Abstract
Objectives:
The Government of Canada has proposed an ‘endgame’ target for cigarette smoking that aims to reduce prevalence below 5% by 2035. To meet this difficult goal, it will be necessary to identify populations where interventions will (1) have the greatest impact in reducing the number of smokers and (2) have the greatest impact in addressing smoking disparities.
Method(s):
Using data from the Canadian Community Health Survey, smoking prevalence was estimated for populations that differed with respect to demographic, substance use, and mental health factors. Risk difference, relative risk, and attributable disparity number, which describes the magnitude of the potential impact if the disparity were addressed, were calculated for each group.
Results:
The strongest disparities (relative risk ⩾ 2) were associated with immigration status (for women), substance use, marital status, and lifetime experience of mental health or substance use disorders. The smallest disparities (relative risk ⩽ 1.5) were associated with sexual orientation, household income, immigration status (men), and province of residence. The groups with the largest attributable disparity number were among those who used cannabis, and those who were not immigrants, not married, and white.
Conclusions:
Disparities which were both strong and had a large potential impact on prevalence overall were found for populations facing mental health and substance use concerns. Differences in rankings were found depending on the scale of the measure. Addressing disparities in smoking rates is an important component of developing tobacco endgame strategies.
Keywords: tobacco use, health status disparities, health policy
Introduction
Tobacco use has been a long-standing cause of preventable death in Canada, spurring public health efforts to encourage smokers to quit, to prevent young people from starting to smoke, and to curb marketing practices of tobacco companies.1 Progress towards the public health goal of reducing the burden of tobacco use is often evaluated by the change in the overall percentage of Canadians who smoke cigarettes on a daily or occasional basis. Focusing on changes in population-wide smoking prevalence rates can mask unequal progress among sub-populations and can deflect attention away from disparities in tobacco use that could exacerbate health inequalities. Smoking is a major risk factor for disease and is more frequently reported by those who are poor, are less well educated, are indigenous, or suffer from mental illness.1’4 Smoking itself is a major contributor to overall health inequalities with international studies (England, Wales, United States, Canada, and Poland) suggesting that it is tobacco use alone which contributes to more than half of the difference in adult male mortality between top and bottom social strata.5
Concerns about persistent inequalities in smoking have prompted calls for government to focus tobacco control efforts on those who are vulnerable, or who are disadvantaged by economic, social, or other circumstances.6 Some have recommended that the current population-level approach to reducing smoking be replaced with a ‘vulnerable population approach’.7
These recommendations come at the same time as others have called for an ‘endgame’ for tobacco use achieved by through new or more intensive interventions aimed at the general population.8 The Government of Canada has now proposed an endgame target of less than 5% smoking prevalence by 2035. This target requires millions of people currently smoking in Canada to quit, with substantial reductions in smoking among all groups. Furthermore, to meet this goal, it may be necessary to target interventions to populations in which interventions may have the largest impact. The potential conflict between the endgame and health equity goals has been identified as one which may exacerbate health inequalities.9
Several measures of health disparities have been presented in the literature. These have been categorized by Messer10 into relative measures of disparities including the rate ratio, index of disparity, relative concentration index, and Theil index, and absolute measures of disparity including the rate difference, between-group variance, and absolute concentration index.10–13 Other including Zhang et al14 had attempted measures that attempt to incorporate both absolute and relative differences such as the priority group index. The choice of disparity measure reflects differences in scale, as well as differences in the potential questions answered by the measure. Messer,10 for instance, suggests that the rate ratio for lung cancer disparities reflects ‘How much more lung cancer occurs in the least healthy group relative to the most healthy group?’, whereas the absolute risk difference reflects ‘How much higher is the lung cancer rate in the least healthy group compared with the rate in the most healthy group?’.10
There are many reasons to address health disparities and the primary reasons to do so are for reasons of social justice and equity. For the purposes, of a Tobacco Endgame an additional relevant question is what impact addressing the disparity has on reducing tobacco use overall. This may be best addressed using the risk difference or attributable risk which estimates the contribution of a risk factor to a disease.15 In this case, we are interested in the disparity itself as a risk factor and the impact that addressing the disparity would have on the absolute level of disease (or level of tobacco smoking in this case).
