Abstract
BACKGROUND
Meta-analyses and a recent guideline acknowledge that conservative management of uncomplicated appendicitis with antibiotics can be successful for patients who wish to avoid surgery. However, guidance as to specific management does not exist.
METHODS
PUBMED and EMBASE search of trials describing methods of conservative treatment was conducted according to Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines.
RESULTS
Thirty-four studies involving 2,944 antibiotic-treated participants were identified. The greatest experience with conservative treatment is in persons 5 to 50 years of age. In most trials, imaging was used to confirm localized appendicitis without evidence of abscess, phlegmon, or tumor. Antibiotics regimens were generally consistent with intra-abdominal infection treatment guidelines and used for a total of 7 to 10 days. Approaches ranged from 3-day hospitalization on parenteral agents to same-day hospital or ED discharge of stable patients with outpatient oral antibiotics. Minimum time allowed before response was evaluated varied from 8 to 72 hours. Although pain was a common criterion for nonresponse and appendectomy, analgesic regimens were poorly described. Trials differed in use of other response indicators, that is, white blood cell count, C-reactive protein, and reimaging. Diet ranged from restriction for 48 hours to as tolerated. Initial response rates were generally greater than 90% and most participants improved by 24 to 48 hours, with no related severe sepsis or deaths. In most studies, appendectomy was recommended for recurrence; however, in several, patients had antibiotic retreatment with success.
CONCLUSION
While further investigation of conservative treatment is ongoing, patients considering this approach should be advised and managed according to study methods and related guidelines to promote informed shared decision-making and optimize their chance of similar outcomes as described in published trials. Future studies that address biases associated with enrollment and response evaluation, employ best-practice pain control and antibiotic selection, better define cancer risk, and explore longer time thresholds for response, minimized diet restriction and hospital stays, and antibiotic re-treatment will further our understanding of the potential effectiveness of conservative management.
LEVEL OF EVIDENCE
Systematic review, level II.
KEY WORDS: Appendicitis, nonoperative, conservative, antibiotics, uncomplicated
Acute appendicitis is the most common reason for an emergency abdominal surgery, with a lifetime appendectomy risk of 12% for males and 23% for females.1 Although conservative (i.e., nonoperative) treatment of acute uncomplicated appendicitis with antibiotics has yet to be routinely recommended over appendectomy, and evidence gaps exist that are being addressed in ongoing trials, this management is becoming increasingly accepted as a reasonable option for patient shared decision-making. In a 2016 guideline, the World Society of Emergency Surgery concluded that antibiotic therapy can be successful in selected patients with uncomplicated appendicitis who wish to avoid surgery (level of evidence 1; grade of recommendation, A).2 A 2014 survey of Irish surgeons found that about one fifth routinely treat appendicitis nonoperatively.3 However, little clinical guidance exists for practitioners in terms of how nonoperative treatment is administered so they can best select and inform patients, and provide care to achieve similar efficacy and safety as established in published trials.
Since the mid-1990s, eight randomized controlled trials (RCTs) have investigated conservative antibiotic treatment in comparison with urgent appendectomy for acute uncomplicated appendicitis.4–11 In 2015, Salminen et al.9 reported by far the largest RCT, which involved 530 adults, and found fewer complications, 6% initial antibiotic nonresponse and 23% 1-year recurrence rates, and 12 fewer disability days compared with mostly open appendectomy. Meta-analyses that included this trial found conservative treatment associated with similar or fewer total complications as surgery and concluded that it can be offered to patients.12–17
We report results of a search of all published trials describing the methods of conservative treatment of acute uncomplicated appendicitis. This systematic review describes specific components of medical management that may affect outcomes including patient selection, imaging, antibiotics, pain and diet management, criteria for antibiotic nonresponse and appendectomy, disposition, and follow-up. We summarize the details of medical management, describe the range of approaches, critically evaluate this management in the context of applicable guidelines and related research, and identify areas of uncertainty.
PATIENTS AND METHODS
Data Sources and Searches
A literature search was conducted according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines using PUBMED (1966) and EMBASE (1947) databases for studies published in English and non-English languages through April 29, 2018, using the keywords (antibiotic or antibiotics or nonoperative or non operative or non-operative or conservative) and (appendicitis). References in the selected publications, including reviews, were searched for additional studies. Two reviewers (clinician and nonclinician) independently searched these databases, then reached consensus on potentially relevant publications, and evaluated candidate articles for final inclusion.
Study Selection and Criteria
Only full-text articles of trials that described initial conservative management of acute uncomplicated appendicitis were considered relevant. Studies with poorly characterized study populations were excluded. All study designs were allowed.
Data Extraction
Studies were included in data extraction if they reported methods of conservative management. Studies were categorized as follows: RCT; prospective, comparative; prospective, noncomparative; retrospective, noncomparative; and RCT comparing antibiotic treatment versus supportive care. The following information was extracted: number of participants that received conservative treatment, ages, patient selection including clinical and imaging criteria, antibiotic regimen, pain and diet management, criteria for initial antibiotic nonresponse, initial response rate, hospital discharge criteria, and follow-up. In some cases, authors were contacted for clarification.
RESULTS
Search Results
PUBMED and EMBASE identified 2,510 and 5,334 references, respectively, of which 192 were considered potentially relevant based on their title and 35 met selection criteria (Fig. 1, PRISMA diagram).4–11,18–44 One RCT was excluded because of subsequent retraction.44
Figure 1.
