Dear Editor,
Mindfulness meditation alleviates symptoms of distress, pain, and many chronic diseases.1, 2, 3 In schizophrenic patients, mindfulness intervention leads to better psychosocial functioning,4 improved positive emotions,5 and reduced negative symptoms.6 It is unknown if mindfulness meditation could reduce positive symptoms in the chronic schizophrenia patients.
Five male patients, averaged age at 55.80 ± 9.45 years old (ranged 44‐66 years), with averaged medical history of 30.20 ± 8.53 years (ranged 21‐41 years) were recruited for present study. All patients received active antipsychotics treatment upon admission (at higher doses than patients on average): chlorpromazine equality averaged at 670.00 ± 176.47 mg/d (ranged 487.5‐900).
These patients demonstrated severe and drug treatment‐resistant hallucination/delusions (score >5; Details in Table 1). The Positive and Negative Syndrome Scale (PANSS), Short Form‐36 Health Survey (SF‐36), and Five Facet Mindfulness Questionnaire (FFMQ) were measured by an expert clinical psychologist.
Table 1.
Clinical data of the five patients
| No | Age | Medical history | First psychosis | Antipsychotics, mg/d | Clinical symptoms | Hallucination score | Delusion score |
|---|---|---|---|---|---|---|---|
| 1 | 64 | 33 | 31 | Chlorpromazine 400 + perphenazine 10 | Severe verbal auditory hallucination, delusion of persecution/reference, paralogism thinking, apathy | 6 | 6 |
| 2 | 66 | 41 | 25 | Chlorpromazine 400 + risperidone 5 | Pseudohallucination, delusion of persecution/reference/grandeur/sin, paralogism thinking, self‐contradict, apathy | 5 | 6 |
| 3 | 56 | 34 | 22 | Chlorpromazine 400 + clozapine 200 | Severe verbal auditory hallucination, delusion of persecution//physical influence, paralogism thinking, apathy | 6 | 6 |
| 4 | 44 | 22 | 22 | Clozapine 275 + chlorpromazine 350 | Verbal auditory hallucination, delusion of persecution/grandeur/love/hypocenesthesia, paralogism thinking, double personality, dysregulated emotion | 6 | 6 |
| 5 | 49 | 21 | 28 | Chlorpromazine 300 + clozapine 125 | Pseudohallucination, delusion of persecution/reference/physical influence, paralogism thinking, apathy | 5 | 6 |
The study has been approved by the ethic committee of medical research in the Minzheng hospital, and written informed consents were obtained from all patients for the study, or the guardians/next of kin of these participants when in need. Informed consent was as well obtained for the publication of this case report. This clinical trial has been registered on the Chinese Clinical Trial Registry (https://www.chictr.org.cn/index.aspx). The registration number is ChiCTR‐OOB‐17014038. Registered December 19, 2017 (retrospectively registered).
Timeline:
February 2017: Recruitment of patients and start of the trial.
Intervention: 8 months, group intervention, and individual training.
Follow‐up: 1, 2, 3, 4, 5, 6, 7, 8 weeks and 8 months after start point of intervention for the hallucination and delusion symptoms, and relevant scales.
Mindfulness meditation was performed with following procedures. In the first 8 weeks, the group intervention (90 minutes each, led by two experienced tutors) was conducted per week, and after the period, the group intervention frequency was once per month. During the continuous 8 months period, the patients performed mindfulness meditation per day for 20‐40 minutes. The records were double checked and confirmed by the tutors. The data were analyzed with SPSS 18.0 software (SPSS Inc., Chicago, IL, USA); paired‐sample t test was used for differences before and after intervention.
The hallucination and delusion symptoms persisted and exhibited no change during the past 8 years (measured at 8 years ago, 4 years ago, 2 weeks ago, and baseline time point) prior to this study. Following mindfulness training intervention, the hallucination and delusion symptoms did not exhibit much change in the first 2 weeks but began to decrease after 3 weeks of intervention. The improvements persisted as the intervention continued. At the end of 8‐month intervention period, significant reductions in both hallucination and delusion symptoms were observed in all patients (P < 0.05; Figure 1). Notably, the PANSS positive symptoms and negative symptoms both decreased following intervention (P < 0.05; Table 2). In addition, the quality of life index in SF‐36 and mindfulness score in FFMQ improved significantly following intervention (P < 0.05; Table 3).
Figure 1.