This article examines 2 questions: (1) in which populations is the difference in risk of smoking greatest (ie, the risk difference), (2) the strength of the gap between smoking prevalence the greatest (ie, the relative ratio or relative risk [RR]), and (3) in which populations would closing that gap have the biggest impact on reducing smoking overall (the absolute disparity number). That is, this study aims to quantify inequalities in tobacco use in Canada and to assess the contribution that closing them would make to achieving population-level reductions in tobacco use.
Methods
Data sources
Data were obtained from the Canadian Community Health Survey (CCHS), a cross-sectional population-based survey which excludes those living on reserves, full-time members of the Canadian Forces, and those living in institutions. All cycles of the survey use similar methodologies, and full information on their design can be found elsewhere.16 Estimates of the demographic and smoking status were primarily obtained from the 2013-2014 CCHS Public Use Microdata File (PUMF). The exceptions to this were data involving aboriginal ancestry and sexual identity, which were obtained from the CCHS Master File 2013-2014, and data involving mental health conditions and substance, which were obtained from the 2012 CCHS mental health survey PUMF. Confidence intervals (CIs) and coefficients of variations were calculated in accordance with the procedures outlined by Statistics Canada using the appropriate weighting applied. Item-level missing data were minimal and were excluded.
The 2013-2014 CCHS involved 128 310 respondents aged 12 years and over, with a 66.2% response rate; the 2012 CCHS Mental Health 2012 involved 25 113 respondents aged 15 and above with a 68.9% response rate down from 70% in 2011. For some questions (occupation, sexual orientation), a narrower age range was used in the survey design, and for some factors (education, marital status) a minimum age of 20 was imposed on the data used in this analysis.
Measures
Smoking behaviour
Cigarette smoking is defined by asking respondents ‘At the present time, do/does you/he or she smoke cigarettes daily, occasionally or not at all?’ Those who reported that they smoked on a daily or an occasional basis were considered smokers in this analysis, consistent with Health Canada’s current smoking indicator. The same set of questions about cigarette smoking was included in all surveys.
Demographic characteristics
All variables are self-reported. Sex is derived as male or female and only asked if the interviewer cannot make a determination. Sexual identity is ascertained through the question ‘Do you consider yourself to be: heterosexual, homosexual or bisexual?’. Race and culture are derived from a question ‘To which ethnic or cultural group did your ancestors belong?’ with responses grouped as ‘white’ and ‘visible minority’. Aboriginal ancestry was assessed by asking respondents if they were ‘an Aboriginal person, that is, First nations, Métis or Inuk (Inuit)? First Nations includes Status and Non-Status Indians’. Province of residence is also reported.
Socio-economic factors
Household income deciles are established by Statistics Canada at the national level to reflect the household income reported, the number of people in the household, and the size of the community. The highest level of education of each respondent is recorded under 1 of 4 categories: those who have not finished high school, those who have finished high school but have not studied further, those who have done some post-secondary studies but did not graduate from a post-secondary institution, and those who are post-secondary graduates. To exclude high school students in this analysis, we considered only those who were 20 years of age or older. Occupation is reported for those of working age (15-75 years), and this analysis employs 3 occupational groupings: Group 1 – ‘white-collar’ workers (management, natural and applied sciences, health, social sciences, education, religion, art, culture and recreation, business, finance, administration); Group 2 – ‘sales and service’ workers; and Group 3 – ‘blue-collar’ workers (trades, transport and equipment operator, occupations unique to primary industry, processing, manufacturing and utilities). The restrictions on the sample allow for the appropriate identification of the denominator for each group.