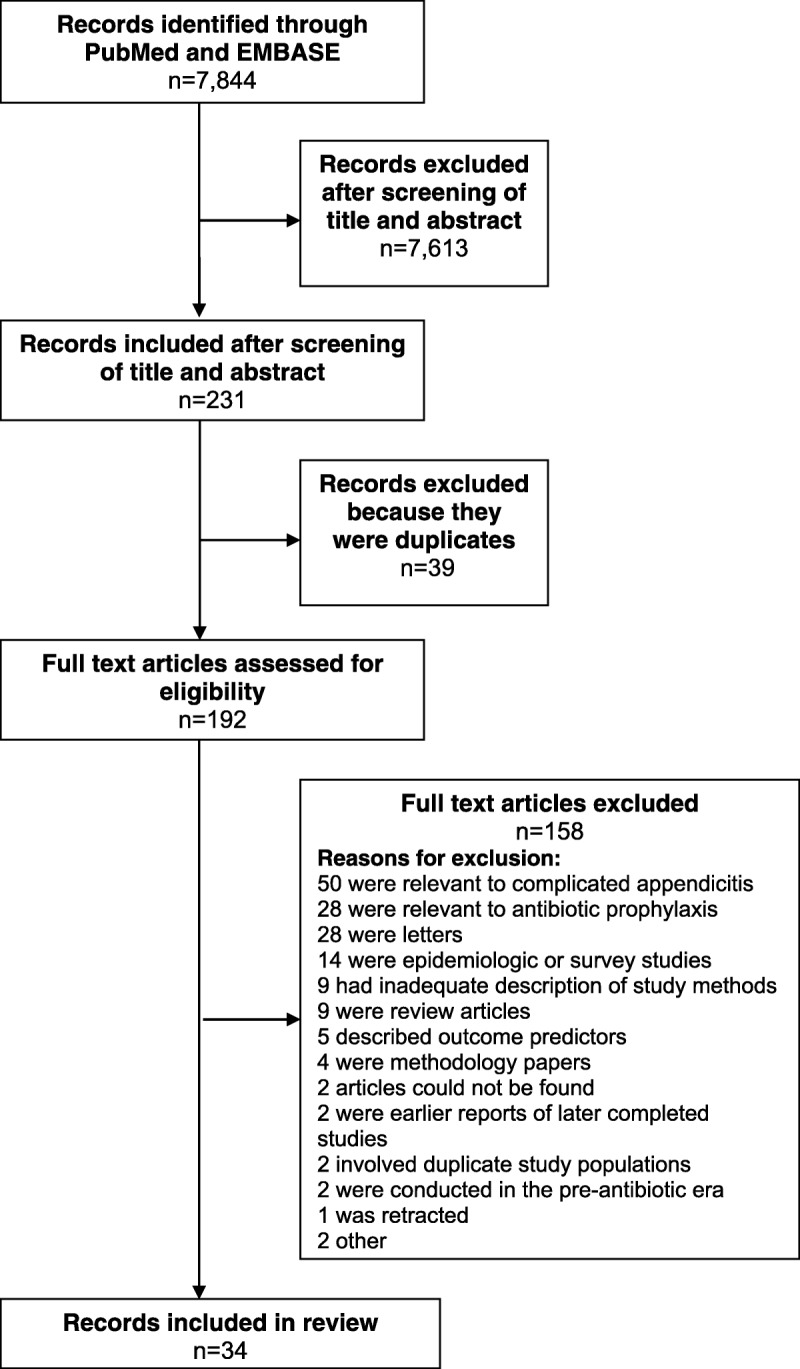
The PRISMA flowchart: selection of relevant studies.
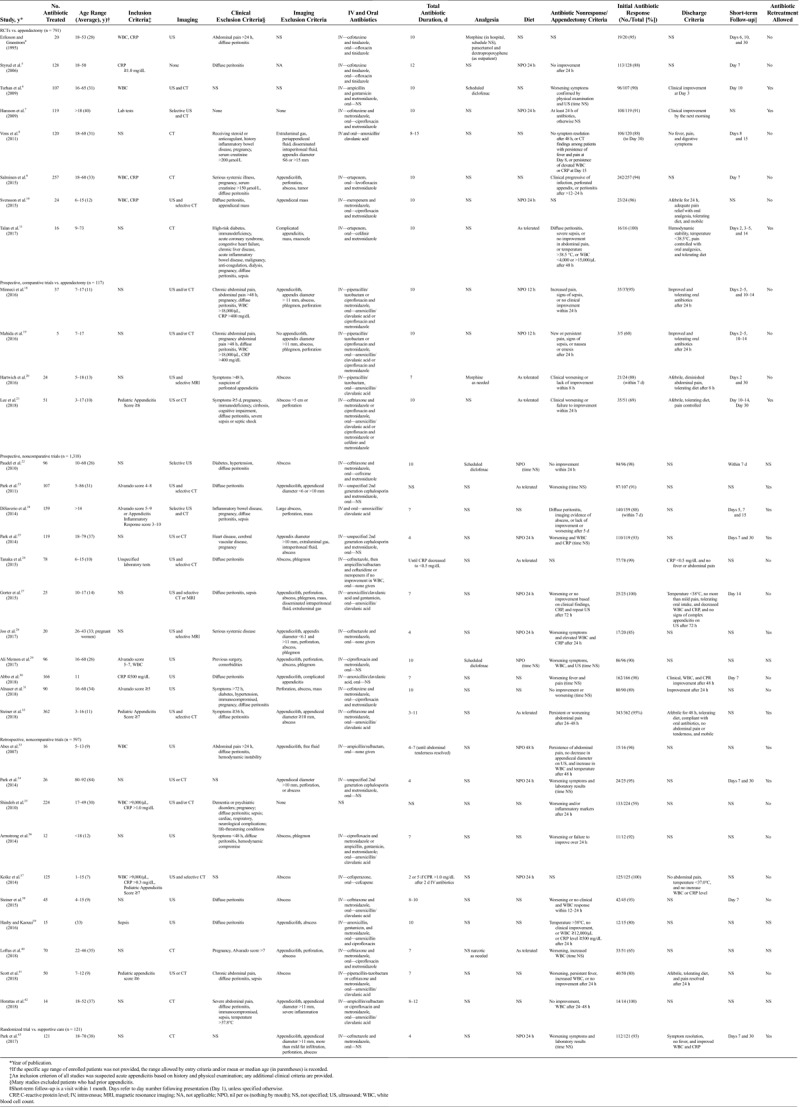
Table 1 summarizes all 34 studies of conservative antibiotic treatment identified and details of medical management provided to a total of 2,944 antibiotic-treated participants.4–11,18–43 Reports were mostly from Europe, Asia, and the United States but also from Nepal,22 Pakistan,29 and Iraq.31 These trials ranged in evidence grade from level II (RCT with negative criteria) to level V (case series) and included eight RCTs4–11 (number antibiotic-treated, 791), four prospective comparative (117),18–21 11 prospective noncomparative (1,318),22–32 10 retrospective noncomparative studies (597),33–42 and one randomized single-blind (patients only) trial comparing conservative antibiotic treatment to supportive care (121).43
TABLE 1.
Selection Criteria and Specific Management of Patients Receiving Conservative Antibiotic Treatment of Acute Uncomplicated Appendicitis in Published Studies
Patient Selection
Most published experience with conservative treatment is in healthy children and adults 5 to 50 years of age. There is only one RCT in children, which involved 24 antibiotic-treated participants.10 The largest pediatric experience is a prospective, noncomparative trial in 362 antibiotic-treated children aged 3 to 16 years.32 Few data are available on children younger than 5 years. Among pediatric trials with available data, the range of minimum ages of enrolled patients was 1 to 7 years and mean or median age was 9 to 14 years. Studies did not enroll many elderly. There is one prospective, noncomparative trial of 26 participants 80 years and older managed conservatively.34 Excluding this study, among adult trials with available data, the range of maximum ages was 60 to 79 years and mean or median age was 26 to 38 years.
