Abstract
Objective
We assessed pain and anxiety using psychological testing instruments (State-Trait Anxiety Inventory for Children, visual analog scale) and a physiological testing instrument (salivary cortisol hormone level) after the insertion of orthodontic appliances and during the initial alignment phase of orthodontic treatment.
Methods
The study group involved two groups matched according to age and gender. Group 1 used 0.016-, 0.016×0.016-, and 0.16×0.22-inch and Group 2 used 0.014-, 0.016-, and 0.016×0.016-inch superelastic nickel-titanium archwires in the initial alignment phase of treatment. Pain and anxiety instruments were applied, and saliva samples were collected from the patients before and after molar band insertions, and bracket and initial archwire placement, and 7 days after the initial bonding and archwire replacements.
Results
Cortisol levels and state anxiety scores revealed statistically significant differences within groups (p<0.01, p<0.05). No significant differences were found between Group 1 and Group 2 in cortisol hormone levels, anxiety scores, or pain measurements (p>0.05). Although not statistically significant, the most severe pain was measured in the posterior teeth after band insertion and in the anterior teeth after the first archwire insertion (p>0.05).
Conclusion
Orthodontic appliances and the initial alignment phase of orthodontic treatment affect patients’ anxiety and cortisol hormone levels. Both archwires were equally effective with regard to perceived pain, anxiety, and stress hormone levels.
Keywords: Anxiety, cortisol, NiTi arcwires, orthodontic pain, visual analogue scale
INTRODUCTION
Orthodontic appliance-induced pain or discomfort is reported by up to 95% of patients, and it has been cited as a reason for discontinuation of treatment and may negatively affect patient cooperation (1–3). The level of pain varies according to the use of different appliance types. Fixed orthodontic appliances cause more pressure, discomfort, and pain than removable appliances (4). Nickel-titanium (NiTi) archwires are used during the initial phase of fixed orthodontic treatment for tooth alignment and leveling. These archwires produce light continuous forces with less patient discomfort and tissue trauma (5–7).
Litt (8) emphasized the effects of anxiety on pain sensation and reported that in clinical situations of acute pain, anxiety, and pain may be indistinguishable. Anxiety reduces the pain threshold and can cause the perception of “painless” stimuli as painful. Dental stimuli are also capable of provoking anxiety; Sergl et al. (9) reported that individual stress-related factors and anxiety influence the intensity of discomfort caused by orthodontic appliances. Pain measurements should be made with an assessment of the patient’s anxiety level (10).
Stress is commonly defined as the physiological and psychological reactions that mobilize an organism’s defenses against external or internal stressors. The anxiety-induced stressor causes activation of the hypothalamus-pituitary-adrenal axis, with increased secretion of cortisol (11,12). Cortisol levels may be measured in saliva, which can be collected readily and safely in a stress-free and non-invasive manner (13).
The two most important aspects of pain and discomfort in orthodontic treatment are its intensity and duration. Understanding these has clinical implications to improve patient satisfaction and the quality of oral health (14). In light of the importance of this mostly overlooked issue, we aimed to assess pain and anxiety using psychological testing instruments (State-Trait Anxiety Inventory for Children [STAIC], visual analog scale [VAS]) and a physiological testing instrument (mid-morning salivary cortisol) after insertion of orthodontic appliances and during the initial alignment and leveling phase of orthodontic treatment
METHODS
Study Group and Clinical Management
The study group consisted of 20 patients (10 girls, 10 boys, mean age 12.83±0.71 years), who visited the Department of Orthodontics of Suleyman Demirel University for orthodontic treatment. The patients were informed about the fixed orthodontic treatment procedures, and informed consent to participate in this study was obtained from all patients. The study protocol was approved by the Research Ethics Committee of the Faculty of Medicine, University of Suleyman Demirel, Isparta (protocol number: B.30.2.SDU.0.01.00.14/219).
