Abstract
This article details perspectives from two individuals with type 1 diabetes (T1DM) who use continuous glucose monitoring (CGM) devices to improve their quality of life and self-management of diabetes. It provides a unique perspective of how CGM can make living with T1DM safer and easier, while improving the time spent in the target glucose range (time in range). The perspectives of these two individuals highlight both the immediate need for improved access and support for CGM as well as the need for an understanding of the benefits of using non-medically approved technologies.
Keywords: Continuous glucose monitoring, CGM, Type 1 diabetes
Perspectives from Two People with Diabetes
Anthony’s Story
I have been a lucky person with diabetes. My timing has been immaculate in that every time I reach a crisis point a solution will have just been invented.
When I was first diagnosed with diabetes in 1977, Dr Arnold Bloom’s book Diabetes Explained had just been published. The first chapter was “If you are aged under 40 you are Type 1 if you are over Type 2”; l was 39 and a half! My excellent general practitioner gave me the good advice “with this condition you have to be your own doctor.” In 4 years, I went through all type 2 diabetes drugs. Each worked for 4 or 5 months as I steadily shrank my intake of carbohydrates down to 40 g daily to keep my urine sticks pink before moving on to the next one. And, in 1981 I ended up on insulin.
My first bit of luck was that Boehringer Mannheim (BM) had just invented the BM blood glucose testing sticks, and as a patient at Guys and St Thomas’s I got them straight away. When I was diagnosed, my kids were 5 and 8 years old, respectively; the same ages that my sister and I were when our Dad died. I became quite obsessive that I would not leave my wife in the same situation as my mother and so hoovered up all the information I could about managing the condition and kept my glycated hemoglobin (HbA1c) level at 6.5% or under for the next 35 years; in retrospect by using my warning signs on a daily basis.
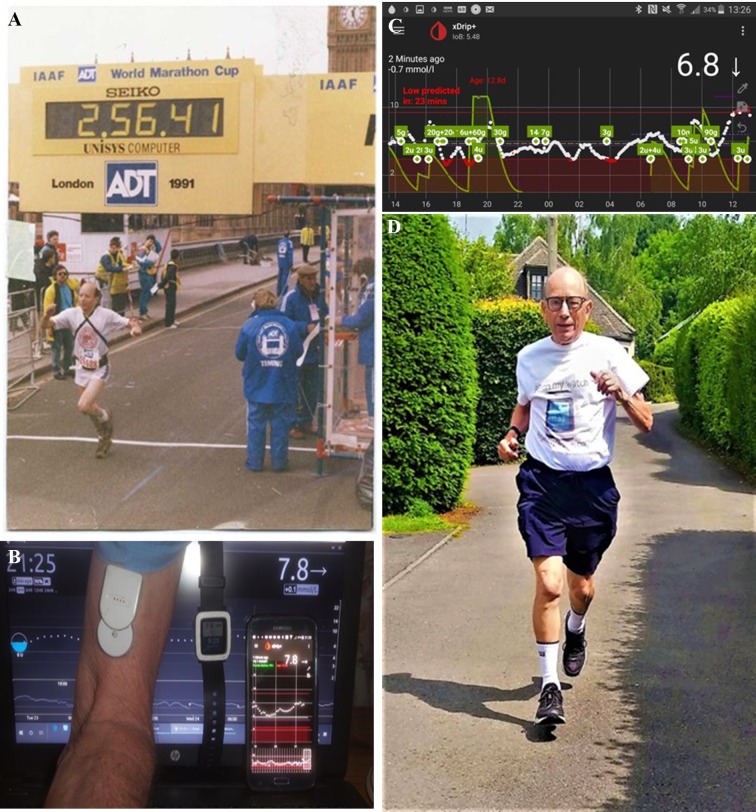
I had picked up early that exercise and diet were key, so I took up running and I eventually became quite a serious runner. One idea hatched up with Brian Hunter, the guy running the British branch of the International Diabetic Athletes Association, was to run a London Marathon quickly and claim it as a diabetic world record, thus getting publicity for the benefit of exercise in diabetes—although that was unlikely as I was 53, and the peak age for a marathon runner is early in the 30′s. We hoped it would get further claims and publicity round the world (the photo [Fig. 1a] shows the result). In the photo you can just see the BM sticks clutched in my left hand and the finger pricker in my right after a crisis and attack of cramp at 18 miles. Unfortunately, Brian had got fed up by the time the race was run, and the UK branch had folded.