Trials generally excluded patients with physical examination evidence of diffuse peritonitis, hemodynamic instability, or sepsis. The most common exclusion criterion was diffuse peritonitis by clinical examination or suggested by imaging, in 32 (94%) of 34 studies4,5,8–11,18–43 (not specified in one study).6 One RCT enrolled 369 unselected patients with appendicitis, which included 13 (3.5%) with diffuse peritonitis, and although there was crossover toward surgery, some participants were treated conservatively.7 Other common exclusion criteria were inflammatory bowel disease, pregnancy, and prior appendicitis. There is one prospective noncomparative trial of 20 pregnant women that reported outcomes in mothers similar to those observed among nonpregnant adults and no obstetrical or fetal complications.28
Imaging
Thirty-three (97%) of 34 trials used ultrasound or computed tomography (CT) imaging to evaluate the diagnosis of appendicitis and exclude findings of complicated appendicitis4,6–11,18–43; ultrasound was used exclusively in five pediatric trials,30,33,36–38 three adult trials,4,29,31 and one with children and adults.22 Twenty studies (59%) specifically excluded patients with any abscess,9,18–20,22,25–29,31,32,34,36–41,43 and three (9%) excluded patients with unspecified complicated appendicitis or mass.10,11,30 However, two (6%) included patients with a small abscess (i.e., <5 cm),21,33 and eight (24%) either did not specify (with exclusion in some based on a maximum appendiceal diameter)4–6,23,24,35,42 or included all patients with appendicitis while reporting subgroups.7 In one RCT of conservative treatment, among participants with a CT scan read as uncomplicated appendicitis, 18% of surgery-assigned patients had complicated appendicitis upon operation.8 Findings suggesting perforation were also common exclusion criteria, but these varied and included extraluminal gas, periappendiceal and intraperitoneal fluid (amount unspecified), and appendiceal diameter of greater than 11 mm. Appendicolith was an exclusion criterion in some studies9,18,23,27–30,32,33,39,40,42,43 and was associated with antibiotic nonresponse or recurrence in some trials8,19,21,35,37,41 and not in others.4–7,11,20,22,24–26,31,34,36,38 Imaging findings suggestive of tumor were exclusion criteria in some adult trials,8,9,11,24,31 with criteria either unspecified or based on an appendiceal diameter of greater than 15 mm.8 One trial compared conservative antibiotic treatment to supportive care and used more selective CT criteria (e.g., no more than mild fat infiltration).43 Some RCTs in adults did not use any imaging5 or used ultrasound selectively,7 with rates of unnecessary surgery as high as 11%.7
Antibiotics
Most antibiotic regimens were consistent with 2010 and 2017 Infectious Diseases Society of America (IDSA) and Surgical Infection Society (SIS) guidelines for treatment of mild-to-moderate community-acquired intra-abdominal infections.45,46 Initial parenteral antibiotic regimens used included a second- or third-generation cephalosporin (e.g., cefmetazole, cefotaxime, or ceftriaxone) plus metronidazole (or tinidazole) or single-agent regimens of amoxicillin-clavulanate (or ampicillin-sulbactam), piperacillin-tazobactam, or a carbapenem (ertapenem or meropenem). Oral (and alternative parenteral) regimens, started upon hospital discharge, included a fluoroquinolone or an advanced generation cephalosporin plus metronidazole, and amoxicillin-clavulanate. Four trials (12%) used intravenous and oral amoxicillin-clavulanate (or ampicillin-sulbactam),8,24,33,42 which are recommended against by IDSA and SIS guidelines. In three pediatric trials, ciprofloxacin was used.10,18,19 One pilot RCT allowed outpatient management facilitated by administration of long-acting ertapenem.11 Daily-dosed ceftriaxone and metronidazole have also been used.21,32,38,41 Conservatively managed patients have been shown to experience more, mostly mild, antibiotic-related side effects compared with appendectomy patients.11
Total intravenous and oral antibiotic duration ranged from 4 to 15 days. The most common total antibiotic duration was 10 days, which was used in 12 trials (35%)4,6,9–11,18,19,21,22,29,31,39; seven trials (21%) used 7 days.20,24,27,30,36,40,41 The shortest duration was 4 days, used in four trials (12%).25,28,34,43
Pain Control
Although worsening or persistent pain were criteria for antibiotic nonresponse leading to appendectomy, pain control regimens generally were not specified in published trials, with only six (18%) reporting analgesia4,6,20,22,29,40 and none describing extent of pain control. Three trials (9%) used a nonsteroidal anti-inflammatory drug (NSAID),6,22,29 diclofenac, as a scheduled regimen, two (6%) used morphine4,20 and one (3%) an unspecified narcotic40 as needed, and one (3%) used paracetamol and dextropropoxyphene for outpatients.4
Diet
Participants were prohibited oral intake 12 hours in two studies (6%),12,18 24 hours in nine studies (26%),5,7,10,25,27,28,34,37,43 and 48 hours in one study (3%),33 and allowed diet as tolerated in seven (21%; four pediatric and three adults trials)11,20,21,23,26,32,40; diet was unspecified in 15 studies (44%).4,6,8,9,22,24,29–31,35,36,38,39,41,42
Response to Treatment
Rates of initial clinical response during the index hospitalization were 88% or greater in 27 studies (79%)4–11,18,20,22–27,29–34,36–38,42,43 There were four (12%) outlier studies with rates in the 60% to 70% range.19,21,35,40 Among 2,944 antibiotic-treated patients, no related deaths or cases of progression to severe sepsis were reported.4–11,18–43
Trials differed regarding the time limit to demonstrate improvement before transition to appendectomy. Eight trials (24%) evaluated response within 24 hours,9,18–22,36,38 eight (24%) between 24 and 48 hours,5,7,28,32,35,39,41,42 and five (15%) after 48 to 72 hours,8,11,24,27,33 and in 13 (38%), this was unspecified.4,6,10,23,25,26,29–31,34,37,40,43 Studies also varied in the specific criteria for antibiotic nonresponse. Most trials indicated no improvement or worsening as criteria. Some trials further required concurrent increase in total white blood cell count or C-reactive protein levels, and/or abnormal findings on repeat imaging.
There is a paucity of data on time course of clinical response to antibiotics. In one adult trial, mean total white blood cell count decreased to normal within 1 day.4 One pediatric trial reported that the mean duration of fever in the antibiotic group was about 1 day.37 One adult trial described that appetite returned in 55% of participants by 18 hours and 98% by 24 hours.22 In one pilot RCT, individual participant responses were described over the first 24 hours of antibiotic treatment.11 Figure 2 shows Alvarado scores initially and after approximately 24 hours in 16 consecutive antibiotic-randomized patients; all initially received one dose of a long-acting antibiotic. The Alvarado score contains components that clinicians might use to follow the progress of an antibiotic-treated patient, that is, fever, nausea, tenderness, and leukocytosis.47 Most participants substantially improved over the first day. A few participants had lower scores that stayed constant over 1 day, but ultimately, their symptoms resolved. At 2 days, 3 to 5 days, 2 weeks, and 1 month, the proportion participants who were pain-free was 31%, 63%, 75%, and 88%, respectively.
Figure 2.
