Abstract
Purpose:
Identifying factors associated with physical activity after dysvascular lower limb amputation could provide targets for improving rehabilitation outcomes. The purpose of this meta-synthesis was to identify modifiable factors that may influence physical activity after dysvascular lower limb amputation, a condition characterized by amputation in the setting of older age, diabetes mellitus, and/or peripheral artery disease.
Methods:
A systematic search of the literature identified qualitative studies exploring the perceptions of physical activity in people with lower limb amputation, older age, diabetes mellitus, or peripheral artery disease. Qualitative rigor was assessed using the McMaster University’s Guidelines for Qualitative Review. Meta-synthesis was undertaken to analyze the findings of included studies.
Results:
Fourteen studies of variable methodological quality were included for analysis. Three overarching factors that may influence physical activity after dysvascular lower limb amputation emerged: 1) educational experiences and motivation, 2) support and self-efficacy, and 3) special concerns after lower limb amputation (e.g., prosthesis, equipment, environment).
Conclusions:
Physical activity after dysvascular lower limb amputation is influenced by relationships among health understanding, motivation, support, and self-efficacy in the presence of disability. Themes from this meta-synthesis can be used to develop and test behavior-based interventions to improve physical activity after dysvascular lower limb amputation.
Keywords: Dysvascular Amputation, Chronic Disease, Qualitative Meta-synthesis, Physical Activity, Behavior
Introduction
Dysvascular lower limb amputation (LLA), amputation due to complications of type II diabetes mellitus (DM) and/or peripheral artery disease (PAD), is characterized by low levels of physical activity [1,2]. People with DM are less physically active than people of similar age without DM, and even lower physical activity is common after dysvascular LLA. People with dysvascular LLA take an average of 1721–3809 steps/day [2,3], falling well below the recommended 6,500 steps/day for people with physical disability [4]. Although the extremely low physical activity behavior frequently is unaddressed within rehabilitation, there may be implications for rehabilitation intervention [3,5].
Greater age, medical complexity, mortality, and severe disability distinguish people with dysvascular LLA as a unique population when compared to limb loss of traumatic etiology [6,7]. An analysis of data from the Center for Medicare & Medicaid Services of people with dysvascular LLA demonstrated that the mean age is 75 years old, 45% of people have four or more comorbid conditions, and 41% mortality one year after amputation [8]. Observational studies measuring functional capacity at 12 months after dysvascular LLA report poor physical function with only 39% returned to prior level of mobility [9], and 60% were able to ambulate in the community [10]. Physical function as measured by the two-minute walk test, timed up-and-go, and L-test are significantly correlated with physical activity after dysvascular LLA, although a significant relationship between physical activity and number of comorbid conditions was not found [2,3]. Although physical function may improve after discharge from rehabilitation, increased physical activity is not often realized after dysvascular LLA [3]. The marginal changes in physical activity may be due to non-physical factors, including psychosocial adjustment [11]. Psychosocial adjustment after LLA (e.g., depression, anxiety, coping) and relationships with rehabilitation outcomes have been extensively studied [11]. For example, finding positive meaning after amputation (coping) is associated with lower levels of depressive symptoms [12], and the presence of depressive symptoms is related to high activity restrictions [13]. Unfortunately, there is limited research focus on the unique population of people with dysvascular LLA [11]. Qualitative inquiry is ideally suited to explore the potential factors that may influence physical activity and guide development of rehabilitation interventions for people after dysvascular LLA, a shortcoming of current quantitative methods in this population.
Interventions based in concepts of behavior change effectively increase physical activity in populations with chronic disease and disability but have not been developed for people with dysvascular LLA [14,15]. For example, motivational interviewing is a patient-centered approach to communication in which patients can explore their own goals and motivations for behavior change. Interventions using this type of framework can focus discussion on psychosocial targets including fear of injury, social support, exercise knowledge, and pain to increase motivation and self-efficacy for increased physical activity in patients with DM and PAD [16–18]. To develop such behavior-based interventions for people with dysvascular LLA, the specific psychosocial factors that influence physical activity behavior must be identified and understood.
Qualitative meta-synthesis is a technique that can be used to gain a deeper understanding of rehabilitation-related phenomena such as physical activity in the context of a patient’s social world [19,20]. Qualitative meta-synthesis uses an interpretive process to analyze similar and unique findings within and across interpretive studies to build and develop theory [21]. The interpretations of multiple interpretive studies leads to a deeper and novel understanding of a phenomena that would otherwise not be possible with one singular study [19,21]. For example, Murray and Forshaw conducted a qualitative meta-synthesis of 15 qualitative manuscripts to better understand the experience of using a prosthesis after amputation [22]. In their meta-synthesis, the authors describe the essence of using a prosthesis after limb-loss with five distinct concepts: becoming an amputee and facing prosthesis use, adjustment to and coping with amputation and prosthesis use, the role of valued relationships in recovery, amputation and prosthesis use in social interaction, and prosthetically enabled identities [22]. The deeper understanding gained from qualitative meta-synthesis provides a foundation for developing rehabilitation interventions to improve coping strategies and education delivery with people after limb-loss [22].
The purpose of this qualitative meta-synthesis was to identify factors that may influence participation in physical activity specifically for people with dysvascular LLA, an amputation in the setting of older age, DM, and/or PAD. The findings of this qualitative meta-synthesis are meant to set the foundation for developing interventions to increase physical activity after dysvascular LLA.
Methods
Study design
Qualitative meta-synthesis of primary qualitative studies was guided by a senior PhD-prepared qualitative researcher, informed by a critical realist approach, and in line with established standards [20,23–25]. The critical realist approach was used to clarify and deepen our understanding of complex social phenomena and better describe potential causes of low physical activity behavior after dysvascular LLA [26]. A defining feature of the critical realist approach is that knowledge is only gained by what has been experienced or represented to us. Therefore, talk is the communication of a persons’ experience and knowledge of a phenomena that can be interpreted.
