Abstract
Objectives:
Melanoma can be prevented through reducing sun exposure and detected early by increasing examination of skin for lesions. First-degree relatives of melanoma cases have higher risk than the general population and therefore could be targets of behavioral interventions through families. We tested the effects of a family-based web delivered intervention to melanoma families on the melanoma risk reduction behaviors of first-degree relatives of melanoma cases.
Methods:
A total of 313 families that included one first-degree relative were recruited to join this randomized trial. All intervention families received access to the Suntalk website developed to promote family communication and behavioral risk reduction among families of melanoma survivors.
Results:
First degree relatives in the intervention arm significantly increased their yearly performance of both skin self examination and thorough provider examination from baseline to 12-month follow-up while the control FDRs decreased their yearly performance of both of those behaviors (p’s =.006 and .005 respectively). Several sun protection behaviors increased significantly in FDRs in the intervention arm but not the control arm, including wearing a covering on the head (p=.005), staying in available shade (p=.008), and avoiding sun exposure during peak hours (p=.010). Some of these changes were mediated by perceptions of risk and other process variables.
Conclusions:
A web-based intervention can reduce risk of melanoma through changes in relevant behaviors among first-degree relatives of melanoma survivors. Future research should identify methods for making this type of intervention accessible to more families and for broadening the reach to other types of cancer families.
Practice Implications:
This program can be provided to melanoma families to improve their sun protection and screening behaviors, at the point of diagnosis.
Keywords: Melanoma, Family, Prevention, Sun exposure, First-degree relatives
Introduction:
Melanoma is the most serious and potentially fatal form of skin cancer, and it is among the top five most prevalent cancers in the United States [1]. First-degree relatives (FDRs, defined as parents, children, and siblings) of melanoma patients are at two to fivefold increased risk of developing melanoma themselves [2]. One of the primary environmental risk factor for melanoma involves ultraviolet radiation exposure delivered via sunlight or indoor tanning facilities [3], thus, sun protection strategies, and avoidance of indoor tanning, are part of melanoma risk reduction. Additionally, given that melanomas largely arise on the skin surface, healthcare provider screening, where all areas of skin are carefully reviewed by a health care professional to identify cancerous or precancerous lesions, as well as self-screening (practiced deliberately and comprehensively) represent important opportunities for identification of melanomas at the earliest, most treatable stages.
Unfortunately, these risk-reducing behaviors are often not pursued by families in which a case of melanoma has been diagnosed. Less than half of first-degree relatives take precautionary measures to reduce sun exposure, and only about 15% of first-degree relatives of melanoma patients engaged in skin self-examination in the last year [4,5]. These relatively low levels of protective behaviors suggest the need for measures to convey information about risk and action to family members of melanoma patients, in order to reduce their risk of harm due to melanoma. Relatively infrequent communication between people diagnosed with cancer and their first-degree relatives may contribute to the problem [6.7].
We developed and evaluated a web-based intervention to promote family communication and information exchange about risk reduction in melanoma families, with the objective of improving familial transmission of helpful information as an encouragement to health behavior change. We selected melanoma as a disease site because it included both women and men, and because it is increasing in incidence and a relatively common cancer. We selected the world-wide-web as the communication system because of its versatility, flexibility, and high potential research into the general public, once evaluated. Our previous publications have documented the recruitment of families [8], baseline levels of melanoma prevention behaviors [9.10], and effects of the intervention on the case’s melanoma prevention behaviors and communication about melanoma [11]. This paper presents the effects of the intervention on sun protection behaviors and skin self- and provider examination in first-degree relatives. In addition, we measured perceived risk and cancer worry for developing melanoma in the future as potential precursors to protective behavior change; our study design allowed for prospective assessment in order to evaluate the components of an individual’s mental model of the disease that may influence risk-related behaviors. Here, we hypothesize that the intervention will have significant effects on FDRs’ sun protection behaviors, as was true for survivors.
