Abstract
Purpose:
The increasing incidence of skin cancer is a global health issue. In order to identify at-risk populations in Texas, we compared sun protection behaviors and sunburn history across rural and urban counties.
Methods:
An online health screening survey collected data from a non-probability sample of Texas residents in 2018. Data were weighted by sex, age, race, and ethnicity. Multinomial multivariable logistic regression identified key factors associated with sun protection behaviors and sunscreen use. Weighted Pearson’s χtest identified differences between urban and rural respondents in strength of sunscreen used and sunburn history.
Findings:
Rural residents in Texas were less likely to seek shade (OR = 0.58; P = .004) and less likely to use sunscreen lotion (OR = 0.65; P = .013) compared to their urban counterparts. Sunscreen use was also lower among current versus never smokers (OR = 0.67; P = .034) but higher in those with personal versus no cancer history (OR = 2.14; P = .004). Although rural versus urban residents were more likely to use higher SPF sunscreen (P < .001), they had more sunburns in the past 12 months (P < .001). They also had more blistering sunburns over the course of their life (P < .001) and these injuries were more likely to occur at an earlier age, between 5–14 years old (P < .001).
Conclusions:
Increased attention to sun protective behaviors among rural communities in Texas is vital to help reduce the high prevalence of sunburn injury and incidence of skin cancer.
Keywords: rural, skin cancer, sun protection, sunburn, sunscreen behaviors
Skin malignancies primarily comprise keratinocyte cancers and melanoma.1 In the US, the incidence of keratinocyte cancers are estimated to be 5.4 million new cases per year.2,3 Despite this high incidence, keratinocyte cancers have relatively low metastatic potential and low mortality.1 Nonetheless, they are associated with substantial morbidity and high disease and economic burden. On the other hand, the incidence of cutaneous melanoma is estimated to be 91,270 new cases and currently ranks fifth highest amongst malignancies in men and sixth highest in women.4,5 Moreover, cutaneous melanoma can be highly aggressive and early detection is paramount.1 Therefore, it is alarming that the incidence of cutaneous melanoma and keratinocyte cancers have been rising over the decades, in both the US and on a global level, and this trend is predicted to continue.1,5 In Texas, cutaneous melanoma incidence and mortality rates are lower compared to the US as a whole.6 Yet, with the second-largest population, the state currently ranks fourth in estimated new cases of melanoma and third in estimated deaths.6
Texas comprises 254 counties, including 77 urban and 177 rural designations.7 Across the state, melanoma incidence varies widely from 2.8 to 25.2 per 100,000 in urban and 8.4 to 26.7 per 100,000 in rural counties.8 Risk for melanoma increases with age overall, and older males are at higher risk compared to older females.1,9 However, melanoma is also the second most common malignancy among adolescents and young adults; in these populations, females are at increased risk.10 Other than age and gender, another primary risk factor for skin cancer is race/ethnicity, with increased susceptibility observed amongst non-Hispanic whites (NHW).1,9
The principal causes of skin cancer include cumulative ultraviolet (UV) exposure and sunburn history.11,12 Primary prevention strategies for skin cancer focus on reducing solar exposure by encouraging adequate protection through use of hats and protective clothing; use of sunscreen of at least SPF15; seeking shade; and minimizing sun exposure during peak hours.13 Refrainment from indoor tanning is also a key prevention strategy.9 Total body skin examination for early detection may be beneficial, at least for those at highest risk.1
Overall, there is a higher incidence of and mortality from cancer in rural compared to urban communities across the US, and this pattern also holds true for melanoma.14 Contributing factors include a greater proportion of aging residents in rural areas; lower health literacy, educational attainment and socioeconomic status; and reduced access to health care.14 In Texas, rural versus urban residents have lower income, higher rates of poverty and unemployment, and lower rates of high school graduation.15 Moreover, Texas has one of the largest elderly populations in the US coupled with a dearth of primary care physicians; this particularly impacts the health of rural communities.16,17
We hypothesized that sun protection behaviors and sunburn prevalence would differ amongst Texas residents living in rural and urban communities. To test this hypothesis, we analyzed data from a 2018 statewide Texas health screening survey that included assessment of cancer prevention behaviors in a non-probability sample of the Texas population to reveal key differences in sunscreen use and sunburn history.18 Our results should help target future intervention strategies for reduction of skin cancer prevalence across the state.
Methods
Participants
The overall study population included a non-probability sample of 2,050 Texas residents including 50% females, 36.5% NHW, 25% NHB, 33.5% Hispanics, and 5% Asians/other (compared to Texas demographics, US Census, V2017: 50.3% females, 42% NHW, 12.7% NHB, 39.4% Hispanics, and 5% Asians).18 Oversampling of NHBs was conducted to ensure more accurate estimates for this minority group. Strata goals were also set for household income in Texas: 48% < $50,000; 30% $50,000–$100,000; 22% >$100,000.19 The NHW category was defined as non-Hispanics selecting white as the sole race and the NHB category as non-Hispanics selecting black/African American, either alone or with any other race. The recruitment target included 60% urban and 40% rural residents. To determine urbanization status, we matched respondent ZIP Codes to county, and county to rural/urban designation as defined by the Texas Department of State Health Services.20,21
Survey Design and Implementation
The Texas health screening survey was composed of 153 measures with the majority of questions derived from the National Health Interview Survey (NHIS), Health Information National Trends Survey (HINTS), and Behavioral Risk Factor Surveillance System Questionnaire, as detailed elsewhere.18 The instrument was prepared in both English and Mexican Spanish using the services of Masterword Services, Inc. (Houston, TX), and administered through the Qualtrics online survey platform (Qualtrics International Inc., Provo, UT and Seattle, WA). To identify any potential technical issues, the survey was piloted among 50 participants prior to full launch. Qualtrics managed survey implementation and compensation of opt-in panelists ($10 or its equivalent) between February 5 and March 5, 2018. Following collection of the first 1,600 complete responses, the sampling targets for Hispanics, lower income categories, and urban residents were primarily met. Subsequently, demographic strata were relaxed to meet the required sample size. The study protocol (PA16–0724) was approved by MD Anderson’s Institutional Review Board.
