Abstract
Background
Through-knee amputation is a common amputation level after battlefield injuries during the medical evacuation process. However, there are limited data comparing through-knee amputation with transfemoral amputation as a definitive amputation level in terms of gait parameters.
Questions/purposes
(1) Does through-knee amputation result in improved gait velocity when compared with matched transfemoral amputees? (2) Do through-knee amputees have a faster gait cadence than matched transfemoral amputees? (3) Do through-knee amputees have a different stride length or stride width than matched transfemoral amputees? (4) Does through-knee amputation result in decreased work of ambulation when compared with matched transfemoral amputees?
Methods
Between January 2008 and December 2012, six male active-duty military patients who had undergone unilateral through-knee amputations as a result of trauma underwent gait studies at our institution. Of those, four of six underwent gait analysis after being able to walk for at least 3 months without assistive devices, and this group was studied here. Most through-knee amputees who were not included had elective revisions of their amputations from through-knee to a transfemoral amputation before completing 3-month gait data. Each of the amputees studied was matched to a transfemoral amputee based on height, body mass index, and contralateral amputation level resulting in a case-control study of active-duty military male amputee patients. Inclusion required complete gait data collected while walking at a self-selected pace wearing custom prosthetic devices. The through-knee amputees had a median (range) age of 32 years (23-41 years) and the transfemoral amputees had a median age of 24 years (22-27 years). Three-dimensional gait data were collected and analyzed. A power analysis found that to detect a clinically important difference (set at a change in work of ambulation of 1 J/kg*m) with a p value of 0.05 and a β set to 0.2, a study population of 56 patients per group would be required; that being said, our results on a much smaller population must be considered exploratory.
Results
With the numbers available, we found no differences in gait velocity when comparing through-knee (1.18 m/sec) and matched transfemoral amputees (1.20 m/sec, difference of medians = 0.02 m/sec; p = 0.964). Likewise, we found no differences in gait cadence when comparing through-knee with transfemoral amputees (104 versus 106 steps/min, respectively, difference of means 2 steps/min, p = 0.971). There was no difference in stride length or stride width when comparing through-knee (70 cm and 18 cm, respectively) with transfemoral amputees (70 cm and 19 cm, respectively; p = 0.948 and p = 0.440). With the numbers available, we did not identify a difference in the work of ambulation for through-knee amputees when compared with matched transfemoral amputees (8.3 versus 7.5 J/kg, respectively; p = 0.396).
Conclusions
Based on our findings, we are unable to demonstrate any functional advantages of knee disarticulation over transfemoral amputation. Although there are theoretical advantages for maintaining an intact femur during the medical evacuation and serial débridement process, we question the utility of knee disarticulation as a definitive amputation level; however, larger numbers of patients are needed to confirm these results.
Level of Evidence:
Level III, therapeutic study.
Introduction
The current conflicts in Afghanistan and Iraq have resulted in 1660 major amputations (defined as proximal to the carpus in the upper extremity or proximal to the ankle in the lower extremity) as of January 31, 2015 [6]. Over 75% of them have been lower extremity amputations [15]. Orthopaedic surgeons treating these patients frequently face the decision of whether to perform through-knee amputation or transfemoral amputation on young, previously healthy service members when a below-knee amputation is not feasible as a result of the extent of the initial injury.
However, medical and rehabilitative outcomes data comparing the two amputation types are sparse. Pinzur et al. [12-14] reported that patients who had through-knee amputations for peripheral vascular disease had higher walking velocity and lower energy cost of ambulation compared with transfemoral amputees. The Lower Extremity Assessment Project (LEAP) Study found that through-knee amputees had worse Sickness Impact Profile scores than transfemoral and below-knee amputees; however, nearly all of these amputations were performed through the zone of injury [4, 7, 16]. Bennett et al. [3] found no difference in SF-36 physical component scores or mental component scores, ability to walk 500 m, prosthetic use, or reported residual limb pain between transfemoral and through-knee amputees. A recent meta-analysis of lower extremity amputations after trauma found that patients with through-knee amputations had higher SF-36 physical component scores and were more likely to be able to walk 500 m; however, they wore their prostheses less and had more pain than transfemoral amputees [8].
In this retrospective, paired, matched-sample study, the gait parameters of four combat-wounded service members with through-knee amputations and contralateral transtibial amputations ambulating on prosthetic limbs were compared with four combat-wounded service members with transfemoral amputations and contralateral transtibial amputations matched for height and body mass index (BMI). The aim of this study was to evaluate the gait parameters of patients undergoing through-knee amputation compared with patients with transfemoral amputation with all patients in both groups having contralateral transtibial amputations to help determine the value of through-knee amputation in combat-injured service members.
