Abstract
Background
Adolescent idiopathic scoliosis (AIS) is the most common spine deformity in adolescent patients. Although structural deformity may affect spinal biomechanics of patients with AIS, little is known regarding various period prevalence proportions of back pain and chronic back pain and factors associated with back pain in such patients.
Questions/purposes
(1) What are the period prevalence rates of back pain among teenagers with AIS? (2) Is back pain in patients with AIS associated with curve severity?
Methods
A total of 987 patients with AIS who were treated without surgery were recruited from a single center’s scoliosis clinic. Between December 2016 and July 2017, this center treated 1116 patients with suspected AIS. During that time, patients were offered surgery when their Cobb angle was at least 50° and had evidence of curve progression between two visits, and most of the patients who were offered surgery underwent it; other patients with AIS were managed nonsurgically with regular observation, brace prescription, posture training, and reassurance. To be included in this prospective, cross-sectional study, a patient needed to be aged between 10 and 18 years with a Cobb angle > 10°. No followup data were required. A total of 1097 patients with AIS were managed nonsurgically (98.3% of the group seen during the period in question). After obtaining parental consent, patients provided data related to their demographics; physical activity levels; lifetime, 12-month, 30-day, 7-day, and current thoracic pain and low back pain (LBP); chronic back pain (thoracic pain/LBP); brace use; and treatments for scoliosis/back pain. Pain was rated on a 10-point numeric rating scale for pain. The Insomnia Severity Index, Epworth Sleepiness Scale, and Depression Anxiety Stress Scales were also assessed. These features and radiologic study parameters between patients with and without back pain were also compared. Factors associated with current and 12-month back pain as well as chronic back pain were analyzed by multivariate analyses.
Results
Depending on the types of period prevalence, the prevalence of thoracic pain ranged from 6% (55 of 987) within 12 months to 14% (139 of 987) within 7 days, whereas that of LBP ranged from 6% (54 of 987) to 29% (289 of 987). Specifically, chronic thoracic pain or LBP had the lowest prevalence. Compared with the no pain group, patients with current back pain had more severe insomnia (odds ratio [OR], 1.80; p = 0.02; 95% confidence interval [CI], 1.10-2.93) and daytime sleepiness (OR, 2.41; p < 0.001, 95% CI, 1.43-4.07). Those with chronic back pain had the same problems along with moderate depression (OR, 2.49; p = 0.03; 95% CI, 1.08-5.71). Older age (OR range, 1.17–1.42; all p values ≤ 0.030) and Cobb angle > 40° (OR range, 2.38–3.74; all p values ≤ 0.015), daytime sleepiness (OR range, 2.39-2.41; all p values ≤ 0.011), and insomnia (OR range, 1.76–2.31; all p values ≤ 0.001) were associated with episodic and/or chronic back pain. Females were more likely to experience back pain in the last 12 months than males. Moderate depression (OR, 3.29; 1.45-7.47; p = 0.004) and wearing a brace (OR, 3.00; 1.47-6.15; p = 0.003) were independently associated with chronic back pain.
Conclusions
Biopsychosocial factors are associated with the presence and severity of back pain in the AIS population. Our results highlight the importance of considering back pain screening/management for patients with AIS with their psychosocial profile in addition to curve magnitude monitoring. In particular, sleep quality should be routinely assessed. Longitudinal changes and effects of psychotherapy should be determined in future studies.
Level of Evidence
Level II, prognostic study.
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common form of spinal deformity affecting 1% to 3% of teenagers [44]. Conventionally, AIS is defined as a three-dimensional spinal deviation with a Cobb angle > 10° of unknown origin occurring in teenagers aged 10 years and older [31]. The presence of spinal deformity may alter the spinal biomechanics and paraspinal musculature function, cause pain, and increase inflammatory responses, thereby increasing the risk of developing back pain [15]. Back pain leads to tremendous socioeconomic and psychologic distressful consequences [17]. Patients with AIS have reported a higher prevalence of back pain than individuals without scoliosis [4], although controversial findings have also been reported [37]. Depending on the types of period prevalence, the reported prevalence of back pain in patients with AIS ranged from 23% to 85% [12, 24, 27, 36, 37, 39, 41]. Sato et al. [38] found that the point prevalence and lifetime prevalence of back pain in adolescents with AIS were higher than that of adolescents without scoliosis (28% versus 11% and 59% versus 33%, respectively). Unfortunately, their findings were limited by a small number of adolescents with AIS (55 of 44,000 adolescents) [38]. Another retrospective study found that the lifetime prevalence of back pain in adolescents with AIS was 47% [40], which was higher than that in adolescents (40%) [7]. However, this study was limited by unclear definitions of back pain and inconsistent data reporting in medical records. Imperatively, no studies have systematically determined different period prevalence rates of back pain or chronic back pain within the same cohort to help understand the extent of the problem and to improve back pain management in this population.