Key meta-synthesis strategies included use of a structured question, search and appraisal review, reciprocal translation, and interdisciplinary interpretive triangulation. Developing and using a structured research question guided the systematic search of literature, selection of studies to be included, and analysis [19,21,27]. Systematic search was undertaken to identify studies that would be used to develop a meaningful synthesis [27]. Included studies were appraised to critically consider the reporting of qualitative findings [21,27,28]. Reciprocal translation is an approach used to understand where our new interpretive findings are positioned within and across the original dataset [29]. Primary studies were examined for how and where evidence of our derived themes to answer our research question could be located as an audit trail for interpretation [23]. Our research team consists of multiple disciplinary perspectives that bring discrete and similar interpretive lenses to our research question. Through discussion, debate, and contextual explanation, our team builds consensus over time about language, naming, and nature of themes identified [30]. For example, difference of opinion for code definitions were resolved with debate from the disciplinarily perspectives of team members. Through this thoughtful discussion of language, interpretive lens, and context, code definitions were refined in an iterative process and agreed upon by the research team. This interdisciplinary interpretive triangulation is used to introduce unique perspectives throughout a study to strengthen the interpretive process of meta-synthesis, considering and discussing concepts that may otherwise be implied [24,30,31].
Search strategy
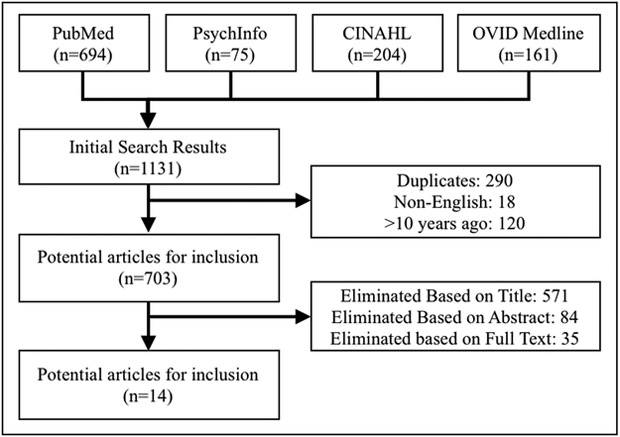
Potential qualitative studies to be included were identified by searching PubMed, Ovid Medline, PsychInfo, and CINAHL databases. Search terms were selected and combined to identify a broad range of qualitative research related to physical activity within the context of 1) DM, 2) PAD, 3) Disability, or 4) Amputation. An initial search, conducted in July of 2017, retrieved 1131 possible articles for review (figure 1). The retrieved manuscript titles, abstracts and full texts were reviewed by two authors (MJM and CBA) for relevance to the research question using inclusion criteria. Inclusion criteria were 1) primary qualitative research studies exploring perceptions of physical activity participation and 2) study samples focusing on aging, type II DM, PAD, or LLA. In the event there was a disagreement about inclusion in the final dataset (MJM and CBA), the manuscript was discussed with the interdisciplinary team to determine if the study would provide meaningful insight to the research question. The final data set was agreed upon by the interdisciplinary research team.
Figure 1.
Search strategy using search terms “Qualitative” and “Physical Activity” and (“Disabled” or “Disability” or “Diabetes Mellitus” or “Peripheral Artery Disease” or “Amputation” or “Amputee”)
Appraisal and analysis
Critical appraisal of manuscripts was completed using the McMaster University Guidelines for Qualitative Review [32]. The McMaster University Guidelines for Qualitative Review is a well-established tool comprising of 24 questions used to assess the rigor of the primary qualitative studies using responses of yes, no, or not addressed. Specific domains or rigor that were assessed with this tool included: study purpose, literature review, study design, sampling strategy, data collection methods, data analysis methods, overall rigor, and conclusions.
Manuscripts were independently evaluated by the first author (MJM). Evaluations were discussed with a co-author (CBA) to obtain agreement. Disagreements were arbitrated by the second author, a senior PhD prepared qualitative researcher. There is no consensus for exclusion of qualitative studies from meta-synthesis based upon critical appraisal [21,28]. Therefore, appraisal was used to critically consider the reporting of qualitative studies, and not used for exclusion of a study from analysis.
This meta-synthesis was led by the first author, and guided by regular discussions with the research team [21,27]. The goal of the analysis was to answer the following research question: What factors may influence participation in physical activity after dysvascular LLA (an amputation in the setting of older age, DM, and/or PAD)? Analysis began with reading and re-reading the manuscripts to become familiar with the data (MJM and CBA). The primary manuscript interpretations (e.g., themes, theory, conceptual analysis) were coded by the first author (MJM). Codes were reviewed and discussed among the research team to refine coding and resolve disagreement. After initial coding was complete, codes were combined into sub-themes and themes relevant to the research question (MJM and CBA). Themes were then refined by the research team in an iterative process of splitting, merging, condensing, and defining over a period of three months. Reciprocal translation of the emergent themes was carried out by the research team to understand our findings within the context of the original dataset and enhance trustworthiness of our interpretations. Reciprocal translation was conducted by identifying what primary studies contained our emergent themes. Finally, the research team discussed 1) the consistency of our findings within and across the included studies, 2) how the findings lead to a deeper understanding of a person’s social world of physical activity, and 3) how the findings may inform clinical practice.
Results
Search results and study characteristics
After screening and assessment, fourteen articles were included for analysis (table 1). Primary reasons for article exclusion were no focus on physical activity (n=514), study samples including adolescents (e.g., type I DM; n = 108) or people with neurologic disorders (e.g., multiple sclerosis, spinal cord injury, stroke; n = 100), and use of quantitative or mixed methodologies (n = 106). Of the final fourteen manuscripts, four studies collected qualitative data using focus groups [33–36], nine conducted single session one-to-one semi-structured interviews [37–45], and one study collected qualitative data over a four-year duration with four one-to-one semi-structured interview sessions [46]. The sample sizes for the included studies ranged from nine to forty-eight participants. Data were analyzed using phenomenology, framework qualitative, qualitative descriptive, and grounded theory.
Table 1.