Patients were selected for this study based on the following inclusion criteria: (1) they required upper and lower fixed orthodontic treatment (without additional appliances, such as a quad helix, transpalatal arch, or headgear, which can cause additional discomfort); (2) they had mild crowding (1–4 mm) in the mandibular anterior teeth; (3) they had no previous active orthodontic treatment; (4) they had no history of medical problems, including diseases of the endocrine or metabolic systems or medications that could influence pain perception and cortisol levels; and (5) they agreed to participate in the study.
Exclusion criteria were the following: (1) the presence of a severe deep bite that could affect the bracket insertion at the initial bonding appointment; (2) malocclusion correction requiring treatment procedures other than continuous archwires and non-extraction protocols; (3) previous active orthodontic treatment; (4) medical problems/medications that could interfere with cortisol levels; and (5) regular use of analgesics for dental or orofacial pain.
Initial crowding was assessed using Little’s irregularity index (15) with digital calipers to an accuracy of 0.01 mm. Patients were matched into groups according to age and gender. Group 1 (5 females, 5 males, mean age 12.6±0.65 years) used 0.016-, 0.016×0.016-, and 0.16×0.22-inch superelastic NiTi memory archwires (American Orthodontics, Sheboygan, WI, USA) in the initial alignment stage of orthodontic treatment. Group 2 (5 females, 5 males, mean age 13.06±0.72 years) used 0.014-, 0.016-, and 0.016×0.016-inch superelastic NiTi memory archwires (American Orthodontics) in the initial alignment stage of orthodontic treatment.
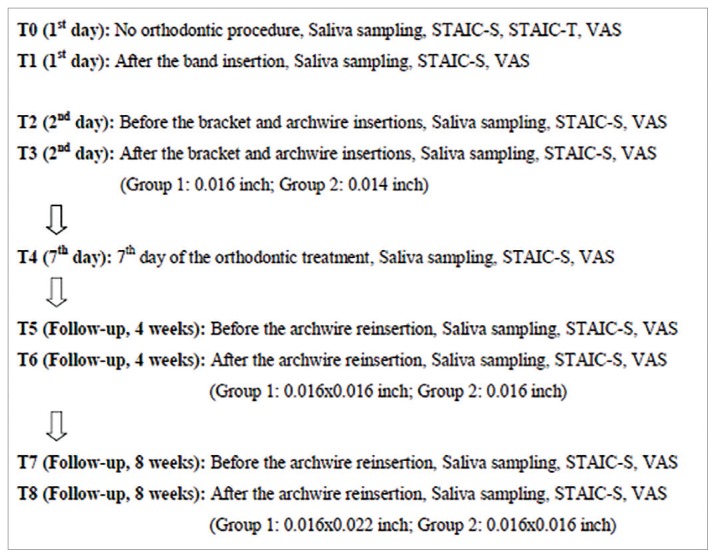
On the first day of orthodontic treatment, molar bands were placed on the first permanent molars. On the next day, 0.018-inch-slot Roth brackets (Mini Master Series, American Orthodontics) were bonded to the buccal surfaces of the upper incisors, canines, and premolars of all patients. Then, a 0.016-inch pre-formed archwire was inserted into the slots of brackets in Group 1, and a 0.014-inch pre-formed archwire was used in Group 2, then fixed with 0.010-inch stainless-steel ligature wires. On the morning of the 7th day, the control appointment was made. The patients were recalled at monthly intervals for 2 months during the stuhdy period, and archwire reinsertions were carried out each month for both groups. The progress of the study is shown in Figure 1.
Figure 1.
Flow chart demonstrating study design
Saliva Collection and Cortisol Assay
Saliva samples were collected from the patients before and after the molar band insertion (T0 and T1 time points), before and after the bracket and archwire insertion (T2 and T3 time points), 7 days after bracket bonding and initial archwire insertion (T4 time point), and before and after archwire reinsertions (T5, T6, T7, and T8 time points).