Outcome Measures
The primary outcome measures for sun protective behaviors were derived from the NHIS 2015 instrument focused on cancer.22 All respondents were presented with the stem question (ID NAF.020_00.000), “When you go outside on a warm sunny day for MORE than one hour, how often do you..,” followed by 6 individual measures: 1) Stay in the shade? 2) Wear a baseball cap or sun visor? 3) Wear a hat that shades your face, ears and neck such as a hat with a wide brim all around? 4) Wear a long sleeved shirt? 5) Wear long pants or other clothing that reaches your ankles? 6) Use sunscreen? Respondents had the choice to answer on a 5-point Likert scale: always, most of the time, sometimes, rarely, and never. An additional option, “Don’t go out in the sun” could also be selected. Several other sun-related exposures were assessed to determine level of SPF use and sunburn history. Two measures were derived from NHIS 2015: 1) What is the SPF number of the sunscreen you use MOST often? Response categories included, 1–14, 15–49, and 50 plus; and 2) During the past 12 months, how many times have you had a sunburn? This question was followed by a fill-in-the-blank response. Two additional measures were derived from the PhenX Toolkit (RTI International, Research Triangle Park, NC) (question ID 061300): 1) About how many blistering sunburns have you gotten in your life? This question was followed by a fill-in-the-blank response; and, 2) How old were you the first time you got a blistering sunburn? Response categories included under 5 years old, 5–15 years old, 15–24 years old, 25–39 years old, 40–64 years old, and 65 years old or older.
Covariates
The explanatory variable selected for this analysis was rural versus urban locale, determined as detailed above. Other covariates were analyzed based on their theoretical significance with sun protection behaviors, including respondent’s sex, age group, ethnicity and race, place of birth, educational attainment, marital status, occupation status, home ownership, and income range. Perception of financial stability was assessed using the question, “Which one of these comes closest to your own feelings about your household income these days?” Behaviors and health variables included smoking status, history and frequency of self-reported depression, diabetes, body mass index (BMI), and personal and family history of cancer.
Statistical Analysis
The analytical data set included 2,034 respondents.18 In order to calibrate the study sample to the state’s demographics, data were weighted by ICF International, Inc. (Fairfax, Virginia) using a 3-dimensional raking approach with iterative post-stratification based on: sex; 3-category age (18–44, 45–59, and 60 and over); and 4-category race/ethnicity (NHW, NHB, Hispanic, and other).23 Population data from the 2015 5-year American Community Survey (US Census Bureau, Suitland, MD) were used to compute weights at base and post-stratification stages. The weighted percentage of ages in the 18–44, 45–59, and 60+ group, sex, race and ethnicity were within 95% confidence intervals of the American Community Survey data aggregated over the state of Texas (see Appendix Table 1, available online only). The R “survey” package (The R Foundation, Vienna, Austria) was used to calculate means, proportions, percentages, and standard deviations. For all questions associated with the stem “When you go outside on a warm sunny day for MORE than one hour, how often do you..,” responses to outcome variables were collapsed into 3 levels: always/most of the time, sometimes, and rarely/never. The “Don’t go out in the sun” response was not included in the regressions. The multilevel response variable was modelled using the multinomial survey logistic regression with survey weights and analyses performed using PROC SURVEYLOGISTIC (SAS for Windows, version 9.4, SAS Institute Inc., Cary, NC) and the generalized logit link function to evaluate the significance of covariates with each of the sun protection behaviors. The category “rarely/never” was used as the reference group. Wald-test-based P values are reported to assess significance of each category of a predictor while adjusting for the presence of other predictors in the model. In addition, we also report type 3 analysis-based P values to assess overall significance of a predictor. The weighted Pearson’s χ2 test was used to determine significance between weighted rural and urban data for measures related to use of sunscreen, SPF level, and sunburn history.
Results
The overall study population included 1,219 respondents from urban and 815 from rural ZIP Codes with weighted mean (median) age of 41 (38) years and 48 (50) years, respectively. The baseline characteristics and weighted percentages for the rural and urban strata are shown in Table 1. Hispanics and NHBs were more prevalent in the urban group whereas NHWs were more prevalent in the rural group. Urban versus rural respondents were more likely to be born outside the US, be college graduates/postgraduates, employed, single/never married, and rent versus own their own home. On the other hand, rural respondents were more likely to be married and/or retired, be current or former smokers, and have class II or extreme obesity, although the incidence of diabetes was similar between groups. Household income distributions were largely comparable, and although the data suggested fewer rural residents reported financial difficulty, this was not significant. Of note, more rural versus urban respondents had a personal or family history of cancer.
Table 1.
Demographics and Health Characteristics of Rural and Urban Respondents
| VARIABLE | OVERALL | URBAN | RURAL | P Value | |||