Methods
Study sample
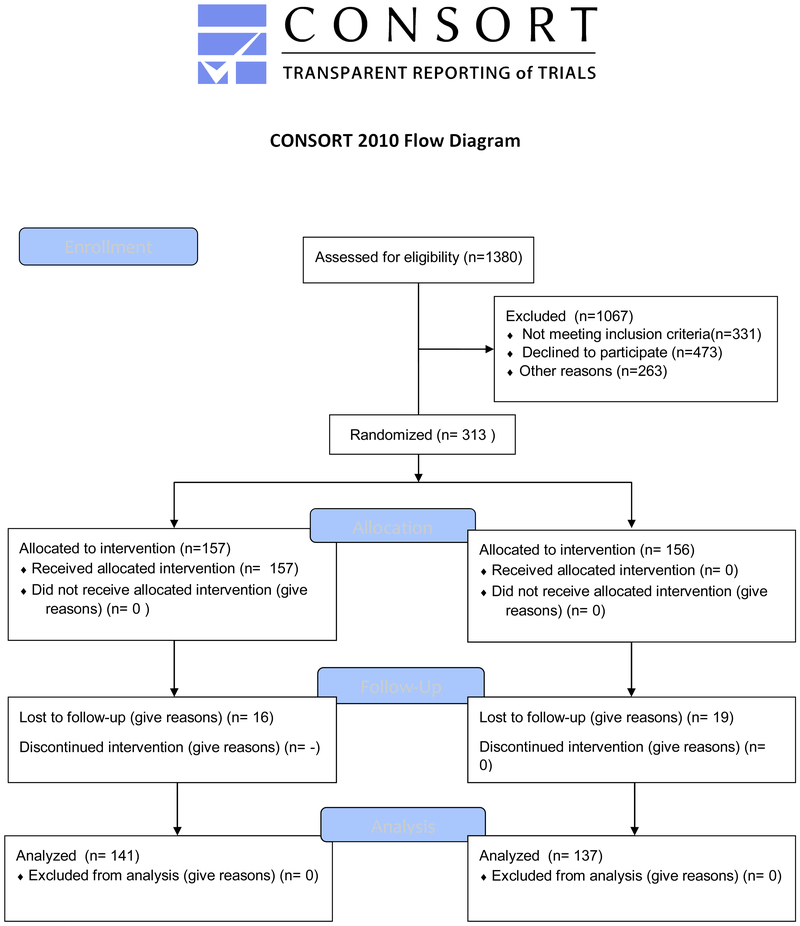
The data for these analyses are from the Suntalk Study, a randomized controlled trial of a web- based communication and support intervention funded by the National Cancer Institute (CA107430). A family was defined as a melanoma case, a first-degree relative (FDR) of the case, and one additional adult family member who is a parent of a child 0-18 years. These families are likely composed of sporadic cases of melanoma, although some of the families had more than one case of melanoma reported. All participants were recruited and assessed via a telephone survey at baseline, and then families were randomized to either an immediate intervention group or a delayed comparison group. Intervention families received access to the study website, which was an interactive communication-oriented system, for approximately one year. Enrolled family members completed a follow-up survey one year later, and then the comparison families received access to the study website. This paper focuses on outcomes measured in FDRs. This report includes all Consolidated Standards of Reporting Trials (CONSORT; 12) required elements, and all study procedures were approved by the Institutional Review Board (IRB) of the Fred Hutchinson Cancer Research Center. No author reported a conflict of interest and this project was funded by the National Cancer Institute.
We used two sources for recruitment of families: 1) the Northwest Cancer Genetics Network (NWCGN) a regional site of the Cancer Genetics Network [13] and 2) The SEER registry (Cancer Surveillance System or CSS) at the Fred Hutchinson Cancer Research Center. Recruitment process and flow is described in detail in a previous manuscript [8]. Melanoma cases diagnosed with a first primary melanoma between April 1st 1998 and October 1st 2001 were recruited from the registries. The case eligibility criteria included a diagnosed with melanoma and being aged 18 years or older, and willing to provide their family contact information to the research team. FDRs were eligible if they were 18 years or older, a first-degree relative of the case, and did not have melanoma themselves. All participants had to have access to the Internet from a setting that would be comfortable for using the study website.
Recruitment Procedures
Recruitment and informed consent for each family consisted of three stages: physician, case, and relative. Prior to approaching the case, his/her physician of record was contacted by mail with a letter explaining the study and seeking feedback if the provider had any reason to believe the potential participant should not be approached. If there was no response from the physician after three weeks, the physician’s permission to contact the case was assumed. Each case was then mailed a letter and study brochure briefly describing the Suntalk Study and offering the opportunity to participate. The case passive consent letter, like the physician mailing, included the project’s phone number for anyone wanting to decline or refuse participation. Study staff contacted cases by telephone to screen for eligibility and interest. If the case was eligible and interested, project staff then collected the names, relationships, and contact information of all possible FDRs and parents. We enumerated the family of each case, and permission to contact was documented for each relative. This report was the basis for recruiting FDRs and parents. Finally, cases were asked to complete a baseline survey over the telephone, either immediately following the screening survey or at a later time. All of the FDRs and parents provided by the case were then approached using the same methods used to approach cases for participation. Once three family members (Case, FDR, Parent) completed the baseline survey, families were randomized using a statistician-generated random set of numbers to receive either the immediate intervention (50%) or to participate in the delayed intervention group that had access to the intervention only after final outcome assessments (50%). All data collection staff were unaware of study condition when collecting data.