Fig. 1.
a Anthony finishing the London marathon in under 3 h. His Boehringer Mannheim blood glucose testing sticks are clutched in his left hand. b The MiaoMiao transmitter overrides the Freestyle Libre sensor and transmits blood glucose data through Bluetooth to the xDrip+ app on the android smartphone, which in turn sends the reading on to the smartwatch, while the Nightscout app on a computer can be read worldwide via the internet. The main phone screen shows 3 h of readings, with 24 h of readings shown across the bottom. c Data on the xDrip+ application on a busy day in Anthony’s life demonstrating how continuous glucose monitoring (CGM) helps with decision-making and dosing adjustments to improve time in optimal glucose range while preventing hypoglycemia. d Running is still a routine activity in Anthony’s life, even after 41 years of living with type 1 diabetes and having reached 80 years of age. The use of CGM has helped Anthony immensely in performing exercise safely
In 2016, I finally realized that the two lumps of fat on my belly were lipohypertrophy, and I switched my injections to my thighs. Instantly I needed half the amount of insulin, down from about 60 Units per day to 30 Units. However, I was a bit slow to adjust to the smaller doses. One night I woke up from a deep dream at 3:00 a.m. to find myself staring into the face of an unshaven thuggish-looking individual; fortunately he was not a burglar trying to extort my debit card pin but, much worse, he was a paramedic. My poor wife had been forced to dial 999 for someone to get me out of a coma. Again, my luck was in, and Dr Google led me to the Dexcom G5 continuous glucose monitoring (CGM) system (Dexcom Inc., San Diego, CA, USA). Two months earlier Dexcom Inc. had taken over the distribution in the UK from their former agents and cut the price to only £3500 per annum!!
This is when I discovered the life-transforming effect of CGM. My favorite analogy is that I have been poking around in a darkened Amazon-type warehouse for 35 years with only the light from my fading phone battery to find the parcels. Then I pull a lever marked CGM, and the whole building is flooded with light, with every package on every shelf visible. I then discovered that spending £3500 per annum was not compulsory. First, the Dexcom sensors could be persuaded to run for 14 days instead of 7 days. Then when I bought the cheaper Flash Glucose monitoring sensor Freestyle Libre (Abbott Laboratories, Chicago, IL, USA), I could buy a transmitter to sit on top of it and connect to my phone which like the Dexcom G5 system would sound alarms. Then, what I thought was a vanity project, I added a watch and found that the ability to check my blood glucose with a glance at my wrist transformed my management yet again. Now wherever I am, out running in the rain, playing golf, shopping, there is no need to grope for my phone as the number is just there on my wrist.
CGM does not explain why on consecutive days the same routine has completely different results, but it exposes them and allows me to take control hour by hour. The greatest scandal for me is that people with type 1 diabetes (T1DM) generally have not been told about it. I have spent the last 6 months building a website http://www.bgonmywatch.com and trying to find a way to inform the 90% of people with T1DM who are unaware of their condition. The website explains about the five sensors currently available and how to obtain each one, and it acts as a primer in getting them up and running with all the necessary links. It seems extraordinary that the thousands of children with T1DM do not have this life-transforming system provided for them, enabling good control but especially relieving the strain on their parents, providing them with alarms at night and the possibility of monitoring their children from the next room or many miles away.
Last year Paul Coker, who has had T1DM for 40 years, ran 40 half-marathons in 1 year, which he followed up by organizing a world record for the most number of completed half-marathons by persons with T1DM in one race. He had the same idea that I had in 1991 of publicizing that exercise was beneficial for persons with T1DM. I saw this as an opportunity to publicize my website and meet a large number of fellow persons with diabetes (PwDs). In the end I got plenty of personal publicity as the oldest man in the race and with T1DM as well. In the Channel 4 documentary of the race I was the only featured runner other than category winners. But no one mentioned the website!
My diabetes is unpredictable. I invented the 16–8 diet. No carbs from 19:00 p.m. to 11:00 a.m. gave me some degree of control. CGM confirms the unpredictability but with alarms and the watch I see it in real time, I can react and am in charge.
Philippa’s Story
Imagine if I asked you to review a new film. You can choose to watch a video of the whole movie or see just three stills taken at random points. Which approach would you choose?
For me that’s the difference between using a CGM system and a standard blood glucose meter. Using a CGM I get to see the full story, in real time, with a trend arrow showing the direction that my glucose levels are heading. Compare this to a series of single numbers every couple of hours with a standard glucose meter.
I have lived with T1DM for 23 years and started using a CGM device 4 years ago. It ranks alongside structured education (Dose Adjusted Insulin For Normal Eating [DAFNE]) and using an insulin pump as major game changers in the management of my diabetes.