Patients were requested not to consume any food or drink an hour before saliva collection; only water was allowed. Saliva was collected into a polypropylene tube for 3 min while the patient was in a normal sitting position. Saliva samples were stored in the freezer at −80°C until the analysis. Cortisol levels in saliva were analyzed by an electrochemiluminescence immunoassay, using the Cobas cortisol kit (Roche Diagnostics, USA) on an Cobas e601 immunoassay system (Roche Diagnostics, Mannheim, Germany) (16).
Assessment of Anxiety
The STAIC consists of two 20-item self-reported scales that were designed for children to measure state and trait anxiety levels. The STAIC state anxiety scale (range 20–60) was used in this study to measure transitory emotional state or a condition characterized by subjective, consciously perceived feelings of tension, apprehension, and worry that vary in intensity and fluctuate over time. The STAIC trait anxiety scale measures how children generally feel, as well as relatively stable individual differences in anxiety proneness (17). In this study, to measure anxiety, patients were asked to fill in the STAIC state anxiety scale at 9 time points (T0, T1, T2, T3, T4, T5, T6, T7, and T8) and the trait anxiety scale at 1 time point (T0).
Assessment of Pain
Pain perception was measured before and after orthodontic procedures using a VAS, which is a 100-mm-long horizontal line with defined end points. One end of the line was labeled “no pain” and the other as “worst pain possible” (18). The VAS is a valid, sensitive, and reliable scale for pain assessment (1, 5, 19). In this study, the patients were asked separately at 9 time points (T0, T1, T2, T3, T4, T5, T6, T7, and T8) whether they had pain and in which areas (anterior/posterior teeth) they perceived the pain. Each patient was asked to place a mark on the line nearest to his or her perceived pain. The mark was then measured from the left margin of the line to the nearest millimeter to quantify the pain, recorded as the VAS score in mm.
Statistical Analysis
All analyses were conducted using the Statistical Package for Social Sciences software version 22.0 (IBM Corp.; Armonk, NY, USA). The Mann-Whitney U test was used to compare differences between archwire groups (Group 1 vs. 2) and gender groups (female vs. male) at the same times of the study. Friedman’s two-way analysis of variance for repeated measures was used to test for within-archwire group differences over time. The significance level was set at p<0.05.
RESULTS
Gender differences were not statistically significant in salivary cortisol levels, anxiety scores, or pain perception (p>0.05), so these findings were evaluated without gender discrimination.
Salivary Cortisol Values
The means and standard deviations (SDs) of the salivary cortisol values are listed in Table 1. Salivary cortisol values were similar and not statistically significant in Group 1 (p>0.05). Statistically significant differences were found in Group 2 (p<0.01), and the highest salivary cortisol values were found at the T3 time point in Group 2. No statistically significant differences were observed in mean salivary cortisol values between Groups 1 and 2 at any time point (p>0.05).
Table 1.
Means and SDs of the salivary cortisol levels (μg/dL) at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95% Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T0 | 0.39±0.03 | 0.31 | 0.47 | 0.41±0.04b | 0.31 | 0.51 | 0.684 |
| T1 | 0.51±0.04 | 0.41 | 0.61 | 0.52±0.06ab | 0.38 | 0.66 | 0.853 |
| T2 | 0.50±0.07 | 0.32 | 0.68 | 0.51±0.04ab | 0.41 | 0.61 | 0.684 |
| T3 | 0.57±0.07 | 0.40 | 0.74 | 0.59±0.03a | 0.50 | 0.68 | 0.579 |
| T4 | 0.46±0.03 | 0.38 | 0.55 | 0.44±0.03b | 0.36 | 0.53 | 0.684 |
| T5 | 0.44±0.03 | 0.35 | 0.52 | 0.42±0.05b | 0.30 | 0.53 | 0.481 |
| T6 | 0.45±0.05 | 0.33 | 0.57 | 0.42±0.03b | 0.34 | 0.51 | 0.739 |
| T7 | 0.38±0.03 | 0.31 | 0.45 | 0.38±0.03b | 0.29 | 0.47 | 1.000 |
| T8 | 0.41±0.02 | 0.35 | 0.48 | 0.40±0.02b | 0.33 | 0.47 | 0.579 |
| p | 0.068 | 0.004** | |||||
p<0.01; superscript letters indicate the differences between the time points
State-Trait Anxiety Values
The means and SDs of the state anxiety values are listed in Table 2. There were statistically significant differences in the state anxiety values for Groups 1 (p<0.01) and 2 (p<0.05). In Group 1, state anxiety values increased gradually and significantly after the first appointment. The T3 state anxiety values were significantly higher than at other time points (T0 and T8). In Group 2, the highest state anxiety values were determined between the T1 and T5 time points, and compared with the other time points, they increased significantly after the T0 time point. Table 3 lists the means and SDs of the trait anxiety values. No statistically significant difference was observed in trait anxiety levels between the groups (p>0.05).
