Abstract
Aim:
Early detection and intervention (EDI) is a main challenge in psychosis research. The Chilean schizophrenia (SZ) national program has universal support and treatment by law for all SZ patients, but this does not yet extend to earlier stages of illness. Therefore, we have piloted an ultra-high risk (UHR) program to demonstrate the utility and feasibility of this public health approach in Chile.
Methods:
We introduce “The University of Chile High-risk Intervention Program,” which is the first national EDI program for UHR youths. Longitudinal follow-up included clinical and cognitive assessments, and monitoring of physiological sensory and cognitive indices, through electroencephalographic techniques.
Results:
We recruited 27 UHR youths over 2 years. About 92.6% met criteria for attenuated psychosis syndrome (APS). Mean Scale of Psychosis-Risk Symptoms (SOPS) ratings in the cohort were 6.9 (SD 4.6) for positive, 9.1 (SD 8.3) for negative, 5.4 (SD 5.3) for disorganized and 6.3 (SD 4.1) for general symptoms. About 14.8% met criteria for comorbid anxiety disorders and 44.4% for mood disorders. Most participants received cognitive behavioural therapy (62.9%) and were prescribed low dose antipsychotics (85.2%). The transition rate to psychosis was 22% within 2 years.
Conclusions:
We describe our experience in establishing the first EDI program for UHR subjects in Chile. Our cohort is similar in profile and risk to those identified in higher-income countries. We will extend our work to further optimize psychosocial and preventive interventions, to promote its inclusion in the Chilean SZ national program and to establish a South American collaboration network for SZ research.
Keywords: Chile, mental health services, preventive psychiatry, psychosis, South America, ultra-high risk
1 |. INTRODUCTION
Psychotic disorders typically emerge during adolescence and early adulthood, leading to functional impairment and significant burden for caretakers and society. In the absence of early detection and prevention, young people with psychotic disorders often obtain care in emergency services in the context of crisis (Corcoran et al., 2007). In the past two decades, therefore, there has been a concerted effort through early detection programs (EDPs) to identify young people with psychotic-like symptoms, with the intention of preventing or delaying psychosis onset, and reducing functional impairment. Interestingly, when compared to inpatient programs, EDP’s have shown to be cost-effective in improving the prognosis of schizophrenia (SZ) spectrum disorders (McCrone, 2010; McGorry, 2015). In this context, a growing number of EDPs for psychosis have been developed in Australia, Europe, North America and more recently in Asia.
Initially, EDPs were focused on shortening the duration of untreated psychosis associated with the first episode of psychosis (FEP). The main focus now is on the putative prodromal period, also known as a clinical high-risk (CHR) or ultra-high risk (UHR) syndrome, that is characterized by attenuated psychotic-like experiences, social isolation and withdrawal, mood symptoms and a decline in social and academic/vocational function (Carpenter, 2016; Yung & McGorry, 1996). An initial meta-analysis suggests that some interventions may reduce rates of onset of psychosis in CHR/UHR participants, though without clear improvement in function (Schmidt et al., 2015). Hence, more work is needed to improve predictive validity for both psychosis and functional impairment, through the identification of biomarkers that in turn can be targets of engagement for developing preventive intervention strategies.
Recently, Latin America has joined this psychosis EDP initiative with a handful of EDP programs, mainly in urban areas in Brazil and Mexico, affiliated with universities for research purposes, though with partnerships with public education and other community-based efforts (Brietzke, Araripe Neto, Dias, Mansur, & Bressan, 2011). Ours is the first EDP program in Chile, capitalizing on academic affiliations with the University of Chile and the Biomedical Neuroscience Institute in Santiago, yet also contextualized within a larger nationwide public health initiative that addresses SZ. Chile is relatively unique worldwide in that a decade ago; it implemented a legal mandate that guaranteed diagnosis and treatment for medical diagnoses that influenced public health, including SZ. In Chile, the Garantías Explícitas en Salud (GES) program, backed by State Law 19.937, has provided universal free access for diagnosis and treatment of SZ (MINSAL, 2009) including “suspected cases” among FEP patients, leading to lower rates of re-hospitalization and better outcomes for patients and families. With respect to services, adherence to medication guidelines has been high at 86%, with about half of patients and families obtaining psychoeducation (Markkula, Alvarado, & Minoletti, 2011). As of now, however, GES for SZ starts with the FEP, leaving UHR patients without health coverage. Research on the UHR state in Chile is therefore critical for determining potential future GES guidelines for early identification and intervention for psychosis risk. Here, we describe the first UHR program in Santiago, Chile, including clinical characterization and therapeutics, and opportunities for research and training, so that this approach can be implemented more broadly throughout Chile and South America.
