45.0 | 46.3 | 45.7 | |
| Age (years) | |||||||
| Female | 64.1 ± 0.2 | 61.2 ± 0.2 | 60.1 ± 0.1 | 59.0 ± 0.1 | 58.6 ± 0.1 | 58.9 ± 0.1 | <10−16 |
| Male | 62.3 ± 0.2 | 60.1 ± 0.2 | 58.9 ± 0.1 | 58.7 ± 0.1 | 58.9 ± 0.1 | 59.0 ± 0.1 | <10−16 |
| Mean LDL‐cholesterol (mg/dL) | |||||||
| Female | 107 ± 0.6 | 110.6 ± 0.5 | 110.5 ± 0.3 | 114.4 ± 0.3 | 116.3 ± 0.3 | 116.4 ± 0.3 | <10−16 |
| Male | 97.8 ± 0.6 | 101.7 ± 0.4 | 103.1 ± 0.3 | 105.5 ± 0.3 | 105.6 ± 0.3 | 107.3 ± 0.3 | <10−16 |
| Age‐adjusted LDL‐cholesterol (mg/dL) | |||||||
| Female | 108.1 ± 0.7 | 111 ± 0.5 | 110.6 ± 0.3 | 114.3 ± 0.3 | 116.1 ± 0.3 | 116.3 ± 0.3 | <10−16 |
| Male | 100.1 ± 0.6 | 102.4 ± 0.5 | 102.9 ± 0.3 | 105.2 ± 0.3 | 105.4 ± 0.3 | 107.2 ± 0.3 | <10−16 |
| Borderline to very‐high LDL (%) | |||||||
| Female | 23.5 ± 0.7 | 27.9 ± 0.6 | 27.7 ± 0.4 | 31.5 ± 0.4 | 33.5 ± 0.3 | 33.8 ± 0.4 | <10−16 |
| Male | 16.9 ± 0.6 | 20.3 ± 0.5 | 22.1 ± 0.4 | 24.6 ± 0.4 | 25.6 ± 0.3 | 27.3 ± 0.4 | <10−16 |
| High to very‐high LDL (%) | |||||||
| Female | 9.3 ± 0.5 | 10.5 ± 0.4 | 10.7 ± 0.3 | 12.0 ± 0.3 | 13.1 ± 0.2 | 13.0 ± 0.3 | <10−16 |
| Male | 5.6 ± 0.4 | 6.8 ± 0.3 | 7.0 ± 0.2 | 8.6 ± 0.2 | 9.5 ± 0.2 | 10.0 ± 0.3 | <10−16 |
| Very‐high LDL (%) | |||||||
| Female | 3.2 ± 0.3 | 3.3 ± 0.2 | 3.2 ± 0.2 | 3.5 ± 0.1 | 4.3 ± 0.1 | 4.1 ± 0.2 | 2.2 × 10−9 |
| Male | 1.5 ± 0.2 | 1.7 ± 0.2 | 2.0 ± 0.1 | 2.2 ± 0.1 | 2.6 ± 0.1 | 2.9 ± 0.1 | 1.6 × 10−14 |
| 2nd follow‐up sample (N) | |||||||
| Female (N) | 966 | 1951 | 4424 | 7135 | 9035 | 8470 | — |
| Male (N) | 990 | 2045 | 4375 | 6151 | 7808 | 7575 | — |
| Male (%) | 50.6 | 51.2 | 49.7 | 46.3 | 46.4 | 47.2 | — |
| Age (years) | |||||||
| Female | 65.0 ± 0.4 | 63.8 ± 0.3 | 61.9 ± 0.2 | 62.0 ± 0.2 | 61.0 ± 0.1 | 61.4 ± 0.1 | <10−16 |
| Male | 63.4 ± 0.4 | 62.5 ± 0.3 | 60.3 ± 0.2 | 60.9 ± 0.2 | 61.2 ± 0.1 | 61.3 ± 0.2 | 0.008 |
| Mean LDL‐cholesterol (mg/dL) | |||||||
| Female | 104.1 ± 1.2 | 103.4 ± 0.8 | 106.8 ± 0.6 | 108.6 ± 0.4 | 113.4 ± 0.4 | 112.9 ± 0.4 | <10−16 |
| Male | 94.3 ± 1.0 | 95.4 ± 0.7 | 98.6 ± 0.5 | 99.4 ± 0.5 | 101.7 ± 0.4 | 99.7 ± 0.4 | 1.5 × 10−12 |
| Age‐adjusted mean LDL‐cholesterol (mg/dL) | |||||||
| Female | 105.1 ± 1.2 | 104.0 ± 0.9 | 106.8 ± 0.6 | 108.7 ± 0.5 | 113.2 ± 0.4 | 112.8 ± 0.4 | <10−16 |
| Male | 95.9 ± 1.1 | 96.4 ± 0.8 | 98.0 ± 0.5 | 99.2 ± 0.5 | 101.7 ± 0.4 | 99.7 ± 0.4 | 1.5 × 10−12 |
| Borderline to very‐high LDL (%) | |||||||
| Female | 21.2 ± 1.3 | 20.4 ± 0.9 | 23.8 ± 0.6 | 26.4 ± 0.5 | 31.5 ± 0.5 | 30.8 ± 0.5 | <10−16 |
| Male | 13.2 ± 1.1 | 15.0 ± 0.8 | 18.7 ± 0.6 | 19.5 ± 0.5 | 22.1 ± 0.5 | 21.4 ± 0.5 | <10−16 |
| High to very‐high LDL (%) | |||||||
| Female | 8.2 ± 0.9 | 7.9 ± 0.6 | 9.1 ± 0.4 | 9.6 ± 0.3 | 11.7 ± 0.3 | 11.9 ± 0.4 | <10−16 |
| Male | 4.5 ± 0.7 | 4.5 ± 0.5 | 5.7 ± 0.3 | 7.1 ± 0.3 | 8.3 ± 0.3 | 8.3 ± 0.3 | <10−16 |
| Very‐high LDL (%) | |||||||
| Female | 2.3 ± 0.5 | 2.5 ± 0.4 | 3.3 ± 0.3 | 3.0 ± 0.2 | 3.6 ± 0.2 | 4.0 ± 0.2 | 4.3 × 10−7 |
| Male | 0.7 ± 0.3 | 1.3 ± 0.3 | 1.3 ± 0.2 | 2.2 ± 0.2 | 2.4 ± 0.2 | 2.2 ± 0.2 | 2.5 × 10−6 |
Except for sample size, values are unadjusted and age‐adjusted mean ± SE for age and LDL cholesterol concentrations, and percentage ± SE for borderline to very‐high (≥120 mg/dL), high to very‐high (≥160 mg/dL) and very high‐LDL‐cholesterol (≥190 mg/dL).