Specifically, we asked: (1) Does through-knee amputation result in improved gait velocity when compared with matched transfemoral amputees? (2) Do through-knee amputees have a faster gait cadence than matched transfemoral amputees? (3) Do through-knee amputees have a different stride length or stride width than matched transfemoral amputees? (4) Does through-knee amputation result in decreased work of ambulation when compared with matched transfemoral amputees?
Patients and Methods
This study was a retrospective case series with a matched control group. The entirety of the study was completed at Naval Medical Center, San Diego (San Diego, CA, USA) with institutional review board approval of the study. The data were collected retrospectively and analyzed from existing records between 2009 and 2014. A power analysis found that to detect a clinically important difference (set at a change in work of ambulation of 1 J/kg*m) with a p value of 0.05 and a β set to 0.2, a study population of 56 patients per group would be required; that being said, our results on a much smaller population must be considered exploratory.
Between January 2008 and December 2012, six male active-duty military patients who had undergone unilateral through-knee amputations as a result of trauma underwent gait studies at our institution. Of those, four of six underwent gait analysis after being able to walk for at least 3 months without assistive devices, and this group was studied here; all of these patients had contralateral below-knee amputations. The through-knee amputees who were not included both had elective revisions of their amputation from through-knee to a transfemoral amputation before completing 3-month gait data as a result of difficulty ambulating with unmatched knee centers for one patient and difficulty sitting in cars and on airplanes for the second. There were two additional through-knee amputees at our institution during this time period who were not included; one additional patient was revised at his request to a transfemoral amputation and the other patient did not have completed gait data at the time of this study. Each of the amputees studied was matched to a transfemoral amputee based on height, BMI, and contralateral amputation level resulting in a case-control study of active-duty military male amputee patients. Inclusion required complete gait data collected while walking at a self-selected pace wearing custom prosthetic devices. The through-knee amputees had a median age of 32 years (range, 23-41 years) and the transfemoral amputees had a median age of 24 years (range, 22-27 years).
Inclusion required complete gait data collected while walking at a self-selected pace wearing custom prosthetic devices. The patients with through-knee amputation were matched for height, BMI, and contralateral amputation level resulting in two matched groups; one group had four patients with a through-knee amputation and a contralateral transtibial amputation and the other group had four patients with a transfemoral amputation and a contralateral transtibial amputation.
Patients wore their customized prostheses and walked at their self-selected paces as three-dimensional gait data were collected with a 12-camera Motion Analysis Corporation (MAC) system (Motion Analysis Corp, Santa Rosa, CA, USA) and four floor-embedded AMTI Force plates (AMTI, Watertown, MA, USA). Trials were processed with Cortex (MAC) and OrthoTrac (MAC) software.
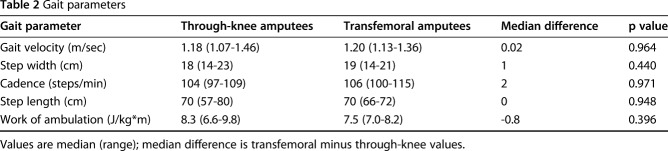
Variables examined included gait velocity, cadence, step width, step length, stride width, single-limb support, total stance time on each side, vertical ground reaction forces at early stance and late stance, and mechanical work. Visual3D (C-Motion, Inc, Germantown, MD, USA) was used to calculate the total mechanical work as the sum of the potential, translational, and rotational energies of each body segment integrated per stride length for both lower limbs and normalized per stride and body mass (J/kg*m). Femoral residual limb ratio was then linearly correlated with temporospatial, kinematic, kinetic, and mechanical work measures. Limb ratio was defined as the residual femoral length relative to the intact femoral length in percent [2]. The residual limbs were measured from the anterosuperior iliac spine to the residual soft tissue of the femur or to the medial knee line (Table 1).
Table 1.
Amputee demographics
Statistical Analysis
All statistical analysis was conducted using SPSS (Version 12; SPSS, Chicago, IL, USA). Mean and SD were calculated for all continuous variables such as age, radiographic displacement, and fragment size. Wilcoxon signed-rank tests were then applied. Bivariate analysis was used to obtain Pearson correlation coefficients to determine the effect of femoral limb ratio on gait parameters.