Description of studies.
| Authors | Study Purpose | Country | Study Design | Methods | Participants | Summary of Findings |
|---|---|---|---|---|---|---|
| [33] Casey et al., 2010 | Assess barriers and facilitators of participation in a supervised exercise program, and adherence to exercise after program completion. | Canada | Phenomenology | Focus group interviews (1.25 hours) | 16 overweight participants (7 women) with type 2 DM who engaged in a supervised exercise program (mean age: 52 years) | Six themes were described: Individual motivation, the importance of supervision/support in exercise program participation, difficulty of transitioning, derailment of exercise participation, program characteristics, walking |
| [37] Crawford et al., 2016 | Qualitatively investigate the barriers and facilitators to physical activity participation in the transtibial osteomyoplastic amputation population. | United States | Phenomenology | One-to-one semi-structured interviews (duration not reported) | 9 men with transtibial osteomyoplastic amputation that were prosthetic users (mean age: 41 years) | The International Classification of Functioning was used to describe barriers and facilitators to physical activity after transtibial osteomyoplastic amputation. |
| [38] Cunningham et al., 2014 | Explore the beliefs and physical activity behavior of patients with peripheral artery disease who have received vascular intervention. | United Kingdom | Phenomenology | One-to-one semi-structured interviews (duration not reported) | 20 people (9 women) who had a vascular procedure due to peripheral artery disease (mean age: 70 years) | Five key themes were identified: walking avoidance, treatable condition, causal beliefs, perceived consequences, and surgeon patient communication |
| [39] Ferrand et al., 2008 | Examine perceived motives for regular physical activity in male and female individuals with type 2 DM who were involved in one patients’ association. | France | Phenomenology | One-to-one semi-structured interviews (1 hour) | 23 participants (14 women) with type 2 diabetes, who participated in 1 year of physical activity with a patients’ association: ‘Move for Health’ (mean age: 56 years [women], 67 years [men]) | Two categories of themes emerged social and psychological. Social themes included: live in a convivial team atmosphere, feel understood and well-supported by others, rediscover the notion of pleasure in a group (women only). Psychological themes included: improve sense of well-being, promote health benefits, and promote a positive body image (women only) |
| [40] Galea Holmes et al., 2017 | Explore illness and treatment beliefs, and experiences of walking among people with intermittent claudication | United Kingdom | Framework Qualitative | One-to-one semi-structured interviews (1-1.25 hours) | 19 participants (6 women) diagnosed with PAD with intermittent claudication (mean age: 66 years old) | 2 superordinate themes emerged: walking is an overlooked self-management opportunity and tailored walking guidance is desired. 5 subthemes emerged: intermittent claudication is benign and leg pain can be overcome, intermittent claudication is severe and there is nothing I can do, varied outcome expectations of walking, barriers to walking to intensity, and limited purposeful walking for exercise |
| [34] Gorely et al., 2015 | Explore individuals’ experience of living with peripheral artery disease, their knowledge about the condition, and their thoughts about physical activity and intervention programs. | United Kingdom | Phenomenology | Focus group interviews | 24 participants (7 women) with intermittent claudication secondary to peripheral artery disease (mean age: 71 years) | Two overriding themes of uncertainty lack of support and empathy surrounding physical activity and peripheral artery disease emerged. |
| [41] Gupta et al., 2016 | Determine perceptions of physical activity held by South Asians and compare them with the views held by members of the Anglo-Australian host population living with type 2 DM and or cardiovascular disease | Australia | Phenomenology | One-to-one semi-structured interviews (0.75 - >2 hours) | 41 South Asian (20 women), and 16 Anglo-Australian (8 women) participants, all with either type 2 diabetes and/or cardiovascular disease. (mean age: 61 years [ South Asian], 59 years [Anglo-Australian]) | Eight key themes emerged: defining physical activity, knowledge of value of physical activity for health maintenance and disease management, perceptions of advice provided by health professionals, personal and ethnic identity tied to physical activity identity, perceptions held by South Asians and Anglo-Australians about their own physical activity, the environment: social and physical intersections, and employment, retirement and physical activity |
| [35] Hardy et al., 2009 | Investigate in depth, salient influences on the choice to exercise in older adults. | United Kingdom | Grounded Theory | Focus group interviews (up to 1.5 hours) | 48 participants (42 women) over 50 years of age (mean age: 69 years) | Six predictors of physical activity emerged: preventing health decline, enjoyment, others as motivators to exercise, superior to younger generations, being out in daylight, and limited appreciation for older people’s needs |
| [42] He et al., 2013 | Explore factors influencing adherence to exercise in Chinese people with type 2 DM | China | Phenomenology | One-to-one semi-structured interviews (1-1.5 hours) | 17 participants (6 women) with type two diabetes (mean age: 58 years) | Six themes emerged: beliefs about the disease, health communication, feasibility of regimen, conducting skills, environmental support, perceived benefits. |
| [43] Littman et al., 2017 | Examine barriers and facilitators to physical activity that persons with lower extremity amputation face. | United States | Phenomenology | One-to-one semi-structured interviews (0.5-1.5 hours) | 27 Veterans (0 women) with lower extremity amputation (mean age: 54 years) | Nine themes related to barriers and facilitators of physical activity after amputation included: routine/purpose, social support, perceived benefits and cost, acceptance, active history, resources, health, self-efficacy, prosthesis issues |
| [36] Mier et al., 2007 | Examine perceptions of physical activity in a population of Mexican-Americans who have type 2 DM to identify motivators and barriers to physical activity in this group. | United States | Phenomenology | Focus group interviews (1-1.5 hours) | 39 participants (34 women) with type 2 DM (mean age: 34 years) | Motivators for physical activity included: sense of physical and mental well-being, family support. Key barriers included: environmental factors, physical pain, depression, being overweight, unsafe neighborhoods and lack of facilities. |
| [46] Peel et al., 2010 | Explore type 2 DM patients’ talk about implementing and sustaining physical activity | United Kingdom | Phenomenology | One-to-one semi-structured interviews, four times after diagnosis (1-3 hours) | 20 participants (9 women) with type 2 DM (mean age: 61 years) | Three themes emerged: incidental walking, incremental physical activity gains, augmenting physical activity maintenance. |
| [44] Rosenberg et al., 2013 | Gain a better understanding of how the built environment impacts neighborhood based physical activity among midlife and older adults with mobility disabilities. | United States | Qualitative Descriptive | One-to-one structured/semi-structured interviews (2 hours) | 35 participants (26 women), >50 years of age, used an assistive device to ambulate, and leave the home at least 3 days a week. (mean age: 67 years) | Environmental barrier/facilitator features were identified (i.e., curbs/ramps, parking, aesthetics, lighting, etc.) |
| [45] Sriskantharajah et al., 2007 | Explore influences on, and attitudes towards, physical activity among South Asian women in the UK with coronary heart disease and DM. | United Kingdom | Phenomenology | One-to-one, semi-structured interviews (1-2 hours) | 15 South Asian women with coronary heart disease and/or type 2 DM (mean age: 52 years) | Seven themes emerged: perceived harm threshold limits activity, insufficient guidance from health professionals about suitable activity, weight loss, maintaining independence and socializing perceived as main benefits of exercise, some understanding of benefit of exercise to improve and limit illness, exercise beyond daily work seen as a ‘selfish’ activity, discomfort with exercising in public, and constrained by not being able to speak English. |
Appraisal of the articles revealed variable degrees of rigor (table 2). All studies clearly stated the purpose of the research study, provided adequate review of the literature, and used appropriate sampling strategies. Five of the fourteen studies clearly detailed rigorous qualitative methods [33,39,40,42–44]. Three studies met three of the four criteria [35,38,45], and the remaining five studies clearly met one of the four criteria for qualitative rigor [33,34,36,41,46]. The greatest weaknesses across studies were auditability, dependability, and confirmability. Only four studies clearly reported methods for auditability [37,38,42,44]. Studies demonstrating dependability and confirmability clearly articulated methods of triangulation, member checking, data analysis strategies, and maintaining neutrality of data [35,37–40,42–44].