|---|---|---|---|---|---|---|---|
| N | % Weighted | N | % Weighted | N | % Weighted | Rural vs Urban | |
| Respondents | 2034 | 100 | 1219 | 51.3 | 815 | 48.7 | |
| Gender (N= 2034) | .0016 | ||||||
| Female | 1348 | 50.8 | 803 | 26.0 | 545 | 24.8 | |
| Male | 686 | 49.2 | 416 | 25.3 | 270 | 24.0 | |
| Ethnicity / Race (N= 2034) | < .0001 | ||||||
| Hispanic | 764 | 35.7 | 558 | 26.2 | 206 | 9.5 | |
| White, non-Hispanic | 639 | 45.5 | 135 | 9.1 | 504 | 36.3 | |
| Black, non-Hispanic | 468 | 10.6 | 390 | 9.0 | 78 | 1.6 | |
| Others | 163 | 8.2 | 136 | 6.9 | 27 | 1.3 | |
| Born In USA(N= 2034) | < .0001 | ||||||
| No | 178 | 8.2 | 158 | 7.1 | 20 | 1.1 | |
| Yes | 1856 | 91.8 | 1061 | 44.1 | 795 | 47.6 | |
| Education (N= 2033) | .0077 | ||||||
| Less than 8 years | 21 | 0.8 | 14 | 0.5 | 7 | 0.3 | |
| 8 through 11 years | 93 | 4.2 | 44 | 1.8 | 49 | 2.5 | |
| 12 years or completed high school | 471 | 22.6 | 247 | 10.5 | 224 | 12.1 | |
| Post high school training other than college (vocational or technical) | 134 | 6.5 | 81 | 3.1 | 53 | 3.5 | |
| Some college | 610 | 29.9 | 358 | 14.7 | 252 | 15.2 | |
| College graduate | 508 | 25.5 | 339 | 14.7 | 169 | 10.8 | |
| Postgraduate | 196 | 10.4 | 135 | 6.0 | 61 | 4.4 | |
| Marital Status (N= 2033) | < .0001 | ||||||
| Divorced | 222 | 11.8 | 124 | 5.2 | 98 | 6.6 | |
| Living as married | 158 | 6.9 | 99 | 3.8 | 59 | 3.1 | |
| Married | 834 | 45.4 | 443 | 20.5 | 391 | 24.9 | |
| Separated | 52 | 2.4 | 27 | 1.0 | 25 | 1.4 | |
| Single, never been married | 696 | 29.2 | 489 | 19.0 | 207 | 10.2 | |
| Widowed | 71 | 4.4 | 36 | 1.9 | 35 | 2.5 | |
| Occupation Status (N= 2032) | < .0001 | ||||||
| Disabled | 122 | 6.7 | 46 | 2.0 | 76 | 4.7 | |
| Homemaker | 214 | 8.8 | 108 | 3.9 | 106 | 4.9 | |
| Retired | 237 | 16.0 | 115 | 5.8 | 122 | 10.2 | |
| Student | 136 | 5.2 | 100 | 3.4 | 36 | 1.8 | |
| Employed | 1050 | 50.6 | 688 | 29.2 | 362 | 21.4 | |
| Unemployed | 228 | 10.6 | 135 | 5.9 | 93 | 4.7 | |
| Other | 45 | 2.2 | 26 | 1.1 | 19 | 1.1 | |
| Rent Or Own (N= 2031) | < .0001 | ||||||
| Occupied without paying monetary rent | 199 | 9.0 | 115 | 4.4 | 84 | 4.7 | |
| Own | 1002 | 56.7 | 519 | 24.6 | 483 | 32.1 | |
| Rent | 830 | 34.3 | 583 | 22.3 | 247 | 12.0 | |
| Income Ranges (N= 2034) | .2492 | ||||||
| $0 to $9,999 | 212 | 8.7 | 122 | 4.5 | 90 | 4.2 | |
| $10,000 to $14,999 | 140 | 6.4 | 69 | 2.9 | 71 | 3.5 | |
| $15,000 to $19,999 | 138 | 6.4 | 89 | 3.5 | 49 | 3.0 | |
| $20,000 to $34,999 | 335 | 15.8 | 208 | 8.9 | 127 | 7.0 | |
| $35,000 to $49,999 | 351 | 17.6 | 222 | 9.4 | 129 | 8.1 | |
| $50,000 to $74,999 | 404 | 20.9 | 224 | 9.4 | 180 | 11.5 | |
| $75,000 to $99,999 | 215 | 11.0 | 131 | 5.8 | 84 | 5.2 | |
| $100,000 to $199,999 | 203 | 11.3 | 130 | 5.9 | 73 | 5.3 | |
| $200,000 or more | 36 | 1.9 | 24 | 1.0 | 12 | 0.9 | |
| Which one of these comes closest to your own feelings about your household’s income these days? (N= 2031) | .1471 | ||||||
| Finding it very difficult on present income | 190 | 8.7 | 110 | 4.4 | 80 | 4.3 | |
| Finding it difficult on present income | 416 | 19.8 | 243 | 19.8 | 173 | 9.7 | |
| Getting by on present income | 831 | 42.2 | 481 | 20.7 | 350 | 21.5 | |
| Living comfortably on present income | 594 | 29.4 | 383 | 16.1 | 211 | 12.2 | |
| Smoking (N= 2032) | < .0001 | ||||||
| Never smokers | 1286 | 58.9 | 845 | 34.7 | 441 | 24.2 | |
| Former smokers | 315 | 19.2 | 145 | 6.5 | 170 | 12.7 | |
| Current smokers | 431 | 21.9 | 228 | 10.1 | 203 | 11.8 | |
| Depression (N= 2032) | .1349 | ||||||
| Daily | 305 | 14.8 | 153 | 6.5 | 152 | 8.2 | |
| Weekly | 301 | 13.9 | 174 | 7.1 | 127 | 6.8 | |
| Monthly | 217 | 10.3 | 134 | 5.8 | 83 | 4.5 | |
| A few times a year | 615 | 30.4 | 385 | 16.1 | 230 | 14.3 | |
| Never | 594 | 30.7 | 371 | 15.7 | 223 | 14.9 | |
| Diabetes (N= 2032) | .6516 | ||||||
| Borderline | 150 | 7.3 | 91 | 3.9 | 59 | 3.4 | |
| No | 1646 | 79.6 | 995 | 41.0 | 651 | 38.5 | |
| Yes | 236 | 13.2 | 132 | 6.4 | 104 | 6.8 | |
| BMI (N=2002) | .0047 | ||||||
| Underweight (<18.5) | 63 | 3.0 | 39 | 1.7 | 24 | 1.3 | |
| Normal (18.5 to <25) | 568 | 27.2 | 368 | 14.9 | 200 | 12.2 | |
| Overweight (25 to <30) | 575 | 30.7 | 360 | 16.4 | 215 | 14.3 | |
| Obesity, Class I (30 to <35) | 387 | 19.3 | 228 | 9.8 | 159 | 9.5 | |
| Obesity, Class II (35 to <40) | 196 | 9.8 | 101 | 4.2 | 95 | 5.6 | |
| Extreme Obesity (40 or above) | 213 | 10.1 | 100 | 4.0 | 113 | 6.1 | |
| Personal history (N=2031) | .0243 | ||||||
| No | 1895 | (91.9) | 1151 | 47.9 | 744 | 44.0 | |
| Yes | 136 | (8.1) | 66 | 3.3 | 70 | 4.8 | |
| Family History (N= 2031) | < .0001 | ||||||
| No | 579 | (26.5) | 420 | 17.3 | 159 | 9.2 | |
| Not sure | 217 | (11.0) | 120 | 5.2 | 97 | 5.8 | |
| Yes | 1235 | (62.6) | 677 | 28.8 | 558 | 33.8 | |
Six measures were assessed to determine sun protection behaviors (Figure 1). Urban versus rural respondents were more likely to stay in the shade always/most of the time (50.0% versus 37.2%). However, the rural group was more likely to wear a cap or visor always/most of the time (38.9% versus 32.9%). The likelihood of wearing a wide-brimmed hat was low amongst both groups with about 55% rarely or never using this form of protection. Compared to their rural counterparts, urban respondents seemed a little more inclined to wear a long-sleeved shirt always/most of the time (19.3% versus 15.5%) and sometimes (27.1% versus 24.7%). However, the majority rarely/never used this type of clothing (51% urban, 57.6% rural). Use of long pants was largely similar between groups. With respect to sunscreen, consistent use seemed to be higher in the urban versus rural group (27.5% versus 24.2%). However, 46.2% of urban and 48.8% of rural respondents rarely or never used any sunscreen.
Figure 1.