Because early onset or persistence of back pain in adolescents was a predictor for future back pain and healthcare utilization in adults [5, 21, 23, 28, 32, 33], multiple studies have attempted to identify potential factors associated with back pain development in adolescents with AIS so that proper preventive measures can be developed and implemented [24, 39-41]. A retrospective study found that patients with reported thoracic scoliosis in their medical records were four times more likely to have thoracic pain than those without a thoracic curve. However, the severity of the Cobb angle was unrelated to pain intensity. Similarly, a cross-sectional study of 500 patients found that older age, not wearing a brace, and a more severe main thoracic curve and lumbar curve were independently associated with respective thoracic and lumbar pain intensity [41]. However, because these studies did not consider other potential physical and psychosocial factors that may be associated with back pain in patients with AIS, the actual association between spinal deformity and back pain remains unclear. Importantly, because no prior studies have been conducted to identify the factors associated with chronic back pain in this population, some high-risk individuals may have been missed for timely back pain interventions.
Therefore, our study questions are: (1) What are the period prevalence rates of back pain among teenagers with AIS? (2) Is back pain in patients with AIS associated with curve severity?
Patients and Methods
The current prospective cross-sectional study was conducted in a tertiary scoliosis outpatient clinic between December 2016 and July 2017. This is one of only two clinics in Hong Kong that receives patients with scoliosis in the region with a long-standing scoliosis screening program [16]. Hence, our clinic is representative of the entire local population of patients with scoliosis. A researcher (PWHC) approached consecutive patients and their guardians attending the clinic for recruitment. Patients aged between 10 and 18 years with a spinal Cobb angle of at least 10° were eligible for the study. Individuals were excluded if they could not communicate in both written and verbal forms of traditional Chinese. Other exclusion criteria included the presence of scoliosis other than idiopathic origin or other orthopaedic deformities such as juvenile idiopathic scoliosis; a history of spinal injury, like a fracture or spinal surgery; spondylolisthesis; spinal inflammation; spinal cancer; illiteracy; or developmental delay. On completion of parental written consent, patients were asked to fill out a set of questionnaires that asked about demographic data such as educational level, physical activity level, current and past back pain (if present), back pain treatments, brace wearing duration per day (thermal sensors), depression, anxiety, the quality and quantity of sleep, daytime sleepiness, physical function, appearance of AIS, and satisfaction of AIS treatments. All patients under brace treatment were prescribed underarm braces. For younger participants who could not complete the questionnaires by themselves, they would complete the questionnaires with assistance from their parents/guardians. The researcher (PWHC) immediately reviewed the completed questionnaires to ensure there were no missing data and to clarify any uncertain answers. The medical and radiologic information of participants was retrieved from the respective electronic medical records. The current study was approved by the institutional review board of The University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW15-584).
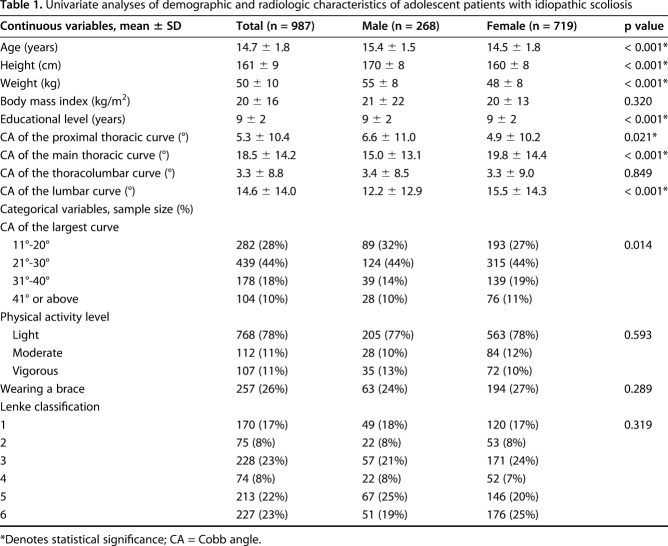
In all, 1116 potential participants were approached in the clinic; 987 met the inclusion criteria and provided consent to participate (Fig. 1). Individuals were excluded because of inappropriate age (n = 93), a history of spinal surgery (n = 16), declined participation (n = 11), juvenile idiopathic scoliosis (n = 6), or absence of scoliosis (n = 3). Compared with female participants (n = 719), male participants (n = 268) were older, taller, and displayed a smaller Cobb angle at the main thoracic curve (Table 1). This study took place at one time point for each patient and no followup was performed. Patients were asked to recall their symptoms as per questionnaire responses.