Table 2.
Means and SDs of the state anxiety scores at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95% Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T0 | 37.00±1.74a | 33.05 | 40.95 | 37.20±1.05a | 34.82 | 39.58 | 0.579 |
| T1 | 42.10±1.13bc | 39.52 | 44.68 | 42.60±1.09b | 40.12 | 45.08 | 0.579 |
| T2 | 43.20±1.12bc | 40.66 | 45.74 | 43.00±1.13b | 40.43 | 45.57 | 0.971 |
| T3 | 43.40±1.57c | 39.84 | 46.96 | 42.90±1.75b | 38.93 | 46.87 | 0.912 |
| T4 | 42.40±1.46bc | 39.07 | 45.72 | 42.20±1.01b | 39.89 | 44.51 | 1.000 |
| T5 | 42.50±1.15bc | 39.88 | 45.12 | 41.90±1.36b | 38.80 | 45.00 | 0.853 |
| T6 | 41.30±1.13bc | 38.73 | 43.87 | 40.90±0.93ab | 38.78 | 43.02 | 1.000 |
| T7 | 40.70±1.02bc | 38.39 | 43.01 | 40.60±0.90ab | 38.54 | 42.66 | 1.000 |
| T8 | 38.80±1.27ab | 35.92 | 41.68 | 39.50±0.83ab | 37.61 | 41.38 | 0.529 |
| p | 0.005** | 0.043* | |||||
p<0.05;
p<0.01; superscript letters indicate the differences between the time points
Table 3.
Means and SDs of the trait anxiety scores at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95% Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T0 | 33.10±1.17 | 30.43 | 35.76 | 34.10±1.42 | 30.87 | 37.32 | 0.631 |
VAS Values and Pain Regions
The means and SDs of the VAS scores are listed in Table 4. Statistically significant differences were found in Groups 1 and 2 (p<0.001). The peak for pain intensity was recorded at the T3 time point in both groups, and it started to decline after the T3 time point.
Table 4.
Means and SDs of the VAS scores at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95% Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T1 | 28.50±4.94ac | 17.31 | 39.69 | 25.50±6.60ac | 10.57 | 40.43 | 0.853 |
| T2 | 17.50±4.78bcd | 6.67 | 28.33 | 19.00±5.46bc | 6.63 | 31.37 | 0.912 |
| T3 | 35.00±5.42a | 22.72 | 47.27 | 38.00±4.16a | 28.58 | 47.42 | 0.631 |
| T4 | 14.75±3.30bc | 7.28 | 22.22 | 16.00±3.63bc | 7.77 | 24.23 | 0.796 |
| T5 | 2.00±1.33d | −1.02 | 5.02 | 2.00±2.00de | −2.52 | 6.52 | 0.796 |
| T6 | 8.00±2.90bd | 1.43 | 14.57 | 13.00±4.72bce | 2.31 | 23.69 | 0.579 |
| T8 | 3.50±2.36bd | −1.84 | 8.84 | 4.00±2.21bd | −1.00 | 9.00 | 0.796 |
| p | 0.000*** | 0.000*** | |||||
p<0.001; superscript letters indicate the differences between the time points
The means and SDs of the VAS scores in the anterior teeth are listed in Table 5. VAS scores in the anterior teeth showed statistically significant differences in Groups 1 and 2 (p<0.001). The T3 VAS scores were significantly greater than at other time points (T5 and T8) for both groups.