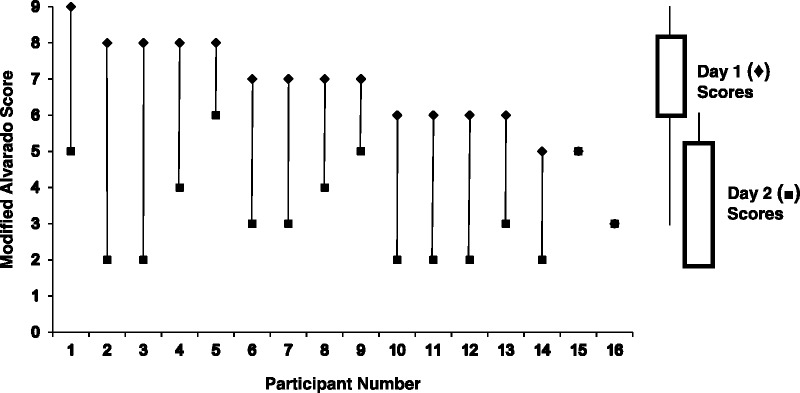
Modified Alvarado scores* at Day 1 and Day 2 for 16 participants with the diagnosis of acute uncomplicated appendicitis randomized to antibiotics-first treatment.11 *The modified Alvarado score consists of the following components (points): right lower quadrant tenderness (0/2); elevated temperature (≥37.3°C or 99.1°F) (0/1); rebound tenderness (0/1); anorexia (0/1); nausea or vomiting (0/1); leukocytosis level of greater than 10,000 cells/μL (0/2); polymorphonuclear cell count of greater than 75% (0/1). The modified score does not include migration of pain to the right lower quadrant since this variable would not be applicable for comparison of serial scores among a cohort of patients with imaging-confirmed appendicitis. The maximum modified Alvarado score is 9 instead of 10 for the original score. There was no change in score between Day 1 and Day 2 scores for patient numbers 15 and 16. Permission was obtained from Elsevier to reprint this figure, which is from Talan et al.11
We explored comparison of four (12%) outlier studies with initial antibiotic response rates in the 60% to 70% range19,21,35,40 to 30 trials (88%) with rates 80% or greater1–18,20,22–34,36–39,41–43 with regard to components of conservative management that might affect outcomes: inclusion of patients with abscess or unspecified, 50% versus 27%; inclusion of patients with appendicolith or unspecified, 75% versus 60%; use of a guideline nonrecommended intravenous and oral antibiotic or unspecified, 25% versus 17%; total antibiotic duration of less than 7 days or unspecified, 25% versus 23%; and allowed time for clinical response less than or equal to 24 hours or unspecified, 75% versus 62%, respectively.
Discharge Criteria and Short-term Follow-up
Seventeen trials (50%) described hospital discharge criteria.6–8,10,11,18–21,26,27,30–32,37,41,43 Studies generally required improvement, control of pain with oral analgesics, and some, resolution of fever. Most studies mandated that antibiotic-treated participants be hospitalized for a minimum 1 to 3 days. One pediatric pilot trial allowed hospital discharge if the participant was afebrile and tolerated a diet after 8 hours of treatment20 and one adult trial if there was improvement by the next morning.31 In one adult pilot RCT, 14 of 15 consecutive antibiotic-randomized adults achieved hemodynamic stability, temperature less than 38.5°C, pain control with oral analgesics, and tolerance for oral fluids and medications and were discharged from the emergency department; all were successfully managed as outpatients and had symptom resolution.11 These patients were initially treated with a long-acting parenteral antibiotic, analgesics and antiemetics as needed, and then observed for at least 6 hours before discharge. Among all studies, follow-up, when specified, occurred as a visit and/or by telephone or email, with contact usually within the first week and additional visits up to 30 days following hospital discharge.
Recurrence and Long-term Follow-up
In most studies, appendectomy was recommended for antibiotic-treated patients who initially had symptom resolution and experienced recurrence. Twelve trials (35%) allowed patients with recurrent appendicitis to be retreated with antibiotics, including among pregnant women.6,7,11,21,23–25,28,32–34,43 In the largest experience in adults, 14 of 22 participants with recurrence were retreated with antibiotics, and in the largest pediatric experience, 30 of 75 children, in all cases successfully.24,32 No study described a long-term follow-up strategy, such as with regard to possible missed appendiceal cancer.
DISCUSSION
The role of conservative antibiotic treatment for initial management of acute uncomplicated appendicitis is an area of continued controversy. Because of evidence gaps, it has not generally been concluded that antibiotic treatment should routinely replace surgery. These gaps include few data outside healthy young adults, limited comparison with laparoscopic surgery, and incomplete assessment of patient-related and long-term outcomes. Meta-analyses have found conservative treatment associated with similar or fewer complications overall compared with surgery,12–17 and a recent guideline now acknowledges that this management can be successful for selected patients who wish to avoid surgery and accept the possibility of recurrence.2 However, guidance does not exist to best advise patients and provide this care. This systematic review describes the patient selection criteria and range of medical treatments used in published trial methods of conservative antibiotic management of acute uncomplicated appendicitis. While RCT (level II; RCTs with some negative criteria) evidence of comparative effectiveness of conservative treatment in relation to urgent appendectomy exists, the full body of experience includes other prospective and retrospective, comparative and noncomparative trials. In total, our search found 34 studies describing 2,944 antibiotic-treated participants.4–11,18–42 For patients, this summary facilitates discussion about the extent to which their clinical profile is supported by trial experience and what they should expect should they choose nonoperative treatment. For providers, this review identifies common patterns of specific care components in order to guide their management.
Most trials of conservative treatment used ultrasound or CT imaging to evaluate the diagnosis of appendicitis and exclude patients with findings of or abscess. No consensus exists regarding definitions of complicated appendicitis and its complement and studies varied regarding specific criteria to distinguish these entities. For example, some studies excluded patients with any evidence of perforation or abscess. Others allowed small lesions (e.g., abscess <5 cm)21,35 consistent with a functional definition of uncomplicated appendicitis as appendicitis that would otherwise receive urgent appendectomy and complicated appendicitis as appendicitis accompanied by a major abscess or phlegmon that would preclude surgery (other than percutaneous drainage) or perforation with diffuse peritonitis that would require urgent operation. Both ultrasound and CT imaging correlate poorly with operative findings,48–50 with one RCT reporting 18% of surgery-randomized patients having complicated appendicitis at operation.8 However, since antibiotic treatment without surgery is a standard approach for treatment of appendicitis accompanied by major phlegmon or abscess because of a high success rate and avoidable ileocecectomy, this may not be an important distinction other than the expected response time and a potentially increased risk of occult malignancy. Some RCTs in adults did not use routine imaging,5,7 with an associated high rate of unnecessary surgery in one study.7 Patients diagnosed with uncomplicated appendicitis based only on clinical evaluation who do not respond to antibiotics must be considered to have other conditions such as complicated appendicitis, tumor, inflammatory bowel disease, or gynecological disorders.
Imaging-identified appendicolith was associated with antibiotic nonresponse in some studies8,19,21,35,37,41 and not in others.4–7,11,20,22,24–26,31,34,36,38 In all trials, clinicians who assessed response were not blinded to baseline findings. It is possible that knowledge of the recognized association of appendicolith with perforation may have biased subsequent evaluation and led to a false association with nonresponse. Lack of blinding of the clinicians evaluating antibiotic response to findings on presentation is a general limitation of past studies to allow identification of response predictors. Also, studies generally did not describe all qualifying patients and compare characteristics of those enrolled and not enrolled to identify potential selection biases. If patients with more mild illness tended to be enrolled, either generally or among subgroups perceived as high risk (e.g., those with appendicolith, leukocytosis, severe pain), as might occur with a nontraditional treatment approach, then response rates could be inflated and differences associated with certain findings obscured.