2 |. METHODS
2.1 |. The UCHIP clinical program: setting, staffing, ascertainment, clinical characterization prospective evaluation and therapeutics
2.1.1 |. Setting
The University of Chile High-risk Intervention Program (UCHIP) is located at the Psychiatric Clinic of the University of Chile Hospital (PCUCH), which is the oldest and among the most prominent training psychiatric centres in the country. Most referrals come from the northern part of Santiago, but as PCUCH is a nationwide referral centre, it provides services to UHR and FEP patients from all over the country. The UCHIP was founded in May of 2014 and its aim and mission is to provide quality, evidence-based and long-term clinical care to teens and young adults who meet criteria for UHR or FEP.
2.1.2 |. Staff
The UCHIP team is comprised of three psychiatrists (one adult and two child and adolescent psychiatrists), one clinical coordinator, one neuropsychologist, three PhD students (two in biomedical sciences and one in psychiatry), three residents in child and adolescent psychiatry and two medicine interns (under rotation).
2.1.3 |. Participant ascertainment
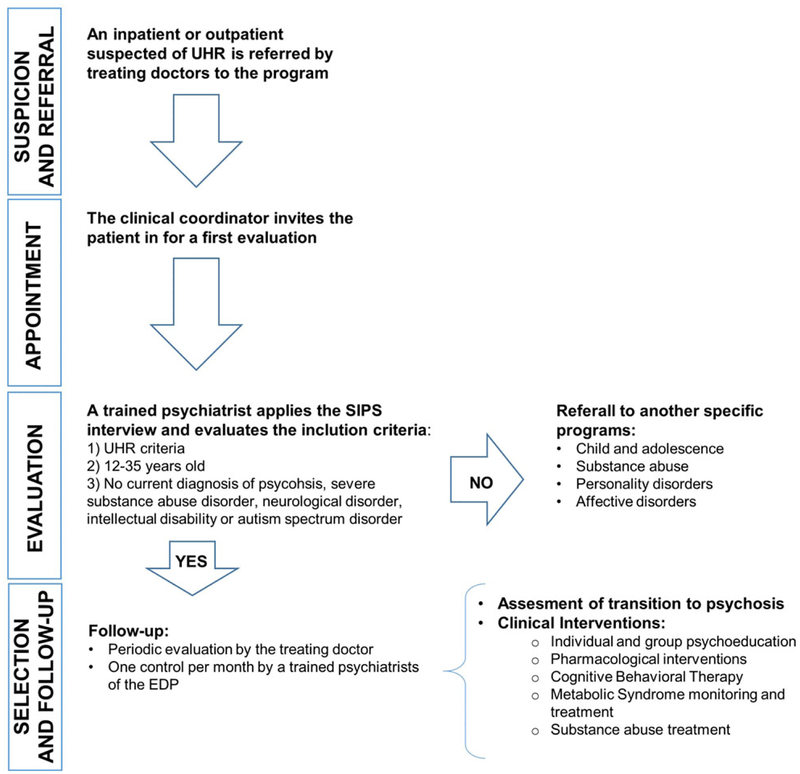
Participants are ascertained from crisis evaluation in the emergency services as well as through outpatient consultation in both the child and adolescent, and adult, psychiatry units. Prior to the founding of UCHIP in 2014, these patients would have had non-expert clinical consultations without the provision of systematic intervention. Inclusion criteria for our participants include; (a) ages 12 to 35 years old and (b) fulfil criteria for at least one of three prodromal syndrome scales: (a) Attenuated Psychotic Symptoms (APS), (b) Brief and Limited Intermittent Psychotic Symptoms (BLIPS) or (c) Genetic Risk and Deterioration (GRD; first-degree family history of psychosis or schizotypal personality disorder with significant functional decline) (Miller et al., 1999). Exclusion criteria include (a) previous threshold psychosis (presence of psychosis criteria), (b) severe abuse or dependence of alcohol or other drugs, (c) intellectual disability, (d) autism spectrum or (e) neurological disorders (Figure 1).