Figure 1 shows that when adjusted for age, baseline fasting total cholesterol concentrations increased between 2012 and 2017 in women (slope ± SE: 0.32 ± 0.06 mg/dL annually, P = 3.8 × 10−8) but not in men (−0.06 ± 0.06, P = 0.32). However, logistic regression showed small annual increases in the age‐adjusted odds of high total cholesterol between 2012 and 2017 in both sexes (women: 1.8%, P = 5.7 × 10−7; men: 1.4%, P = 0.003).
Figure 1.
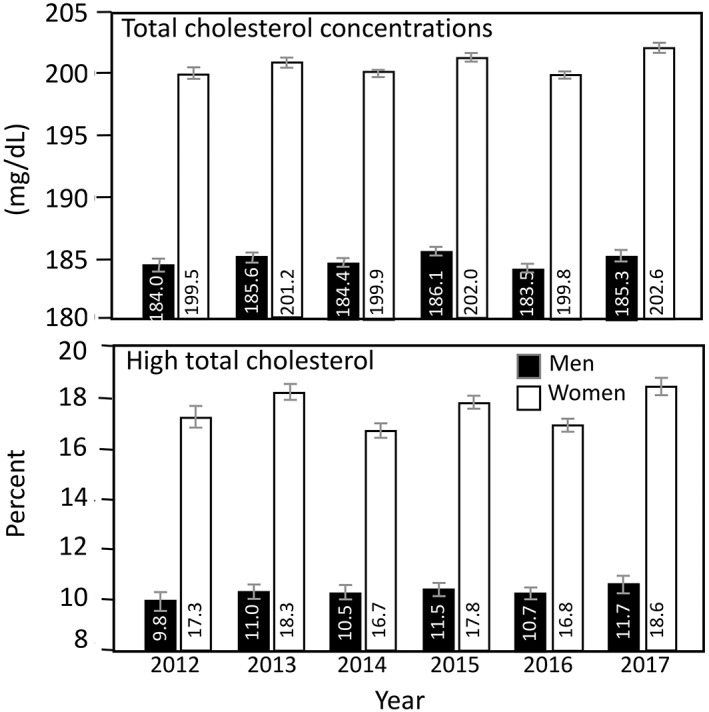
Analysis of covariance of the mean total cholesterol concentrations and the percent of subjects with high total cholesterol concentrations at baseline adjusted for age. Brackets represent 95% confidence intervals. Logistic regression analyses estimated that the odds of subjects with high total cholesterol increased by an average of per year in men and per year in women. All subjects were aged 16 years and older
Average fasting LDL‐cholesterol concentrations increased significantly from 2012 through 2017 (Table 1). Men's and women's baseline LDL‐cholesterol concentration increased annually by an average of 1.13 ± 0.06 and 0.97 ± 0.05 mg/dL, respectively. This was confirmed by average LDL‐cholesterol increases of 1.63 ± 0.10 and 2.05 ± 0.10 mg/dL per year on the men's and women's first follow‐up visit, respectively, and by 1.14 ± 0.16 and 2.53 ± 0.16 mg/dL per year, respectively, on their second follow‐up (P < 10−9). Adjustment for age had little effect on these trends: 0.84 ± 0.06 mg/dL per year in men and 1.03 ± 0.05 mg/dL in women at baseline, 1.34 ± 0.10 mg/dL per year in men and 1.87 ± 0.10 mg/dL in women at the 1st follow‐up, and 1.04 ± 0.16 mg/dL per year in men and 2.35 ± 0.16 mg/dL in women at the 2nd follow‐up (all P ≤ 10−10). Figure 2 shows that LDL‐cholesterol concentrations increased between 2012 and 2017 for men and women 40 and 75 years old (the age range specifically targeted by the ACC/AHA recommendations, males: 1.24 ± 0.06 mg/dL average increase per year P < 10−16; females: 1.41 ± 0.06 mg/dL average increase per year, P < 10−16), and men and women 60 and 75 years old (ie, the age group most directly affected by expanding eligibility by ASCVD risk, males: 1.24 ± 0.09 mg/dL average increase per year P < 10−16; females: 1.97 ± 0.09 mg/dL average increase per year, P < 10−16).
Figure 2.
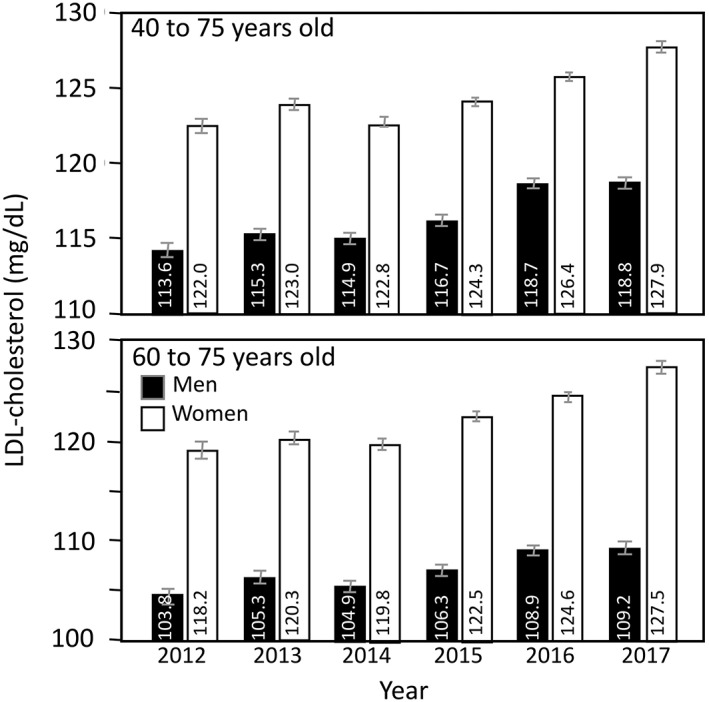
Mean low‐density lipoprotein cholesterol concentrations in adults 40 to 75 (the age range targeted by the ACC/AHA guidelines) and adults 60 to 74 years (the age range expected to be particularly impacted by the treat for risk approach of the ACC/AHA guidelines) at baseline adjusted for age
In addition, Table 1 shows that the proportion of the sample with LDL‐cholesterol ≥130 (borderline to very high), ≥160 (high to very high), and ≥ 190 mg/dL (very high LDL‐cholesterol) also increased significantly between 2012 and 2017 at baseline and during follow‐up. In men, each year after 2012 increased the age‐adjusted odds for borderline to very‐high LDL‐cholesterol by 4.6% (95% confidence interval [CI]: 4.0%‐5.3%, P < 10−16), for high to very‐high LDL‐cholesterol by 5.9% (95% CI: 5.1%‐6.9%, P < 10−16), and for very‐high LDL by 9.2% (95% CI: 7.6%‐10.8%, P < 10−16). The corresponding values for women were 4.7% (95% CI: 4.1%‐5.3%, P < 10−16), 4.8% (95% CI: 4.1%‐5.6%, P < 10−16), and 5.4% (95% CI: 4.1%‐6.6%, all P < 10−16).