My CGM device is linked to my mobile phone and a smart watch. I can see my levels, at a glance, as often as I want throughout the day and night.
When I started using CGM, it proved I had no idea what was happening in the time between blood glucose checks. Seeing the CGM trace immediately changed how I bolused for meals. I hadn’t realized the chaos breakfast caused or the mismatch between meal absorption and insulin action later in the day. I now pre-bolus for breakfast, wait for the CGM graph to start dipping before eating, and use the bolus options on my insulin pump to better match insulin delivery to the food I’m eating.
The CGM trend arrows help me make better decisions. A meter just gives a single reading (5.5 mmol for example). That same reading on a CGM device with a → (straight arrow) is very different from one with ↗ (arrow sloping up) or ⇊ (double arrow down) which would require urgent action. These arrows also influence how I bolus for meals. If my levels are trending up I give more insulin than if they were heading down.
I keep an eye on my CGM device throughout the day but using the CGM alarms catches anything I miss. I set my low alert at a level at which I can treat a low before it actually happens and my high alert at a level at which I need to take action. Although the alarms can be annoying, especially at night, I console myself that it’s always better to know what’s happening. Every day with T1DM is different. My CGM data helps me spot patterns and trends, letting me adjust my insulin levels accordingly.
My CGM device and insulin pump are not linked, but they definitely complement each other. The CGM device shows me what’s happening, and my pump enables me to take action using small boluses and temporary bolus rates to nudge things back into my target glucose range. Together they have helped me increase the time I spend in my target range.
A lot of the time my CGM device just reassures me things are OK. Whether at work, in the gym or just shopping at the supermarket, it takes away that nagging feeling at the back of my mind.
A CGM device is expensive but I can’t imagine life without the information it gives. It just makes life with diabetes that bit more manageable and, surely, that has to be a good thing.
Physician Perspective
Anthony’s story demonstrates the recent advancements in T1DM care. His experiences, as well as those of Phillipa, highlight the benefits of real-time CGM (RT-CGM) in improving diabetes care. Key messages from both perspectives are improved diabetes self-management, flexibility and quality of life with RT-CGM.
Real-Time CGM
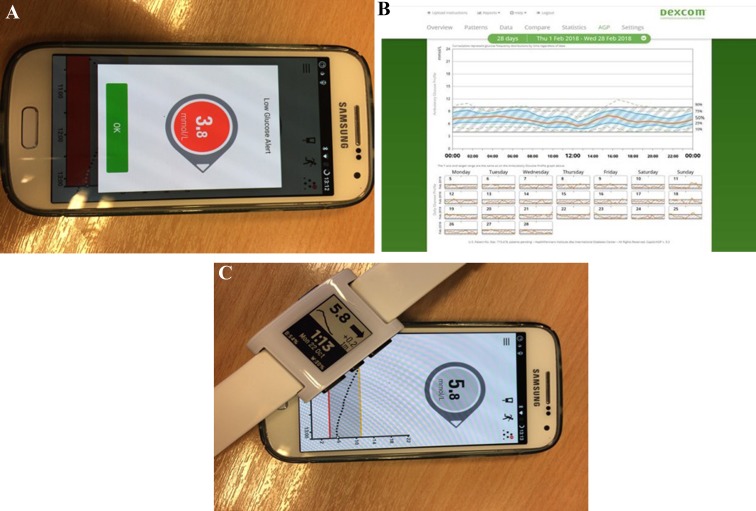
Real-time CGM offers users frequent glucose readings, trend arrows to show directionality and rate of change as well as customizable alarms and alerts (Fig. 2a, c). All of these can guide treatment decisions in a proactive manner to significantly improve time in the optimal glucose range and avoid hypoglycemia [1]. As shown in Figs. 1c and 2c, RT-CGM systems provide instant retrospective information on trends over last several hours. It can also produce more detailed reports, including data over several days, weeks or months, that help customize and adjust insulin therapy, as shown in Fig. 2b. The ease of access and review of retrospective data can greatly help self-management of diabetes and self-directed therapy adjustments. In the clinic, review of RT-CGM data helps healthcare professionals to make data-driven decisions on managing that patient’s diabetes, identifying areas of self-management that need to be improved, troubleshooting and planning ahead for special situations [2].