Fig. 1.
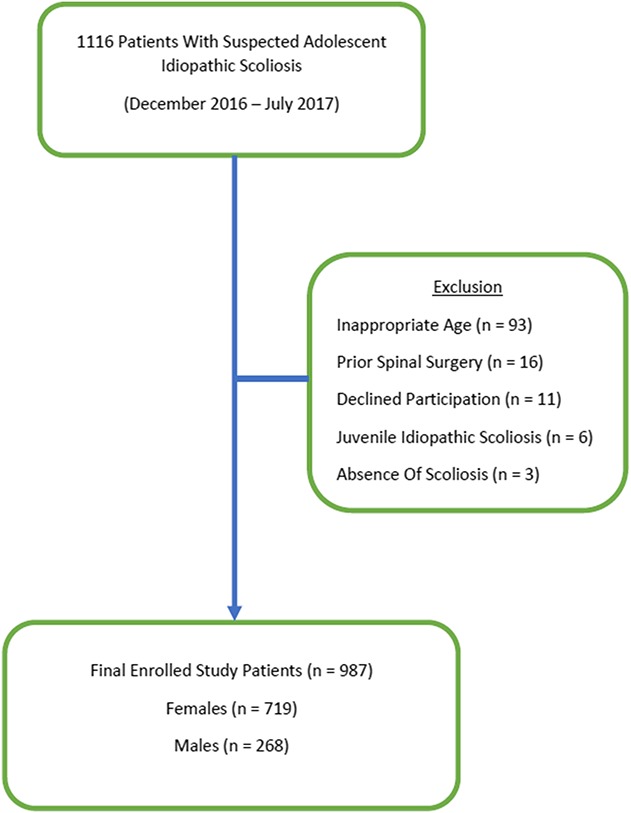
STROBE diagram showing the recruitment process of study patients. After exclusion, a total of 987 patients were enrolled into the study.
Table 1.
Univariate analyses of demographic and radiologic characteristics of adolescent patients with idiopathic scoliosis
Outcome Instruments
Demographic and Pain Questionnaire
The questionnaire comprised questions related to participants’ educational level, their parents’ educational levels and occupations, physical activity levels in the last 7 days, brace use, and daily duration brace use for those who used it. We classified the respondents’ physical activity level as light (all or most leisure time spent in minimal physical activity), moderate (two to six times in the last week participating in physical activity/exercises during leisure time), and vigorous (seven or more times in the last week participating in physical activity/exercises during leisure time).
Additionally, the questionnaire also collected data regarding current pain in the thoracic and lumbar region; thoracic and lumbar pain at rest or during activity in the last 7 days, 30 days, 12 months, and lifetime as well as chronic thoracic and lumbar pain that lasted for at least 3 months during the last 12 months. If respondents reported back pain during any of those periods, they rated their pain using a 11-point numeric pain rating scale (NPRS), where 0 means no pain and 10 means the worst imaginable pain [46]. The minimal clinical important difference for the NPRS is 2 [8, 10]. They also answered questions regarding the types of healthcare practitioners they visited for the current or previous spinal pain; the presence of radiating leg pain at rest or during activity in the last 7 days, 30 days, and 12 months; the number of recurrent back pain episodes in the last 12 months; and the impact of pain on one’s studying hours, working hours, and leisure activities. Participants also rated their degrees of satisfaction with their back pain treatments and their perceived acceptance of living with thoracic or lumbar pain for the rest of their life on an 11-point numeric rating scale (-5 means extremely unsatisfied and 5 means extremely satisfied).
A human body silhouette was used to help the respondent demarcate the location of their pain and the nature of the pain such as burning, pins and needles, dull ache, or sharp pain. A similar method has been used in prior research to document back pain in adolescents with AIS [27].