Table 5.
Means and SDs of the VAS scores in the anterior teeth at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95% Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T3 | 28.50±7.45a | 11.63 | 45.36 | 40.00±5.05a | 28.56 | 51.44 | 0.247 |
| T4 | 28.00±7.85a | 10.22 | 45.78 | 25.00±7.49b | 8.05 | 41.94 | 0.684 |
| T5 | 6.00±2.66bc | −0.03 | 12.03 | 11.00±4.33bd | 1.20 | 20.80 | 0.529 |
| T6 | 13.50±4.83ac | 2.57 | 24.43 | 18.00±5.73bd | 5.03 | 30.97 | 0.579 |
| T8 | 5.50±2.83bc | −0.91 | 11.91 | 3.00±2.13cd | −1.83 | 7.83 | 0.684 |
| p | 0.000*** | 0.000*** | |||||
p<0.001; superscript letters indicate the differences between the time points
The means and SDs of the VAS scores in the posterior teeth are listed in Table 6. VAS scores in the posterior teeth showed statistically significant differences in Groups 1 and 2 (p<0.001). Severe pain was perceived in the posterior teeth at the T1 time point in both groups.
Table 6.
Means and SDs of the VAS scores in the posterior teeth at each time point
| Group 1 | Group 2 | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Time points | X̄±SD | 95%Confidence interval | X̄±SD | 95% Confidence interval | p | ||
|
|
|
||||||
| Lower bound | Upper bound | Lower bound | Upper bound | ||||
| T1 | 30.50±5.39a | 18.29 | 42.71 | 41.00±5.55a | 28.43 | 53.57 | 0.105 |
| T2 | 14.75±3.30ac | 7.28 | 22.22 | 16.00±3.63bc | 7.77 | 24.23 | 0.796 |
| T3 | 18.50±6.23ac | 4.39 | 32.61 | 22.25±5.35b | 10.14 | 34.36 | 0.481 |
| T4 | 12.00±4.42bc | 1.99 | 22.00 | 16.00±5.46bc | 3.63 | 28.37 | 0.684 |
| T6 | 4.00±2.66b | −2.03 | 10.03 | 12.00±4.66bc | 1.44 | 22.56 | 0.247 |
| T8 | 1.00±1.00b | −1.26 | 3.26 | 4.00±2.21c | −1.00 | 9.00 | 0.436 |
| p | 0.000*** | 0.000*** | |||||
p<0.001; superscript letters indicate the differences between the time points
DISCUSSION
Many studies have investigated the degree of pain during the insertion of separators, bands, braces, and archwires (5, 7, 14, 20–23). However, to the best of our knowledge, no reports have documented the evaluation of pain, stress, and anxiety among preadolescent patients using psychometric and physiological methods after the insertion of orthodontic appliances and during the initial aligning phase of orthodontic treatment.
Sandhu and Sandhu (21) reported that orthodontic pain was affected significantly by the individual’s age and gender. Biophysiological, psychosocial, and physical factors can contribute to the age and gender interactions and affect pain perception during adolescence. Pain perception among boys and girls changes after puberty, and girls tend to report more pain, due to fluctuations in hormone levels during the menstrual cycle (24). Considering the effects of these factors, the age group used in the present study represented early adolescence (11–14 years), according to the criteria of early adolescence of the American Academy of Pediatrics (25).
In this study, saliva samples of each individual were taken at the same time in the morning, and a sample taken before the molar band placement with no application of any procedure served for each individual as his or her own control. Salivary cortisol values were generally higher after the molar band placement (T1) and bracket and archwire insertion (T3). Similarly, Gecgelen et al. (1) found that salivary cortisol levels were higher on the day the maxillary expansion appliance was cemented on the teeth. The difference could probably be due to these procedures creating anxiety and pain in patients. At later time points, cortisol values were similar to those in the control saliva samples; patients may have adapted to the appliances and orthodontic-induced pain.