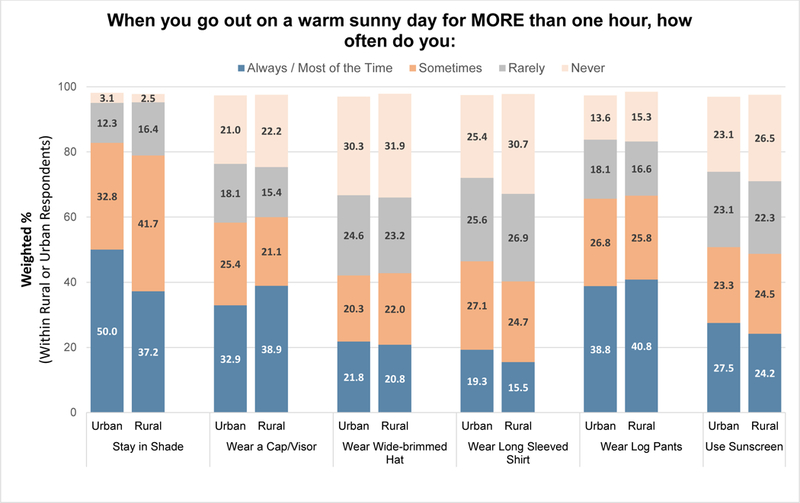
Sun Protection Behaviors
To determine if rurality was a significant factor for any of the sun protection behaviors, multinomial survey logistic regression analyses were performed across all outcomes that measured use of shade, sun protective clothing, and sunscreen. After adjusting for other possible relevant covariates, rurality was found to be a significant predictor for the 2 outcomes: when you go out on a warm sunny day for MORE than 1 hour, how often do you 1) stay in the shade, and 2) use sunscreen? (Table 2). Thus, rural compared to urban residents were less likely (always/most of the time versus rarely/never) to stay in the shade (OR = 0.58; P = .004, Type 3 P = .004) and use sunscreen (OR = 0.65; P = .013, Type 3 P = .044).
Table 2.
Factors Associated with Sun Protection Behaviors
| COVARIATES |
When you go out on a warm sunny day for MORE than one hour, how often do you STAY IN THE SHADE? |
When you go out on a warm sunny day for MORE than one hour, how often do you USE SUNSCREEN? |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sometimes vs rarely/never |
Always/most of the time vs rarely/never |
Sometimes vs rarely/never |
Always/most of the time vs rarely/never |
|||||||||||
| OR | 95% CI | P Value | OR | 95% CI | P Value | Type 3 P Value |
OR | 95% CI | P Value | OR | 95% CI | P Value | Type 3 P Value |
|
| Locale | .004 | .044 | ||||||||||||
| Rural vs Urban | 0.86 | 0.59–1.25 | .434 | 0.58 | 0.40–0.84 | .004 | 0.90 | 0.65–1.24 | .516 | 0.65 | 0.46–0.91 | .013 | ||
| SEX | < .001 | < .001 | ||||||||||||
| Female vs Male | 1.24 | 0.90–1.72 | .193 | 1.93 | 1.40–2.66 | < .001 | 1.41 | 1.06–1.88 | .020 | 2.58 | 1.92–3.47 | < .001 | ||
| AGE | .552 | .292 | ||||||||||||
| ≤ 22 years vs 56–65 years | 0.89 | 0.41–1.93 | .770 | 0.63 | 0.29–1.36 | .236 | 0.86 | 0.42–1.74 | .666 | 1.31 | 0.69–2.49 | .410 | ||
| 23–35 years vs 56–65 years | 0.87 | 0.48–1.59 | .648 | 0.87 | 0.47–1.60 | .643 | 1.20 | 0.70–2.06 | .499 | 1.38 | 0.84–2.29 | .205 | ||
| 36–55 years vs 56–65 years | 0.82 | 0.48–1.42 | .484 | 0.81 | 0.48–1.39 | .453 | 1.24 | 0.76–2.01 | .394 | 1.70 | 1.09–2.65 | .020 | ||
| ≥ 66 years vs 56–65 years | 0.72 | 0.35–1.48 | .375 | 1.22 | 0.57–2.58 | .610 | 0.73 | 0.38–1.42 | .352 | 1.14 | 0.63–2.10 | .662 | ||
| Race and Ethnicity | .136 | < .001 | ||||||||||||
| NHB vs NHW | 0.86 | 0.53–1.41 | .552 | 1.47 | 0.91–2.35 | .115 | 0.32 | 0.21–0.49 | < .001 | 0.29 | 0.18–0.45 | < .001 | ||
| Hispanic vs NHW | 0.91 | 0.60–1.39 | .661 | 1.18 | 0.78–1.77 | .437 | 0.70 | 0.48–1.01 | .056 | 0.66 | 0.45–0.95 | .026 | ||
| Other race vs NHW | 0.70 | 0.37–1.31 | .264 | 0.88 | 0.48–1.59 | .666 | 0.89 | 0.52–1.53 | .671 | 0.84 | 0.49–1.45 | .540 | ||
| Born in US | .461 | .175 | ||||||||||||
| No vs Yes | 0.91 | 0.50–1.68 | .768 | 1.20 | 0.68–2.12 | .531 | 0.63 | 0.39–1.03 | .064 | 0.79 | 0.50–1.25 | .308 | ||
| Education (vs 12 years/completed high school) | .518 | .453 | ||||||||||||
| Less than high school | 1.14 | 0.54–2.40 | .733 | 0.98 | 0.48–2.00 | .965 | 0.87 | 0.46–1.67 | .683 | 1.15 | 0.61–2.16 | .672 | ||
| Post High School/some college | 1.02 | 0.66–1.56 | .933 | 0.82 | 0.54–1.25 | .363 | 0.88 | 0.61–1.26 | .473 | 1.08 | 0.75–1.57 | .672 | ||
| College graduate/postgraduate | 1.31 | 0.82–2.09 | .252 | 0.90 | 0.57–1.42 | .647 | 1.13 | 0.77–1.67 | .526 | 1.47 | 0.98–2.18 | .060 | ||
| Marital Status | .449 | .144 | ||||||||||||
| Divorced/separated vs married/living as married | 0.98 | 0.57–1.66 | .928 | 1.19 | 0.71–1.97 | .509 | 0.92 | 0.58–1.48 | .743 | 1.77 | 1.15–2.73 | .010 | ||
| Single/never been married vs married/living as married | 1.41 | 0.95–2.09 | .092 | 1.41 | 0.95–2.09 | .085 | 1.02 | 0.71–1.46 | .929 | 1.25 | 0.87–1.80 | .225 | ||
| Widowed vs married/living as married | 1.82 | 0.64–5.23 | .264 | 1.69 | 0.58–4.94 | .341 | 0.71 | 0.34–1.47 | .355 | 0.94 | 0.43–2.05 | .881 | ||
| Total Household | 1.00 | 0.91–1.09 | .909 | 1.01 | 0.92–1.09 | .912 | .963 | 0.98 | 0.90–1.06 | .551 | 1.00 | 0.92–1.08 | .940 | .828 |
| Employment Status | .075 | .520 | ||||||||||||
| Disabled vs Employed | 1.93 | 0.85–4.40 | .118 | 1.84 | 0.86–3.94 | .117 | 0.67 | 0.34–1.32 | .250 | 0.51 | 0.26–0.99 | .046 | ||
| Homemaker vs Employed | 1.34 | 0.77–2.33 | .301 | 1.05 | 0.62–1.78 | .865 | 1.02 | 0.65–1.60 | .920 | 0.89 | 0.58–1.37 | .585 | ||
| Retired vs Employed | 0.69 | 0.27–1.74 | .429 | 0.73 | 0.30–1.76 | .482 | 1.35 | 0.60–3.04 | .466 | 0.85 | 0.34–2.16 | .735 | ||