Family environment
Marital status, which was considered in this analysis only for those more than 20 years of age, is reported in 4 categories: married, living common law, formerly married (widowed, separated, divorced), or single. Homeownership is reported in 2 categories: whether the home is owned by the respondent or a member of the households and whether it is rented, even if no cash is paid.
Substance use and mental health
Variables which provide national estimates of cannabis use, alcohol dependency and abuse, and mental health disorders are only included in the 2012 CCHS Mental Health survey. Cannabis use is reported use on more than 1 occasion in their lifetime as well as in the past year. Lifetime and past year alcohol dependency and abuse uses the World Health Organization AUDIT measure (ever vs never). The 2013-2014 CCHS asked respondents whether they had ever been diagnosed with a mood disorder or an anxiety disorder.
Analysis
The strength of the smoking disparity was calculated as the RR of being a current smoking between the comparison group and the reference group (eg, the smoking prevalence of men divided by the smoking prevalence of women). For each population considered, the group with the lowest smoking prevalence was identified as a reference group, and the group with the highest smoking prevalence was identified as the comparison group.
The absolute disparity number, potential impact of eliminating the disparity, is derived from the calculation of attributable number. It represents the number of fewer smokers there would be in the comparison group if smoking prevalence were the same as in the reference group (eg, the number of fewer men who would smoke if the same percentage of men smoked as do women).
The absolute disparity number is calculated as
where Nc is the total population of the comparison group (ie, blue-collar workers), Pc is the proportion of people who smoke in the comparison group, and Pr is the proportion of people who smoke in the reference group (ie, white-collar workers). This is an equivalent value to the standard calculation of the attributable risk multiplied by the population size.17
This analysis assumes the existence of an intervention that would eliminate the disparity and presented the population size if it were standardized to the reference group level.
Results
Attributable risk
Differences in prevalence between the comparison populations are shown in Table 1. The largest attributable risks are for cannabis users (past year user Prevalence Difference (PD) = 28.6; 95% CI: 24.3, 32.9), lifetime mental health or substance use disorder (PD = 19.7; 95% CI: 10.8, 28.6), and aboriginal ancestry (PD = 16.5; 95% CI: 14.5, 18.5).
Table 1.
Number of smokers, smoking prevalence, risk difference of smoking, and absolute disparity number, during 2013 to 2014.
| Comparison group | Reference group | Number of smokers |
Smoking prevalence |
Prevalence difference |
Potential impact of eliminating disparity |
||
|---|---|---|---|---|---|---|---|
| Comparison group |
Reference group |
Comparison group |
Reference group |
||||
| C (n) | D (n) | E (%) | F (%) | E – F (%) | C – (total population of reference group × E) (n) | ||
| Demographic | |||||||