Following the molar band placement, patients began to feel pain, and cortisol values and state anxiety scores increase. This was an expected result, in that anxiety/pain exhibited a parallel relationship with cortisol levels.
In this study, we found no statistically significant differences between salivary cortisol and gender. The present results were consistent with previous studies (1, 12, 13, 26), in that gender did not influence cortisol secretion.
State anxiety values increased gradually after the first orthodontic treatment appointment. It is clear from the existing literature that orthodontic procedures, such as band placement, archwire insertion, and activation, are stressful and anxiety-provoking procedures in orthodontics. Although patients were informed about their orthodontic treatment, their concerns about the treatment process, and dental anxiety and fear from the beginning of the treatment, caused a sense of discomfort. State anxiety values decreased from the 7th day of the orthodontic treatment to the end of study period. The patients may have adapted to orthodontic appliances over a period of time.
Although some studies reported higher levels of anxiety among females than males (27, 28), we observed no significant gender difference in the state or trait anxiety levels, consistent with other studies (1, 13). This may be because gender differences in anxiety and depression emerge after puberty.
Trait anxiety levels of patients were determined at the beginning of the treatment in this study. One limitation of this study was not assessing the trait anxiety scores at the end of the study period. We observed no difference between the groups in terms of trait anxiety values, and the pretreatment values were similar to pretreatment values reported in other studies (1, 29).
Following band insertion, the patients started to feel discomfort and pain. We found statistically significant differences between the pain perceived by those in whom different-sized archwires were inserted and different procedures were performed. However, we observed no statistically significant differences between the groups. The most severe pain was measured for the posterior teeth after the band insertion and for the anterior teeth after the first archwire insertion. Rakshan and Rakshan (14) reported that discomfort and pain caused in the initial stage of fixed orthodontic treatment can be moderate to severe and might last for more than 1 month. Generalized dentogingival discomfort is more prevalent than localized discomfort.
We found no significant difference between pain and gender, consistent with the findings of Cesur and Aksoy (2), Abdelrahman et al. (7), Sandhu and Sandhu (21), and Erdinç and Dinçer (23). We also found no statistically significant difference between the archwire groups for overall pain measurements. Erdinç and Dinçer (23) found no statistically significant difference in terms of perception of pain between the 0.014- and 0.016inch groups during the first week of initial alignment. Sandhu and Sandhu (5) found no statistically significant difference between 0.016-inch superelastic NiTi and 0.0175-inch multistranded stainless steel for overall pain experience. Similarly, Abdelrahman et al. (6) reported that the three forms of archwires used (0.014-inch superelastic NiTi, 0.014-inch thermoelastic NiTi, and 0.014-inch conventional NiTi) yielded similar pain intensities during the initial aligning stage of fixed orthodontic treatment. These findings are in accordance with our results.
This study was limited in some aspects. We used psychological and physiological testing instruments to assess pain and anxiety during the different stages of fixed orthodontic treatment with a limited sample size. Future studies should be conducted on larger sample sizes and should be determined by power calculations.
CONCLUSION
We assessed pain and anxiety after the insertion of orthodontic appliances and during the initial alignment and leveling phase of orthodontic treatment for mild crowding. Gender differences were not statistically significant in salivary cortisol levels, anxiety scores, and pain perception. Orthodontic appliances and the initial alignment phase of orthodontic treatment affect patients’ anxiety and cortisol levels. Pain was perceived after the insertion of the bands and wires of different sizes used for initial alignment.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Research Ethics Committee of the University of Süleyman Demirel School of Medicine (Protocol Number: B.30.2.SDU.0.01.00.14/219).