| Student vs Employed | 1.59 | 0.80–3.15 | .183 | 0.95 | 0.47–1.94 | .896 | 0.98 | 0.52–1.85 | .954 | 0.93 | 0.53–1.61 | .781 | ||
| Unemployed vs Employed | 1.59 | 0.78–3.26 | .203 | 0.76 | 0.38–1.52 | .435 | 1.28 | 0.69–2.37 | .434 | 1.19 | 0.63–2.27 | .590 | ||
| Other vs Employed | 1.30 | 0.75–2.28 | .353 | 0.76 | 0.44–1.31 | .315 | 0.59 | 0.36–0.97 | .037 | 0.76 | 0.46–1.26 | .286 | ||
| Income | .237 | .239 | ||||||||||||
| <$20,000 vs $50,000 - $74,999 | 0.56 | 0.33–0.97 | .037 | 0.69 | 0.41–1.16 | .162 | 0.77 | 0.49–1.21 | .257 | 0.66 | 0.42–1.05 | .079 | ||
| $20,000 - $49,999 vs $50,000 - $74,999 | 0.83 | 0.53–1.33 | .441 | 0.75 | 0.48–1.17 | .209 | 0.87 | 0.60–1.27 | .465 | 0.68 | 0.47–0.99 | .043 | ||
| $75,000 - $99,999 vs $50,000 - $74,999 | 0.56 | 0.31–1.00 | .050 | 0.59 | 0.34–1.03 | .064 | 1.21 | 0.74–1.98 | .441 | 1.19 | 0.75–1.90 | .464 | ||
| ≥$100,000 vs $50,000 - $74,999 | 0.88 | 0.49–1.60 | .672 | 0.70 | 0.39–1.23 | .212 | 0.78 | 0.47–1.31 | .348 | 0.93 | 0.59–1.47 | .765 | ||
| Home Ownership | .705 | .262 | ||||||||||||
| Occupied vs Own | 0.67 | 0.37–1.19 | .168 | 0.74 | 0.42–1.33 | .315 | 0.76 | 0.45–1.28 | .302 | 0.64 | 0.37–1.10 | .106 | ||
| Rent vs Own | 0.85 | 0.58–1.24 | .387 | 0.93 | 0.65–1.32 | .671 | 0.86 | 0.62–1.19 | .361 | 0.74 | 0.54–1.00 | .048 | ||
| BMI | .238 | .215 | ||||||||||||
| Underweight vs normal | 0.61 | 0.25–1.53 | .294 | 1.14 | 0.46–2.79 | .780 | 1.21 | 0.54–2.70 | .641 | 1.43 | 0.68–3.01 | .346 | ||
| Overweight vs normal | 1.11 | 0.74–1.67 | .609 | 1.04 | 0.70–1.56 | .838 | 0.82 | 0.57–1.17 | .268 | 1.13 | 0.80–1.59 | .487 | ||
| Obesity Class I vs normal | 0.91 | 0.58–1.45 | .700 | 1.11 | 0.71–1.72 | .652 | 0.73 | 0.49–1.08 | .117 | 0.78 | 0.53–1.16 | .218 | ||
| Obesity Class II vs normal | 1.38 | 0.73–2.57 | .320 | 1.76 | 0.95–3.24 | .072 | 0.71 | 0.43–1.18 | .185 | 0.58 | 0.34–0.99 | .046 | ||
| Obesity Class III vs normal | 1.21 | 0.64–2.28 | .566 | 1.80 | 1.00–3.24 | .051 | 0.62 | 0.37–1.04 | .070 | 0.81 | 0.50–1.31 | .393 | ||
| Smoking Status | .375 | .018 | ||||||||||||
| Current vs Never | 1.25 | 0.83–1.88 | .285 | 0.93 | 0.63–1.39 | .730 | 0.61 | 0.43–0.88 | .008 | 0.67 | 0.46–0.97 | .034 | ||
| Former vs Never | 1.33 | 0.83–2.13 | .232 | 1.14 | 0.72–1.79 | .584 | 0.72 | 0.48–1.10 | .125 | 1.09 | 0.75–1.60 | .642 | ||
| Diabetes | .232 | .174 | ||||||||||||
| Borderline vs No | 0.82 | 0.45–1.48 | .501 | 0.69 | 0.39–1.22 | .196 | 0.92 | 0.56–1.52 | .743 | 0.68 | 0.39–1.19 | .175 | ||
| Yes vs No | 0.81 | 0.47–1.41 | .460 | 1.17 | 0.71–1.94 | .537 | 0.74 | 0.46–1.20 | .226 | 1.25 | 0.83–1.89 | .291 | ||
| Depression | .204 | .074 | ||||||||||||
| Few times per year vs Never | 1.34 | 0.90–2.01 | .153 | 1.14 | 0.77–1.69 | .519 | 1.31 | 0.92–1.85 | .133 | 0.94 | 0.67–1.32 | .722 | ||
| Daily/monthly/weekly vs Never | 0.99 | 0.67–1.47 | .965 | 1.16 | 0.80–1.70 | .438 | 0.90 | 0.63–1.29 | .572 | 0.72 | 0.51–1.01 | .054 | ||
| Cancer History, Personal | .242 | .015 | ||||||||||||
| Yes vs No | 0.70 | 0.37–1.32 | .272 | 1.07 | 0.59–1.95 | .819 | 1.36 | 0.78–2.38 | .284 | 2.14 | 1.27–3.61 | .004 | ||
| Cancer History, Family | .393 | .124 | ||||||||||||
| Not sure vs No | 1.23 | 0.69–2.20 | .485 | 0.91 | 0.52–1.59 | .727 | 0.75 | 0.46–1.22 | .249 | 0.78 | 0.47–1.29 | .329 | ||
| Yes vs No | 0.98 | 0.67–1.43 | .906 | 0.78 | 0.54–1.11 | .168 | 0.65 | 0.47–0.90 | .008 | 0.79 | 0.57–1.09 | .145 | ||
P values < .05 are bolded
Other factors associated with “stay in the shade” included sex and income. For example, females compared to males were more likely (always/most of the time versus rarely/never) to stay in the shade (OR = 1.93; P < .001). Factors associated with “use sunscreen” included sex, age, race and ethnicity, marital status, employment status, income, home ownership, obesity, smoking, and cancer history. For example, significantly increased use of sunscreen (always/most of the time versus rarely/never) was apparent amongst 36- to 55-year-olds compared to 56- to 65-year-olds (OR = 1.70; P = .020) and those with versus without personal history of cancer (OR = 2.14; P = .004). Decreased use of sunscreen was associated with being NHB versus NHW (OR = 0.29; P < .001), Hispanic versus NHW (OR = 0.66; P = .026), reporting $20,000 - $49,999 versus $50,000 - $74,999 household income (OR = 0.68; P = .043), and being current versus never smokers (OR = 0.67; P = .034). See Table 2 for full results.