FIGURE 1.
University of Chile High-risk Intervention Program patient flowchart (EDP, early detection program; UHR, ultra-high risk)
2.1.4 |. Clinical characterization
Screening and diagnosis followed the guidelines established at Yale University’s Prevention through Risk Identification, Management and Education (PRIME) program. The Structured Interview for Psychosis-Risk Syndromes/Scale of Psychosis-Risk Symptoms (SIPS/SOPS) (Miller et al., 1999) was administered by psychiatrists at UCHIP trained to reliability, with function assessed using the Global Assessment of Functioning (Hall, 1995). The Mini International Neuropsychiatric Interview for adults (MINI) and adolescents (MINI-KID) (Sheehan et al., 2010) was also administered to diagnose other comorbidities (Figure 1). The exclusion diagnoses (autism spectrum disorders, severe substance abuse disorder and intellectual disability) were performed according to the diagnostic guidelines of the DSM-5.
2.1.5 |. Prospective evaluation
The UCHIP program does weekly ratings and clinical monitoring at least monthly, and more often for acuity. There is also a group evaluation twice a year. Medical, psychiatric and environmental risk assessments are also completed using a semi-structured interview, with a focus on identifying sources of personal and family stress. Also, there is monitoring of features of potential metabolic syndrome, including body mass index, vital signs, fasting glucose, lipid profile, hepatic profile and thyroid-stimulating hormone, at baseline and then at least every 6 months, with greater frequency of assessment as needed (Figure 1). If there is a personal or family history of heart disease, an electrocardiogram is requested to rule out this pathology, considering the high possibility of using antipsychotics in the longitudinal follow-up. Electroencephalography (EEG), neuroimaging (computed tomography scan or magnetic resonance imaging), urine toxicology and testing for sexually transmitted diseases (HIV and syphilis) are also assessed if clinically indicated to make differential diagnosis with other relevant conditions.
2.1.6 |. Therapeutics
Antipsychotic medication is prescribed only for selected cases with moderate to severe symptoms, following GES-SZ guidelines (MINSAL, 2009), beginning with a second-generation antipsychotic (SGA) medication dosed at lower levels of the recommended dose range and chosen based on clinical profile and potential side-effects. Antipsychotic dose is increased after 3 weeks if there is minimal to moderate response and medication is switched to another SGA if there is inadequate clinical response. Antidepressants, anxiolytics and mood stabilizers are used as needed to target other non-psychotic symptoms. Mild to moderate substance abuse is treated using psychoeducation and standard motivational interviewing techniques, with cognitive behavioural therapy used to sustain abstinence. The development of more severe abuse or dependence prompts referral to specialty programs for abuse and dependence (Figure 1).
All participants, and their family members, are offered a standardized psychoeducational group intervention at baseline and every 6 months, following the protocol from the Programa de Intervención en Psicosis Adolescente (PIENSA) program from Spain (Ruiz-Sancho et al., 2012). Likewise, all participants are offered cognitive behavioural therapy, individualized for each participant, but generally comprising of development of social skills, problem solving abilities, emotional regulation techniques, management of cognitive distortions and behavioural modification.