Results
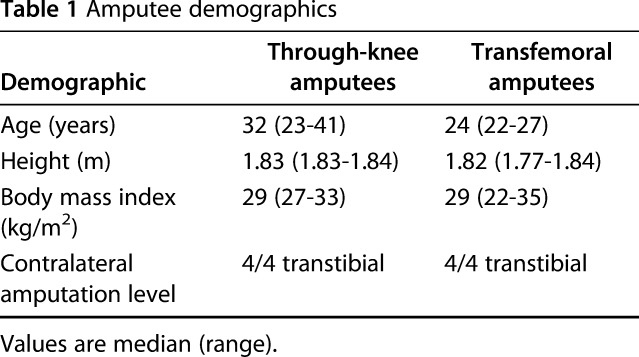
There was no difference identified between the median of gait velocities for through-knee amputees (1.18 m/sec) and matched transfemoral amputees (1.20 m/sec, difference of medians = 0.02 m/sec; p = 0.964) (Table 2).
Table 2.
Gait parameters
Through-knee amputees in this study had a median cadence of 104 steps/min compared with 106 steps/min for transfemoral amputees (difference of medians = 2 steps/min; p = 0.971) (Table 2).
The median stride length for through-knee amputees was 70 cm and the mean stride width was 18 cm. For transfemoral amputees, the median stride length was also 70 cm and the median step width was 19 cm (difference of medians = 0 and 1 cm; p = 0.948 and p = 0.440, respectively) (Table 2).
The median work of ambulation measured in Joules per kilogram per meter was 8.3 for through-knee amputees and 7.5 for transfemoral amputees (difference of medians = 0.8 J/kg*m; p = 0396). With the numbers available, none of the studied gait parameters were different between the two groups.
Discussion
Through-knee amputation was associated with poorer outcomes in the LEAP Study when compared with transfemoral and transtibial amputation levels [4, 7]. Through-knee amputation is an amputation level that is through a natural tissue plane that can be rapidly accomplished in a forward-deployed austere environment; however, the results of this as a final amputation level in a military population have not been well studied [1, 5, 11]. The current study found no difference in gait parameters between through-knee and transfemoral amputees.
This study had a number of limitations. First, our sample size of four through-knee amputees is small because this is a rare final amputation level. Our power analysis determined we would need 56 through-knee amputees and a matched same-sized cohort to confidently identify the minimum clinically important change in work of ambulation, which we established as a change of 1 J/kg*m. That being said, our no-difference results need to be interpreted cautiously, and future, larger studies are needed to replicate or refute the findings made here. Second, we did not have any patient-reported outcomes to compare the two groups. Future study should be directed toward evaluating all through-knee amputees across the military population with gait data and obtaining functional outcome scores such as SF-36 scores and comparing their gait parameters and functional outcome scores with matched control transfemoral amputees.
Pinzur et al. [9, 10] reported that patients who had through-knee amputations for peripheral vascular disease had higher walking velocity and lower energy cost of ambulation compared with transfemoral amputees. The current study did not identify a difference between the gait velocity of through-knee amputees with the numbers available. Likewise, we are not aware of any studies directly comparing gait cadence between through-knee and transfemoral amputees. In the current study, there was no difference with the numbers available in gait cadence between through-knee and transfemoral amputees.
Similarly, we are not aware of any studies directly comparing stride length or stride width between through-knee and transfemoral amputees. In the current study, with the numbers available, there was no difference between step width in through-knee and transfemoral amputees or stride length between through-knee and transfemoral amputees. A larger study would be required to make any definitive conclusions comparing through-knee and transfemoral amputation with regard to any gait parameters. Obtaining a large enough sample size to be sufficiently powered would require obtaining data from multiple military treatment facilities and potentially require multinational data collection. This study could serve as pilot data for such an investigation. Based on the results of further study, physicians treating traumatic injuries resulting in lower extremity amputation could better counsel patients and make more informed decisions intraoperatively when deciding between through-knee and transfemoral amputation.
Waters and Mulroy [17] found that oxygen consumption per kilogram per meter was higher for unilateral traumatic through-knee amputees than unilateral traumatic transfemoral amputees. They did not have any patients with through-knee amputations with contralateral amputations. In the present study, the work of ambulation for transfemoral amputees was no different than that of transfemoral amputees. A larger study would provide surgeons the knowledge of whether a through-knee amputation is best utilized as a temporary level for damage-control orthopaedics or for transport or if it is a viable permanent amputation level.
In conclusion, our data demonstrate that with the numbers available, there are no functional differences in any of the gait parameters tested between our groups of matched patients with transfemoral and through-knee amputations and contralateral transtibial amputations. Based on the size of our sample, we cannot make any definitive conclusions and the data here are likely best suited to serve as pilot data for a larger study. There are theoretical advantages for maintaining an intact femur during the medical evacuation and serial débridement process; further study could delineate the value of through-knee amputation as a definitive amputation level. Even if knee disarticulation is determined by future study not to be a viable final level, keeping the femur intact, if not already violated from the injury, can be useful during transport. The femur can ideally be cut to the final amputation level at the time of definitive closure. We do not advocate keeping the femur intact if it at all limits the ability to perform thorough soft tissue débridement.