Table 2.
Summary of study appraisals.
| Overall Rigor Criteria | Credibility: Are descriptions and interpretations of participants’ experiences recognizable? |
Transferability: Can the findings be transferred to other situations? |
Dependability: Is there a clear explanation of the research methods? |
Confirmability: Were strategies employed to minimize bias? |
|---|---|---|---|---|
| [33] Casey et al | no | yes | no | no |
| [37] Crawford et al | yes | yes | yes | yes |
| [38] Cunningham et al | yes | no | yes | yes |
| [39] Ferrand et al | yes | yes | yes | yes |
| [40] Galea-Holmes et al | yes | yes | yes | yes |
| [34] Gorely et al | yes | no | no | no |
| [41] Gupta et al | no | yes | no | no |
| [35] Hardy et al | yes | no | yes | yes |
| [42] He et al | yes | yes | yes | yes |
| [43] Littman et al | yes | yes | yes | yes |
| [36] Mier et al | no | yes | no | no |
| [46] Peel et al | no | yes | no | no |
| [44] Rosenburg et al | yes | yes | yes | yes |
| [45] Sriskantharajah et al | yes | yes | no | yes |
Studies were primarily conducted in urban and suburban environments in Europe, North America, Australia, and Asia (table 1). Represented patient groups included people with LLA, older adults (>50 years of age), DM and/or PAD. An aggregate of 353 participant experiences were included in our final dataset.
Meta-synthesis
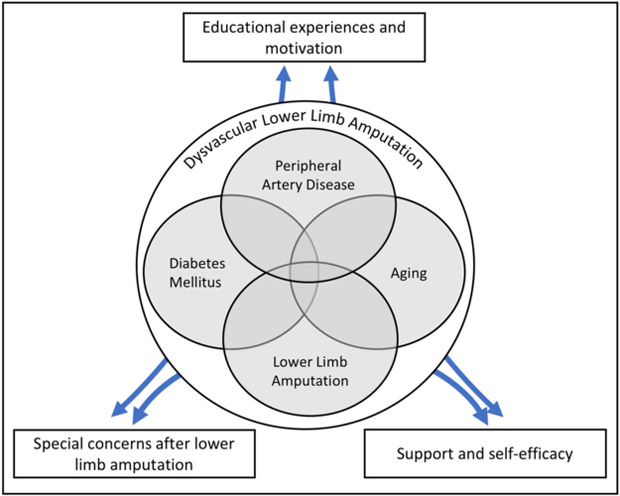
Three interdependent themes emerged from this meta-synthesis aimed at identifying factors influencing physical activity after dysvascular LLA (figure 2): 1) educational experiences and motivation, 2) support and self-efficacy, and 3) special concerns after LLA.
Figure 2.
Theoretical figure of factors influencing physical activity after dysvascular lower limb amputation
Participant definitions of physical activity were highly variable. Physical activity, used interchangeably with exercise, consisted of structured strengthening programs [33], aerobic activities (e.g., running, cycling) [37,41,43,46], home and social activities (e.g., cleaning, gardening, dancing) [34,36,42], and organized sports [37,41]. Finally, walking was commonly perceived as a form of physical activity that was safe and feasible to integrate into everyday living [33,34,36–38,40,41,45,46].
Educational experiences and motivation
Tailored and empathetic education to acquire meaningful knowledge:
Sufficient knowledge in the context of a patient’s chronic disease and disability was required for engaging in physical activity. Patients who were inactive commonly did not understand mechanisms and consequences of disease [34,38], non-surgical treatment options [34,38,40], and/or physical activity recommendations [34,40,45]. Confusion about what was considered physical activity hindered participation. For example, “I don’t know [if walking helps], that’s what we need to know” [34]. Due to confusion and lack of understanding, some patients felt there was nothing they could do, other than surgery, to treat their chronic disease, and did not consider physical activity a first line of treatment [34,38,40].
Across a majority of studies, participants valued empathetic and meaningful education that was tailored to unique personal factors [33,34,36–38,40,41,45,46]. Particularly valued were collaborative and empathetic providers who used personalized approaches to care. Tailored care providers were identified as acknowledging unique personal factors such as age, sex and cultural differences [35,36,39,41,42,45], education level and health literacy [34,38,40,41,46], and severity of disease and disability [37,40,45]. Tailored approaches to care also included unique personal narratives, such as “She was so nice, and she said, ‘let’s go, let’s go, you can’, because I never did exercise before and I thought I would never do it, and she always pushed me to doing it” [33]. In the absence of empathy and tailored education, patients did not retain education and were left feeling frustrated, angry, and helpless [37].