The level of sunscreen protection used and sunburn history was also compared between rural and urban respondents (Table 3). A greater proportion of rural respondents used higher levels of SPF sunscreen (P < .001), although they tended to have more (4+) sunburns within the past 12 months (P < .001). Rural respondents also had significantly more lifetime blistering sunburns with 67% versus 45% reporting 3 or more such injuries (P < .001). These blistering sunburns were also more likely to occur at a younger age with 61.2% versus 43.2% reporting 5–14 years as the age of their first blistering sunburn (P < .001).
Table 3.
Sunscreen Use and Sunburn History
| Question | Overall | Rural | Urban | P Valuea | ||
|---|---|---|---|---|---|---|
| N | N | % weighted | N | % weighted | ||
| What is the SPF number of the sunscreen you use MOST often? | ||||||
| SPF 1–14 | 220 | 61 | 10.4 | 159 | 17.2 | < .001 |
| SPF 15–49 | 708 | 283 | 52.2 | 425 | 50.0 | |
| SPF 50+ | 509 | 222 | 37.4 | 287 | 32.8 | |
| sum | 1437 | 566 | 100 | 871 | 100 | |
| During the past 12 months, how many times have you had a sunburn? | ||||||
| Burns, 0 | 27 | 9 | 3.8 | 18 | 6.6 | < .001 |
| Burns, 1 | 158 | 71 | 37.8 | 87 | 37.2 | |
| Burns, 2 | 117 | 59 | 27.4 | 58 | 26.0 | |
| Burns, 3 | 59 | 25 | 10.9 | 34 | 16.1 | |
| Burns, 4+ | 67 | 39 | 20.0 | 28 | 14.1 | |
| sum | 428 | 203 | 100 | 225 | 100 | |
| About how many blistering sunburns have you gotten in your life? | ||||||
| Blistering burns, 0 | 76 | 23 | 3.3 | 53 | 9.9 | < .001 |
| Blistering burns, 1 | 165 | 55 | 10.6 | 110 | 23.7 | |
| Blistering burns, 2 | 183 | 95 | 19.1 | 88 | 21.4 | |
| Blistering burns, 3+ | 468 | 299 | 67 | 169 | 45 | |
| sum | 892 | 472 | 100 | 420 | 100 | |
| How old were you the first time you got a blistering sunburn? | ||||||
| <5 years old | 59 | 30 | 5.7 | 29 | 6.6 | < .001 |
| 5–15 years old, | 454 | 284 | 61.2 | 170 | 43.2 | |
| 15–24 years old, | 286 | 130 | 27.4 | 156 | 37.1 | |
| ≥ 25 years old | 85 | 25 | 5.7 | 60 | 13.1 | |
| sum | 884 | 469 | 100 | 415 | 100 | |
Weighted Pearson’s χ2 test-based P value
Discussion
This study compared current sun protection behaviors and prevalence of sunburn amongst rural and urban residents in Texas. After adjusting for a battery of covariates, our data show that rural residents in Texas were less likely to seek shade and less likely to apply sunscreen lotion compared to their urban counterparts. Interestingly, when sunscreen lotion was applied, rural versus urban residents were more likely to use a higher SPF. However, they reported more sunburns in the past 12 months and more blistering sunburns over the course of their life. Of particular importance, rural versus urban residents were more likely to have had blistering sunburns at an earlier age.
National estimates of sun protection behaviors have been summarized from NHIS 2015 data.11 In comparing our results, we find that both urban and rural residents in Texas versus the US as a whole were more likely to always/most of the time wear long-sleeved shirts (19.3% and 15.5%, respectively, versus 12.8%), long-sleeved pants (38.8% and 40.8%, respectively, versus 29.6%) and wide brimmed hats (21.8% and 20.8%, respectively, versus 14.7%). Urban residents in Texas were also more likely to always/most of the time stay in the shade (50% versus 39%) compared to national estimates. In contrast, the frequency of sunscreen use in Texas was lower, particularly amongst rural residents (24.2% versus 34.8% for US). Overall, these data suggest that Texas residents preferentially use shade and protective clothing rather than sunscreen application. Nonetheless, with routine use of shade and protective clothing falling short for many Texans, it is particularly concerning that sunscreen is an underused preventive measure. Sunscreen is known to decrease not only sunburn but also keratinocyte cancers, new nevi in children, and melanoma.24–26 Indeed, a recent large cohort study reported that using sunscreen SFP 15 or greater could reduce risk of melanoma by 18% in women age 40–75 years.27
Our findings on reduced sunscreen use and limited seeking of shade in rural compared to urban residents are in keeping with prior observations.28–30 Although one such study has largely attributed such variances to confounders, including demographic, regional, and behavioral differences in rural versus urban populations, our findings remained significant even after adjustment for these confounders and covariates.28 In agreement with national data and other studies, sunscreen use amongst our population positively correlated with being female, NHW and middle aged.9
It was encouraging to find more compliance with sunscreen use amongst those with a personal history of cancer compared to those with no cancer diagnosis. Indeed, increased sunscreen use has previously been reported amongst both rural and urban skin cancer survivors.28 However, other evidence across studies shows that 7%−38% of melanoma survivors never apply sunscreen.31 It was disappointing that there was only a marginal increase in sunscreen use amongst those with a family history of any cancer. That rural versus urban individuals may be less likely to modulate their behavior after a family diagnosis of skin cancer has been previously reported.28 Thus, despite increased awareness, other barriers are preventing personal uptake of preventative behavior change. Barriers to inconsistent sunscreen use are multifactorial and include anticipation of shade cover, perceptions of short periods of sun exposure, lack of time, and discomfort during intensive physical activity, amongst others.32 Intervention strategies to enhance risk reduction practices have had varying success.33–35
In our study, current versus never smokers were less likely to use sunscreen and this correlates with other reports describing decreased skin cancer protection amongst those engaged in risky health behaviors.36 Biased risk perceptions may help explain these observations. However, this is particularly concerning since smoking itself is a risk factor for squamous cell carcinoma.11,37 There was also some evidence suggesting a trend towards lower sunscreen use amongst those with lower income. Although underlying factors can be complex, this may be explained in part by lack of financial resources to routinely purchase sunscreen.