Acknowledgments
We thank Dr Robert Riffenburgh for his assistance with the statistical analysis of our data.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Naval Medical Center San Diego, San Diego, CA, USA.
Dustin J. Schuett, Marilynn P. Wyatt, Trevor Kingsbury, and Kevin M. Kuhn are employees of the US Government and this work was prepared as part of their official duties. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of the Army, Department of Defense, nor the US Government. Nothing in the presentation implies any Federal/Department of Defense/Department of the Navy endorsement.
References
- 1.Batch JW, Spittler AW, McFaddin JG. Advantages of the knee disarticulation over amputations through the thigh. J Bone Joint Surg Am. 1954;36:921–930. [PubMed] [Google Scholar]
- 2.Baum BS, Schnall BL, Tis JE, Lipton JS. Correlation of residual limb length and gait parameters in amputees. Injury. 2008;39:728–733. [DOI] [PubMed] [Google Scholar]
- 3.Bennett PM, Sargeant ID, Midwinter MJ, Penn-Barwell JG. Unilateral lower limb loss following combat injury: medium-term outcomes in British military amputees. Bone Joint J. 2013;95:224–229. [DOI] [PubMed] [Google Scholar]
- 4.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski ML, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347:1924–1931. [DOI] [PubMed] [Google Scholar]
- 5.Bowker JH, San Giovanni TP, Pinzur MS. North American experience with knee disarticulation with use of a posterior myofasciocutaneous flap. Healing rate and functional results in seventy-seven patients. J Bone Joint Surg Am. 2000;82:1571–1574. [DOI] [PubMed] [Google Scholar]
- 6.Fischer H. A. Guide to US Military Casualty Statistics: Operation New Dawn, Operation Iraqi Freedom, and Operation Enduring Freedom. Congressional Research Service Report for Congress. 2014;7–5700. [Google Scholar]
- 7.MacKenzie EJ, Bosse MJ, Castillo RC, Smith DG, Webb LX, Kellam JF, Burgess AR, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, Travison TG, McCarthy ML. Functional outcomes following trauma-related lower-extremity amputation. J Bone Joint Surg Am. 2004;86:1636–1645. [DOI] [PubMed] [Google Scholar]
- 8.Penn-Barwell JG. Outcomes in lower limb amputation following trauma: a systematic review and meta-analysis. Injury. 2011;42:1474–1479. [DOI] [PubMed] [Google Scholar]
- 9.Pinzur MS. Gait analysis in peripheral vascular insufficiency through-knee amputation. J Rehabil Res Dev. 1993;30:388–392. [PubMed] [Google Scholar]
- 10.Pinzur MS, Bowker JH. Knee disarticulation. Clin Orthop Relat Res. 1999;361:23–28. [DOI] [PubMed] [Google Scholar]
- 11.Pinzur MS, Gold J, Schwartz D, Gross N. Energy demands for walking in dysvascular amputees as related to the level of amputation. J Orthop. 1992;15:1033-1036; discussion 1036–1037. [DOI] [PubMed] [Google Scholar]
- 12.Pinzur MS, Reddy NK, Osterman H. Through-knee amputation in peripheral vascular insufficiency: functional outcome. Contemp Orthop. 1992;24:157–160. [Google Scholar]
- 13.Pinzur MS, Smith DG, Daluga DJ, Osterman H. Selection of patients for through-the-knee amputation. J Bone Joint Surg Am. 1988;70:746–750. [PubMed] [Google Scholar]
- 14.Pinzur MS, Smith D, Tornow D, Meade K, Patwardhan A. Gait analysis of dysvascular below-knee and contralateral through-knee bilateral amputees: a preliminary report. J Orthop. 1993;16:875–879. [DOI] [PubMed] [Google Scholar]
- 15.Potter BK, Scoville CR. Amputation is not isolated: an overview of the US Army Amputee Patient Care Program and associated amputee injuries. J Am Acad Orthop Surg. 2006;14:S188–190. [DOI] [PubMed] [Google Scholar]
- 16.Tintle SM, Forsberg JA, Keeling JJ, Shawen SB, Potter BK. Lower extremity combat-related amputations. J Surg Ortho Adv. 2010;19:35–43. [PubMed] [Google Scholar]
- 17.Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9:207–231. [DOI] [PubMed] [Google Scholar]