Motivation:
Motivation for physical activity was developed from participants’ expected or experienced benefits. One participant reported, “Just a hint that [physical activity] would make it better and I would make more of an effort” [34]. High-value expected benefits were typically needed to initiate physical activity [34–37,39,40,42,43,45], whereas experiencing benefits were needed to engage in continued physical activity [33,35–37,39,42,43,45].
Expected benefits of physical activity included prevention of complications [36,39], physiologic improvement of disease [34,40,42], improved body image [37,39], and optimizing ability to engage in meaningful life roles [35–37,39,43]. Although some participants reported specific physiologic benefits of physical activity in the setting of chronic disease [34], other participants perceived physical activity could prevent functional decline [35]. The experience of losing family members or friends to complications of chronic disease occasionally motivated physical activity participation [35,45].
Experiencing benefits of physical activity motivated people to continue physical activity. Experienced benefits included improved disease management [33,42,45], increased energy [37], enjoyment and sense of well-being [35,39,42,43], regaining or maintaining mobility [35,39,43,45], and positive body image [36,39,43]. The experience of physical activity benefit provided participants with a feeling of success and potential for continued success with persistent physical activity.
Although a foundation to physical activity, not all patients were motivated by knowledge. Some patients reported understanding of recommendations and known benefits, yet continued minimal physical activity participation [34,38,40,41,45,46]. Additionally, some participants did not appreciate a collaborative approach, valuing a directive approach of “experts” [35].
Support and self-efficacy to manage symptoms of disease
Support: a source of self-efficacy:
Participants largely endorsed the need for the support from others to engage in physical activity. Perceptions of support consistently emerged from positive interactions with medical providers, family, and others with similar difficulties. Medical provider supervision, follow-up phone calls, counseling, and encouragement enabled patients to overcome perceived barriers to physical activity [33,39–41,43]. Interactions with people who had similar difficulties (e.g., DM, amputation) provided opportunities to openly discuss challenges, fears, problem solve with non-family members, and allowed participants to “be with friends without judgement” [36,37,39,40,42,43,45]. Additionally, talking to people with similar experiences provided a sense of belonging to a group, which was a source of enhancing confidence in the ability to overcome the barriers to initiating and maintaining physical activity [34–37,39].
Family was an inconsistent form of support. For some, family was considered a source of encouragement and confidence for physical activity [36,39,41,43]. For others, family support was not discussed [39] or was thought of as a barrier to participating in physical activity [43]. Family members were most commonly considered barriers to physical activity when family members had low confidence in their loved one’s ability to successfully participate in meaningful physical activity [43].
Physical activity persistence requires self-efficacy:
Physical activity participation was commonly acknowledged as a difficult process [33,37,39], requiring persistence, problem solving, and confidence in the setting of challenge and failure. Participants were reassured when they acknowledged the process of improvement and recovery would be slow and difficult [34]. Challenges of physical activity were contextualized by descriptions of participating in physical activity alone [33,39,46], balancing life roles [36,41,45], managing health conditions and overcoming symptoms of disease [35–38,40], and finding time [34–37,41,42]. Participants commonly reported the need for specific skills to initiate and continue physical activity. For example, participants needed physical skills (e.g., table tennis, walking) [42,43] or non-physical skills (e.g., problem solving, time management, prioritizing) [36,39,42,43]. Additionally, goal attainment facilitated persistence and perceptions of control [39,42]. Finally, openness to engaging in new forms of physical activity was directly linked to self-efficacy for those with amputation [37,43].
Although patients desired physical activity and participation in meaningful life roles, feelings of helplessness, anger, frustration, and fear commonly precluded participation in physical activity [38,40]. Such low self-efficacy was consistently linked to limited physical activity for people with chronic disease and disability [33,38,40]. Primary symptoms of chronic disease that moderated physical activity participation included pain and fatigue [34,36–38,43,45,46]. Participants with low self-efficacy commonly reported high symptom severity and rarely participated in physical activity [34,36–38,40,41,43,45]. However, there were participants who perceived severe symptoms and continued to participate in physical activity despite extensive challenges. Furthermore, participants with amputation reported non-participation due to fear of falling or injury, or because of difficulties they experienced in public [37]. Falling or other negative experiences in the presence of low self-efficacy commonly resulted in additional barriers to physical activity [43].
Disability specific concerns after LLA: prosthesis, equipment, and the environment
Prosthesis fit and equipment are related to function and physical activity:
Specific prosthesis and physical function concerns were identified for those living with LLA. The fit of the prosthesis and how the prosthesis interfaces with the residual limb directly influenced the ability to participate in physical activity [37,43]. Fit of the socket due to fluctuating shape of the residual limb required readjustment for comfort over the course of the day. Furthermore, poor fit during prolonged activity increased the risk for pain or skin issues (e.g., blisters, ingrown hairs), preventing participation in physical activity [37]. Additionally, the use of specialized equipment in the presence of amputation was necessary for specific types of physical activity (e.g., hand cycle, specialized prostheses, sport wheelchairs). Specialized equipment provided an opportunity to continue previously enjoyed activities, or initiate new activities [43]. Physical impairments were broadly reported as barriers to physical activity. Common physical impairments included weakness, cardiovascular endurance, range of motion, muscular strength, and balance [35,37–39,43].
Disability and environmental factors related to physical activity:
Environmental factors consistently influenced physical activity for people living with chronic disease and disability. Neighborhood crime, greater travel distances, lack of transportation, limited facilities and poor weather (e.g., rain, heat, ice, snow) were reported as physical activity barriers [33,34,36,41,42,44,45]. More specifically, participants reported fear of crime and lack of enjoyment with poor weather, thus limiting their engagement in physical activity when these conditions were present [33,35,42,44]. Additionally, geographic features including excessive slopes, inadequate lighting, uneven surfaces, stairs, and street crossings hinder participation in physical activity, especially walking [34–36,43,44]. There were, however, individuals who would engage in physical activity despite environmental challenges. “Rain, hail, shine, winter, summer, you know, except if I’m on holiday somewhere. But then when we go on holidays, I walk there anyway, you know” [41].