It has been suggested that increased use of imaging may be identifying appendicitis at an earlier stage than in the past, and also misidentifying nonappendicitis, leading to unnecessary care of what would otherwise be a self-resolving condition.51 One recent RCT reported comparable outcomes among participants treated with supportive care without antibiotics as with antibiotics.43 However, in this study, participants were selected as low-risk based on clinical and CT criteria (e.g., no more than mild fat infiltration), as well as their and their physician's willingness for enrollment, and accounted for only about 20% of all presenting patients with presumed appendicitis (whereas at operation, about 80% are nonperforated). Furthermore, there was no surgery control arm to confirm the existence and severity of appendicitis. Despite this one intriguing study, considering the recognized life-threatening complications of appendicitis in the presurgery/antibiotic era and absence of serious septic events reported in conservative treatment trials, if surgery is not performed, antibiotic treatment remains prudent.
Antibiotic treatment used in most trials was consistent with 2010 and 2017 IDSA and SIS guidelines for mild-to-moderate community-acquired intra-abdominal infections.45,46 These guidelines are based on clinical trials of antibiotics for patients with a range of intra-abdominal infections, including complicated appendicitis, and in vitro activity. One exception is that ampicillin-sulbactam and amoxicillin-clavulanic acid were used in four trials (12%)8,20,24,33,42 but are recommended against by guidelines because of high Escherichia coli resistance rates and inferior clinical outcomes in comparative trials. One RCT that used intravenous and oral amoxicillin-clavulanic acid could not demonstrate noninferiority of nonoperative treatment.8 Inadequate in vitro activity of these antibiotics was cited as a trial limitation.52 However, antibiotic response rates in trials using these drugs were high, 88% to 100%. Other trials used oral amoxicillin-clavulanic acid following improvement on a more broadly active intravenous antibiotic regimen.18–21,27,32,36,38,41
The most common total intravenous and oral antibiotic duration was 7 to 10 days. Four trials (12%) used only a 4-day duration.25,28,34,43 The Study to Optimize Peritoneal Infection Therapy trial demonstrated that antibiotic treatment for a median of 4 days (i.e., 2 days after symptom resolution) resulted in similar outcomes as treatment for a median of 8 days among patients with intra-abdominal infection.53 As opposed to conservative management of appendicitis, all patients in the Study to Optimize Peritoneal Infection Therapy trial had source control. However, among studies of nonoperative treatment of appendicitis, lower initial antibiotic response rates did not appear to be associated with shorter treatment duration, suggesting a shorter antibiotic course may be possible.
Guidelines do not recommend broad-spectrum regimens with activity against Pseudomonas aeruginosa and fluoroquinolone-resistant and extended-spectrum β-lactamase–producing bacteria for patients with mild-to-moderate community-acquired infections unless antimicrobial resistance risk factors exist, such as recent antimicrobial exposure, past infection with a resistant strain, or high prevalence of resistance in the patient's community or in recent areas of travel.45,46 Several trials used broad-spectrum regimens such as piperacillin-tazobactam or meropenem,10,18–20,41 which are discouraged by guidelines to promote antibiotic stewardship.
A major limitation of most past trials is absence of any specific pain control protocol or description of the extent to which pain control was achieved. Persistent or worsening symptoms were consistent criteria for transition to appendectomy, and inadequate analgesia could confound evaluation of antibiotic effectiveness. Related pain management research and guidelines may inform optimal care.54 For example, concern about masking findings of rupture during antibiotic treatment may cause providers to undertreat pain. However, it has been established that pain control for suspected appendicitis can be achieved safely, including with opiates if necessary, without adversely affecting diagnostic accuracy or obscuring findings of peritonitis.55 Preappendectomy NSAID administration has been demonstrated safe and opiate sparing.56 Multimodal analgesia, using acetaminophen, NSAIDs, and opiates,54 and scheduled as opposed to as needed administration, have been shown to optimize analgesia effectiveness.57 Therefore, a scheduled oral or parenteral NSAID, as was used in a few trials,6,22,29 and/or acetaminophen, and as needed opiates to control pain while treating with antibiotics can be expected to optimize pain control and limit unnecessary opiate use.
While diet approaches varied and included restricting intake to nothing by mouth 8 to 48 hours, early introduction of oral fluids and a diet as tolerated was used in about one third of trials in which this was specified,11,20,21,23,26,32,40 appears safe, and may promote comfort and earliest discharge.
The optimal time to allow for an antibiotic response is unknown. However, of 21 trials that specified response time threshold,5,7–9,11,18–22,24,27,28,32,33,35,36,38,39,41,42 38% allowed more than 24 to 48 hours5,7,28,32,35,39,41,42 and 24% more than 48 to 72 hours,8,11,24,27,33 with no related deaths or cases of progression to severe sepsis. Compared with patients with uncomplicated appendicitis, those with complicated appendicitis appear to take longer to respond to antibiotics. For example, in one series of 88 patients with perforated appendicitis complicated by abscess who were treated nonoperatively, mean time to resolution of fever and leukocytosis was approximately 3 days, and the success rate was greater than 95%.58 In the few trials that described time to response to conservative antibiotic treatment for patients with clinical- and imaging-diagnosed uncomplicated appendicitis, most participants responded within 1 to 2 days.4,11,22,37 Since both providers and patients need to know what to expect with conservative care, including atypical responses, additional initial response data from future trials would be helpful. Patients with perforation, not identified on CT, which may occur in about 20% and reflect the degree to which patients with more advanced disease are included,8 likely take longer to respond to antibiotics than those without perforation. This may contribute to the observation of a slightly higher rate of complicated appendicitis found at surgery among antibiotic nonresponders than surgery-randomized patients12 (and higher antibiotic nonresponse rates among those with conditions associated with complicated appendicitis, e.g., appendicolith) and supports allowing a longer antibiotic trial (i.e., 72 hours) in those uncommon patients who are slow to respond and who still wish to avoid surgery, with ongoing careful monitoring. Although there were only four studies with low initial antibiotic response rates, these more frequently allowed less than 24 hours for response and did not exclude patients with small appendiceal abscess or appendicolith.19,21,35,40 The relationship of serial laboratory and imaging findings to antibiotic responsiveness has yet to be determined.