Intervention
All family members were provided with unique links to the study website designed specifically for melanoma survivors and their family members. The website consisted of a home page with weekly rotating messages about prevention. Viewers were directed to a page that depicted their own personal risk for melanoma, based on a model developed by colleagues at Harvard University [14] called Your Chronic Disease Risk, using baseline data from each participant to complete the risk algorithm. The risk graphic included a thermometer shaped risk tool that provided an indication of the likelihood of future lifetime melanoma tailored to the individuals’ risk status and risk factors. The study website also linked to specific sites with more information. Additional sections from which the viewer could choose included how to reduce risk, how to prevent sun exposure, how to self-screen, how to request a skin screening from a provider, how to help protect children from sun exposure, and guides on how to talk about melanoma risk with a provider, with the family member who has had melanoma and with other family members about risk. The web site also included a chat room and an interactive section for family members. Viewers could select any or all pages and could view them as much as they desired to during the one year study period. Every three months prompts would be emailed by the study team to convey information of interest to participants and to remind them to use the website and to pay attention to melanoma prevention behaviors. The website assessed the number of times a user logged into the website and viewed at least one page. This continuous count of logins was coded dichotomously as 1 (1) or more than one time (2).
Outcome measures
At baseline and at one year after randomization, the following outcome measures were assessed by self-report:
Skin Self-examination.
We assessed whether FDRs performed deliberate and comprehensive skin self-examinations (SSE) of specific bodily areas at least once every two months. Body areas included: the front of the individual from the waist up, the front of the thighs and legs, the bottoms of the feet, the calves, the back of the thighs and legs, the buttocks and lower portion of the back, and the upper back [15]. We also explored whether or not individuals performed thorough skin examinations, looking for particular marks, freckles, or moles, or just casually checking their skin. Those marking “I do a thorough skin examination” were considered adherent to the protective behavior; all other methods were coded as “0”.
Sun protection behaviors.
Sun protection behaviors of the previous seven days were assessed (wearing a long-sleeved shirt or blouse, wearing long pants or skirts, wearing sunscreen with an SPF of 15 or higher, wearing something on the head such as a hat, cap, or scarf, and staying in available shade such as under a tree, awning or umbrella)6. Responses were dichotomized by those who responded “often” or “always” to the questions (adherence =1, non-adherent = 0). Given that sun protection likely varies across the seasons of the year, we adjusted all regressions for season. The month in which baseline data collection occurred for each participant was used to determine the season for each observation. The seasonal categories were organized such that winter included December through March, spring included April through June, summer included July through September, and fall included October through November. We labelled this seasonality.
Provider screening.
Skin screening conducted during a routine visit to a health care provider was assessed according to Weinstock and colleagues’ (17) prior research. Participants were asked “What does your provider do during a skin examination?” Participants could have checked any or all of the following response options: a) look at all areas of your skin that you are concerned about, b) check places exposed to the sun, c) look at all your moles or freckles, d) check all of your skin, by asking you to take your clothes off, e) take pictures of your skin to record changes, f) other. For the current analysis having all of one’s skin checked, without clothing, was used as a outcome measure of provider screening coded as 1. All other response options were coded as 0.
Process measures
We measured perceived risk for developing melanoma in the future by asking “What do you think your chances of getting melanoma are?” with a fill-in-the blank answer. Cancer worry, defined as an emotional reaction to the threat of cancer was assessed by calculating a summary score of 4-16 points, with those reporting a score of 8 or higher considered high worry and those with 7 and lower considered low worry. Family cohesion was measured using the Moos Family Environment Scale cohesion subscale, used to measure the cohesiveness of family as perceived by the respondent [22]. At baseline and follow-up we measured two other aspects of participants’ mental models of melanoma using items about melanoma prevention and severity developed for this study. Items included a question about tanning “Most people look better with a tan.” and a second question about ability to identify a lesion “How confident to you feel in noticing abnormal marks on skin during self-examination?” Both had 5-point response categories of 1=Not at all to 5=extremely. For all of these mental model questions we calculated changes scores from baseline to follow-up for the intervention group members to assess changes due to intervention.