Discussion
This qualitative meta-synthesis identified factors that may influence physical activity participation after dysvascular LLA. Participants characterized by LLA, older age, DM and/or PAD related three distinct themes to participating in physical activity: 1) educational experiences and motivation, 2) support and self-efficacy to manage symptoms of disease, and 3) special concerns after LLA. These findings advance our understanding of what factors may need to be targeted to improved physical activity after dysvascular LLA.
Our findings agree with prior literature that shows meaningful experiences with providers and clear understanding of their health condition is linked to greater motivation for physical activity participation. For example, a collaborative-care approach between patient and healthcare provider enhances positive emotional responses and motivation for self-management behaviors (e.g., diet, physical activity, medication management) [47,48]. Additionally, empathetic provider communication and patient understanding of provider education are predictive of self-management behavior for those living with DM [49]. It is important to test if collaborative-care approaches (e.g., motivational interviewing, cognitive behavioral therapy) improve physical activity following dysvascular LLA.
The relationship of self-efficacy and physical activity following dysvascular LLA is not surprising. Self-efficacy, or confidence in one’s ability to achieve a desired behavior, has long been established as a predictor of health and physical activity behavior [50,51]. Proposed sources of self-efficacy include personal and vicarious experiences, persuasion, and physiologic states [50,52]. Providers should act as sources of support, encouraging and persuading patients to experience personal success and physiologic benefits of physical activity (e.g., enjoyment, strength, function). Additionally, the support of non-family members can enhance self-efficacy for physical activity through vicarious experience and persuasion, especially when family members are not effectively supporting the patient. Following amputation, higher levels of goal pursuit and goal adaptability are related to greater positive affect, enhanced self-efficacy, and lower levels of disability [53,54]. Interventions targeting improved self-efficacy for people with dysvascular LLA should integrate strategies of optimizing the support of family, friends, and providers.
The special needs of those living with amputation of any etiology are well recognized. Rehabilitation recommendations have been developed to maximize physical function after amputation [5,55]. Such recommendations are focused on the physical limitations after amputation and prescription of a prosthesis in hopes of minimizing the effects of disability. Additionally, physical rehabilitation attempts to minimize negative influence of environmental barriers (e.g., stairs, ramps, uneven ground). Rehabilitation recommendations broadly acknowledge special considerations for those with dysvascular LLA (e.g., pre-existing medical conditions, advanced age, cognitive impairment), yet provide little guidance for how to address the psychosocial factors (e.g. understanding, motivation, self-efficacy) identified in this meta-synthesis. These meta-synthesis findings can be used as a starting point for research aimed at identifying mechanisms and targets that should be addressed through behavior-based interventions specifically for people with dysvascular LLA.
Behavior-based interventions effectively improve physical activity for those with DM and PAD without LLA [14,15]. Unfortunately, our analysis of qualitative studies suggests there are specialized needs (e.g. prosthetic equipment, severe disability) that are not addressed by existing behavior-based interventions. To improve physical activity after dysvascular LLA, our findings can be used to develop behavior-based interventions that can be integrated into accepted rehabilitation recommendations. For example, a rehabilitation therapist or prosthetist can use collaborative communication approaches enhance patient understanding of how to effectively use prosthetic components. This supportive approach to communication may not only enhance understanding but may increase self-efficacy and motivation for physical activity in the setting of LLA, DM, PAD, and older age, defining characteristics of dysvascular LLA. Conversely, there may be patients who do not appreciate a collaborative approach and may benefit from more directive or prescriptive approaches to rehabilitation. Future research is necessary to develop and test behavior-based interventions that can be implemented within clinical practice.
Our meta-synthesis across contexts of living with dysvascular LLA (e.g., LLA, older age, DM, PAD) is a strength, building upon the uniqueness of each study to develop a deeper understanding of the factors that may influence physical activity after dysvascular LLA. A broad search yielded exemplary studies with a large diversity of sex, ethnicity, and race. The analysis was conducted with an interdisciplinary research team, broadening the interpretive perspective on the results. However, the findings should be considered in the context of the study limitations. Although our search was extensive, we included studies published within the past 10 years and may not have identified or analyzed all relevant historical qualitative studies. Our appraisal of the qualitative studies highlighted variable rigor, namely in the clarity of analysis techniques used to obtain qualitative findings and strategies used to minimize bias. Although the rigor was variable, consistency of findings within and across studies was robust and should bolster confidence in the findings. Finally, although an interdisciplinary study team was used, the findings could be influenced by the professional backgrounds of the team (e.g., rehabilitation focus of a physical therapist, medical complexity of a nurse, prosthesis focus of a certified prosthesist orthotist).
Conclusions
Participation in physical activity after dysvascular LLA may be influenced by complex relationships among understanding, motivation, support, self-efficacy, and special concerns. Our findings suggest that interventions that address modifiable psychosocial factors and physical limitations may improve physical activity outcomes following dysvascular LLA.
Implications for Rehabilitation:
Physical activity participation after dysvascular lower limb amputation is complicated by the presence of chronic conditions, severe disability, and unaddressed psychosocial factors.
Addressing a patient’s self-efficacy, social support, motivation, and understanding during physically focused rehabilitation may improve participation in physical activity after dysvascular lower limb amputation.
Rehabilitation professionals can address self-efficacy, motivation, and understanding by using collaborative, empathetic communication strategies known to enhance a patient’s sense of support.
Acknowledgements/Funding:
Declaration of Interests: The authors report no conflicts of interest. This work was supported by the National Institutes of Health [NIH K12 HD055931] and the Foundation for Physical Therapy [Promotion of Doctoral Studies Scholarship].