Following symptom resolution, about 10% to 25% of medically treated patients experience recurrence over the next year.12–17 It appears that almost all recurrences happen in the first 2 years,59,60 In one report, among 710 antibiotic-treated patients, cumulative probability of recurrence was 0.09, 0.12, 0.12, and 0.13 at 1, 2, 3, and 5 years, respectively.59 Five-year follow-up of 256 antibiotic-assigned patients in the RCT by Salminen et al.60 revealed appendectomy rates of 0.27 (includes 6% initial nonresponse rate), 0.34, 0.35, 0.37, and 0.39, respectively. Salminen et al.60 reported that the complication rate associated with appendectomy in the antibiotic group was similar to that in the group randomized to initial surgery. The 5-year overall complication rate was significantly less in the antibiotic than the surgery group, 6.5% vs. 24.4%, respectively. In most trials, appendectomy was done for patients with recurrence. However, in about one third, participants were offered antibiotic retreatment, which had good success, although selection criteria for this approach were not described.6,7,11,21,23–25,28,32–34,43
Studies have not described long-term care. Older adults are greater risk of occult appendiceal malignancy (for all primary neoplasms, mean age is 55 years), which has been estimated to occur in 0.9% of patients based on histopathological review of 7,970 appendectomy specimens.61,62 Studies of conservative management excluded patients with suspicion of tumor on imaging. Salminen et al.60 found 4 (1.5%) of 272 surgery-assigned patients had an appendiceal tumor (3 neuroendocrine tumors, and one polyp); no appendiceal tumors were discovered over 5 years in the antibiotic group. The rate, tumor types, risk factors, and course of occult malignancy require further investigation in a much larger number of patients. Patients reevaluated for recurrent abdominal symptoms may have tumor detected on reimaging. For conservatively treated patients older than 40 years with complicated appendicitis who remain asymptomatic, selective reimaging and colonoscopy have been suggested.63 Although conservatively treated patients with uncomplicated appendicitis appear to be a less risk of occult malignancy than those with complicated appendicitis, this may also be a reasonable follow-up approach for patients with uncomplicated appendicitis after successful antibiotic treatment, with appendectomy preferred for recurrence.
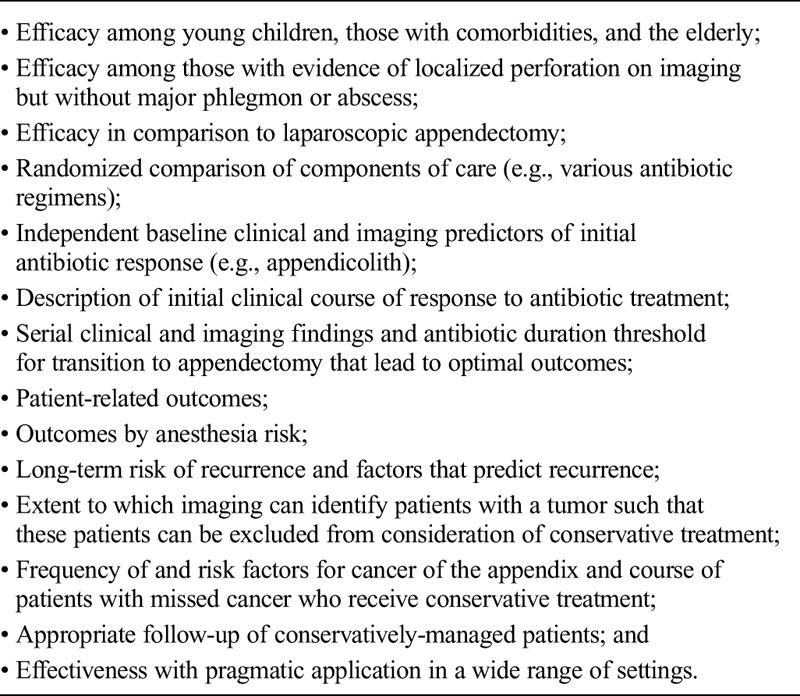
This systematic review has limitations. First, these were open trials in which enrollment and outcomes, such as antibiotic response, may have been influenced by provider and patient knowledge of and attitudes toward treatment assignments. Second, evidence gaps exist that preclude a full understanding of the comparative effectiveness of conservative treatment in relation to surgery so that shared decision-making can be well-informed. These areas of uncertainty are summarized in Table 2. Third, at the present state of investigation, conservative treatment is bundled, that is, antibiotics, pain and diet management, response criteria, and follow-up strategies have been compared together versus surgery; individual components of this care have yet to be subjected to randomized trials. However, in care of any complexity, many interventions are involved, and trials that may or may not attempt to control for various aspects of management still inform care. We can look for common approaches related to good outcomes in large numbers of patients to guide treatment as well as observed associations to generate hypotheses for future trials. Fourth, our search may not have identified all relevant trials, particularly non-RCTs since, to our knowledge, this is the first attempt to assemble all studies of conservative treatment. Fifth, over the approximately two-decade span of this research, comfort with conservative treatment has increased, and this review may not identify trends in care. For example, whereas requisite 3-day hospitalization was justified in the largest RCT to “ensure the safety of this unproved therapeutic modality,”64 emergency department discharge of stable patients has been demonstrated feasible11 and is now incorporated in the methods of a ongoing multicenter US trial (ClincalTrials.gov, NCT02800785). Avoided or shortened hospitalization could substantially reduce costs and inconvenience. One author who was contacted about a study's low initial response rate commented that it was done “in an era of aggressive (and sometimes) unnecessary surgery” (J. Shindoh, MD, PhD, May 2018, e-mail communication), and suspected success rates are currently higher.35 Finally, we also continue to learn more about possible functions of the appendix that may support or deem unnecessary its preservation, such as in cancer immunity65 and as a gastrointestinal microbiome reservoir.66
TABLE 2.
Areas of Uncertainty for Conservative Antibiotic Treatment of Acute Uncomplicated Appendicitis
This systematic review identifies patient populations most studied and common selection criteria and care methods, provides critical analysis in the context of applicable clinical guidelines and related research, and highlights areas of uncertainty so that patients can be best informed and managed should they consider this approach and researchers can better target unanswered questions about this care. Future studies that address biases associated with enrollment and response evaluation, use best-practice pain control and antibiotic selection, better define cancer risk, and explore longer time thresholds for response, minimized diet restriction and hospital stays, and antibiotic retreatment will further our understanding of the potential effectiveness of conservative management.
ACKNOWLEDGMENT
We thank Anusha Krishnadasan, PhD, for her assistance with the literature search and the many colleagues who have collaborated in the care and investigation of patients with appendicitis who have been treated with conservative antibiotic management.
AUTHORSHIP
D.A.T. conducted the literature search and drafted the article and tables. D.J.S., D.A.D., and G.J.M. reviewed and edited the article.
DISCLOSURE
The authors declare no conflicts of interest. All authors are faculty of the David Geffen School of Medicine at UCLA, Los Angeles, California.
Footnotes
Published online: December 4, 2018.