Table 2 shows that the lack of an LDL‐decrease was also observed for calculated LDL, that is, showing no change or increased annually in men and women at baseline (regression slope ± SE, men: 0.09 ± 0.06, women: 0.09 ± 0.05 mg/dL per year), and first (men: 0.55 ± 0.10, women: 0.94 ± 0.10 mg/dL per year) and second follow‐up measurements (men: 0.30 ± 0.16, women: 1.38 ± 0.16 mg/dL per year) when adjusted for age. Age‐adjusted Non‐HDL‐cholesterol also showed no change or a slight increase over times. Despite the significant decreases in plasma triglyceride concentrations between 2012 and 2017, age‐adjusted apoB concentrations increased significantly over time for baseline (men: 0.81 ± 0.04, women: 0.88 ± 0.04 mg/dL per year) and first (men: 1.07 ± 0.07, women:1.35 ± 0.07 mg/dL per year), and second follow‐up measurements (men: 0.76 ± 0.12, women: 1.60 ± 0.12 mg/dL per year).
Table 2.
BMI, and fasting concentrations of total cholesterol, triglycerides, calculated low‐density lipoprotein (LDL) cholesterol concentrations, non‐HDL‐cholesterol, and apo B concentrations by year
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Trend (P) | |
|---|---|---|---|---|---|---|---|
| Baseline mean BMI (kg/m2) | |||||||
| Female | 29.89 ± 0.10 | 29.34 ± 0.07 | 28.89 ± 0.06 | 28.60 ± 0.05 | 28.78 ± 0.04 | 28.24 ± 0.06 | <10−16 |
| Male | 29.98 ± 0.08 | 30.12 ± 0.06 | 29.83 ± 0.05 | 29.65 ± 0.04 | 29.70 ± 0.04 | 29.37 ± 0.06 | <10−16 |
| Mean age‐adjusted BMI (kg/m2) | |||||||
| Female | 30.01 ± 0.10 | 29.39 ± 0.07 | 28.89 ± 0.06 | 28.57 ± 0.05 | 28.76 ± 0.04 | 28.23 ± 0.06 | <10−16 |
| Male | 30.14 ± 0.08 | 30.14 ± 0.06 | 29.80 ± 0.05 | 29.62 ± 0.04 | 29.68 ± 0.04 | 29.39 ± 0.06 | <10−16 |
| Mean total cholesterol (mg/dL) | |||||||
| Female | 200.5 ± 0.4 | 201.7 ± 0.2 | 200.0 ± 0.2 | 201.8 ± 0.2 | 199.6 ± 0.2 | 202.4 ± 0.2 | 0.05 |
| Male | 182.2 ± 0.3 | 185.1 ± 0.2 | 184.6 ± 0.2 | 186.3 ± 0.2 | 183.9 ± 0.2 | 185.4 ± 0.3 | 0.0005 |
| Mean age‐adjusted total cholesterol (mg/dL) | |||||||
| Female | 199.5 ± 0.3 | 201.2 ± 0.2 | 199.9 ± 0.2 | 202.0 ± 0.2 | 199.8 ± 0.2 | 202.6 ± 0.2 | <10−7 |
| Male | 184.0 ± 0.3 | 185.6 ± 0.2 | 184.4 ± 0.2 | 186.1 ± 0.2 | 183.5 ± 0.2 | 185.3 ± 0.3 | 0.32 |
| Mean triglycerides (mg/dL) | |||||||
| Female | 130.9 ± 0.7 | 125.4 ± 0.4 | 122.7 ± 0.4 | 118.0 ± 0.3 | 116.5 ± 0.3 | 116.0 ± 0.4 | <10−16 |
| Male | 143.6 ± 0.8 | 144.8 ± 0.6 | 145.4 ± 0.6 | 141.7 ± 0.5 | 139.6 ± 0.5 | 140.7 ± 0.7 | <10−12 |
| Mean age‐adjusted triglycerides (mg/dL) | |||||||
| Female | 129.0 ± 0.6 | 124.4 ± 0.4 | 122.5 ± 0.4 | 118.3 ± 0.3 | 116.9 ± 0.3 | 116.4 ± 0.4 | <10−16 |
| Male | 145.3 ± 0.9 | 145.2 ± 0.6 | 145.3 ± 0.6 | 141.6 ± 0.5 | 139.2 ± 0.5 | 140.6 ± 0.7 | <10−16 |
| Mean LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 114.3 ± 0.3 | 115.2 ± 0.2 | 113.5 ± 0.2 | 115.8 ± 0.2 | 113.7 ± 0.2 | 115.3 ± 0.2 | 0.23 |
| Male | 106.5 ± 0.3 | 108.6 ± 0.2 | 108.2 ± 0.2 | 110.2 ± 0.2 | 108.5 ± 0.2 | 109.4 ± 0.2 | <10−10 |
| Mean age‐adjusted LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 114.2 ± 0.3 | 115.1 ± 0.2 | 113.5 ± 0.2 | 115.8 ± 0.2 | 113.7 ± 0.2 | 115.3 ± 0.2 | 0.08 |
| Male | 108.2 ± 0.3 | 109.0 ± 0.2 | 108.0 ± 0.2 | 110.0 ± 0.2 | 108.2 ± 0.2 | 109.3 ± 0.2 | 0.12 |
| Mean non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 138.7 ± 0.6 | 140.1 ± 0.2 | 137.9 ± 0.2 | 139.4 ± 0.2 | 137.9 ± 0.2 | 139.7 ± 0.2 | 0.73 |
| Male | 137.2 ± 0.6 | 136.8 ± 0.2 | 136.1 ± 0.2 | 137.8 ± 0.2 | 136.0 ± 0.2 | 137.2 ± 0.3 | 0.62 |
| Mean age‐adjusted non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 138.3 ± 0.6 | 139.9 ± 0.2 | 137.8 ± 0.2 | 139.5 ± 0.2 | 138.0 ± 0.2 | 139.8 ± 0.2 | 0.32 |