2.2 |. Training and research at the UCHIP clinical program
UCHIP emphasizes academic activities such as research and training, as it is within the clinical branch of the Translational Psychiatry Laboratory at the University of Chile in Santiago. The Translational Psychiatry Laboratory emphasizes the application of clinical neuroscience to the study of neuropsychiatric disorders, including SZ and its risk states, as well as bipolar, personality, attention-deficit/hyperactivity and autism spectrum disorders.
2.2.1 |. Training
UCHIP is a place of training for national and international undergraduate and graduate students. Likewise, the UCHIP staff actively participates in the academic activities of the University of Chile.
2.2.2 |. Research
We have focused on the study of putative biomarkers of psychosis risk and functional outcome at UCHIP, in particular, cognitive and sensory processing in the visual and auditory domains assessed both behaviourally and at the physiological level using event-related potentials (ERP) and event-related spectral decomposition (ERSD) measures, as well as genetic markers. Cognition is assessed using the Montreal Cognitive Assessment (MoCA; Nasreddine, Phillips, Bédirian, Char-bonneau, & Whitehead, 2005) and a Spanish version of the MATRICS Consensus Cognitive Assessment Battery (MCCB; Nuechterlein et al., 2008). For neurophysiological studies, the ongoing (resting-state) EEG is measured as well as ERPs elicited during working memory and perception tasks (visual, auditory and bimodal). In all cases, electrophysio-logical recordings are carried out with a 72-channel Biosemi EEG system. Resting-state and task-related electrophysiological measures are evaluated in parallel to assess underlying circuitry and functional connectivity patterns. Finally, serum for genotyping is collected from both participants and first-degree relatives. For comparison, all of the above measures are also acquired in healthy volunteers, and patients with FEP or SZ, in order to evaluate stage-specific deficits in UHR individuals.
2.3 |. Statistical analyses
Following are descriptive statistics and group comparisons, using non-parametric tests, for the participants ascertained to date, with respect to demographics, clinical characteristics and therapeutics. We determined the predictive value of clinical severity for psychosis outcome. We also conducted proportional hazards survival analysis, generating Kaplan-Meier survival curves, both overall and by gender, to show the pattern of psychosis onset over time within the UHR cohort, and Cox regression analysis to determine age effects on rates of transition to psychosis.
3 |. RESULTS
3.1 |. Demographics
We recruited 27 UHR (19 male), ages 12 to 28 (mean 17.6 years), with years of education ranging from 5 to 16 (mean 9.8 years). All participants were single and only one was employed. All but one participant lived in the Santiago Metropolitan area. Mean number of days of follow-up was 349 days (Table 1).
TABLE 1.
Baseline demographics of ultra-high risk subjects
| Mean (SD) | Median (range) | |
|---|---|---|
| Age (years) | 17.6 (2.9) | 17 (12–28) |
| Education (years) | 9.8 (3.9) | 10 (5–16) |
| n | % | |
|---|---|---|
| Gender (male) | 19 | 70.3 |
| Marital status (single never married) | 27 | 100 |
| Residence (Santiago) | 26 | 96.3 |
3.2 |. Clinical characteristics
Of the 27 participants, 25 met criteria for APS at baseline, with only 2 participants meeting criteria for GRD. There were no baseline BLIPS diagnoses in our cohort. Mean SOPS ratings in the cohort were 6.9 (SD 4.6) for positive, 9.1 (SD 8.3) for negative, 5.4 (SD 5.3) for disorganized and 6.3 (SD 4.1) for general symptoms. On the other hand, most of the cohort (74.1%) scored mild symptoms. The prevalence of anxiety and mood disorders, determined by the MINI interview, was respectively, 14.8% and 44.4% (Table 2).
TABLE 2.