| Men | Women | 3 199 000 | 2 364 450 | 21.7 (± 0.7) | 15.7 (± 0.6) | 6.1 (± 0.9) | 892 800 (±135 041) |
| Gay or bisexual | Heterosexual | 186 000 | 4 219 700 | 33.6 (±4) | 22.5 (±0.6) | 5 (±2) | 61 500 (±22 687) |
| Non-immigrant men | Immigrant men | 2 468 700 | 618 000 | 22.8 (±1.8) | 18.1 (±0.7) | 4.7 (±1.9) | 509 600 (±208 226) |
| Non-immigrant women | Immigrant women | 2 066 200 | 233 000 | 18.8 (±2.4) | 6.4 (±0.3) | 12.4 (±2.4) | 1 360 800 (±302 097) |
| White | Visible minority | 4 671 200 | 975 300 | 21.2 (±0.5) | 14.1 (±0.8) | 7.2 (±0.9) | 1 575 700 (±207 428) |
| Aboriginal ancestry | Non-aboriginal ancestry | 389 000 | 4 870 200 | 34.3 (±1.9) | 17.9 (±0.4) | 16.5 (±2.0) | 191 300 (±22 999) |
| Not British Columbia | British Columbia | 4 959 400 | 604 100 | 19.2 (±0.5) | 15.3 (±1.1) | 3.9 (±1.0) | 1 015 500 (±323 728) |
| Socio-economic | |||||||
| Bottom 80% | Top 20% | 4 618 600 | 902 500 | 19.4 (±0.5) | 15.2 (±1) | 4.3 (±1.1) | 1 010 400 (±265 566) |
| Not a post-secondary graduate | Post-secondary graduate | 2 597 300 | 2 595 600 | 25.9 (±1.0) | 16 (±0.6) | 9.9 (±1.2) | 989 800 (±119 739) |
| Non white-collar | White-collar | 2 185 600 | 1 474 300 | 26.8 (±1.1) | 15.3 (±0.8) | 11.5 (±1.3) | 934 419 (±109 795) |
| Blue-collar | White-collar | 1 199 600 | 1 474 300 | 30.4 (±1.7) | 15.3 (±0.8) | 6.9(±2.3) | 593 500 (±73 759) |
| Sales/service | White-collar | 986 000 | 1 474 300 | 23.5 (±1.5) | 15.3 (±0.8) | 8.2 (±1.1) | 341 000 (±72 942) |
| Family environment | |||||||
| Not married | Married | 3 436 670 | 1 852 000 | 27.2 (±0.9) | 13.3 (±0.6) | 13.9 (±1.0) | 1 754 222 (±131 786) |
| Single | Married | 1 664 200 | 1 852 000 | 28.6 (±1.3) | 13.3 (±0.6) | 15.3 (±1.4) | 891 141 (±82 720) |
| Common law | Married | 927 200 | 1 852 000 | 29.0 (±1.9) | 13.3 (±0.6) | 15.7 (±2.4) | 501 630 (±62 964) |
| Divorced, separated, widowed | Married | 845 300 | 1 852 000 | 23.2 (±1.5) | 13.3 (±0.6) | 9.9 (±1.6) | 361 452 (±58 865) |
| Renter | Homeowner | 2 268 800 | 3 144 500 | 29 (±1.1) | 14.8 (±0.6) | 14.2 (±1.2) | 1 112 300 (±96 046) |
| Mental health and substance use | |||||||
| Used cannabis more than once | Used cannabis less than twice | 3 473 500 | 2 451 100 | 36.7 (±2.2) | 13.1 (±1.0) | 19.5 (±2.2) | 2 235 000 (±231 310) |
| Used cannabis more than once in the past 12 months | Used cannabis less than twice in the past 12 months | 1 575 300 | 4 348 700 | 48.7 (±4.3) | 17.4 (±0.9) | 28.6 (±4.3) | 1 011 400 (±142 108) |
| Alcohol abuse or dependence in lifetime | No alcohol abuse or dependence in lifetime | 1 910 600 | 3 946 800 | 37.8 (±3.3) | 17.2 (±1.0) | 5.5 (±3.3) | 1 039 000 (±176 641) |
| Mental health or substance use disorder in lifetime | No mental health or substance use disorder in lifetime | 2 941 900 | 2 855 700 | 32.3 (±2.5) | 15.5 (±1.2) | 19.7 (±8.9) | 1 530 800 (±249 408) |
| Diagnosis of mood disorder | No diagnosis of mood disorder | 768 600 | 4 785 700 | 33.6 (±2.2) | 17.4 (±0.5) | 16.2(±2.2) | 370 300 (±50 898) |
| Diagnosis of anxiety disorder | No diagnosis of anxiety disorder | 695 300 | 4 857 400 | 34 (±2.7) | 17.5 (±0.5) | 16.4(±2.7) | 336 300 (±55 391) |
Values in parenthesis are 95% confidence intervals.
For each of the groups identified, there were differences in smoking prevalence.