| Male | 138.6 ± 0.5 | 137.4 ± 0.2 | 136.1 ± 0.2 | 137.7 ± 0.2 | 135.7 ± 0.2 | 137.2 ± 0.3 | 0.0008 |
| Mean Apo B (mg/dL) | |||||||
| Female | 97.5 ± 0.2 | 95.3 ± 0.3 | 98.1 ± 0.1 | 98.0 ± 0.1 | 98.8 ± 0.1 | 99.7 ± 0.1 | <10−16 |
| Male | 95.0 ± 0.2 | 94.2 ± 0.2 | 97.8 ± 0.2 | 97.8 ± 0.1 | 98.2 ± 0.1 | 99.1 ± 0.2 | <10−16 |
| Mean age‐adjusted apo B (mg/dL) | |||||||
| Female | 97.0 ± 0.2 | 95.1 ± 0.2 | 98.1 ± 0.1 | 98.1 ± 0.1 | 98.9 ± 0.1 | 99.7 ± 0.1 | <10−16 |
| Male | 96.0 ± 0.2 | 94.4 ± 0.2 | 97.7 ± 0.2 | 97.7 ± 0.1 | 98.0 ± 0.1 | 99.1 ± 0.2 | <10−16 |
| 1st follow‐up mean BMI (kg/m2) | |||||||
| Female | 29.87 ± 0.18 | 29.82 ± 0.15 | 29.27 ± 0.11 | 28.69 ± 0.10 | 28.85 ± 0.08 | 28.56 ± 0.09 | <10−16 |
| Male | 29.99 ± 0.14 | 30.27 ± 0.12 | 29.94 ± 0.09 | 29.72 ± 0.09 | 29.66 ± 0.07 | 29.45 ± 0.08 | <10−9 |
| Mean age‐adjusted BMI (kg/m2) | |||||||
| Female | 30.22 ± 0.17 | 29.94 ± 0.15 | 29.35 ± 0.11 | 28.59 ± 0.10 | 28.76 ± 0.08 | 28.56 ± 0.10 | <10−16 |
| Male | 30.30 ± 0.14 | 30.31 ± 0.11 | 29.93 ± 0.09 | 29.64 ± 0.09 | 29.60 ± 0.07 | 29.49 ± 0.08 | <10−14 |
| Mean total cholesterol (mg/dL) | |||||||
| Female | 187.3 ± 0.7 | 190.4 ± 0.5 | 189.6 ± 0.4 | 195.2 ± 0.3 | 193.5 ± 0.3 | 194.9 ± 0.4 | <10−16 |
| Male | 166.4 ± 0.7 | 170.9 ± 0.5 | 171.2 ± 0.4 | 174.8 ± 0.4 | 170.6 ± 0.3 | 174.3 ± 0.4 | <10−12 |
| Mean age‐adjusted total cholesterol (mg/dL) | |||||||
| Female | 187.6 ± 0.7 | 190.5 ± 0.5 | 189.6 ± 0.4 | 195.2 ± 0.3 | 193.5 ± 0.3 | 194.8 ± 0.3 | <10−16 |
| Male | 168.7 ± 0.7 | 171.6 ± 0.5 | 171.0 ± 0.4 | 174.4 ± 0.4 | 170.4 ± 0.3 | 174.2 ± 0.4 | <10−5 |
| Mean triglycerides (mg/dL) | |||||||
| Female | 127.0 ± 1.2 | 125.4 ± 1.2 | 123.5 ± 0.7 | 118.8 ± 0.6 | 114.7 ± 0.5 | 114.4 ± 0.6 | <10−16 |
| Male | 135.9 ± 1.8 | 134.2 ± 1.4 | 136.1 ± 0.9 | 136.0 ± 0.9 | 128.4 ± 0.7 | 130.8 ± 0.9 | <10−8 |
| Mean age‐adjusted triglycerides (mg/dL) | |||||||
| Female | 126.3 ± 1.3 | 125.1 ± 1.0 | 123.4 ± 0.7 | 118.9 ± 0.6 | 114.8 ± 0.5 | 114.4 ± 0.6 | <10−16 |
| Male | 138.6 ± 1.7 | 135.0 ± 1.3 | 135.9 ± 0.9 | 135.6 ± 0.9 | 128.1 ± 0.7 | 130.6 ± 0.9 | <10−12 |
| Mean LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 101.7 ± 0.6 | 105.0 ± 0.5 | 103.6 ± 0.3 | 109.4 ± 0.3 | 107.3 ± 0.3 | 107.9 ± 0.3 | <10−16 |
| Male | 92.5 ± 0.6 | 95.9 ± 0.4 | 96.6 ± 0.3 | 100.1 ± 0.3 | 96.5 ± 0.3 | 99.4 ± 0.3 | <10−15 |
| Mean age‐adjusted LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 102.8 ± 0.7 | 105.4 ± 0.5 | 103.8 ± 0.3 | 109.2 ± 0.3 | 107.1 ± 0.3 | 107.7 ± 0.3 | <10−16 |
| Male | 94.8 ± 0.6 | 96.6 ± 0.4 | 96.4 ± 0.3 | 99.7 ± 0.3 | 96.3 ± 0.3 | 99.3 ± 0.3 | <10−7 |
| Mean non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 124.7 ± 1.1 | 130.0 ± 0.5 | 128.5 ± 0.4 | 132.9 ± 0.3 | 130.9 ± 0.3 | 131.7 ± 0.3 | <10−10 |
| Male | 117.4 ± 1.1 | 122.2 ± 0.5 | 123.2 ± 0.4 | 126.1 ± 0.4 | 121.9 ± 0.3 | 125.4 ± 0.4 | 0.0002 |
| Mean age‐adjusted non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 125.9 ± 1.2 | 130.3 ± 0.5 | 128.6 ± 0.4 | 132.9 ± 0.3 | 130.7 ± 0.3 | 131.7 ± 0.3 | <10−7 |
| Male | 120.7 ± 1.2 | 123.1 ± 0.5 | 123.1 ± 0.4 | 125.8 ± 0.4 | 121.7 ± 0.3 | 125.3 ± 0.3 | 0.07 |
| Mean Apo B (mg/dL) | |||||||
| Female | 89.9 ± 0.4 | 89.4 ± 0.3 | 93.1 ± 0.3 | 94.9 ± 0.2 | 95.5 ± 0.2 | 95.8 ± 0.2 | <10−16 |
| Male | 86.1 ± 0.4 | 85.7 ± 0.3 | 90.5 ± 0.3 | 91.5 ± 0.2 | 90.6 ± 0.2 | 92.7 ± 0.3 | <10−16 |
| Mean age‐adjusted apo B (mg/dL) | |||||||
| Female | 90.3 ± 0.5 | 89.5 ± 0.4 | 93.1 ± 0.3 | 94.8 ± 0.2 | 95.4 ± 0.2 | 95.7 ± 0.2 | <10−16 |