Fig. 2.
a CGM provides real-time alerts of hypoglycemia as well as predictive lows that are an important feature in avoiding and reducing hypoglycemic events for Philippa while maintaining excellent glycemic control and a busy lifestyle. b The Dexcom graph showing ambulatory blood glucose profile of a period of 28 days, which can help wearers of a CGM device like Philippa to understand trends and make adjustments to their own treatments. c Using smartphones as receivers for CGM and linking with other connectable and wearable devices, such as smartwatches, helps users such as Philippa in tracking and responding to glucose changes in busy situations
Flash (Intermittent) Glucose Monitoring
Flash or intermittent glucose monitoring is a cheaper alternative to RT-CGM [3]. This device uses a sensor that needs to be scanned by a separate reader to display glucose values, trends and a retrospective review of glucose. Limitations include the lack of real-time alerts and alarms coupled with lower accuracy, especially at lower glucose levels [3, 4]. Early experience highlights that flash CGM can be a good option for improving control and quality of life, but for those with hypoglycemia unawareness that has not improved with other treatments, real-time CGM remains the standard option for improving this challenging problem [5].
Adjunct Technologies
As shown in Fig. 1b, real-time remote sharing of data with carers or healthcare professionals using platforms such as Nightscout can be used to further support people with diabetes, including young children with T1DM [6]. It also opens up the potential of exporting data to smartwatches, apps and widgets available for smartphones (Figs. 1b, 2c). Non-medically approved adjunctive technologies, such as adaptations to flash CGM devices and third-party smartphone apps such xDrip+ as described in Anthony’s story, can provide a cost-effective approach to the PwD looking for features of RT-CGM and not meeting current funding criteria. While objective evaluations are needed and there may be limitations to the accuracy of such systems, healthcare professionals need to support their use given the potential benefits they can offer.
Evidence for RT-CGM
Over the last decade, RT-CGM systems have improved with respect to their ease of use and accuracy. While most trials have been performed using older systems, the results still provide strong support for using RT-CGM to improve diabetes management. RT-CGM significantly improves glycemic control with a reduction in HbA1c from 0.5 to 1.4% [7, 8]. As for constant subcutaneous insulin infusion therapy, the reduction in HbA1c is greater with a higher starting HbA1c [9]. In patients with HbA1C at the optimal target (< 7%), using RT-CGM significantly reduces the number of hypoglycemic events [10]. RT-CGM improves diabetes-specific quality of life measures, with users reporting increased hypoglycemic confidence, especially during sleep and driving, and reduced diabetes distress [11]. This and other benefits are evident in an analysis of patients’ narratives using RT-CGM [11].
The consensus from the literature, recent data, clinical and patient experience highlights that RT-CGM can improve time in range, with a reduction in hypoglycemic events and glycemic variability. RT-CGM makes diabetes management safer and easier, leading to significant improvement in quality of life, reduced anxiety and improved flexibility in adapting to 21st century living where shift-work, unpredictable activity and meals are a common scenario.
Funding and Commissioning
Despite its advantages, RT-CGM use in Europe remains low [12]. Funding and access are key issues in limiting the widespread use of RT-CGM devices. In England and Wales, the National Institute for Health and Care Excellence (NICE) recommends considering RT-CGM in limited settings relating mostly to impaired awareness of hypoglycemia or severe hypoglycemia [13]. However, there is no mandate for funding, and the majority of diabetes care facilities have no policy to allow those meeting NICE criteria to access funding [13]. Variations and disparities in accessing diabetes technologies and T1DM care are also evident in England and Wales [14, 15]. Given the immediate need to improve outcomes for T1DM care in England and Wales, improving access to technologies needs to be an important priority for the National Health Service [16]. Recent consensus of opinion in England suggests considering CGM options alongside continuous subcutaneous insulin infusion to improve glycemic control [17].
We are living in an exciting era for persons with T1DM, given the pace of development in technologies. Issues of access, device cost and funding need to be urgently improved to meet the needs for those living with T1DM.
Supporting Self-Management with RT-CGM
As illustrated in the two accounts presented here, there is a need for improved education to support RT-CGM users so that they can exploit features, such as dosing with trend arrows, and make use of non-medically approved adjunctive technological features. Thankfully, this progress is also coming from those directly living with T1DM, as demonstrated recently by the Nightscout project as well as Anthony’s own website [18]. Afterall #WeAreNotWaiting.
Acknowledgements
Funding
The authors are fully responsible for all content and editorial decisions and received no financial support or other form of compensation related to the development of this manuscript.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. The opinions expressed in the manuscript are those of the authors.
Disclosures
Isra Ahmed Mohamed, Anthony Fisher, Philippa Cooper and Sufyan Hussain have nothing to disclose.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors. Permission was granted from the people with diabetes discussed for use of their stories and figures in this article.