Particularly concerning was the much higher likelihood of rural versus urban residents to have experienced blistering sunburns, and most importantly between the early ages of 5–14 years. These types of injuries during childhood are associated with a greater risk of skin cancer compared to such injuries in older adults.38 The increased prevalence of blistering sunburns in rural respondents correlated with their lower use of sunscreen, even though they tended to use higher SPF compared to their urban counterparts. Paradoxically, use of sunscreen has been linked to increased prevalence of sunburn.27 For rural residents using sunscreen, it is possible that untimely reapplication as well as misjudgment of sunscreen effectiveness resulting in longer solar exposure times contributed to our findings. It is also feasible that increased likelihood of experiencing blistering sunburn amongst our rural compared to urban respondents is due to occupational hazards rather than intentions to tan, and increased outdoor leisure time activities.
Conclusions
Overall, our data highlight a distinct need for increased cancer prevention and control activities on sun protective behaviors across Texas, particularly for rural communities. Of importance, promotion of such behaviors is currently part of the Texas Cancer Plan.39 Targeting schools to better educate students, parents, teachers, and staff on the harms of sunburn and the benefits of sun protection behaviors is one such approach and national guidelines have been developed.40 Notably, Texas passed a state law in 2015 allowing students to carry and apply sunscreen at school.41 However, it is unclear how many parents are fully aware of this opportunity and how many urban and rural Texas schools are proactively encouraging such behavior. To enhance sun protection behaviors among children, sun safety programs have been developed for elementary grades, such as “Ray and the Sunbeatables,” with current dissemination across 44 states.42 Among national initiatives, municipality shade policies and improved availability of sunscreen at parks, recreation centers, sporting venues, and beaches are intended to promote stronger adherence to sun protection behaviors.9 Clearly, increased physician counseling, targeting those at high risk and with a history of blistering sunburn, would be expected to yield benefit. In Texas, policy makers have been educated on the harms of indoor tanning and this has led to new legislation banning minors from using public tanning bed facilities in Texas.43 Although it is clear that much more work needs to be done, our current findings should further help guide cancer prevention and control activities across the state, particularly in the rural areas.
Strengths and Limitations
The strengths and limitations of the overall survey have been discussed previously.18 Relevant to the current study, non-probability sampling may have enriched for respondents with a particular interest in cancer prevention and thus behaviors may not reflect the general Texas population. However, survey data were weighted to be representative of the state population and the weighted percentages of income, homeownership, and several other core measures matched well with the national Health Information National Trends Survey (HINTS) and Texas state Behavioral Risk Factors Surveillance System (BRFSS). Self-reporting of data may also be impacted by social desirability bias. The electronic mode of our survey primarily reached NHWs in the rural areas, although this may not reflect a major drawback in this particular analysis since NHWs are more at risk for skin cancer than NHBs and Hispanics. Our data were not adjusted for confounding variables such as occupational and recreational sun exposure, and therefore these factors cannot be accounted for. Finally, we did not apply adjustments for multiple comparisons, as for descriptive and exploratory studies such an adjustment is not considered necessary.44
Supplementary Material
Appendix: Table 1. Comparison of Select Characteristics of Texas Health Screening Survey with American Community Survey-Texas
Acknowledgments
Funding: This study was supported by the National Cancer Institute (5P30CA016672, and 5P30CA016672 Sub-Project ID: 5697 to S. Shete) and The Barnhart Family Distinguished Professorship in Targeted Therapy to S. Shete.
Footnotes
Disclosures: The authors declare no conflicts of interest.
References
- 1.Apalla Z, Lallas A, Sotiriou E, Lazaridou E, Ioannides D. Epidemiological trends in skin cancer. Dermatol Pract Concept. 2017;7(2):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Key Statistics for Basal and Squamous Cell Skin Cancers. American Cancer Society. Available at: https://www.cancer.org/cancer/basal-and-squamous-cell-skin-cancer/about/key-statistics.html Accessed on: October 9, 2018.
- 3.Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015;151(10):1081–1086. [DOI] [PubMed] [Google Scholar]
- 4.Key Statistics for Melanoma Skin Cancer. American Cancer Society. Available at: https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html Accessed on: November 5, 2018.
- 5.Cronin KA, Lake AJ, Scott S, et al. Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics. Cancer. 2018;124(13):2785–2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cancer Statistics Center. American Cancer Society. Available at: https://cancerstatisticscenter.cancer.org Accessed on: August 9, 2018.
- 7.Texas Department of Health State Services. Available at: https://www.dshs.texas.gov/chs/hprc/counties.shtm Accessed on: July 2, 2018.
- 8.State Cancer Profiles. National Cancer Institute, Available at: http://statecancerprofiles.cancer.gov/index.html Accessed on: July 31, 2018.
- 9.Tripp MK, Watson M, Balk SJ, Swetter SM, Gershenwald JE. State of the science on prevention and screening to reduce melanoma incidence and mortality: The time is now. CA Cancer J Clin. 2016;66:460–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Indini A, Brecht I, Del Vecchio M, Sultan I, Signoroni S, Ferrari A. Cutaneous melanoma in adolescents and young adults. Pediatr Blood Cancer. 2018:e27292. [DOI] [PubMed] [Google Scholar]
- 11.American Cancer Society. Cancer Prevention & Early Detection Facts & Figures, 2017–2018. Available at: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-prevention-and-early-detection-facts-and-figures/cancer-prevention-and-early-detection-facts-and-figures-2017.pdf Accessed on: July 30, 2018.
- 12.Garbe C, Leiter U. Melanoma epidemiology and trends. Clin Dermatol. 2009;27(1):3–9. [DOI] [PubMed] [Google Scholar]
- 13.Division of Cancer Prevention and Control, Centers for Disease Control and Prevention. Skin Cancer Prevention Fact Sheets. Available at: http://www.cdc.gov/cancer/skin/basic_info/fact_sheets.htm. Accessed on: August 11, 2018.