Footnotes
Disclosure statement
This material is the result of work supported with resources and facilities of the VA Eastern Colorado Healthcare System. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
References:
- 1.Christiansen CL, Fields T, Lev G, Stephenson RO, Stevens-Lapsley JE. Functional outcomes after the prosthetic training phase of rehabilitation after dysvascular lower extremity amputation. PM R. 2015;7:1118–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paxton RJ, Murray AM, Stevens-Lapsley JE, Sherk KA, Christiansen CL. Physical activity, ambulation, and comorbidities in people with diabetes and lower-limb amputation. J Rehabil Res Dev. 2016;53:1069–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desveaux L, Goldstein RS, Mathur S, Hassan A, Devlin M, Pauley T, Brooks D. Physical Activity in Adults with Diabetes Following Prosthetic Rehabilitation. Can J Diabetes. 2016;40:336–341. [DOI] [PubMed] [Google Scholar]
- 4.Tudor-Locke C, Craig CL, Aoyagi Y, Bell RC, Croteau KA, De Bourdeaudhuij I, Ewald B, Gardner AW, Hatano Y, Lutes LD, et al. How many steps/day are enough? For older adults and special populations. Int J Behav Nutr Phys Act. 2011;8:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Rehabilitation of Individuals with Lower Limb Amputation Work Group. VA / DoD Clinical practice guidelines for rehabilitation of individuals with lower limb amputation Washington, DC: Department of Veterans Affairs & Department of Defense; 2017. [Google Scholar]
- 6.Dillingham TR, Pezzin LE, MacKenzie EJ. Incidence, acute care length of stay, and discharge to rehabilitation of traumatic amputee patients: an epidemiologic study. Arch Phys Med Rehabil. 1998. March;79:279–287. [DOI] [PubMed] [Google Scholar]
- 7.Varma P, Stineman MG, Dillingham TR. Epidemiology of limb loss. Phys Med Rehabil Clin N Am. 2014;25:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dillingham TR, Pezzin LE. Rehabilitation setting and associated mortality and medical stability among persons with amputations. Arch Phys Med Rehabil. 2008;89:1038–1045. [DOI] [PubMed] [Google Scholar]
- 9.Norvell DC, Turner AP, Williams RM, Hakimi KN, Czerniecki JM. Defining successful mobility after lower extremity amputation for complications of peripheral vascular disease and diabetes. J Vasc Surg. 2011;54:412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies B, Datta D. Mobility outcome following unilateral lower limb amputation. Prosthet Orthot Int. 2003;27:186–90. [DOI] [PubMed] [Google Scholar]
- 11.Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil. 2004. July;26:837–850. [DOI] [PubMed] [Google Scholar]
- 12.Dunn DS. Well-being following amputation: Salutary effects of positive meaning, optimism, and control. Rehabil Psychol. 1996;41:285–302. [Google Scholar]
- 13.Williamson GM, Schulz R, Bridges MW, Behan AM. Social and psychological factors in adjustment to limb amputation. J Soc Behav Personal. 1994;9:249–268. [Google Scholar]
- 14.McDermott MM, Guralnik JM, Criqui MH, Ferrucci L, Zhao L, Liu K, Domanchuk K, Spring B, Tian L, Kibbe M, et al. Home-based walking exercise in peripheral artery disease: 12-month follow-up of the goals randomized trial. J Am Heart Assoc. 2014;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Heal Psychol. 2009;28:690–701. [DOI] [PubMed] [Google Scholar]
- 16.Huebschmann AG, Crane LA, Belansky ES, Scarbro S, Marshall JA, Regensteiner JG. Fear of injury with physical activity is greater in adults with diabetes than in adults without diabetes. Diabetes Care. 2011;34:1717–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korkiakangas E, Taanila AM, Keinänen-Kiukaanniemi S, Keinanen-Kiukaanniemi S. Motivation to physical activity among adults with high risk of type 2 diabetes who participated in the Oulu substudy of the Finnish Diabetes Prevention Study. Heal Soc Care Community. 2011;19:15–22. [DOI] [PubMed] [Google Scholar]
- 18.Caldieraro-Bentley AJ, Andrews JO. An integrative review: Application of self-efficacy instruments for walking in populations with peripheral arterial disease. J Vasc Nurs. 2013;31:118–130. [DOI] [PubMed] [Google Scholar]
- 19.Jensen LA, Allen MN. Meta-synthesis of qualitative findings. Qual Heal Res. 1996;6:553–560. [Google Scholar]
- 20.VanderKaay S, Moll SE, Gewurtz RE, Jindal P, Loyola-Sanchez A, Packham TL, Lim CY. Qualitative research in rehabilitation science: opportunities, challenges, and future directions. Disabil Rehabil. 2018. March;40:705–713. [DOI] [PubMed] [Google Scholar]
- 21.Finlayson KW, Dixon A. Qualitative meta-synthesis: a guide for the novice. Nurse Res. 2008;15:59–71. [DOI] [PubMed] [Google Scholar]
- 22.Murray CD, Forshaw MJ. The experience of amputation and prosthesis use for adults: a metasynthesis. Disabil Rehabil. 2013. July;35:1133–1142. [DOI] [PubMed] [Google Scholar]
- 23.Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012. November;12:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones J, Nowels CT, Sudore R, Ahluwalia S, Bekelman DB. The future as a series of transitions: qualitative study of heart failure patients and their informal caregivers. J Gen Intern Med. 2015;30:176–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goins RT, Jones J, Schure M, Rosenberg DE, Phelan EA, Dodson S, Jones DL. Older Adults’ Perceptions of Mobility: A Metasynthesis of Qualitative Studies. Gerontologist. 2015;55:929–942. [DOI] [PubMed] [Google Scholar]
- 26.Schiller CJ. Critical realism in nursing: an emerging approach. Nurs Philos. 2016. April;17:88–102. [DOI] [PubMed] [Google Scholar]
- 27.Bondas T, Hall EOC. Challenges in approaching metasynthesis research. Qual Health Res. 2007. January;17:113–121. [DOI] [PubMed] [Google Scholar]