Background variables
We collected background information from FDRs using standard questions on age, gender, ethnic/racial background: (White /Caucasian, Black or African-American, Native American or Aleut or Eskimo, Asian, Pacific Islander, Hawaiian, Spanish, Hispanic or Latino, other), education level (8 years or less, some high school, high school graduate or GED, some college or technical school, graduated from college or beyond), marital status (never married, married or living as married, separated, divorced, widowed), income (less than $15k, $15k-$30k, $31k-$50k, $51k-$70k, $71k-$99k, $100k or above). We used zip code to identify whether FDRs lived in the same city as the case and coded this as 0=not close and 1=close to case.
Analyses
Sample size was calculated with 80% power and a proposed effect size based on our previous research [29]. We first examined descriptive analyses of all variables to identify any outliers or aberrant data points. We found neither outliers nor aberrant data points. We then examined differences between intervention and control FDRs, and between participants who provided and did not provide follow-up data. We next examined the unadjusted outcomes of the study (sun protection behaviors, SSE and provider screening) using the measures described above as dichotomized outcome variables. We tested these measures with Cochran-Mantel-Haenszel tests after adjusting for season of the year. Finally, conducted mediational analysis using Baron and Kenny’s methods to identify any mediators of the intervention effects. We used mediation variables found to be related to the main outcomes of the study, as specified by Baron and Kenny [31]. We entered the mediation variables one by one to see if they contributed anything to the regression model above the powerful intervention effect, thus indicating mediation.
Results
We randomized 311 families, each with one case of melanoma, one FDR, and one parent of a child 0-17. Therefore, there were 311 FDRs of melanoma cases enrolled in the study. We were able to collect follow-up data on 89% of the FDRs at the one year follow-up, and there were no differences between intervention and control participants in provision of follow-up data. Table 1 presents the baseline demographic data of FDRs. As shown in this Table, the FDRs were almost all White, slightly more likely to be female than male, and mostly of moderate income and education. Overall, the randomization process worked well, in that there were no differences between intervention and control FDRs on any demographic variable or any outcome variable (data not shown).
Table 1:
Demographic characteristics of first-degree relatives (FDRs) in the Suntalk Study at baseline
| Variable | Categories | ||
|---|---|---|---|
| Age (years) | Average age (SD) | 51.32 | - |
| [Range] | [19-91] | - | |
| N | % | ||
| Gender | Female | 199 | 63.6% |
| Male | 114 | 36.4% | |
| Ethnicity | Hispanic | 1 | 0.3% |
| Non-Hispanic | 312 | 99.7% | |
| Race | White | 299 | 95.53% |
| Non-white | 14 | 4.47% | |
| Education | ≤ High school degree | 35 | 11.2% |
| Some college or technical school | 102 | 32.6% | |
| ≥ College degree | 176 | 56.2% | |
| Marital status |
Never married | 37 | 11.8% |
| Married or living as married | 225 | 71.9% | |
| Separated/Divorced | 33 | 10.5% | |
| Widowed | 18 | 5.7% | |
| Income | ≤ 50K | 96 | 30.7% |
| 51-70K | 55 | 17.6% | |
| ≥ 70K | 137 | 43.8% | |
| Refused/did not know | 25 | 8.0% |
As shown in Table 2, improvement in several melanoma risk reduction behaviors occurred for intervention FDRs compared to control FDRs. Specifically, FDRs in the intervention arm significantly increased their yearly performance of both SSE and thorough provider examination from baseline to 12-month follow-up while the control FDRs decreased their yearly performance of both of those behaviors. Intervention participants increased SSE from a baseline value of 14.65% to 31.7% at follow-up and provider examination from 14.65% to 41.67% (p’s =.006 and .005 respectively). Several sun protection behaviors increased significantly in FDRs in the intervention arm but not the control arm, including wearing a covering on the head (p=.005), staying in available shade (p=.008), and avoiding sun exposure during peak hours (p=.010).
Table 2.
Changes in risk reduction behaviors from before to after web-based intervention in FDRs (n=313).2.