- 14.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends. Cancer Epidemiol Biomarkers Prev. 2017;26(7):992–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rural Health Information Hub, Texas. Available at: https://www.ruralhealthinfo.org/states/texas Accessed on: August 13, 2018.
- 16.Aging in Texas. Texas Demographic Center, June 2016. Available at: http://demographics.texas.gov/Resources/publications/2016/2016_06_07_Aging.pdf Accessed on: July 3, 2018.
- 17.Shomaker TS. The Texas physician workforce: current status and future direction. Tex Med. 2009;105(11):e1. [PubMed] [Google Scholar]
- 18.Cunningham SA, Yu R, Shih YT, et al. Perceived Cancer-related Risks and Beliefs in Texas: Findings rom a 2018 Population-level Survey. In Press, Cancer Epidemiol Biomarkers Prev. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Household Income in Texas. Statistical Atlas. Available at: https://statisticalatlas.com/state/Texas/Household-Income Accessed on: February 13, 2018.
- 20.Definitions of County Designations. Texas Health and Human Services. Available at: https://www.dshs.texas.gov/chs/hprc/counties.shtm Accessed on: February 13, 2018.
- 21.Texas ZIP Codes. Available at: https://www.zip-codes.com/state/tx.asp accessed on: February 13, 2018.
- 22.National Health Interview Survey (NHIS), 2015. Available at: https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm Accessed on: July 14, 2018.
- 23.Mercer A, Lau A, Kennedy C. Pew Research Center. For Weighting Online Opt-In Samples, What Matters Most? Available at: http://assets.pewresearch.org/wp-content/uploads/sites/12/2018/01/26170902/Weighting-Online-Opt-In-Samples.pdf Accessed on: July 23, 2018.
- 24.Green A, Williams G, Neale R, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet. 1999;354(9180):723–729. [DOI] [PubMed] [Google Scholar]
- 25.Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329(16):1147–1151. [DOI] [PubMed] [Google Scholar]
- 26.Gallagher RP, Rivers JK, Lee TK, Bajdik CD, McLean DI, Coldman AJ. Broad-spectrum sunscreen use and the development of new nevi in white children: A randomized controlled trial. JAMA. 2000;283(22):2955–2960. [DOI] [PubMed] [Google Scholar]
- 27.Ghiasvand R, Weiderpass E, Green AC, Lund E, Veierod MB. Sunscreen Use and Subsequent Melanoma Risk: A Population-Based Cohort Study. J Clin Oncol. 2016;34(33):3976–3983. [DOI] [PubMed] [Google Scholar]
- 28.Zahnd WE, Goldfarb J, Scaife SL, Francis ML. Rural-urban differences in behaviors to prevent skin cancer: an analysis of the Health Information National Trends Survey. J Am Acad Dermatol. 2010;62(6):950–956. [DOI] [PubMed] [Google Scholar]
- 29.Michielutte R, Dignan MB, Sharp PC, Boxley J, Wells HB. Skin cancer prevention and early detection practices in a sample of rural women. Prev Med. 1996;25(6):673–683. [DOI] [PubMed] [Google Scholar]
- 30.Moore J, Zelen D, Hafeez I, Ganti AK, Beal J, Potti A. Risk-awareness of cutaneous malignancies among rural populations. Med Oncol. 2003;20(4):369–374. [DOI] [PubMed] [Google Scholar]
- 31.Nahar VK, Allison Ford M, Brodell RT, et al. Skin cancer prevention practices among malignant melanoma survivors: a systematic review. J Cancer Res Clin Oncol. 2016;142(6):1273–1283. [DOI] [PubMed] [Google Scholar]
- 32.Shuk E, Burkhalter JE, Baguer CF, et al. Factors associated with inconsistent sun protection in first-degree relatives of melanoma survivors. Qual Health Res. 2012;22(7):934–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Geller AC, Emmons KM, Brooks DR, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107(4):806–814. [DOI] [PubMed] [Google Scholar]
- 34.Manne S, Jacobsen PB, Ming ME, Winkel G, Dessureault S, Lessin SR. Tailored versus generic interventions for skin cancer risk reduction for family members of melanoma patients. Health Psychol. 2010;29(6):583–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gritz ER, Tripp MK, Peterson SK, et al. Randomized controlled trial of a sun protection intervention for children of melanoma survivors. Cancer Epidemiol Biomarkers Prev. 2013;22(10):1813–1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the U.S. population. Am J Prev Med. 2008;34(2):87–93. [DOI] [PubMed] [Google Scholar]
- 37.Dusingize JC, Olsen CM, Pandeya NP, et al. Cigarette Smoking and the Risks of Basal Cell Carcinoma and Squamous Cell Carcinoma. J Invest Dermatol. 2017;137(8):1700–1708. [DOI] [PubMed] [Google Scholar]
- 38.Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Shibuya KC, Patnode CD. Behavioral Counseling for Skin Cancer Prevention: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville, MD: U.S. Preventive Services Task Force; 2018. [PubMed] [Google Scholar]
- 39.Texas Cancer Plan 2018. Available at: http://www.cprit.state.tx.us/images/uploads/tcp2018_web_09192018.pdf Accessed on: November 8, 2018. [Google Scholar]
- 40.Glanz K, Saraiya M, Wechsler H, Centers for Disease C, Prevention. Guidelines for school programs to prevent skin cancer. MMWR Recomm Rep. 2002;51(RR-4):1–18. [PubMed] [Google Scholar]
- 41.Legislature of the State of Texas. Act of June 1, 2015: 84th Legislature, Regular Session, Ch. 1139, §1, 2015. Texas General Laws 3849–3850 (codified at Texas Education Code §38.021). Austin, TX: Texas Legislative Counsel; 2015; Avaialble at: https://texas.public.law/statutes/tex._educ._code_section_38.021 Accessed on: August 13, 2018. [Google Scholar]
- 42.Ray and the Sunbeatables. Available at: https://sunbeatables.org/ Accessed on: August 13, 2018.
- 43.Tripp MK, Gershenwald JE, Davies MA, et al. Assessment of Compliance With Texas Legislation Banning Indoor UV Tanning by Minors. JAMA Dermatol. 2016;153(2):228–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schochet PZ. Technical methods report: Guidelines for multiple testing in impact evaluations (NCEE No. 2008–4018). Washington, DC: National Center for Educational Evaluation and Regional Assistance, Institute of Education Sciences, U.S. Department of Education; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Table 1. Comparison of Select Characteristics of Texas Health Screening Survey with American Community Survey-Texas