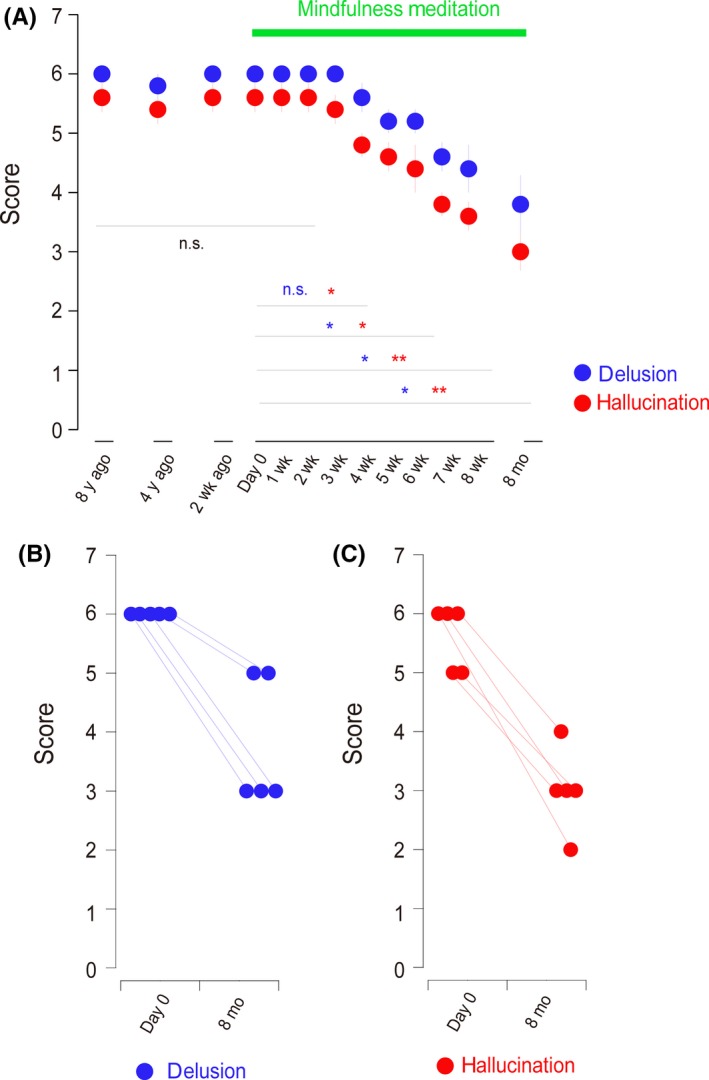
Eight‐month‐lasting mindfulness meditation reduces hallucination and delusion scores in the chronic severe schizophrenia patients (* for P < 0.05). A, Time‐dependent changes of hallucination and delusion scores following mindfulness meditation training. B, All patients exhibited reduced delusion score following mindfulness meditation training. C, All patients exhibited reduced hallucination score following mindfulness meditation training
Table 2.
PANSS Score changes
| 8 y before | 4 y before | 2 wk before | Baseline | 4 wk after | 8 wk after | 8 y later | Baseline vs 8 y later | ||
|---|---|---|---|---|---|---|---|---|---|
| Z value | P value | ||||||||
| Positive symptoms | 32.78 ± 3.42 | 31.97 ± 2.87 | 32.60 ± 2.88 | 32.60 ± 2.88 | 28.40 ± 2.88 | 23.40 ± 5.27 | 19.40 ± 5.94 | −2.032 | 0.042 |
| Negative symptoms | 32.01 ± 3.97 | 31.64 ± 4.21 | 31.40 ± 4.98 | 31.40 ± 4.98 | 28.80 ± 3.56 | 26.80 ± 4.97 | 25.80 ± 4.43 | −2.023 | 0.043 |
| Common symptoms | 52.43 ± 3.42 | 51.97 ± 2.78 | 51.00 ± 4.00 | 51.00 ± 4.00 | 46.60 ± 1.95 | 42.40 ± 3.21 | 39.40 ± 5.27 | −2.041 | 0.041 |
| Hallucinations | 5.60 ± 0.55 | 5.20 ± 0.55 | 5.60 ± 0.55 | 5.60 ± 0.55 | 4.60 ± 0.55 | 3.60 ± 0.55 | 3.00 ± 0.71 | −2.06 | 0.039 |
| Delusions | 6.00 ± 0.00 | 5.60 ± 0.45 | 6.00 ± 0.00 | 6.00 ± 0.00 | 5.20 ± 0.45 | 4.40 ± 0.89 | 3.80 ± 1.10 | −2.07 | 0.038 |
| Total score | 117.00 ± 8.12 | 115.42 ± 7.02 | 115.00 ± 7.45 | 115.00 ± 7.45 | 103.80 ± 3.63 | 92.60 ± 9.04 | 84.60 ± 9.96 | −2.023 | 0.043 |
Table 3.