Depression, Anxiety, and Stress Scale-21 (DASS-21)
The DASS-21 is the shortened form of DASS for the assessment of the 1-week emotional states of depression, anxiety, and stress [34]. It includes three seven-item subscales. Each subscale can be administered separately to evaluate respective emotional states. Each item is rated on a 4-point Likert-type scale; 0 means does not apply to the respondent, whereas 3 indicates applies to the respondent very much or most of the time. The sum of the item scores within each subscale equals the subscale scores (ranging from 0 to 21). From the subscale scores, the emotional condition is classified into normal (0-6), moderate to severe (7-13), and very severe (≥ 14). In the current study, only the depression and anxiety subscales were used to minimize the burden of respondents. The depression subscale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia. The anxiety subscale evaluates autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The use of the DASS-21 has been validated for assessing depression and anxiety among adolescents in various countries with excellent psychometric properties (such as reliability) and good internal consistency [25, 43]. Because only 2.0% of participants reported very severe depression and 3.2% reported anxiety, participants were dichotomized into having no depression/anxiety and moderate-to-very severe depression/anxiety categories.
Insomnia Severity Index (ISI)
This seven-item scale evaluates the severity of insomnia, the satisfactory level with sleep, noticeability of insomnia, perceived stress associated with insomnia, and interference of insomnia on daily functioning. It is a clinically reliable instrument in detecting insomnia [47]. Each item is rated on a 5-point Likert scale, where 0 indicates no problem and 4 indicates a very severe problem, yielding a high score of 28. The overall score is interpreted as follows: absence of clinically significant insomnia (0–7), subthreshold insomnia (8–14), moderate insomnia (15–21), and severe insomnia (22–28). The Chinese version of the ISI has demonstrated satisfactory test-retest reliability (r = 0.79) and high validity in detecting clinical insomnia among adolescents in Hong Kong [11]. Because only 2.6% of participants reported having moderate insomnia and 0.1% reported having severe insomnia, participants were dichotomized into no insomnia and having subthreshold-to-severe insomnia categories.
Epworth Sleepiness Scale (ESS)
This eight-item self-reported questionnaire measures daytime sleep tendency [11]. Respondents rated their tendency of dozing under eight daily living situations on a 3-point scale, where 0 indicates never dozing and whereas 3 indicates high propensity of dozing. From the overall scores of the ESS, participants were classified into normal daytime sleepiness (< 10), mild-to-moderate excessive daytime sleepiness (10-15), and severe excessive daytime sleepiness (16-24). Previous research has adopted the ESS in assessing daytime sleepiness of local adolescents with high test-retest reliability [11]. Because only 1% of the participants reported having severe excessive daytime sleepiness, participants were dichotomized into normal daytime sleepiness and mild-to-severe daytime sleepiness categories.
Refined Scoliosis Research Society-22 (SRS-22r) Patient Questionnaire
This questionnaire is the most commonly used self-reported outcome measure for evaluating adolescents with AIS [1, 2]. The Chinese version of the SRS-22r has demonstrated high reliability and concurrent validity in the local population [9]. The questionnaire consists of 22 questions encompassing five domains: function/activity (five items); pain (five items); self-perceived image (five items); mental health (five items); and satisfaction with scoliosis treatment (two items). Each item is rated at a 5-point scale ranging from 1 (worst) to 5 (best). The total scores in the first four domains range from 5 to 25, whereas that in the satisfaction domain ranges from 2 to 10. The highest total sum of all domains scores is 110. In the current study, the average score in each domain (total scores within the domain divided by the respective number of items) and average total score of the SRS-22r questionnaire were calculated to estimate differences between people with and without back pain.
Medical and Radiology Records
A blinded investigator (PWHC) retrieved the most recent medical information regarding comorbidities, age, sex, height, and weight from each participant’s electronic medical record, whereas an experienced orthopaedic specialist (JPYC), who was blinded to the questionnaire results, collected the radiographic information of each consented participant from the same system. Specifically, the standing coronal and sagittal radiographs were used to classify the spinal curve type of each participant using the Lenke classification [26]. The coronal Cobb angles of all curves were measured and were classified as proximal thoracic, main thoracic, thoracolumbar/lumbar, and lumbar curves. Apical vertebral rotation (AVR) was measured at the apex of the spinal curve(s) using the Nash-Moe method [30]. Thoracic kyphosis between T5 and T12 was classified into hypokyphosis (< 10°), normal kyphosis (10°-40°), and hyperkyphosis (> 40°) [26]. Risser staging (0-5) was also documented on the same radiograph.