Baseline clinical characteristics of UHR subjects
| n | % | Mean (SD) | |
|---|---|---|---|
| UHR subtype | |||
| APS | 25 | 92.6 | - |
| GRD | 2 | 7.4 | - |
| BLIPS | 0 | 0 | - |
| SOPS clinical scores | |||
| Total positive | - | - | 6.9 (4.6) |
| Total negative | - | - | 9.1 (8.3) |
| Total disorganized | - | - | 5.4 (5.3) |
| Total general | - | - | 6.3 (4.1) |
| Comorbidity | |||
| Anxiety disorders | 4 | 14.8 | - |
| Mood disorders | 12 | 44.4 | - |
| Medication use | |||
| Antipsychotics | 23 | 85.2 | - |
| Antidepressants | 12 | 44.4 | - |
| Anxiolytics | 5 | 18.5 | - |
| PUFA | 6 | 22.2 | - |
| Psychotherapy | 17 | 62.9 |
Abbreviations: APS, attenuated psychosis syndrome; BLIPS, Brief and Limited Intermittent Psychotic Symptoms; GRD, genetic risk and deterioration; PUFA, polyunsaturated fatty acids; SOPS, Scale of Psychosis-Risk Symptoms; UHR, ultra-high risk.
3.3 |. Therapeutics
Compliance with treatment was relatively high, with all participants receiving psychoeducation, 62.9% receiving CBT and 85.2% prescribed daily low-dose SGA (Aripiprazole 5–10 mg, Risperidone 1–2 mg, Quetiapine 25–150 mg, Olanzapine 5 mg). Five percent of participants were prescribed anxiolytics, 12% antidepressant medication (eg, Sertraline 25–100 mg, Escitalopram 10–20 mg), although 22% were prescribed omega-3 polyunsaturated fatty acids (PUFA) (Table 2).
3.4 |. Psychosis outcome
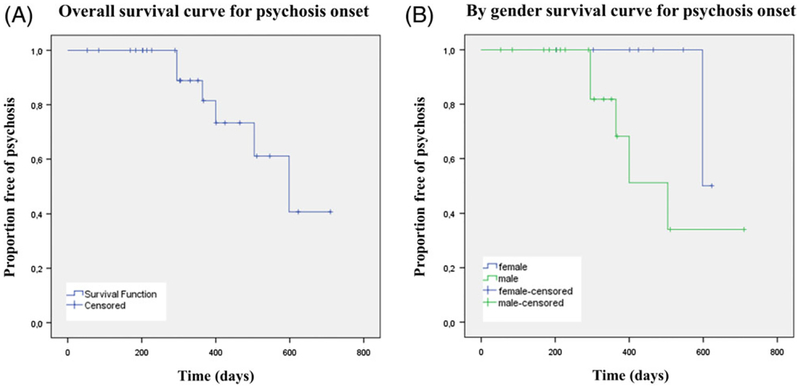
Twenty-two percent of the UHR cohort met criteria for threshold psychosis and 18% for personality disorder within 2 years. Survival analysis showed a mean (SD) time to transition of 348.9 (162) days and a median (CI) time of transition of 331 (53–710) days. Specifically, transition occurred at day 295 for two individuals, with the other transitions occurring respectively on days 364, 400, 504 and 598 (Figure 2). There was a trend effect for mean survival by gender with males transitioning to psychosis more quickly: 499 days (95% CI 380–618 days) for males vs 611 days (95% CI 593–627 days) for females (Log rank test P = 0.09). Age was unrelated to survival in this small cohort (beta = 0.859; 95% CI: 0.6–1.2). For the dichotomous analysis of transition, all the SIPS categories (positive, negative, general and disorganized symptoms) showed small effect sizes (0.2 or less), which suggests that baseline symptoms severity did not predict transition significantly (Table 3).
FIGURE 2.
Survival to psychosis onset–overall and by gender
TABLE 3.