SF‐36 and FFMQ scale score changes
| Baseline | 4 wk after | 8 wk after | 8 mo after | Baseline vs 8 y later | ||
|---|---|---|---|---|---|---|
| Z value | P value | |||||
| SF‐36 | ||||||
| Physical functioning | 65.00 ± 20.31 | 72.00 ± 13.51 | 78.00 ± 14.83 | 85.00 ± 14.58 | −2.070 | 0.038 |
| Role‐physical | 35.00 ± 41.83 | 45.00 ± 44.72 | 60.00 ± 37.91 | 70.00 ± 44.72 | −1.732 | 0.083 |
| Bodily pain | 77.80 ± 22.63 | 83.00 ± 24.45 | 82.00 ± 14.28 | 92.80 ± 16.10 | −1.604 | 0.109 |
| General health | 52.00 ± 7.58 | 61.00 ± 20.43 | 68.00 ± 21.68 | 79.00 ± 16.73 | −2.032 | 0.042 |
| Vitality | 61.00 ± 20.43 | 74.00 ± 21.62 | 79.00 ± 19.17 | 83.00 ± 15.65 | −2.041 | 0.041 |
| Social functioning | 55.00 ± 28.78 | 67.50 ± 24.37 | 80.00 ± 27.39 | 85.00 ± 27.10 | −1.857 | 0.063 |
| Role‐emotional | 53.32 ± 44.73 | 60.00 ± 43.47 | 60.00 ± 43.47 | 66.66 ± 47.15 | −1.342 | 0.180 |
| Mental health | 59.20 ± 10.73 | 64.80 ± 12.13 | 73.60 ± 8.30 | 77.60 ± 6.07 | −2.032 | 0.042 |
| FFMQ | ||||||
| Observing | 15.40 ± 6.08 | 18.40 ± 6.47 | 23.00 ± 5.19 | 25.00 ± 4.83 | −1.219 | 0.223 |
| Describing | 23.00 ± 3.54 | 24.00 ± 3.32 | 26.20 ± 5.40 | 28.60 ± 6.88 | −1.604 | 0.109 |
| Acting with awareness | 14.20 ± 4.44 | 16.60 ± 5.81 | 19.40 ± 5.55 | 21.20 ± 7.12 | −2.023 | 0.043 |
| Nonjudging of inner experience | 20.60 ± 8.10 | 21.60 ± 9.23 | 24.00 ± 6.82 | 27.60 ± 5.60 | −2.032 | 0.042 |
| Nonreactivity to inner experience | 17.20 ± 6.69 | 21.40 ± 4.98 | 23.00 ± 3.08 | 25.80 ± 5.17 | −2.023 | 0.043 |
| Total score | 97.60 ± 25.52 | 103.80 ± 21.06 | 113.00 ± 19.79 | 125.80 ± 23.05 | −2.023 | 0.043 |
In present study, we reported the effectiveness of 8‐month mindfulness meditation intervention in five severe schizophrenia patients with more than 20 years’ medical history. There are several potential mechanisms underlying the interventional effects of mindfulness meditation on hallucination and delusion. First, mindfulness meditation produces brain oscillation changes and increases brain network integration,7 which could contribute to the decreased abnormal brain activities and reduced hallucination/delusion. Second, mindfulness training increases acceptance and ameliorates anxiety/distress emotion, resulting in general improvement in psychotic symptoms.
In the future, it will be important to investigate the meditation‐evoked brain changes to further elucidate the potential mechanisms of the benefits from intervention. One limitation of the current study, however, is the small sample size and the lack of a proper control. Larger randomized clinical trials are yet required to confirm the efficacy of mindfulness training in treatment of chronic schizophrenia patients.
In conclusion, our results demonstrated the promising potential of mindfulness meditation on the management of severe chronic schizophrenia patients.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The study is supported by National Key R&D Program of China (2017YFC0909200); the National Natural Foundation of China (81671336); SJTU Joint Medical and Engineering Funding (YG2016ZD06), and SJTU Joint Art and Science Funding (14JCRZ05); Shanghai Key laboratory of Psychotic Disorders (13dz2260500). The funds provide support for research materials used in present study.
REFERENCES
- 1. Pascoe MC, Thompson DR, Jenkins ZM, Ski CF. Mindfulness mediates the physiological markers of stress: Systematic review and meta‐analysis. J Psychiatric Res. 2017;95:156‐178. [DOI] [PubMed] [Google Scholar]
- 2. Xue T, Li H, Wang MT, et al. Mindfulness meditation improves metabolic profiles in healthy and depressive participants. CNS Neurosci Ther. 2018;24(6):572‐574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Deckersbach T, Holzel BK, Eisner LR, et al. Mindfulness‐based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neurosci Ther. 2012;18(2):133‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chien WT, Thompson DR. Effects of a mindfulness‐based psychoeducation programme for Chinese patients with schizophrenia: 2‐year follow‐up. Brit J Psychiatry. 2014;205(1):52‐59. [DOI] [PubMed] [Google Scholar]
- 5. Tabak NT, Horan WP, Green MF. Mindfulness in schizophrenia: Associations with self‐reported motivation, emotion regulation, dysfunctional attitudes, and negative symptoms. Schizophr Res. 2015;168(1–2):537‐542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Johnson DP, Penn DL, Fredrickson BL, et al. A pilot study of loving‐kindness meditation for the negative symptoms of schizophrenia. Schizophr Res. 2011;129(2–3):137‐140. [DOI] [PubMed] [Google Scholar]
- 7. van Lutterveld R, van Dellen E, Pal P, Yang H, Stam CJ, Brewer J. Meditation is associated with increased brain network integration. NeuroImage. 2017;158:18‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]