| Male | 87.5 ± 0.4 | 86.0 ± 0.3 | 90.5 ± 0.3 | 91.1 ± 0.2 | 90.4 ± 0.2 | 92.6 ± 0.2 | <10−16 |
| 2nd follow‐up mean BMI (kg/m2) | |||||||
| Female | 30.37 ± 0.31 | 29.97 ± 0.25 | 28.94 ± 0.18 | 28.71 ± 0.15 | 28.50 ± 0.13 | 28.69 ± 0.13 | <10−9 |
| Male | 30.87 ± 0.27 | 29.83 ± 0.18 | 30.40 ± 0.15 | 29.81 ± 0.13 | 29.55 ± 0.11 | 29.62 ± 0.11 | <10−7 |
| Mean age‐adjusted BMI (kg/m2) | |||||||
| Female | 30.66 ± 0.30 | 30.18 ± 0.23 | 29.05 ± 0.19 | 28.71 ± 0.15 | 28.35 ± 0.13 | 28.67 ± 0.13 | <10−14 |
| Male | 31.05 ± 0.25 | 29.97 ± 0.18 | 30.38 ± 0.14 | 29.78 ± 0.13 | 29.47 ± 0.11 | 29.65 ± 0.11 | <10−9 |
| Mean total cholesterol (mg/dL) | |||||||
| Female | 183.6 ± 1.4 | 182.4 ± 1.0 | 185.0 ± 0.7 | 189.1 ± 0.5 | 190.7 ± 0.5 | 192.2 ± 0.5 | <10−16 |
| Male | 162.0 ± 1.2 | 164.0 ± 0.9 | 166.1 ± 0.6 | 167.6 ± 0.5 | 166.7 ± 0.5 | 166.1 ± 0.5 | 0.008 |
| Mean age‐adjusted total cholesterol (mg/dL) | |||||||
| Female | 184.2 ± 1.4 | 182.8 ± 1.0 | 185.1 ± 0.7 | 189.2 ± 0.5 | 190.6 ± 0.5 | 192.1 ± 0.5 | <10−16 |
| Male | 163.6 ± 1.3 | 164.9 ± 0.9 | 165.5 ± 0.6 | 167.4 ± 0.5 | 166.8 ± 0.5 | 166.1 ± 0.5 | 0.03 |
| Mean triglycerides (mg/dL) | |||||||
| Female | 130.3 ± 2.3 | 124.1 ± 1.6 | 122.2 ± 1.2 | 119.5 ± 0.9 | 113.6 ± 0.7 | 115.7 ± 0.8 | <10−16 |
| Male | 135.9 ± 2.7 | 135.1 ± 2.2 | 134.2 ± 1.4 | 132.5 ± 1.2 | 126.7 ± 1.1 | 125.9 ± 1.0 | <10−10 |
| Mean age‐adjusted triglycerides (mg/dL) | |||||||
| Female | 130.1 ± 2.3 | 124.0 ± 1.6 | 122.2 ± 1.1 | 119.5 ± 0.9 | 113.6 ± 0.8 | 115.7 ± 0.8 | <10−16 |
| Male | 138.0 ± 2.9 | 136.4 ± 2.0 | 133.3 ± 1.4 | 132.2 ± 1.2 | 126.7 ± 1.0 | 126.0 ± 1.1 | <10−11 |
| Mean LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 98.8 ± 1.2 | 98.2 ± 0.9 | 100.0 ± 0.6 | 103.2 ± 0.5 | 104.1 ± 0.4 | 104.2 ± 0.4 | <10−16 |
| Male | 88.5 ± 1.0 | 89.7 ± 0.7 | 92.0 ± 0.5 | 93.8 ± 0.5 | 92.6 ± 0.4 | 91.9 ± 0.4 | 0.01 |
| Mean age‐adjusted LDL‐cholesterol calculated (mg/dL) | |||||||
| Female | 99.8 ± 1.2 | 98.2 ± 0.8 | 100.0 ± 0.6 | 103.2 ± 0.5 | 104.1 ± 0.4 | 104.2 ± 0.4 | <10−16 |
| Male | 90.0 ± 1.1 | 90.5 ± 0.8 | 91.4 ± 0.5 | 93.6 ± 0.5 | 92.6 ± 0.4 | 91.9 ± 0.4 | 0.05 |
| Mean non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 123.9 ± 2.2 | 122.4 ± 0.9 | 124.5 ± 0.6 | 127.0 ± 0.5 | 127.6 ± 0.5 | 128.2 ± 0.5 | <10−11 |
| Male | 111.8 ± 2.0 | 115.9 ± 0.9 | 118.2 ± 0.6 | 119.6 ± 0.5 | 117.4 ± 0.5 | 117.1 ± 0.5 | 0.91 |
| Mean age‐adjusted non‐HDL‐cholesterol (mg/dL) | |||||||
| Female | 125.3 ± 2.3 | 123.0 ± 1.0 | 124.6 ± 0.6 | 127.1 ± 0.5 | 127.4 ± 0.5 | 128.1 ± 0.5 | <10−9 |
| Male | 114.6 ± 2.3 | 117.1 ± 0.9 | 117.5 ± 0.6 | 119.4 ± 0.5 | 117.5 ± 0.5 | 117.2 ± 0.5 | 0.73 |
| Mean Apo B (mg/dL) | |||||||
| Female | 88.2 ± 0.8 | 85.2 ± 0.6 | 91.4 ± 0.4 | 91.6 ± 0.3 | 94.0 ± 0.3 | 94.0 ± 0.3 | <10−16 |
| Male | 84.0 ± 0.8 | 82.1 ± 0.5 | 87.6 ± 0.4 | 88.1 ± 0.4 | 88.1 ± 0.3 | 87.6 ± 0.3 | <10−12 |
| Mean age‐adjusted Apo B (mg/dL) | |||||||
| Female | 88.7 ± 0.9 | 85.5 ± 0.6 | 91.4 ± 0.4 | 91.6 ± 0.3 | 93.9 ± 0.3 | 94.0 ± 0.3 | <10−16 |
| Male | 84.9 ± 0.8 | 82.7 ± 0.6 | 87.4 ± 0.4 | 87.9 ± 0.4 | 88.0 ± 0.3 | 87.7 ± 0.3 | <10−10 |
Table 3 examines LDL‐cholesterol concentration in 636 604 total patients without regard to fasting status, corresponding to the analyses by Kaufmann et al.5 Again, age‐adjusted mean LDL‐C concentrations increased significantly (P < 10−16) in men and women, and the percentage with LDL‐cholesterol ≥160 mg/dL also increased significantly (P < 10−7) in men and women. Similar results were obtained for ages 40 to 75 years old (corresponding to ACC/AHA guidelines).