| Baseline #(%) |
Follow-up #(%) |
Baseline #(%) |
Follow-up #(%) |
p- value |
|
|---|---|---|---|---|---|
| I [n=157) | I (n=141) | C (n=156) | C (n=137) | ||
| Do a thorough skin self-examination (SSE) once or more in last year1 | 23 (14.65) | 44 (31.20) | 13 (18.33) | 10 (16.80) | 0.006 |
| Engage in thorough provider screening of skin by taking all clothes off once or more in last year | 23 (14.65) | 65(41.67) | 23 (14.74) | 16 (10.26) | 0.005 |
| Sun protection behaviors | |||||
| Wear a long-sleeved shirt or blouse | 108 (68.79) | 98 (62.42) | 91 (58.33) | 99 (63.46) | 0.054 |
| Wear long pants or long skirt | 133 (84.71) | 113 (71.97) | 127 (81.41) | 128 (82.05) | 0.770 |
| Wear sunscreen SPF 15+ | 57 (36.31) | 46 (29.30) | 57 (36.54) | 55 (35.26) | 0.875 |
| Wear something on your head? (hat, cap, scarf) | 46 (29.30) | 79 (47.39) | 28 (17.95) | 42 (26.92) | 0.005 |
| Wear a hat with a brim at least 2.5 in wide all the way around | 20 (12.74) | 23 (14.65) | 9 (5.77) | 13 (8.33) | 0.388 |
| Wear sunglasses | 85 (54.14) | 77 (49.04) | 89 (57.05) | 82 (52.56) | 0.860 |
| Stay in available shade | 67 (42.68) | 82(58.15) | 59 (37.82) | 45 (28.85) | 0.008 |
| Avoid outdoors when the sun is strongest | 48 (30.57) | 73 (51.77) | 42 (26.92) | 34 (21.79) | 0.010 |
Yes was coded as half the time or more, no was never or sometimes
Adjusted for season of the year
We assessed whether there were significant changes in intermediate variables from baseline to follow-up among FDRs in the intervention group. These included perceived risk, cancer worry, and two melanoma-related beliefs. Variables that changed significantly from baseline to follow-up in the intervention group included perceived risk (increased from mean of 11% to mean of 27%; p<0.01) and belief in looking better with a tan (decreased from mean of 2.9 to mean of 2.1 ;p<0.05). These two variables were used in the final regression analyses for intervention group FDRs.
Table 3 presents the mediation of melanoma prevention behavior changes from pre- to post-intervention among intervention FDRs using important predictors of FDR outcomes found significant in Table 2. The variables we considered as mediators of the relationship between intervention and outcomes included changes in perceived risk and in belief about looking better with tan, baseline geographical closeness to case, baseline cohesion of family, and website use frequency during the study (all of FDRs). As shown in this table, increases in perceived risk from baseline to follow-up significantly predicted increases in multiple outcomes, including SSE, sunscreen use, and head covering increase. FDR living close to the case and FDR baseline ratings of family cohesion both significantly increased the likelihood of several desirable behavioral outcomes. FDRs living closer to the case increased the likelihood of SSE, sunscreen use, head covering, and avoiding sun. All of the mediation effects were small, but in the hypothesized direction, high FDR family cohesion increased the likelihood of SSE, sunscreen use, head covering, and seeking shade. The change in beliefs about tan as better looking and the baseline variables of, frequency of website use, and stage of case’s melanoma, did not influence any of the outcomes.
Table 3.
Mediators of 1-year melanoma prevention behavior change for FDRs (n=157) of families in Suntalk study intervention arm.
| Variable | SSE1 | Provider screening |
Sunscreen | Head covering |
Shade | Avoid sun |
|---|---|---|---|---|---|---|
| AOR2 CI |
AOR CI |
AOR CI |
AOR CI |
AOR CI |
AOR CI |
|
| FDR perceived risk change | 1.43 (1.5,4.3) | 1.03 (.7, 2.0) | 1.60 (1.1,2.5) | !.38 (1.3,2.4) | 1.01 (.4,1.7) | 1.03 (.3,1,4) |
| FDR belief in looking better with tan change | .78 (.7,1.9) | .34 (.4,2.7) | .99 (.8,2.9) | 1.00 (.8,2.8) | 1.02 (.8,1.1) | .74 (.4,1.8) |
| FDR living close to case baseline | 2.4 (1.5,2.8) | 1.01 (.9,3.6) | 2.58 (1.9.3.5) | 1.67 (1.3,3.0) | 1.20 (.4,1.6) | 2.66 (1.7,3.9) |
| FDR family cohesion baseline | 3.56 (1.7,4.9) | 1.04 (.4,3.9) | 2.89 (2.1,3.8) | 1.03 (1.0,3.5) | 1.06 (1.6,3.4) | 2.27 (1.5,1.4) |
| FDR website use frequency | 1.01 (.1,1.6) | 1.04 (.1,1.4) | 1.02 (.7,2,7) | 1.02 (.8,2.4) | 1.00 (.6,2.7) | 1.10 (.4,2.8) |
For outcomes yes=1; each predictor was separate regression model
AOR = Adjusted odds ratio, CI = confidence intervals. Model included intervention arm and each mediation variable separately. Adjusted for season of the year
Discussion
Our web-based intervention was designed for families at increased risk for melanoma, to promote melanoma prevention behaviors through increasing communication among family members. These behaviors include protecting oneself from the sun through several means, and increasing frequency of self-examination of the skin and provider examination of the skin to identify suspicious lesions that need further follow-up. For many of these outcomes, the intervention was successful in increasing the overall frequency of performing these behaviors in melanoma FDRs, including self and provider screening and several sun protection behaviors. These outcomes are in line with current recommendations to consider screening, both self and provider screening, as methods of identifying skin lesions early in the cancer development process, removing them at an early stage, and therefore preventing them from growing and metastasizing beyond local areas of the skin [23, 24]. The outcomes also are supported by recommendations to increase awareness and protection from ultraviolet radiation exposure to prevent sunburn and the overall accumulation of UV exposure; both of these types of exposure are implicated in the development of melanoma.