- 28.Dixon-Woods M, Booth A, Sutton AJ. Synthesizing qualitative research: a review of published reports. Qual Res. 2007. August 1;7:375–422. [Google Scholar]
- 29.Melendez-Torres GJ, Grant S, Bonell C. A systematic review and critical appraisal of qualitative metasynthetic practice in public health to develop a taxonomy of operations of reciprocal translation. Res Synth Methods. 2015. December;6:357–371. [DOI] [PubMed] [Google Scholar]
- 30.Creswell JW, Poth CN. Qualitative Inquiry & Research Design - Choosing Among Five Approaches. 4th ed. Thousand Oaks, California: SAGE Publications; 2018. [Google Scholar]
- 31.Messer LH, Johnson R, Driscoll KA, Jones J. Best friend or spy: a qualitative meta-synthesis on the impact of continuous glucose monitoring on life with Type 1 diabetes. Diabet Med. 2018. April;35:409–418. [DOI] [PubMed] [Google Scholar]
- 32.Law Letts S., Stewart M, Bosch D, Westmorland J, LW M. Guidelines for critical review form: Qualitative studies (Version 2.0). 2007;2017. Available from: https://srs-mcmaster.ca/wp-content/uploads/2015/05/Guidelines-for-Critical-Review-Form-Qualitative-Studies.pdf
- 33.Casey D, De Civita M, Dasgupta K. Understanding physical activity facilitators and barriers during and following a supervised exercise programme in Type 2 diabetes: a qualitative study. Diabet Med. 2010;27:79–84. [DOI] [PubMed] [Google Scholar]
- 34.Gorely T, Crank H, Humphreys L, Nawaz S, Tew GA. “Standing still in the street”: experiences, knowledge and beliefs of patients with intermittent claudication--a qualitative study. J Vasc Nurs. 2015;33:4–9. [DOI] [PubMed] [Google Scholar]
- 35.Hardy S, Grogan S. Preventing disability through exercise: investigating older adults’ influences and motivations to engage in physical activity. J Heal Psychol. 2009;14:1036–1046. [DOI] [PubMed] [Google Scholar]
- 36.Mier N, Medina AA, Ory MG. Mexican Americans with type 2 diabetes: perspectives on definitions, motivators, and programs of physical activity. Prev Chronic Dis. 2007;4:A24. [PMC free article] [PubMed] [Google Scholar]
- 37.Crawford DA, Hamilton TB, Dionne CP, Day JD. Barriers and Facilitators to Physical Activity Participation for Men with Transtibial Osteomyoplastic Amputation: A Thematic Analysis. J Prosthetics Orthot. 2016;28:165–172. [Google Scholar]
- 38.Cunningham MA, Swanson V, Pappas E, Ocarroll RE, Holdsworth RJ, O’Carroll RE, Holdsworth RJ. Illness beliefs and walking behavior after revascularization for intermittent claudication: a qualitative study. J Cardiopulm Rehabil Prev. 2014;34:195–201. [DOI] [PubMed] [Google Scholar]
- 39.Ferrand C, Perrin C, Nasarre S. Motives for regular physical activity in women and men: a qualitative study in French adults with type 2 diabetes, belonging to a patients’ association. Heal Soc Care Community. 2008;16:511–520. [DOI] [PubMed] [Google Scholar]
- 40.Galea Holmes MN, Weinman JA, Bearne LM. “You can’t walk with cramp!” A qualitative exploration of individuals’ beliefs and experiences of walking as treatment for intermittent claudication. J Heal Psychol. 2017;22:255–265. [DOI] [PubMed] [Google Scholar]
- 41.Gupta SS, Aroni R, Teede H. Experiences and perceptions of physical activity among South Asian and Anglo-Australians with type 2 diabetes or cardiovascular disease: Implications for clinical practice. Qual Heal Res. 2016;27:391–405. [DOI] [PubMed] [Google Scholar]
- 42.He W, Zhang Y, Zhao F. Factors influencing exercises in Chinese people with type 2 diabetes. Int Nurs Rev. 2013;60:494–500. [DOI] [PubMed] [Google Scholar]
- 43.Littman AJ, Bouldin ED, Haselkorn JK. This is your new normal: A qualitative study of barriers and facilitators to physical activity in Veterans with lower extremity loss. Disabil Heal J. 2017. [DOI] [PubMed] [Google Scholar]
- 44.Rosenberg DE, Huang DL, Simonovich SD, Belza B. Outdoor built environment barriers and facilitators to activity among midlife and older adults with mobility disabilities. Gerontologist. 2013;53:268–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Fam Pr. 2007;24:71–76. [DOI] [PubMed] [Google Scholar]
- 46.Peel E, Douglas M, Parry O, Lawton J. Type 2 diabetes and dog walking: patients’ longitudinal perspectives about implementing and sustaining physical activity. Br J Gen Pr. 2010;60:570–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Novak M, Costantini L, Schneider S, Beanlands H. Approaches to self-management in chronic illness. Semin Dial. 2013;26:188–194. [DOI] [PubMed] [Google Scholar]
- 48.Robertson SM, Stanley MA, Cully JA, Naik AD. Positive emotional health and diabetes care: concepts, measurement, and clinical implications. Psychosomatics. 2012;53:1–12. [DOI] [PubMed] [Google Scholar]
- 49.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bandura A Health promotion by social cognitive means. Heal Educ Behav. 2004;31:143–164. [DOI] [PubMed] [Google Scholar]
- 51.McAuley E, Konopack JF, Morris KS, Motl RW, Hu L, Doerksen SE, Rosengren K. Physical activity and functional limitations in older women: influence of self-efficacy. J Gerontol B Psychol Sci Soc Sci. 2006. September;61:P270–7. [DOI] [PubMed] [Google Scholar]
- 52.Bandura A Social cognitive theory. 1989:1–60. [DOI] [PubMed] [Google Scholar]
- 53.Coffey L, Gallagher P, Desmond D, Ryall N. Goal pursuit, goal adjustment, and affective well-being following lower limb amputation. Br J Heal Psychol. 2014;19:409–424. [DOI] [PubMed] [Google Scholar]
- 54.Coffey L, Gallagher P, Desmond D. Goal pursuit and goal adjustment as predictors of disability and quality of life among individuals with a lower limb amputation: a prospective study. Arch Phys Med Rehabil. 2014;95:244–252. [DOI] [PubMed] [Google Scholar]
- 55.Esquenazi A, DiGiacomo R. Rehabilitation after amputation. J Am Pod Med Assoc. 2001;91:13–22. [DOI] [PubMed] [Google Scholar]