REFERENCES
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925. [DOI] [PubMed] [Google Scholar]
- 2.Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M, Sugrue M, De Moya M, et al. WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. 2016;11:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly ME, Khan A, Ur Rehman J, Waldron RM, Khan W, Barry K, Khan IZ. A national evaluation of the conservative management of uncomplicated acute appendicitis: how common is this and what are the issues? Dig Surg. 2015;32(5):325–330. [DOI] [PubMed] [Google Scholar]
- 4.Eriksson S, Granstrom L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82(2):166–169. [DOI] [PubMed] [Google Scholar]
- 5.Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, Rex L, Badume I, Granström L, et al. Appendectomy versus antibiotic treatment in acute appendicitis. A prospective multicenter randomized controlled trial. World J Surg. 2006;30(6):1033–1037. [DOI] [PubMed] [Google Scholar]
- 6.Turhan AN, Kapan S, Kutukcu E, Yiğitbaş H, Hatipoğlu S, Aygün E. Comparison of operative and non operative management of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2009;15(5):459–462. [PubMed] [Google Scholar]
- 7.Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473–481. [DOI] [PubMed] [Google Scholar]
- 8.Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, Karoui M, Alves A, Dousset B, Valleur P, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777):1573–1579. [DOI] [PubMed] [Google Scholar]
- 9.Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Tuominen R, Hurme S, Virtanen J, Mecklin JP, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340–2348. [DOI] [PubMed] [Google Scholar]
- 10.Svensson JF, Patkova B, Almström M, Naji H, Hall NJ, Eaton S, Pierro A, Wester T. Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children: a pilot randomized controlled trial. Ann Surg. 2015;261(1):67–71. [DOI] [PubMed] [Google Scholar]
- 11.Talan DA, Saltzman DJ, Mower WR, Krishnadasan A, Jude CM, Amii R, DeUgarte DA, Wu JX, Pathmarajah K, Morim A, et al. Antibiotics-first versus surgery for appendicitis: a US pilot randomized controlled trial allowing outpatient antibiotic management. Ann Emerg Med. 2017;70(1):1–11.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Findlay JM, Kafsi JE, Hammer C, Gilmour J, Gillies RS, Maynard ND. Nonoperative management of appendicitis in adults: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg. 2016;223(6):814–824.e2. [DOI] [PubMed] [Google Scholar]
- 13.Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, Agoritsas T, Heels-Ansdell D, Guyatt GH, Tikkinen KA. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rollins KE, Varadhan KK, Neal KR, Lobo DN. Antibiotics versus appendicectomy for the treatment of uncomplicated acute appendicitis: an updated meta-analysis of randomised controlled trials. World J Surg. 2016;40(10):2305–2318. [DOI] [PubMed] [Google Scholar]
- 15.Harnoss JC, Zelienka I, Probst P, Grummich K, Müller-Lantzsch C, Harnoss JM, Ulrich A, Büchler MW, Diener MK. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017;265(5):889–900. [DOI] [PubMed] [Google Scholar]
- 16.Sakran JV, Mylonas KS, Gryparis A, Stawicki SP, Burns CJ, Matar MM, Economopoulos KP. Operation versus antibiotics—the “appendicitis conundrum” continues: a meta-analysis. J Trauma Acute Care Surg. 2017;82(6):1129–1137. [DOI] [PubMed] [Google Scholar]
- 17.Podda M, Cillara N, Di Saverio S, Lai A, Feroci F, Luridiana G, Agresta F, Vettoretto N. ACOI (Italian Society of Hospital Surgeons) Study Group on Acute Appendicitis. Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15(5):303–314. [DOI] [PubMed] [Google Scholar]
- 18.Minneci PC, Mahida JB, Lodwick DL, Sulkowski JP, Nacion KM, Cooper JN, Ambeba EJ, Moss RL, Deans KJ. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg. 2016;151(5):408–415. [DOI] [PubMed] [Google Scholar]
- 19.Mahida JB, Lodwick DL, Nacion KM, Sulkowski JP, Leonhart KL, Cooper JN, Ambeba EJ, Deans KJ, Minneci PC. High failure rate of nonoperative management of acute appendicitis with an appendicolith in children. J Pediatr Surg. 2016;51(6):908–911. [DOI] [PubMed] [Google Scholar]
- 20.Hartwich J, Luks FI, Watson-Smith D, Kurkchubasche AG, Muratore CS, Wills HE, Tracy TF., Jr Nonoperative treatment of acute appendicitis in children: a feasibility study. J Pediatr Surg. 2016;51(1):111–116. [DOI] [PubMed] [Google Scholar]
- 21.Lee SL, Spence L, Mock K, Wu JX, Yan H, DeUgarte DA. Expanding the inclusion criteria for nonoperative management of uncomplicated appendicitis: outcomes and cost. J Pediatr Surg. 2017;S0022-3468(17):30636–X. [DOI] [PubMed] [Google Scholar]
- 22.Paudel GR, Agrawal CS, Agrawal S. Conservative treatment in acute appendicitis. JNMA J Nepal Med Assoc. 2010;50(180):295–299. [PubMed] [Google Scholar]
- 23.Park HC, Kim BS, Lee BH. Efficacy of short-term antibiotic therapy for consecutive patients with mild appendicitis. Am Surg. 2011;77(6):752–755. [PubMed] [Google Scholar]
- 24.Di Saverio S, Sibilio A, Giorgini E, Biscardi A, Villani S, Coccolini F, Smerieri N, Pisano M, Ansaloni L, Sartelli M, et al. The NOTA Study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260(1):109–117.24646528 [Google Scholar]
- 25.Park HC, Kim MJ, Lee BH. The outcome of antibiotic therapy for uncomplicated appendicitis with diameters ≤10 mm. Int J Surg. 2014;12(9):897–900. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Takazawa S, Deie K, Amano H. Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg. 2015;50(11):1893–1897. [DOI] [PubMed] [Google Scholar]
- 27.Gorter RR, van der Lee JH, Cense HA, Kneepkens CM, Wijnen MH, In 't Hof KH, Offringa M, Heij HA. APAC Study Group. Initial antibiotic treatment for acute simple appendicitis in children is safe: short-term results from a multicenter, prospective cohort study. Surgery. 2015;157(5):916–923. [DOI] [PubMed] [Google Scholar]
- 28.Joo JI, Park HC, Kim MJ, Lee BH. Outcomes of antibiotic therapy for uncomplicated appendicitis in pregnancy. Am J Med. 2017;130(12):1467–1469. [DOI] [PubMed] [Google Scholar]
- 29.Memon AG, Memon AI, Shah SKA, Sahito RA, Habib-ur-Rehman Leghari S, Baloch S. An experience of treatment outcome in acute appendicitis with antibiotics and appendectomy at a tertiary care hospital. Med Forum. 2017;28(3):136–140. [Google Scholar]
- 30.Abbo O, Trabanino C, Pinnagoda K, Ait Kaci A, Carfagna L, Mouttalib S, Combelles S, Vial J, Galinier P. Non-operative management for uncomplicated appendicitis: an option to consider. Eur J Pediatr Surg. 2018;28(1):18–21. [DOI] [PubMed] [Google Scholar]
- 31.Alnaser MKH, Hassan QA, Hindosh LN. Effectiveness of conservative management of uncomplicated appendicitis: a single hospital based prospective study. Int J Surg Open. 2018;10. [Google Scholar]
- 32.Steiner Z, Buklan G, Gutermacher M, Litmanovitz I, Landa T, Arnon S. Conservative antibiotic treatment for acute uncomplicated appendicitis is feasible. Pediatr Surg Int. 2018;34(3):283–288. [DOI] [PubMed] [Google Scholar]