Table 3.
Baseline LDL‐cholesterol concentrations by year without regard to fasting status (fasting, nonfasting and unknown fasting status) corresponding to the analyses by Kaufmann et al5
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Trend (P) | |
|---|---|---|---|---|---|---|---|
| Age ≥ 16 years sample | |||||||
| Female | 23 645 | 48 333 | 61 971 | 73 110 | 95 306 | 49 177 | |
| Male | 23 049 | 43 181 | 51 161 | 58 394 | 73 924 | 35 353 | |
| Mean age‐adjusted LDL‐cholesterol (kg/m2) | |||||||
| Female | 120.3 ± 0.3 | 121.4 ± 0.2 | 119.8 ± 0.2 | 120.8 ± 0.1 | 122.3 ± 0.1 | 123.6 ± 0.2 | <10−16 |
| Male | 114.3 ± 0.3 | 115.9 ± 0.2 | 114.8 ± 0.2 | 116.1 ± 0.2 | 117.5 ± 0.1 | 117.0 ± 0.2 | <10−16 |
| High LDL‐cholesterol (≥160 mg/dL, %) | |||||||
| Female | 15.2 ± 0.2 | 15.8 ± 0.2 | 14.5 ± 0.1 | 14.7 ± 0.1 | 16.0 ± 0.1 | 16.8 ± 0.2 | <10−16 |
| Male | 11.9 ± 0.2 | 12.9 ± 0.2 | 12.6 ± 0.1 | 13.3 ± 0.1 | 14.6 ± 0.1 | 14.7 ± 0.2 | <10−16 |
| Age 45‐74 years sample | |||||||
| Female | 5323 | 10 744 | 14 699 | 17 954 | 23 886 | 12 605 | |
| Male | 4719 | 9219 | 11 556 | 13 333 | 17 569 | 8575 | |
| Mean age‐adjusted LDL‐cholesterol (kg/m2) | |||||||
| Female | 122.9 ± 0.3 | 124.1 ± 0.2 | 122.8 ± 0.2 | 124.3 ± 0.2 | 126.0 ± 0.1 | 127.9 ± 0.2 | <10−16 |
| Male | 114.2 ± 0.3 | 116.0 ± 0.2 | 115.1 ± 0.2 | 116.8 ± 0.2 | 118.6 ± 0.2 | 118.8 ± 0.2 | <10−16 |
| High LDL‐cholesterol (≥160 mg/dL, %) | |||||||
| Female | 16.5 ± 0.3 | 17.3 ± 0.2 | 16.4 ± 0.2 | 16.9 ± 0.2 | 18.4 ± 0.1 | 19.6 ± 0.2 | <10−16 |
| Male | 12.1 ± 0.2 | 13.1 ± 0.2 | 12.8 ± 0.2 | 13.8 ± 0.2 | 15.2 ± 0.2 | 15.5 ± 0.2 | <10−16 |
4. DISCUSSION
Our analyses in 507 752 patient fasting blood samples failed to demonstrate any significant reduction in LDL‐cholesterol levels nationally with respect to overall mean LDL‐cholesterol or the percentage of the patient population classified as borderline, high or very high LDL‐cholesterol by ATP‐III guidelines. We were also unable to demonstrate LDL‐cholesterol reductions in the 45 to 74‐year‐old patient group specifically targeted by the 2013 ACC/AHA recommendations, nor in the 60 to 75 year old age bracket for whom the new recommendations would likely have the greatest impact. This was further confirmed in the patients' first and second follow‐up samples. These results are inconsistent with our expectation that expanded statin eligibility and higher recommended doses should further decrease LDL‐cholesterol. It is unlikely that the potential to reduce LDL‐cholesterol levels nationally had already been achieved by 2012 given the inclusion of heretofore untargeted patients, and clear evidence that higher statin doses further decrease LDL‐cholesterol. LDL‐cholesterol reduction with moderate and intense statin therapy has been reported to be 10.4% with 40 mg/d pravastatin (moderate therapy) and 41.5% with 80 mg/d atorvastatin (intensive therapy).16 Moreover, only 8.8 million of the 33 million Americans meeting new eligibility meeting new guidelines for primary prevention of ASCVD are estimated to take statins.17
Using a national sample of the U.S. population, Pencina et al. estimated that the new guidelines would qualify an additional 12.8 million adults (11.1%) between 40 to 75 years old for statin therapy.8 Maddox et al reported that 32.4% of statin‐eligible cardiology patients had not received statins, of whom 12.6% had LDL‐cholesterol <100 mg/dL, from a retrospective analysis of 1 174 545 of the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence (NCDR PINNACLE) registry between 2008 and 2012.18 Thirty‐six percent of diabetics and 37% of patients with an estimated ASCVD risk of ≥7.5% were untreated.19 Patients with LDL‐cholesterol previously characterized as normal (70 to 100 mg/dL) would now be considered for pharmacotherapy, and many have risk >7.5% on the basis of age alone, including nearly all African‐American men over the age of 63. Because age is such an important determinant of CVD risk, under the new guidelines statins would be indicated for approximately 77% of adults between 60 and 75 years of age.20
Our results are consistent with other reports showing little change in statin therapy following the guideline release. Nationally, prevalence of high cholesterol increased non‐significantly from 11.0% in 2013‐2014 to 12.4% in 2015‐2016,4 and heart disease deaths increased from 167.0 per 100 000 population in 2014 to 168.5 in 2015.3 Okerson et al… reported that LDL‐cholesterol levels have remained unchanged in 90 287 ASCVD patients who were continuously enrolled 6 months before and 7 months after the first ASCVD diagnosis between 2012 and 2014.12 Tran et al reported little appreciable change in statin use, only a slight increase in prescription intensity, and no changes in patient LDL‐cholesterol levels after the guideline release in 610 535 ASCVD and diabetes patients belonging to a US health insurance organization.9 Retrospective analysis of 1 100 682 patients in the Veterans Affairs Corporate Data Warehouse found that use of moderate to high‐intensity statins increased by less than 1 % following the guideline change and by 2% following formulary change.10 They concluded that greater accessibility of genetic atorvastatin was more important than the revised guidelines in increasing moderate‐to‐high‐intensity prescriptions. In another study from the Veterans Affairs Health System, Rodriguez et al.. reported that high‐intensity statin use increased from 28% in 331 927 ASCVD patients before the guidelines release to 35% in 326 759 ASCVD patients after guideline's release.11 Men, younger individuals, and patients in academic and West Coast hospitals were more likely to receive more intensive statin therapy relative to pre‐release levels.12 However, Rosenson et al.. reported that statin use following hospital discharge for myocardial infarction had increased from 33.5% in 2011 to 71% in 2014 for patients with commercial health care and from 24.8% in 2011 to 57.5% in 2014 for Medicare patients.21