The percent of control participants performing SSE and provider examination decreased from baseline to follow-up, and we have no a priori explanation for this potential decrease. One possible explanation would be a Hawthorne effect operating at baseline, where initially participants worked harder and reported higher levels at the initial assessment. For many participants, we heard anecdotally that the Suntalk study was the first time they had heard of familial history as a risk factor. Future studies could include an extra measurement to remove this effect from the actual change score, and so assist with interpretation.
This improvements in SSE and provider screening among intervention participants seem particularly relevant because these participants were first-degree relatives of cases of melanoma, and so at already higher risk than the general population for future melanoma diagnosis. Consistent evidence indicates that survivors do not bring up melanoma risk with family members frequently if unprompted, losing an opportunity to talk about getting screened by a health care professional and to ask FDRs to consider screening as an option. In the present study all family members were given access to the website multiple times, possibly increasing the conversation frequency and/or content about melanoma risk. This website did not rely on cases to initiate communication with FDRs about melanoma risk, but it did incorporate any conversation that occurred and that supported family members in their conversations with each other. In another settings we have shown that participating in the intervention increased agreement in beliefs between melanoma survivors and their FDRs [26], but we do not know if increased communication and the type, content, or frequency of the communication mediated the increases in screening or sun protection behaviors. This study was not powered to test for interactions of this sort, given the variability in communication measures, and therefore, this question will be the subject of another study. Therefore, we cannot rule out that improved outcomes were simply a function of individual exposure to the web site, irrespective of effects on family communication. Future research should address these mechanisms.
The findings of this study are supported by several other studies that, in different ways, have targeted the relatives of melanoma survivors with interventions to reduce risk through one or more of these behaviors [27-29] Manne and colleagues compared a tailored intervention to a generic intervention for FDRs of melanoma survivors, and found that the tailored version produced almost a two fold increase in provider examinations and trends in other melanoma prevention behaviors [27]. Geller and colleagues tested an intervention in siblings of melanoma patients to improve their screening and SSE behaviors, and found a doubling of the rates of behaviors performed at the one year follow up [28]. The order of magnitude of intervention effect is slightly greater in the present study, possibly due to the involvement of entire families in the intervention process. Taken together, these data indicate that a promising avenue for encouraging behavior change is to work through families. One method of working through families is by identifying a case in the family and assisting with contact of other family members. More research should identify possible mechanisms and pathways that could benefit from increasing familial attention to the problem and working with families through accessible conduits.
The Suntalk web-based intervention resulted in improved skin protective behaviors, although the frequency of web use was not associated with any of the main outcomes. The average number of log-ins’ on was relatively low (1.9) but practically all intervention FDRs did log on at least once during the study period (12). This suggests that web-based cancer screening interventions can be effective even if FDRs do not engage repeatedly with the program. In prior, related work on breast cancer screening, we found a similar web-based intervention effect without a “dosage” effect. (30). As research shows that it is difficult to achieve (ongoing) engagement with web-based interventions, the results of our study are encouraging and important. The Suntalk web-based program encouraged interpersonal communications between study FDRs and cases. Future studies should explore the mechanisms by which the web-programs stimulate multi-step flow of communication, to separate the effect of the web-content from the effect of subsequent social network discussions.
The limited test of the mechanism of success in the intervention provided some clues as to possible mechanism of action of this intervention. Variables that were important in mediating intervention outcome included perceived risk, family cohesion and living in the same city or town as the case. These variables might be indicating that the closer a person is to a case of melanoma in a family setting, the more likely that case is to influence how the relative behaves, through possible increases in communication frequency or content. We do not have the data to test these speculative hypotheses explicitly, but these ideas can form the basis of future studies that explore these mechanisms in detail.