Baseline clinical symptoms and psychosis outcome
| SOPS | Transition UHRto FEP | n | Mean rank | Z | P value | Effect size |
|---|---|---|---|---|---|---|
| Positive | No | 21 | 13.21 | −0.98 | 0.32 | 0.19 |
| Yes | 6 | 16.75 | ||||
| Negative | No | 21 | 13.00 | −0.69 | 0.49 | 0.13 |
| Yes | 6 | 15.60 | ||||
| Disorganized | No | 21 | 12.76 | −1.02 | 0.31 | 0.20 |
| Yes | 6 | 16.60 | ||||
| General | No | 21 | 13.26 | −0.33 | 0.74 | 0.06 |
| Yes | 6 | 14.50 |
Abbreviations: FEP, first episode of psychosis; SOPS, Scale of Psychosis-Risk Symptoms; UHR, ultra-high risk. Mann-Whitney U test. Confidence level 95%. Sig. 2-tailed.
4 |. DISCUSSION
Individuals suffering from neuropsychiatric disorders in low- and middle-income countries (LAMIC countries) frequently do not receive adequate evidence-based care, leading to chronicity, poor prognosis and increased costs of care. Early prevention and promotion of mental health in psychosis have become a priority in Asia, Latin America and Europe (McGorry, 2015). Increasingly, LAMIC countries in Latin America have successfully implemented EDPs (Brietzke et al., 2011). In this context, we have described our experience in establishing the first EDP for 27 UHR subjects in Chile.
When we compared our sample with the largest UHR cohort in the Western Hemisphere, the North American Prodrome Longitudinal Study (NAPLS-2, n = 764), we found that our cohort was younger (17.6, SD = 2.9 vs 19.7, SD = 4.7) and with fewer years of education (9.8, SD = 3.9 vs 12.7, SD = 3.6). It also had a higher proportion of males (70.3% vs 50.4%), but with similar marital status (100% vs 95% single/never married). The proportion of psychosis-risk syndromes was also similar with 92.6% vs 92.1% APS in the NAPLS-2. (Addington et al., 2015). Prevalence of other clinical diagnoses in UHR was similar for mood disorders (44.4% vs 49.2%) but not for anxiety disorders, which was lower in our sample (14.8% vs 47.8%; Addington et al., 2017). Regarding treatment, we were more prone to use a SGA (85.2% vs 12.3%) than psychotherapy (62.9% vs 73.7%) (Cadenhead et al., 2010). Our transition rate of 22% is comparable to the 29% transition rate identified in a meta-analysis done by Fusar-Poli et al. (2012). Overall, our cohort is similar in profile and risk to those found in high-income countries. In our small cohort, baseline symptom severity does not predict transition to psychosis, likely due to insufficient power. We expect that as our cohort increases in size over time, identified predictors of psychosis onset in other cohorts, such as some positive (unusual thought content and suspiciousness) and negative (anhedonia, asociality) symptoms (Cannon et al., 2016; Fusar-Poli et al., 2013; Schmidt et al., 2017), will also have prognostic value in our cohort. Sample will show similar results.
Our program is in its early stages, such that we are working on improving prevention and care in an iterative fashion. To date, we have focused on standard pharmacological and psychological treatment to target the UHR syndrome and its comorbid diagnoses (Schmidt et al., 2015), combined with treatment of substance abuse and metabolic indices, but we have not yet included the common community-based psychosocial interventions. We are now also developing community-based education and greater access to service, including home-based assessment and clinical hours outside of typical work hours, as recommended by McGorry (2015). As we acquire more resources, we will include individual case managers to organize support, develop family programs and implement rehabilitation strategies for academic and vocational function. Other plans include group programs with peer support, and a formal cardiovascular assessment and treatment program, including a gym for our patients, in order to prevent metabolic complications and improve functioning (Shiers & Curtis, 2014). As new evidence emerges for other preventive intervention strategies, we will incorporate them into our program, considering local cultural factors.