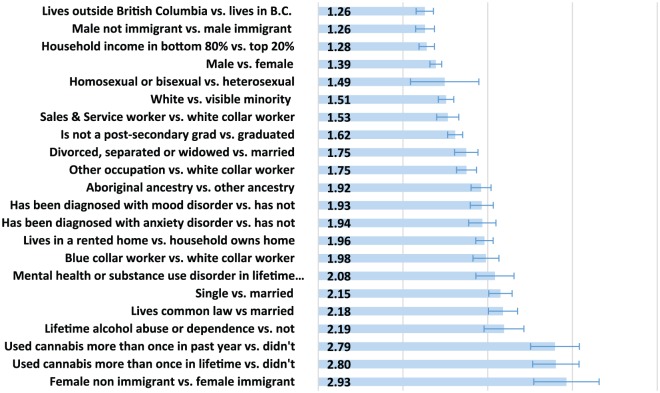
Relative risk
Among the group reviewed, the smallest intensity of disparity was a 26% higher RR of being a current smoker (RR = 1.26; 95% CI: 1.25, 1.27) which was associated with living in a province other than British Columbia. The largest RR of 2.93 (95% CI: 2.55, 3.31) was associated with being a non-immigrant woman. Additional populations associated with at least a 2-fold higher risk of smoking included having experienced a substance use or mental health disorder in one’s lifetime, being formerly married (divorced, separated, or widowed), having experienced alcohol dependence, having used cannabis more than once, and being a non-immigrant woman. Groups associated with 50% to 100% higher risk than the reference were being in poor mental health, being white (and not a visible minority), being aboriginal (and not white or another visible minority), working in a sales and service or blue-collar occupation instead of a white-collar job, not having graduated from college or university, and living in a rental home instead of a home owned by a family member. Additional populations associated with an RR of less than 1.5 were household income, being a man, being homosexual or bisexual, and being a non-immigrant man. Results are shown in Table 1 and Figure 1.
Figure 1.
Relative risk of smoking disparities, shown as relative risk of being a current smoker, during 2013 to 2014 (95% confidence interval is shown).
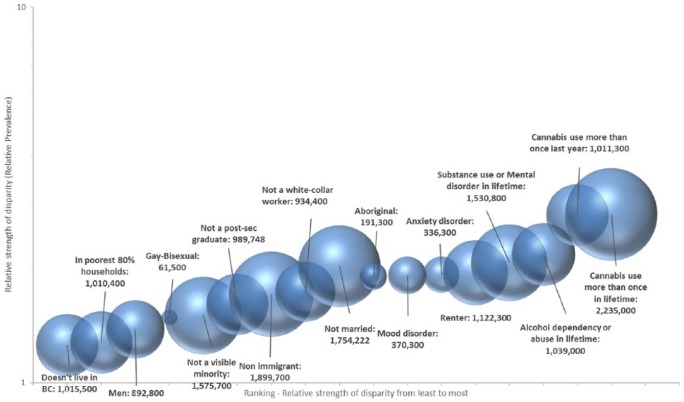
Attributable disparity number
The populations which were associated with the largest number of additional smokers associated with a disparity were the use of cannabis on more than 1 occasion in one’s lifetime or in the previous 12 months, not being an immigrant, not being married, being white, having experienced a mental health or substance use disorder in one’s lifetime, having a household income below the top 20%, living in rental housing, having been dependent on alcohol or abused alcohol in one’s lifetime, and living in a province other than British Columbia. For each of these populations, the impact of smoking disparities was greater than 1 million people, equal to one- to two-fifths of the 5.56 million smokers identified by the survey. Results are shown in Table 1 and Figure 2. The attributable disparity number was highly sensitive to the number of people in the population.
Figure 2.
Strength and potential impact of smoking disparities, from 2013 to 2014.
BC, British Columbia.
Smoking disparities were ranked from the lowest to highest. The size of bubble and number refer to potential impact on the number of smokers by eliminating the disparity.