Study limitations include the regional location of the study in the Pacific Northwest, and the decision to limit this study to people with web access, which meant that relatively poor people would have been less likely to participate. The strengths of this study include the nature of the design, a randomized controlled trial, the relatively unbiased method of sampling cases through a cancer registry that reflects the population of cancer survivor families, and the measurement of multiple outcomes. These characteristics give the study some generalizability to other settings and other relevant behaviors, and support the idea that using an intervention like this one in clinical practice would be a positive and potentially influential activity for melanoma families to engage in [32]. A next line of research is to identify the methods of reaching people without web access to enable those families or members within existing web accessed families to fully participate. All of these will be considered in future research.
Practice Implications
This study has direct implications for usual care of melanoma families. Upon diagnosis, cases and FDRs can be provided with this website, and can be encouraged to use it to guide behavioral choices. The best ways of doing this are unclear, but could include providing the weblink in the oncology setting, providing access to all patients and families in the survivorship period, or both. Identification of the best methods of providing the website to families might be the topic of a new research project, focused on the dissemination of this weblink to all relevant families. In addition, other cancer site families, such as breast and colorectal, could benefit from this type of comprehensive mHealth support tool for families. As we gain sophistication in the use of mHealth tools in encouraging behavior change, we can use these tools to promote health in multiple settings.
Figure 1.
CONSORT flowchart for the present randomized trial
Acknowledgments
Funding: This study was funded by the National Cancer Institute (CA107430).
Footnotes
Conflict of Interest: Bowen declares that she has no conflict of interest. Hay declares that she has no conflict of interest. Meischke declares that she has no conflict of interest. Mayer declares that she has no conflict of interest. Harris-Wai declares that she has no conflict of interest. Burke declares that she has no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.National Cancer Institute. (2015a) SEER Stat Fact Sheets: Melanoma of the skin. Available at: http://seer.cancer.gov/statfacts/html/melan.html.
- 2.Vuong K, Armstrong BK, Weiderpass E, Lund E, Adami HO, Veierod MB, Barrett JH, Davies JR, Bishop DT, Whiteman DC, Olsen CM, Hopper JL, Mann GJ, Cust AE, McGeechan K; and the Australian Melanoma Family Study Investigators (2016) Development and external validation of a melanoma risk prediction model based on self-assessed risk factors. JAMA Dermatol. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Institute. (2015b) UV exposure and sun protective practices. Available at: http://progressreport.cancer.gov/prevention/sun_protection.
- 4.Bowen DJ, Jabson JM, Haddock N, Hay J.,Edwards K (2011) Skin care behaviors among melanoma survivors. Psycho-Oncology doi: 10.1002/pon. [DOI] [PubMed] [Google Scholar]
- 5.Pitceathly C, Maguire P (2003) The psychological impact of cancer on patients’ partners and other key relatives. European Journal of Cancer doi: 10.1016/S0959-8049(03)00309-5. [DOI] [PubMed] [Google Scholar]
- 6.Novilla MLB, Barnes MD, Natalie G, Williams PN, Rogers J (2006) Public health perspectives on the family: An ecological approach to promoting health in the family and community. Family & Community Health 29(1), 28–42. [DOI] [PubMed] [Google Scholar]
- 7.Hay J, Shuk E, Brady MS, Berwick M, Ostroff J, Halpern A (2008) Family communication after melanoma diagnosis. Archives of Dermatology doi: 10.1001/archderm.144.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oliveria SA, Heneghan MK, Halpern AC, Hay JL, Geller AC (2012) Communication about family members' risk of melanoma: self-reported practices of dermatologists in the United States. Arch Dermatol. 148(5):621–7. [DOI] [PubMed] [Google Scholar]