Finally, we have encountered a difficulty in our UHR program that is common to other programs in Latin America, which is the struggle to recruit enough participants to both achieve a social impact proportional to the prevalence of this condition and a sufficiently large sample to make the appropriate statistical analyses. For example, in the Evaluation and Follow-up of Adolescents and Young Adults in São Paulo (ASAS) Program in Brazil, researchers studied a cohort of 18 participants meeting criteria for UHR, out of an initial sample of 894 (Brietzke et al., 2011). In this respect, our data represent a similar contribution, with 27 UHR subjects, which is not yet comparable with other larger cohorts described in the literature, such as the Personal Assessment and Crisis Evaluation (PACE) clinic in Melbourne, Australia (n = 416; Mechelli et al., 2017), the European Prediction of Psychosis Study (EPOS, n = 233; von Reventlow et al., 2014), the Center of Prevention and Evaluation (COPE), located in New York City (n = 200; Brucato et al., 2017) and the NAPLS-2 (n = 764; Addington et al., 2015). Therefore, we are working to expand our network of clinical collaborators in Chile and more broadly across South America. Our plan is to continue this initiative and to expand to other regions of Chile and South America, with the intent of building a South American psychosis risk research network.
We hope that in Chile, our initiative will lead to the further financing and universal treatment of UHR individuals as well as SZ patients by the GES.
ACKNOWLEDGEMENTS
R.I.C. is supported by the National Commission for Scientific and Technological Research (CONICYT)–PCHA, Doctorado Nacional, 2015–21150063, Ministry of Education, Chile. P.G. is funded by CONICYT, FONDECYT initiation into research 2014, Grant No. 11140464 and OAIC grant from the Clinical Hospital of the University of Chile. The Biomedical Neuroscience Institute (BNI) and the Millennium Nucleus to Improve the Mental Health of Adolescents and Youths (IMHAY) also support P.G. C.M.C. is supported by RO1 MH107558 02 and the Office of Mental Health in the State of New York, United States.
Funding information
FONDECYT initiation into research 2014, Grant/Award Number: 11140464; National Commission for Scientific and Technological Research (CONICYT) - PCHA, Doctorado Nacional, Grant/Award Number: 2015–21150063; NIH Research Project Grant Program, Grant/Award Number: RO1 MH107558 02
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
REFERENCES
- Addington J, Liu L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, … McGlashan TH (2015). North American Prodrome longitudinal study (NAPLS 2): The prodromal symptoms. The Journal of Nervous and Mental Disease, 203(5), 328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD, … Woods SW (2017). Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophrenia Research, 190, 90–95. 10.1016/j.schres.2017.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brietzke E, Araripe Neto AG, Dias A, Mansur RB, & Bressan RA (2011). Early intervention in psychosis: A map of clinical and research initiatives in Latin America. Revista Brasileira de Psiquiatria, 33(Suppl. 2), s213–s224. [DOI] [PubMed] [Google Scholar]
- Brucato G, Masucci MD, Arndt LY, Ben-David S, Colibazzi T, Corcoran CM, … Girgis RR (2017). Baseline demographics, clinical features and predictors of conversion among 200 individuals in a longitudinal prospective psychosis-risk cohort. Psychological Medicine, 47, 1923–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadenhead KS, Addington J, Cannon T, Cornblatt B, McGlashan T, Perkins D, … Heinssen R (2010). Treatment history in the psychosis prodrome: Characteristics of the north American Prodrome longitudinal study cohort. Early Intervention in Psychiatry, 4(3), 220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon TD, Yu C, Addington J, Bearden CE, Cadenhead KS, Cornblatt BA, … Kattan MW (2016). An individualized risk calculator for research in prodromal psychosis. The American Journal of Psychiatry, 173, 980–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter WT (2016). Early detection of psychosis vulnerability: Progress, opportunity, and caution. The American Journal of Psychiatry, 173(10), 949–950. [DOI] [PubMed] [Google Scholar]