- 33.Abes M, Petik B, Kazil S. Nonoperative treatment of acute appendicitis in children. J Pediatr Surg. 2007;42(8):1439–1442. [DOI] [PubMed] [Google Scholar]
- 34.Park HC, Kim MJ, Lee BH. Antibiotic therapy for appendicitis in patients aged ≥80 years. Am J Med. 2014;127(6):562–564. [DOI] [PubMed] [Google Scholar]
- 35.Shindoh J, Niwa H, Kawai K, Ohata K, Ishihara Y, Takabayashi N, Kobayashi R, Hiramatsu T. Predictive factors for negative outcomes in initial non-operative management of suspected appendicitis. J Gastrointest Surg. 2010;14(2):309–314. [DOI] [PubMed] [Google Scholar]
- 36.Armstrong J, Merritt N, Jones S, Scott L, Bütter A. Non-operative management of early, acute appendicitis in children: is it safe and effective? J Pediatr Surg. 2014;49(5):782–785. [DOI] [PubMed] [Google Scholar]
- 37.Koike Y, Uchida K, Matsushita K, Otake K, Nakazawa M, Inoue M, Kusunoki M, Tsukamoto Y. Intraluminal appendiceal fluid is a predictive factor for recurrent appendicitis after initial successful non-operative management of uncomplicated appendicitis in pediatric patients. J Pediatr Surg. 2014;49(7):1116–1121. [DOI] [PubMed] [Google Scholar]
- 38.Steiner Z, Buklan G, Stackievicz R, Gutermacher M, Erez I. A role for conservative antibiotic treatment in early appendicitis in children. J Pediatr Surg. 2015;50(9):1566–1568. [DOI] [PubMed] [Google Scholar]
- 39.Hasby S, Kaouui H. Place du traitement non opératoire dans les appendicitis aiguës. Ētude rétrospective chez 44 patients. J Afr Hépatol Gastroentéol. 2016;10:115–117. [Google Scholar]
- 40.Loftus TJ, Brakenridge SC, Croft CA, Smith RS, Efron PA, Moore FA, Brakenridge SC, Mohr AM, Jordan JR. A protocol for non-operative management of uncomplicated appendicitis. J Trauma Acute Care Surg. 2018;84(2):358–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott A, Lee SL, DeUgarte DA, Shew SB, Dunn JCY, Shekherdimian S. Nonoperative management of appendicitis. Clin Pediatr (Phila). 2018;57(2):200–204. [DOI] [PubMed] [Google Scholar]
- 42.Horattas MC, Horattas IK, Vasiliou EM. Early uncomplicated appendicitis—who can we treat nonoperatively? Am Surg. 2018;84(2):174–180. [PubMed] [Google Scholar]
- 43.Park HC, Kim MJ, Lee BH. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg. 2017;104(13):1785–1790. [DOI] [PubMed] [Google Scholar]
- 44.Malik AA, Bari SU. Conservative management of acute appendicitis. J Gatstrointest Surg. 2009;13:966–970. [DOI] [PubMed] [Google Scholar]
- 45.Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, O'Neill PJ, Chow AW, Dellinger EP, Eachempati SR, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis. 2010;50(2):133–164. [DOI] [PubMed] [Google Scholar]
- 46.Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, Chang PK, O'Neill PJ, Mollen KP, Huston JM, et al. The Surgical Infection Society revised guidelines on the management of intra-abdominal infection. Surg Infect (Larchmt). 2017;18(1):1–76. [DOI] [PubMed] [Google Scholar]
- 47.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557–564. [DOI] [PubMed] [Google Scholar]
- 48.Tulin-Silver S, Babb J, Pinkney L, Strubel N, Lala S, Milla SS, Tomita S, Fefferman NR. The challenging ultrasound diagnosis of perforated appendicitis in children: constellations of sonographic findings improve specificity. Pediatr Radiol. 2015;45(6):820–830. [DOI] [PubMed] [Google Scholar]
- 49.Gaskill CE, Simianu VV, Carnell J, Bhargava P, Flum DR, Davidson GH. Use of computed tomography to determine perforation in patients with acute appendicitis. Curr Probl Diagn Radiol. 2018;47(1):6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bixby SD, Lucey BC, Soto JA, Theysohn JM, Ozonoff A, Varghese JC. Perforated versus nonperforated acute appendicitis: accuracy of multidetector CT detection. Radiology. 2006;241(3):780–786. [DOI] [PubMed] [Google Scholar]
- 51.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mason RJ, Moazzez A, Sohn H, Katkhouda N. Meta-analysis of randomized trials comparing antibiotic therapy with appendectomy for acute uncomplicated (no abscess or phlegmon) appendicitis. Surg Infect (Larchmt). 2012;13(2):74–84. [DOI] [PubMed] [Google Scholar]
- 53.Sawyer RG, Claridge JA, Nathens AB, Rotstein OD, Duane TM, Evans HL, Cook CH, O'Neill PJ, Mazuski JE, Askari R, et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996–2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–157. [DOI] [PubMed] [Google Scholar]
- 55.Thomas SH, Silen W, Cheema F, Reisner A, Aman S, Goldstein JN, Kumar AM, Stair TO. Effects of morphine analgesia on diagnostic accuracy in emergency department patients with abdominal pain: a prospective, randomized trial. J Am Coll Surg. 2003;196(1):18–31. [DOI] [PubMed] [Google Scholar]
- 56.Jangjoo A, Bahar MM, Soltani E. Effect of preoperative rectal indomethacin on postoperative pain reduction after open appendectomy. J Opioid Manag. 2010;6(1):63–66. [DOI] [PubMed] [Google Scholar]
- 57.Bollinger AJ, Butler PD, Nies MS, Sietsema DL, Jones CB, Endres TJ. Is scheduled intravenous acetaminophen effective in the pain management protocol of geriatric hip fractures? Geriatr Orthop Surg Rehabil. 2015;6(3):202–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, Vargas H, Stamos MJ. Initial nonoperative management for periappendiceal abscess. Dis Colon Rectum. 2001;44(7):936–941. [DOI] [PubMed] [Google Scholar]
- 59.Lundholm K, Hansson-Assarsson J, Engström C, Iresjö BM. Long-term results following antibiotic treatment of acute appendicitis in adults. World J Surg. 2017;41(9):2245–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, Aarnio M, Rantanen T, Hurme S, Mecklin JP, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018;320(12):1259–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCusker ME, Coté TR, Clegg LX, Sobin LH. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer. 2002;94(12):3307–3312. [DOI] [PubMed] [Google Scholar]
- 62.Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41(1):75–80. [DOI] [PubMed] [Google Scholar]
- 63.Sakorafas GH, Sabanis D, Lappas C, Mastoraki A, Papanikolaou J, Siristatidis C, Smyrniotis V. Interval routine appendectomy following conservative treatment of acute appendicitis: is it really needed. World J Gastrointest Surg. 2012;4(4):83–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Paajanen H, Grönroos JM, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Dean K, Jartti A, Mecklin JP, et al. A prospective randomized controlled multicenter trial comparing antibiotic therapy with appendectomy in the treatment of uncomplicated acute appendicitis (APPAC trial). BMC Surg. 2013;13:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu SC, Chen WT, Muo CH, Ke TW, Fang CW, Sung FC. Association between appendectomy and subsequent colorectal cancer development: an Asian population study. PLoS One. 2015;10(2):e0118411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sanders NL, Bollinger RR, Lee R, Thomas S, Parker W. Appendectomy and Clostridium difficile colitis: Relationships revealed by clinical observations and immunology. World J Gastroenterol. 2013;19(34):5607–5614. [DOI] [PMC free article] [PubMed] [Google Scholar]