Discussion
Disparities in cigarette smoking represent a major concern for tobacco control. This article found that disparities which were both strong and had a large potential impact on prevalence overall were found for populations facing mental health and substance use concerns. One-half of Canadian smokers have experienced mental health or substance use disorders in their lifetime. If those facing such challenges were no more likely to smoke than those who are not, there would be 1.5 million fewer smokers in Canada, and the nation’s overall smoking rate would fall to 13.5%.
In populations where the strength of the disparity is high, even if the overall potential impact on the overall number of smokers is low, a high percentage of the sub-population may be harmed by the consequences of tobacco use, and this may contribute to health inequalities already present in those populations. In cases where the potential impact of closing the gap of the disparity is high, even if the strength of the disparity is low, the impact may be felt on the overall health status of Canadians.
The attributable fraction has historically received less attention than measures of relative proportion, but each is important in addressing different research questions and highlight different aspects of disparity.18 Previous measures of disparities have assessed both relative and absolute measures of disparities, but not directly the attributable number.10,15 Existing, similar measures such as measurements of between-group variance and the absolute concentration index rely on the calculation of the overall population mean, do not assess the impact addressing the population-specific disparity directly, and are meant to assess the contribution towards the total disparity rather than the absolute impact of the disparity.10 This difference is important for programming and policies’ purposes and further investigations into understanding the causes of those disparities.
Some disparities in tobacco use align with well-accepted contributors to social and economic disadvantage, some do not. Higher smoking rates were found, as expected, among those with lower household incomes, with less education, and with mental health and substance use challenges. In other cases, populations which are not conventionally viewed as being disadvantaged (including men, ‘white’ people, non-immigrants) were found to have higher smoking rates than their counterparts (women, visible minorities, immigrants). Cigarette smoking may therefore exacerbate health inequalities in some populations and may mitigate them in others.
Reducing disparities for other large sub-populations could similarly contribute to a significant reduction in the number of Canadian smokers. Closing the gap between those who are married and those who are not, for example, would affect 1.75 million Canadians over the age of 20 and would bring Canada’s smoking prevalence below 13%. Bringing cigarette smoking among cannabis users down to the level of non-users would drop the national smoking prevalence rate down to 11% with 2.2 million fewer smokers.
For smaller sub-populations, the benefits of reducing disparities would bring important benefits to individuals and their communities, although the impact on overall use in Canada might be modest. Closing the disparity gap experienced by those with aboriginal ancestry who live off-reserve, for example, would improve the health of almost 200 000 indigenous people, but it would reduce the overall Canadian smoking rate by less than 1 percentage point. If those who have been diagnosed with a mood disorder such as depression were no more likely to smoke than those who have not, more than a third of a million Canadians would benefit, but overall prevalence would still be more than 17%.
Limitations
Limitations in the methods used hinder comparison of the intensity or magnitude of disparities between different factors. The survey populations were not identical, as not all of the variables used the same age range. The age range included also includes some people who might in the future graduate from college or university, potentially misclassifying this group. The CCHS does not survey all Canadians, including indigenous people living on reserve and the institutionalized, and therefore underestimates some populations important to equity issues. The groupings are not mutually exclusive, as individuals defined by one factor will also be defined by other factors: this is illustrated by the hypothetical examples of an immigrant woman (a low prevalence group) who is also a renter (a higher prevalence group), or a recent cannabis user (a very high prevalence group) who is also married (a low prevalence group).
Importantly, this analysis does not assume any causal associations between the groups and smoking, but does assume the existence of an intervention that would be able to eliminate the disparity. That is, we do not consider the groups causal to smoking, but groups that may be targets for policy and programming. As such, there may be significant intersectionality within the group that may contribute or explain differences. The impact of any proposed intervention should be assessed for its potential effect to reduce (or exacerbate) disparities in smoking. Furthermore, it should be noted that interventions aimed at reducing social inequalities may or may not reduce smoking depending on the causal mechanism of the intervention.