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Supervision - A.A., M.G.C.; Design - A.A., M.G.C.; Supervision - A.A.; Resources - A.A.; Materials - F.G., B.H.D., G.K.; Y.A.Ö.; Materials - F.G., B.H.D., G.K., Y.A.Ö.; Data Collection and/or Processing - G.K., Y.A.Ö., F.G., B.H.D.; Analysis and/or Interpretation - A.A.; Literature Search - M.G.C., A.A.; Writing Manuscript - A.A., M.G.C.; Critical Review - A.A., M.G.C.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: This work was supported by the Süleyman Demirel University Scientific Research Projects Unit (2494-M-10).
REFERENCES
- 1.Gecgelen M, Aksoy A, Kirdemir P, Doguc DK, Cesur G, Koskan O, et al. Evaluation of stress and pain during rapid maxillary expansion treatments. J Oral Rehabil. 2012;39:767–75. doi: 10.1111/j.1365-2842.2012.02330.x. [DOI] [PubMed] [Google Scholar]
- 2.Cesur MG, Aksoy A. Evaluation of Perceived Pain During the First Week of Rapid Maxillary Expansion Treatment. Meandros Med Dent J. 2018;19:39–44. doi: 10.4274/meandros.02411. [DOI] [Google Scholar]
- 3.Mangnall LAR, Dietrich T, Scholey JM. A randomized controlled trial to assess the pain associated with the debond of orthodontic fixed appliances. J Orthod. 2013;40:188–96. doi: 10.1179/1465313313Y.0000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuncer Z, Ozsoy FS, Polat-Ozsoy O. Self-reported pain associated with the use of intermaxillary elastics compared to pain experienced after initial archwire insertion. Angle Orthod. 2011;81:807–11. doi: 10.2319/092110-550.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandhu SS, Sandhu J. A randomized clinical trial investigating pain associated with superelastic nickel-titanium and multistranded stainless steel archwires during the initial leveling and aligning phase of orthodontic treatment. J Orthod. 2013;40:276–85. doi: 10.1179/1465313313Y.0000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abdelrahman RS, Al-Nimri KS, Al Maaitah EF. Pain experience during initial alignment with three types of nickel-titanium archwires: A prospective clinical trial. Angle Orthod. 2015;85:1021–6. doi: 10.2319/071614-498.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdelrahman RSh, Al-Nimri KS, Al Maaitah EF. A clinical comparison of three aligning archwires in terms of alignment efficiency: A prospective clinical trial. Angle Orthod. 2015;85:434–9. doi: 10.2319/041414-274.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Litt MD. A model of pain and anxiety associated with acute stressors: distress in dental procedures. Behav Res Ther. 1996;34:459–76. doi: 10.1016/0005-7967(96)00015-0. [DOI] [PubMed] [Google Scholar]
- 9.Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop. 1998;114:684–91. doi: 10.1016/S0889-5406(98)70201-X. [DOI] [PubMed] [Google Scholar]
- 10.Otasevic M, Naini FB, Gill DS, Lee RT. Prospective randomized clinical trial comparing the effects of a masticatory bite wafer and avoidance of hard food on pain associated with initial orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:6.e9–6.e15. doi: 10.1016/j.ajodo.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 11.Doepel M, Soderling E, Ekberg EL, Nılner M, Le Bell Y. Salivary cortisol and IgA levels in patients with myofascial pain treated with occlusal appliances in the short term. J Oral Rehabil. 2009;36:210–6. doi: 10.1111/j.1365-2842.2008.01923.x. [DOI] [PubMed] [Google Scholar]
- 12.Benjamins C, Asscheman H, Schuurs AH. Increased salivary cortisol in severe dental anxiety. Psychophysiology. 1992;29:302–5. doi: 10.1111/j.1469-8986.1992.tb01703.x. [DOI] [PubMed] [Google Scholar]