- Corcoran C, Gerson R, Sills-Shahar R, Nickou C, McGlashan T, Malaspina D, & Davidson L (2007). Trajectory to a first episode of psychosis: A qualitative research study with families. Early Intervention in Psychiatry, 1(4), 308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, … McGuire P (2012). Predicting psychosis: Meta-analysis of transition outcomes in individuals at high clinical risk. Archives of General Psychiatry, 69(3), 220–229. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Borgwardt S, Bechdolf A, Addington J, Riecher-Rössler A, Schultze-Lutter F, … Yung A (2013). The psychosis high-risk state: A comprehensive state-of-the-art review. JAMA Psychiatry, 70(1), 107–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall RC (1995). Global assessment of functioning. A modified scale. Psychosomatics, 36(3), 267–275. [DOI] [PubMed] [Google Scholar]
- Markkula N, Alvarado R, & Minoletti A (2011). Adherence to guidelines and treatment compliance in the Chilean national program for first-episode schizophrenia. Psychiatric Services, 62(12), 1463–1469. [DOI] [PubMed] [Google Scholar]
- McCrone P (2010). Cost-effectiveness of an early intervention service for people with psychosis. The British Journal of Psychiatry, 196(5), 377–382. [DOI] [PubMed] [Google Scholar]
- McGorry PD (2015). Early intervention in psychosis: Obvious, effective, overdue. The Journal of Nervous and Mental Disease, 203(5), 310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechelli A, Lin A, Wood S, McGorry P, Amminger P, Tognin S, … Yung A (2017). Using clinical information to make individualized prognostic predictions in people at ultra high-risk for psychosis. Schizophrenia Research, 184, 32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Woods SW, Stein K, Driesen N, Corcoran CM, … Davidson L (1999). Symptom assessment in schizophrenic prodromal states. The Psychiatric Quarterly, 70(4), 273–287. [DOI] [PubMed] [Google Scholar]
- Ministerio de Salud. (2009). Guía Clínica para el tratamiento de personas desde primer episodio de esquizofrenia. Santiago: MINSAL. [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, … Chertkow H (2005). The Montreal cognitive Assesment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, … Marder SR (2008). The MATRICS consensus cognitive battery, part 1: Test selection, reliability, and validity. The American Journal of Psychiatry, 165(2), 203–213. [DOI] [PubMed] [Google Scholar]
- Ruiz-Sancho A, Calvo A, Rapado-Castro M, Moreno M, Moreno C, Sanchez-Gutierrez T, … Mayoral M (2012). PIENSA: Development of an early intervention program for adolescents with early-onset psychosis and their families. Adolescent Psychiatry, 2(3), 229–236. [Google Scholar]
- Schmidt A, Cappucciati M, Radua J, Rutigliano G, Rocchetti M, Dell’Osso L, … Fusar-Poli P (2017). Improving prognostic accuracy in subjects at clinical high risk for psychosis: Systematic review of predictive models and meta-analytical sequential testing simulation. Schizophrenia Bulletin, 43(2), 375–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, Maric NP, Salokangas RK, Riecher-Rossler A, … Ruhrmann S (2015). EPA guidance on the early intervention in clinical high-risk states of psychoses. European Psychiatry, 30(3), 388–404. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … Wilkinson B (2010). Reliability and validity of the Mini international neuropsychiatric interview for children and adolescents (MINI-KID). The Journal of Clinical Psychiatry, 71(3), 313–326. [DOI] [PubMed] [Google Scholar]
- Shiers D, & Curtis J (2014). Cardiometabolic health in young people with psychosis. Lancet Psychiatry, 1(7), 492–494. [DOI] [PubMed] [Google Scholar]
- von Reventlow HG, Krüger-Özgürdal S, Ruhrmann S, Schultze-Lutter F, Heinz A, Patterson P, … Juckel G (2014). Pathways to care in subjects at high risk for psychotic disorders – A European perspective. Schizophrenia Research, 152(2–3), 400–407. [DOI] [PubMed] [Google Scholar]
- Yung AR, & McGorry PD (1996). The prodromal phase of first-episode psychosis: Past and current conceptualizations. Schizophrenia Bulletin, 22(2), 353–370. [DOI] [PubMed] [Google Scholar]