A number of factors may contribute to the lack of decline in blood LDL‐cholesterol values following the 2013 ACC/AHA guidelines. Admittedly, changes in medical practice are generally sluggish‐the Institute of Medicine has estimated that the incorporation of new knowledge into clinical practice takes an average of 17 years.22 One year after the ACC/AHA guidelines were published, Virani et al found that health care providers were unaware of the ACC/AHA guidelines, use of the 10‐years ASCVD risk estimator to guide statin treatment, and the four major groups likely to benefit from statin use.23 Most continued to prescribe statins in response to targeted LDL‐C levels. Patients and physicians might also be reluctant to prescribe a cholesterol lowering medication in the absence of high cholesterol and concern for statin overtreatment.24 The very success of ATP‐III may also discourage change. Resistance to the new guidelines might also arise from the publication of other guidelines that still employ the “treat to target” approach to high cholesterol.25, 26 An additional factor may be the inclusion of the “Shared Decision Making (SDM)” concept of the ACA/AHA guidelines that involved inclusion of the patient in the decision to use lipid lowering agents.6, 27 An analysis of a secondary prevention population in a managed care organization reported that only 37.2% of ASCVD patients were on high‐intensity statin therapy.2 The decreased emphasis on nonstatin drug therapy in the 2013 ACC/AHA guidelines suggests many high‐risk patients should receive statin therapy and nothing else.28
The 2013 guidelines do not negate the clinical significance of lowering LDL‐cholesterol to reduce ASCVD risk, rather, none of the randomized controlled clinical trials used to prove the benefits of statin therapy titrated dosing to a specific LDL‐cholesterol goal. Lifestyle changes for lowering LDL‐cholesterol continue to be a major component of the recommendations. Epidemiological evidence clearly shows very low CHD risk for LDL‐cholesterol levels <100 mg/dL vs accelerated risk for high (160‐189 mg/dL) and very high LDL‐cholesterol (≥190 mg/dL).29 Moreover, randomized trials of LDL‐cholesterol reduction have demonstrated the lower the LDL‐cholesterol achieved, the greater the reduction in cardiovascular events.30 More simply said, there is a clinical benefit to higher dose statin than need to achieve lower LDL‐cholesterol levels. As a result of some confusion some investigators have called for reconsideration of the new guidelines.31
Caveats and limitations: The strength of our results is the large sample size from throughout the United States using a standard laboratory assay in a single laboratory. A second strength is the inclusion of first and second repeat blood value sample analysis to assess temporal change during follow‐up care. However, our results are based on a sample of opportunity rather than a rigorously designed sampling strategy for precisely estimating total and LDL‐cholesterol levels throughout the country. Limited data were available for characterizing the population. Boston Heart Diagnostics provides a series of more advanced lipoprotein measurements and one limitation is that the sample may include a higher proportion of patients who did not respond satisfactorily to standard treatment. The database did not containing information on the source of the sample to preserve anonymity. Although most of the samples were provided from general and specialty practice rather than institutions, the exact proportion are not known. In addition, treatment status is unknown for many patients in that it is not known whether a nonresponse to cholesterol medication use means no drugs were used or the question was ignored.
Another limitation is that improvements in LDL‐cholesterol could theoretically be missed due to the perceived discouragement for follow‐up blood work. For example, 20.8% of received multiple measurement LDL‐cholesterol measurements that would now become unnecessary for cholesterol management from retrospective analysis of 1 174 545 of the National Cardiovascular Data Registry Practice Innovation and Clinical Excellence (NCDR PINNACLE) registry between 2008 and 2012.19 However, Table 2 shows an absence of change over time for the first and second follow‐up measurements LDL‐cholesterol, this suggest to us that changes in LDL‐cholesterol monitoring does not explain the apparent stable or slightly increasing LDL‐cholesterol levels since 2012.
5. CONCLUSIONS
In conclusion, our analyses in 507 752 patients provide preliminary evidence that the expected increase in statin therapy, following the ACC/AHA guidelines, did not occur nationally, and that total and LDL‐cholesterol levels actually increased contrary to expectations. One possibility may be sluggish implementation of the new guidelines into clinical practice as well as ambiguity in, or lack of clear evidence for, the management recommendations.19 Others report that disagreement with the recommendations was the main hindrance to adoption of the 2013 ACC/AHA Guidelines for the Prevention of Primary and Secondary Atherosclerotic Disease.24
CONFLICTS OF INTEREST
The authors declare no potential conflict of interests.
ACKNOWLEDGEMENTS
This work was conducted in Framingham Massachusetts at Boston Heart Diagnostics. Superko H. Robert, MD, is a part‐time consultant for Boston Heart Diagnostics. Paul T. Williams, PhD is a part‐time statistical consultant for Boston Heart Diagnostics. Michael Dansinger, MD is employed by Boston Heart Diagnostics as the Vice President of Medical Affairs. Ernst Schaefer, MD is employed by Boston Heart Diagnostics as the Chief Medical Officer.