Conclusions
Tobacco control strategies which reduce smoking disparities will contribute to narrowing health inequalities and also to reducing the overall burden of tobacco use in Canada. The wide range of socio-economic, mental health, occupational, family, lifestyle, and demographic factors associated with such inequalities suggests that a correspondingly diverse research, policy, and programme response is warranted. The populations for whom smoking disparity is the strongest and for whom reducing that disparity would have the greatest impact would be those with mental health and substance abuse issues.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: MC and CC collaboratively conceptualized, conducted the analysis, drafted and edited the manuscript.
References
- 1. Reid JL, Hammond D, Driezen P. Socio-economic status and smoking in Canada, 1999-2006: has there been any progress on disparities in tobacco use? Can J Public Health. 2010;101:73–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Canadian Institutes for Health Information. Trends in income-related health inequalities in Canada. https://secure.cihi.ca/free_products/trends_in_income_related_inequalities_in_canada_2015_en.pdf?_ga=2.196620008.596881966.1552286917-247049801.1552286917. Technical report. Published July 2016.
- 3. Reid JL, Hammond D, Rynard VL, Burkhalter R. Tobacco Use in Canada: Patterns and Trends. Waterloo, ON, Canada: Propel Centre for Population Health Impact, University of Waterloo; 2015. [Google Scholar]
- 4. Kelly-Scott K, Smith K. Aboriginal peoples: fact sheet for Canada. Statistics Canada. https://www150.statcan.gc.ca/n1/en/catalogue/89-656-X. Up-dated November 3, 2015. [Google Scholar]
- 5. Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet. 2006;368:367–370. [DOI] [PubMed] [Google Scholar]
- 6. Health Disparities Task Group of the Federal/Provincial/Territorial Advisory Committee on Population Health and Health Security. Reducing health disparities – roles of the health sector. http://nccdh.ca/resources/entry/reducing-health-disparities. Discussion paper. Published 2005.
- 7. Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98:216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chaiton M, Schwartz R. Reducing the burden of tobacco: what’s the endgame? Isr J Health Policy Res. 2014;3:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gostin L. Tobacco endgame: the poverty conundrum. Hastings Cent Rep. 2014;44:10–11. [DOI] [PubMed] [Google Scholar]
- 10. Messer LC. Invited commentary: measuring social disparities in health – what was the question again? Am J Epidemiol. 2008;167:900–904. [DOI] [PubMed] [Google Scholar]
- 11. Kakwani N, Wagstaff A, van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econom. 1997;77:87–103. [Google Scholar]
- 12. Theil H. Economics and Information Theory. Amsterdam, The Netherlands: North-Holland; 1967. [Google Scholar]
- 13. Macintyre S, McKay L, Der G, Hiscock R. Socio-economic position and health: what you observed depends on how you measure it. J Public Health Med. 2003;25:288–294. [DOI] [PubMed] [Google Scholar]
- 14. Zhang B, Cohen JE, O’Connor S. The priority group index: a proposed new method incorporating high risk and population burden to identify target populations for public health interventions. J Public Health Manag Pract. 2014;20:E1–E11. [DOI] [PubMed] [Google Scholar]
- 15. Harper S, Lynch J. Methods for Measuring Cancer Disparities: Using Data Relevant to Healthy People 2010 Cancer-Related Objectives. Washington, DC: National Cancer Institute; 2006. [Google Scholar]
- 16. Statistics Canada. Canadian Community Health Survey Annual Component (CCHS). http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226. Accessed August 2016.
- 17. Dictionary of Epidemiology. Oxford Reference. doi: 10.1093/acref/9780199976720.001.0001. Accessed January 28, 2019. [DOI] [Google Scholar]
- 18. Nakayama T, Zaman M, Tanaka H. Reporting of attributable and relative risks, 1966-97. Lancet. 1998;351:1179. [DOI] [PubMed] [Google Scholar]