Statistical Analysis
SPSS Version 24.0 software (IBM, Armonk, NY, USA) was used for statistical analyses. Descriptive data are expressed as means, SDs, or percentages. To identify the factors associated with back pain (thoracic, low back pain, or concurrent thoracic and low back pain) in adolescents with current back pain and back pain in the last 12 months, the demographic data (including age, sex, height, weight, body mass index, physical activity level, brace wearing status), radiologic data (Cobb angles at the proximal thoracic curve, main thoracic curve, thoracolumbar curve, lumbar curve, AVR at the four spinal regions, sagittal Cobb angles at the main thoracic region, single curve to double curve ratio, Lenke grades, Risser grades), depression, anxiety, and sleep-related factors between adolescents with and without back pain at present and in the last 12 months were first compared by independent t-tests, Mann-Whitney tests, or chi-square tests depending on the normality and types of data, either continuous or categorical. Potential parameters (that is, Cobb angles at the main thoracic and lumbar curves, AVR at the thoracolumbar region, Risser sign, anxiety, depression, dichotomized ISI variable, and dichotomized ESS variable) that showed considerable differences between groups (p < 0.20) were then entered into the respective stepwise logistic regression models. Specifically, we entered each dichotomized pain variable such as current back pain, back pain in the last 12 months, or chronic back pain in the last 12 months as a dependent variable while we entered the potential variables as independent variables. Age and sex were also entered into the models as independent variables because prior research reported that they might be factors associated with spinal pain in patients with AIS [41]. On completion of the multivariate analyses, we found that Cobb angles at the main thoracic and the lumbar regions were related to back pain. To help clinicians apply these findings when identifying patients with AIS at risk for back pain, especially chronic back pain, we repeated separate multivariate analyses using dichotomized Cobb angles at the main thoracic and lumbar curves with cutoffs at 20°, 30°, and 40°. The significance level was set at < 0.05. Odds ratios (ORs) and 95% confidence intervals (CIs) were used to assess the strength of association and precision, respectively.
Results
Point Prevalence, 7-day, 30-day, 12-month, and Lifetime Prevalence of Back Pain
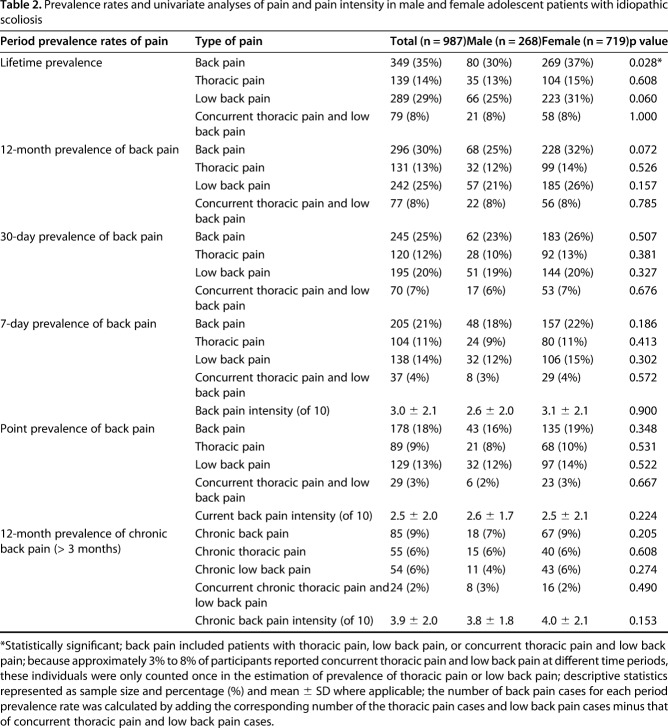
Because approximately 2% to 8% of participants reported concurrent thoracic and low back pain at different time periods, these individuals were only counted once in the estimation of prevalence of back pain. There was no difference in all period prevalence rates of back pain (thoracic or lumbar pain) between male and female participants except that female participants (37%) had a higher lifetime prevalence than male participants (30%) (OR, 1.1; 95% CI, 1.02-1.2; p = 0.028) (Table 2). The point prevalence of thoracic pain was 9%, the 7-day prevalence was 11%, 30-day prevalence was 12%, 12-month was 13%, and lifetime prevalence of thoracic pain was 14%. For low back pain, the point prevalence was 13%, 7-day was 14%, 30-day was 20%, 12-month was 25%, and lifetime prevalence was 29%. Similarly, the point prevalence of back pain (thoracic pain, low back pain, or concurrent thoracic and low back pain) was 18%, 7-day was 21%, 30-day prevalence was 25%, 12-month was 30%, and lifetime prevalence was 36% (Table 2). The 12-month prevalence of chronic thoracic pain was 6%, for low back pain it was 6%, and for back pain it was 9%.