- 9.Bowen DJ, Hay JL, Mayer J, Kuniyuki A, Meischke H, Harris J, Asgari M, Shoveller J, Press N, Burke W (2012) Predictors of recruited melanoma families into a behavioral intervention project. Contemporary Clinical Trials 33(1):85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris JN, Kuniyuki A, Hay J, Asgari M, Press N, Bowen DJ (2010). Using a family systems approach to investigate cancer risk communication within melanoma families. Psycho-Oncology, 19(10), 1102–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torres SM, Ramos M, Leverence R, Bowen D, Berwick M, Hay J. (2014). A pilot study of skin cancer risk reduction behaviors, cancer communications, and skin cancer beliefs in Hispanics in a Southwestern primary care practice. Californian Journal of Health Promotion, 12(1), 95–100. [Google Scholar]
- 12.Bowen DJ, Burke W, Hay J, Meischke H, Harris J. (2015). Effects of web-based intervention on risk reduction behaviors in melanoma survivors, Journal of Cancer Survivorship, 9(2), 279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulz KF, Altman DG, Moher D, for the CONSORT Group (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomized trials. Ann Int Med 152. Epub [PMC free article] [PubMed] [Google Scholar]
- 14.Anton-Culver H, et al. (2003) The Cancer Genetics Network: recruitment results and pilot studies. Community Genet 6(3): p. 171–7. [DOI] [PubMed] [Google Scholar]
- 15.http://www.yourdiseaserisk.wustl.edu/ Accessed Sept 30, 2017
- 16.Weinstock M, Risica P, Martin R, Rakowski W, Dube C, Berwick M, Goldstein M, Acharyya S, Lasater T (2007) Melanoma early detection with thorough skin self-examination the ‘check it out’ randomized trial. American Journal of Preventive Medicine doi: 10.1016/j.amepre.2007.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oh SS, Mayer JA, Lewis EC, Slymen DJ, Sallis JF, Elder JP, et al. (2004) Validating outdoor workers' self-report of sun protection. Preventive Medicine 39(4), 798–803. [DOI] [PubMed] [Google Scholar]
- 18.Kovalyshyn I (2011) The impact of physician screening on melanoma detection. Archives of Dermatology [DOI] [PubMed] [Google Scholar]
- 19.Novilla MLB, Barnes MD, Natalie G, Williams PN, Rogers J (2006) Public health perspectives on the family: An ecological approach to promoting health in the family and community. Family & Community Health 29(1), 28–42. [DOI] [PubMed] [Google Scholar]
- 20.Leventhal H. (1987). Behavioral theories and the problem of compliance. Patient Education and Counseling, 10(2), 117–138. [Google Scholar]
- 21.Leventahl H (in press) Dual process theory of predicting behaviors, in Diefenbach MA, Miller SM, & Bowen D. (In Press). Handbook of Health Decision Science. New York, NY: Springer Verlag [Google Scholar]
- 22.Lerman C, Daly M, Masny A, Balshem A (1994) Attitudes about genetic testing for breast-ovarian cancer susceptibility. Journal of Clinical Oncology vol. 12 no. 4 843–850. [DOI] [PubMed] [Google Scholar]
- 23.Moos RH and Moos BS, (1986) The family environment scale: The manual. Palo Alto CA: Consulting Psychologists Press. [Google Scholar]
- 24.Geller AC, Halpern AC (2013) The ever-evolving landscape for detection of early melanoma: challenges and promises. J Invest Dermatol. 133(3):583–5. [DOI] [PubMed] [Google Scholar]
- 25.Manne S, & Lessin S (2006). Prevalence and correlates of sun protection and skin self-examination practices among cutaneous malignant melanoma survivors. Journal Behavioral Medicine, 29, 419–34. [DOI] [PubMed] [Google Scholar]
- 26.Bowen DJ, Albrecht T, Hay J, Eggly S, Harris-Wei J, Meischke H, Burke W (2018) Communication among melanoma family members. FamComm, 16(4):597–603.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geller AC, Emmons KE, Brooks DR, Powers C, Zhang Z, Koh HK, Heeren T, Sober AJ, Li F, Gilchrest BA (2006) A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer doi: 10.1002/cncr.22050. [DOI] [PubMed] [Google Scholar]
- 28.Manne S, Jacobsen PB, Ming ME, Winkel W, Dessureault S, Lessin SR (2010) Tailored versus generic interventions for skin cancer risk reduction for family members of melanoma patients. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gritz ER, Tripp MK, Peterson SK, Prokhorov AV, Shete SS, Urbauer DL, Fellman BM, J Lee JE, Gershenwald JE (2013) Randomized controlled trial of a sun protection intervention for children of melanoma survivors. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bowen D, & Powers D (2010) Effects of a mail and telephone intervention on breast health behaviors. Health Education & Behavior, 37(4), 479–489 [DOI] [PubMed] [Google Scholar]
- 31.Baron RM and Kenny D (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology Vol. 51, No. 6, 1173–1182. [DOI] [PubMed] [Google Scholar]
- 32.Hay J, Meischke H, Bowen D, Mayer J, Shoveller J, Press N, .Burke W (2007). Anticipating dissemination of cancer genomics in public health: A theoretical approach to psychosocial and behavioral challenges. Ann. Behav. Med, 34(3), 275–286. [DOI] [PubMed] [Google Scholar]