Superko HR, Williams PT, Dansinger M, Schaefer E. Trends in low‐density lipoprotein‐cholesterol blood values between 2012 and 2017 suggest sluggish adoption of the recent 2013 treatment guidelines. Clin Cardiol. 2019;42:101–110. 10.1002/clc.23115
REFERENCES
- 1. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults . Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486‐2497. [DOI] [PubMed] [Google Scholar]
- 2. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227‐239. [DOI] [PubMed] [Google Scholar]
- 3. National Center for Health Statistics . Health, United States 2016 With Chartbook on Long‐term Trends in Health. Vol 2017 Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 4. Carroll MD, Fryar CD, Nguyen DT. High total and low high‐density lipoprotein cholesterol in adults: United States, 2015–2016. NCHS data brief, no 290. Hyattsville, MD: National Center for Health Statistics:2017. [PubMed] [Google Scholar]
- 5. Kaufman HW, Blatt AJ, Huang X, Odeh MA, Superko HR. Blood cholesterol trends 2001‐2011 in the United States: analysis of 105 million patient records. PLoS One. 2013;8(5):e63416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S1‐S45. [DOI] [PubMed] [Google Scholar]
- 7. Ioannidis JPA. More than a billion people taking statins?: potential implications of the new cardiovascular guidelines. JAMA. 2014;311:463‐464. [DOI] [PubMed] [Google Scholar]
- 8. Pencina MJ, Navar‐Boggan AM, D'Agostino B, et al. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422‐1431. [DOI] [PubMed] [Google Scholar]
- 9. Tran JN, Kao TC, Caglar T, et al. Impact of the 2013 cholesterol guideline on patterns of lipid‐lowering treatment in patients with atherosclerotic cardiovascular disease or diabetes after 1 year. J Manag Care Spec Pharm. 2016;22:901‐908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Markovitz AA, Holleman RG, Hofer TP, Kerr EA, Klamerus ML, Sussman JB. Effects of guideline and formulary changes on statin prescribing in the Veterans Affairs. Health Serv Res. 2017;52:1996‐2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodriguez F, Lin S, Maron DJ, Knowles JW, Virani SS, Heidenreich PA. Use of high‐intensity statins for patients with atherosclerotic cardiovascular disease in the veterans affairs health system: practice impact of the new cholesterol guidelines. Am Heart J. 2016;182:97‐102. [DOI] [PubMed] [Google Scholar]
- 12. Okerson T, Patel J, DiMario S, Burton T, Seare J, Harrison DJ. Effect of 2013 ACC/AHA blood cholesterol guidelines on statin treatment patterns and low‐denisty lipoprotein cholesterol in atherosclerotic cardiovascular disease patients. J Am Heart Assoc. 2017;6:e004909 10.1161/JAHA.116.004909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470‐475. [PubMed] [Google Scholar]
- 14. Miida T, Nishimura K, Hirayama S, et al. Homogeneous Assays for LDL‐C and HDL‐C are Reliable in Both the Postprandial and Fasting State. J Atheroscler Thromb. 2017;24(6):583‐599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low‐density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499‐502. [PubMed] [Google Scholar]
- 16. Cannon CP, Braunwald E, McCabe CH, et al. For the pravastatin or atorvastatin evaluation and infection therapy–thrombolysis in myocardial infarction 22 investigators. Intensive versus moderate lipid lowering with statins after acute coronary syndrome. N Engl J Med. 2004;350:1495‐1504. [DOI] [PubMed] [Google Scholar]
- 17. Yang Q, Zhong Y, Gillespie C, et al. Assessing potential population impact of statin treatment for primary prevention of atherosclerotic cardiovascular diseases in the USA: population‐based modelling study. BMJ Open. 2017;7(1):e011684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Maddox TM, Borden WB, Tang F, et al. Implications of the 2013 ACC/AHA cholesterol guidelines for adults in contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J Am Coll Cardiol. 2014;64(21):2183‐2192. [DOI] [PubMed] [Google Scholar]
- 19. Tilson EC. Dissemination and Adoption of Guidelines. The Experience of Community Care of North Carolina. N Carolina Med J. 2015;76:251‐255. 10.18043/ncm.76.4.251. [DOI] [PubMed] [Google Scholar]
- 20. Keaney JF Jr, Curfman GD, Jarcho JA. A pragmatic view of the new cholesterol treatment guidelines. N Engl J Med. 2014;370:275‐278. [DOI] [PubMed] [Google Scholar]
- 21. Rosenson RS, Farkouh ME, Mefford M, et al. Trends in use of high‐intensity statin therapy after myocardial infarction, 2011 to 2014. J Am Coll Cardiol. 2017;69:2696‐2706. [DOI] [PubMed] [Google Scholar]
- 22. Institute of Medicine. Committee on Quality of Health Care in America . Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 23. Virani SS, Pokharel Y, Steinberg L, et al. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol. 2016;10:497‐504.e4. [DOI] [PubMed] [Google Scholar]
- 24. Jamé S, Wittenberg E, Potter MB, Fleischmann KE. The new lipid guidelines: what do primary care clinicians think? Am J Med. 2015;128:914.e5‐914.e10. 10.1016/j.amjmed.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European atherosclerosis society (EAS). Eur Heart J. 2011;32:1769‐1818. [DOI] [PubMed] [Google Scholar]
- 26. Cainzos‐Achirica M, Desai CS, Wang L, et al. Pathways forward in cardiovascular disease prevention one and a half years after the publication of the 2013 ACC/AHA prevention guidelines. Mayo Clin Proc. 2015;90:1262‐1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Drozda JP, Ferguson TB, Jneid H, et al. 2015 ACC/AHA focused update of secondary prevetion lipid performance measures. Circ Cardiovasc Qual Outcomes. 2016;9:68‐95. [DOI] [PubMed] [Google Scholar]
- 28. Bellows BK, Olsen CJ, Voelker J, Wander C. Antihyperlipidemic medication treatment patterns and statin adherence among patients with ASCVD in a managed care plan after release of the 2013 ACC/AHA guideline on the treatment of blood cholesterol. J Manag Care Spec Pharm. 2016;22:892‐900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blumenthal RS, Nasir K. Introduction: What have we learned since the 2013 ACC/AHA guidelines? Am J Cardiol. 2016(228):1A‐3A. [DOI] [PubMed] [Google Scholar]
- 30. Soran H, Kwok S, Adam S, Ho JH, Durrington PN. Evidence for more intensive cholesterol lowering. Curr Opin Lipidol. 2017;28(4):291‐299. [DOI] [PubMed] [Google Scholar]
- 31. Cholesterol Treatment Trialists' (CTT) Collaborators , Mihaylova B, Emberson J, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta‐analysis of individual data from 27 randomised trials. Lancet. 2012;380:581‐590. 10.1016/S0140-6736(12)60367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