Table 2.
Prevalence rates and univariate analyses of pain and pain intensity in male and female adolescent patients with idiopathic scoliosis
Factors Associated With Current Back Pain, Back Pain in the Last 12 Months, and Chronic Back Pain
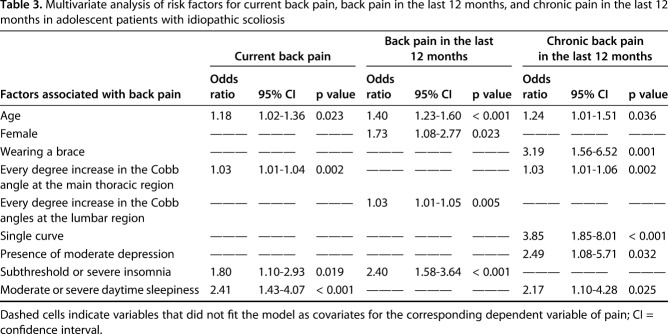
After controlling for potential confounding variables (including Risser sign, Cobb angles of the lumbar curve), our analysis revealed that the presence of insomnia (OR, 2.48; 95% CI, 1.10-2.93), moderate/severe daytime sleepiness (OR, 1.75; 95% CI, 1.43-4.07), older age (OR, 1.18 per year; 95% CI, 1.02-1.36), and larger Cobb angles at the main thoracic curve (OR, 1.03 per degree; 95% CI, 1.01-1.04) were independent factors associated with the presence of current back pain (Table 3). Similarly, insomnia (OR, 2.40; 95% CI, 1.58-3.64), female sex (OR, 1.73; 95% CI, 1.08-2.77), older age (OR, 1.40 per year; 95% CI, 1.23-1.60), and larger Cobb angles at the lumbar curve (OR, 1.03 per degree; 95% CI, 1.01-1.05) were factors associated with back pain in the last 12 months. The factors associated with chronic back pain in patients with AIS included the presence of a single curve (OR, 3.85; 95% CI, 1.85-8.01), brace wearing (OR, 3.19; 95% CI, 1.56-6.52), moderate depression (OR, 2.49; 95% CI, 1.08-5.71), moderate/severe daytime sleepiness (OR, 2.17; 95% CI, 1.10-4.28), and older age (OR, 1.24 per year; 95% CI, 1.01-1.51) (Table 3).
Table 3.
Multivariate analysis of risk factors for current back pain, back pain in the last 12 months, and chronic pain in the last 12 months in adolescent patients with idiopathic scoliosis
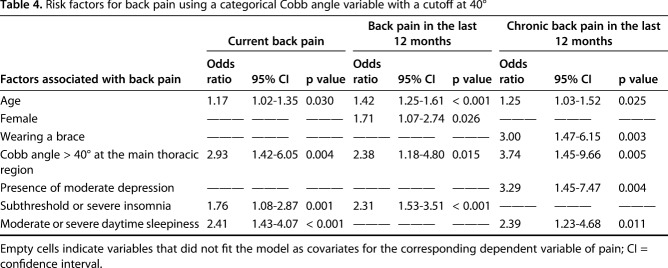
After controlling for potential confounding variables such as height, weight, and body mass index, we found that a coronal Cobb angle > 40° at the main thoracic curve and older age were universal independent factors associated with back pain episodes and chronic back pain in patients with AIS (Table 4). The factors associated with current back pain included a main thoracic curve with coronal Cobb angles > 40° (OR, 2.93; 95% CI, 1.42-6.05), moderate/severe daytime sleepiness (OR, 2.41; 95% CI, 1.43-4.07), subthreshold or severe insomnia (OR, 1.76; 95% CI, 1.08-2.87), and older age (OR, 1.17 per year; 95% CI, 1.02-1.35). Likewise, a main thoracic curve with coronal Cobb angles > 40° (OR, 2.38; 95% CI, 1.18-4.80), subthreshold to severe insomnia (OR, 2.31; 95% CI, 1.53-3.51), older age (OR, 1.42 per year; 95% CI, 1.25-1.61), and females (OR, 1.71; 95% CI, 1.07-2.74) were factors associated with back pain within the last 12 months. Similarly, patients were likely to have chronic back pain if they had main thoracic Cobb angles > 40° (OR, 3.74; 95% CI, 1.45-9.66), presented with moderate depression (OR, 3.74; 95% CI, 1.45-9.66), daytime sleepiness (OR, 2.39; 95% CI, 1.23-4.68), wore a brace (OR, 3.00; 95% CI, 1.47-6.15), and were older (OR, 1.25 per year; 95% CI, 1.03-1.52) (Table 4). Although the dichotomized variable of Cobb angles > 30° was also related to current back pain (OR, 1.83; 95% CI, 1.06-3.15) and back pain in the last 12 months (OR, 1.74; 95% CI, 1.07-2.84) in two of the multivariate analyses, it was not associated with chronic back pain in the last 12 months (Appendix, Supplemental Digital Content 1, http://links.lww.com/CORR/A112).
Table 4.
Risk factors for back pain using a categorical Cobb angle variable with a cutoff at 40°
Discussion