Peer Review
Please note, contrary to the journal’s standard single-blind peer review process, as a commentary this article underwent review by a member of the journal’s Editorial Board.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.7588838.
References
- 1.Beck RW, Riddlesworth T, Ruedy K, et al. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections: the DIAMOND randomized clinical trial. JAMA. 2017;317(4):371–378. doi: 10.1001/jama.2016.19975. [DOI] [PubMed] [Google Scholar]
- 2.Scheiner G. CGM retrospective data analysis. Diabetes Technol Ther. 2016;18(Suppl 2):S2-14–S2-22. doi: 10.1089/dia.2015.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilmot E, Leelarathna L. Flash forward: a review of flash glucose monitoring. Diabet Med. 2018;35:472–482. doi: 10.1111/dme.13584. [DOI] [PubMed] [Google Scholar]
- 4.Crabtree TSJ, Sathyapalan T, Wilmot E. FreeStyle Libre: available on the NHS? Br J Diabetes. 2018;18:3–6. doi: 10.15277/bjd.2018.168. [DOI] [Google Scholar]
- 5.Diabetes UK (2017). Diabetes UK consensus guideline for flash glucose monitoring. Available at: https://www.diabetes.org.uk/resources-s3/2017-09/1190_Flash%20glucose%20monitoring%20guideline_SB_V9%5B4%5D.pdf. Accessed 5 Jan 2019.
- 6.The Nightscout Foundation. The Nightscout project. Available from: http://www.nightscout.info. Accessed 25 Oct 2018.
- 7.Garg S, Zisser H, Schwartz S, Bailey T, Kaplan R, Ellis S, Jovanovic L. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor. Diabetes Care. 2006;29(1):44–50. doi: 10.2337/diacare.29.01.06.dc05-1686. [DOI] [PubMed] [Google Scholar]
- 8.Bailey TS, Zisser HC, Garg SK. Reduction in hemoglobin A1c with real-time continuous glucose monitoring: results from a 12-week observational study. Diabetes Technol Therap. 2007;9:203–210. doi: 10.1089/dia.2007.0205. [DOI] [PubMed] [Google Scholar]
- 9.Polonsky WH, Hessler D, Ruedy KJ, Beck RW. The impact of continuous glucose monitoring on markers of quality of life in adults with type 1 diabetes: further findings from the DIAMOND randomized clinical trial. Diabetes Care. 2017;40(6):736–741. doi: 10.2337/dc17-0133. [DOI] [PubMed] [Google Scholar]
- 10.JDRF Study Group Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359:1464–1476. doi: 10.1056/NEJMoa0805017. [DOI] [PubMed] [Google Scholar]
- 11.Pickup JC, Holloway MF, Samsi K. Real-time continuous glucose monitoring in type 1 diabetes: a qualitative framework analysis of patient narratives. Diabetes Care. 2015;38(4):544–550. doi: 10.2337/dc14-1855. [DOI] [PubMed] [Google Scholar]
- 12.Parkin CG, Holloway M, Truesdell J, Walker TC. Is continuous glucose monitoring underappreciated in the UK? Eur Endocrinol. 2017;13(2):76–80. doi: 10.17925/EE.2017.13.02.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institute for Health and Care Excellence (NICE). Type 1 diabetes in adults: diagnosis and management. NICE Guideline {NG17}. 2015. Available from: https://www.nice.org.uk/guidance/ng17. Accessed 25 Oct 2018. [PubMed]
- 14.NHS Digital (2018). National diabetes insulin pump audit (NDIPA) 2016–2017. England and Wales. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/insulin-pump-report-2016-17. Accessed 30 Oct 2018.
- 15.Perera R, Oliver N, Wilmot E, Marriott C. Variations in access to and reimbursement for continuous glucose monitoring systems for people living with Type 1 diabetes across England. Diabet Med. 2018;35(11):1617–1618. doi: 10.1111/dme.13766. [DOI] [PubMed] [Google Scholar]
- 16.NHS Digital (2017) National diabetes audit, 2016–2017, Report 1: care processes and treatment targets. England and Wales. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/national-diabetes-audit-report-1-care-processes-and-treatment-targets-2016-17. Accessed 30 Oct 2018.
- 17.Diabetes UK (2018). Type 1 diabetes technology: a consensus guidelines. Available at: https://www.diabetes.org.uk/resources-s3/2018-06/Diabetes%20UK%20consensus%20guideline.pdf. Accessed 30 Oct 2018.
- 18.Fisher A. BGONMYWATCH. Available at: www.bgonmywatch.com. Accessed 30 Oct 2018.