- 13.Hashem AA, Claffey NM, O’Connell B. Pain and anxiety following the insertion of dental implants. Int J Oral Maxillofac Implants. 2006;21:943–50. [PubMed] [Google Scholar]
- 14.Rakhshan H, Rakhshan V. Pain and discomfort perceived during the initial stage of active fixed orthodontic treatment. Saudi Dent J. 2015;27:81–7. doi: 10.1016/j.sdentj.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–63. doi: 10.1016/0002-9416(75)90086-X. [DOI] [PubMed] [Google Scholar]
- 16.Vogeser M, Durner J, Seliger E, Auernhammer C. Measurement of late-night salivary cortisol with an automated immunoassay system. Clin Chem Lab Med. 2006;44:1441–5. doi: 10.1515/CCLM.2006.244. [DOI] [PubMed] [Google Scholar]
- 17.Spielberger CD, editor. Manual for the state-trait anxiety inventory for children. Consulting Psychologists Press; 1973. [Google Scholar]
- 18.Huskisson EC. Visual analogue scales. In: Melzack R, editor. Pain measurement and assessment. New York: Raven Press; 1983. pp. 33–7. [Google Scholar]
- 19.Abu Alhaija ES, Abu Nabaa MA, Al Maaitah EF, Al-Omairi MK. Comparison of personality traits, attitude toward orthodontic treatment, and pain perception and experience before and after orthodontic treatment. Angle Orthod. 2015;85:474–9. doi: 10.2319/121813-927.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Balbeesi HO, Bin Huraib SM, AlNahas NW, AlKawari HM, Abu-Amara AB, Vellappally S, et al. Pain and distress induced by elastomeric and spring separators in patients undergoing orthodontic treatment. J Int Soc Prev Community Dent. 2016;6:549–53. doi: 10.4103/2231-0762.195519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sandhu SS, Sandhu J. Orthodontic pain: an interaction between age and sex in early and middle adolescence. Angle Orthod. 2013;83:966–72. doi: 10.2319/030113-174.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campos MJS, Fraga MR, Raposo NRB, Ferreira AP, Vitral RWF. Assessment of pain experience in adults and children after bracket bonding and initial archwire insertion. Dental Press J Orthod. 2013;18:32–7. doi: 10.1590/S2176-94512013000500007. [DOI] [PubMed] [Google Scholar]
- 23.Erdinç AME, Dinçer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 24.Myers CD, Tsao JCI, Glover DA, Kim SC, Turk N, Zeltzer LK. Sex, gender, and age: contributions to laboratory pain responding in children and adolescents. J Pain. 2006;7:556–64. doi: 10.1016/j.jpain.2006.01.454. [DOI] [PubMed] [Google Scholar]
- 25.Greydanus DE, Bashe P. American Academy of Pediatrics Caring for Your Teenager: The Complete and Authoritative Guide. New York, NY: Bantam Books; 2003. [Google Scholar]
- 26.Blomqvist M, Holmberg K, Lindblad F, Fernell E, Ek U, Dahllöf G. Salivary cortisol levels and dental anxiety in childen with attention deficit hyperactivity disorder. Eur J Oral Sci. 2007;115:1–6. doi: 10.1111/j.1600-0722.2007.00451.x. [DOI] [PubMed] [Google Scholar]
- 27.Garip H, Abalı O, Göker K, Göktürk Ü, Garip Y. Anxiety and extraction of third molars in turkish patients. Br J Oral Maxillofac Surg. 2004;42:551–4. doi: 10.1016/S0266-4356(04)00139-1. [DOI] [PubMed] [Google Scholar]
- 28.Özusta ŞH. Çocuklar İçin Durumluk-Sürekli Kaygı Envanteri Uyarlama Geçerlik ve Güvenilirlik Çalışması. Türk Psikoloji Dergisi. 1995;10:32–44. [Google Scholar]
- 29.Karibe H, Shimazu K, Okamoto A, Kawakami T, Kato Y, Warita-Naoi S. Prevalence and association of self-reported anxiety, pain, and oral parafunctional habits with temporomandibular disorders in Japanese children and adolescents: a cross-sectional survey. BMC Oral Health. 2015;15:8. doi: 10.1186/1472-6831-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]