Patients with AIS appear to have a higher prevalence of back pain, but it is unclear whether there is any important association between this symptom and spinal deformity. There is also limited understanding of the severity of this problem and factors associated with its occurrence, severity, or chronicity [7, 38, 41, 42]. Our results suggest that back pain is not uncommon (8.6%) among these patients. However, more importantly, patients with AIS and back pain not only experienced pain and physical dysfunction, but also demonstrated clinically significant anxiety, depression, insomnia, and daytime sleepiness. Factors including main thoracic Cobb angles > 30°, moderate-to-severe insomnia or daytime sleepiness, older age, and female sex were closely related to back pain at present or over a 12-month period. Other associated factors with chronic back pain include Cobb angles > 40°, brace wearing, depression, moderate-to-serve insomnia, and daytime sleepiness. These revelations suggest that clinicians should not only focus on the curve magnitude, but also investigate if there is any back pain and modifiable psychosocial factors such as sleep quality and depression.
Like with any study, limitations exist. Recall bias is an important and commonly encountered limitation with a cross-sectional study design because patients may have difficulty in recalling pain over longer periods and may overestimate/underestimate pain episodes based on current mood or current pain intensity [14, 18, 22]. Because the longer the recall period, the greater the risk of unreliable data [20, 29], we only asked patients to recall pain intensity within 7 days or chronic pain intensity within the last 12 months. This recall period aligns well with other similar epidemiologic studies [29]. The current study was also limited by the adoption of some questionnaires (the DASS-21, ISI, and ESS) that have not been validated in Chinese teenagers with AIS. However, because they have been used in the pediatric population, our results should be relevant. Additionally, although the questionnaires used to collect data regarding the presence of back pain at different time periods or the perceived acceptance of living with back pain for the rest of their life have not validated, these questionnaires are simple and straightforward, and their findings should be easy to interpret. Even so, without validation, we urge some caution in their application.
Similar to prior research on the epidemiology of back pain in adolescents [29], our participants were asked to report back pain episodes over different time periods regardless of pain intensity or pain at rest or during activity. Although this might have overestimated some period prevalence rates of back pain in adolescents with AIS, this simple definition of pain could minimize the burden on adolescents in answering the questionnaire. Future studies should investigate the impacts of different definitions of back pain in affecting the reported prevalence of back pain in this population. In addition, the causal relationship between the identified factors and back pain cannot be established by our study. A prospective study design is warranted to address this relationship. Furthermore, because extra radiographic imaging was not taken at the time of this study, the spinal parameters were measured from the latest radiologic images in the electronic medical record. However, because patients usually undergo annual radiography, the changes in spinal structures should not be substantial. Limited analysis of sagittal spinopelvic parameters was conducted in the current study. Sagittal parameters like the sagittal vertical axis or pelvic incidence may play a role in back pain, although other factors (such as Lenke type) may also be associated with both sagittal parameters and back pain. A dedicated future study on sagittal alignment in the AIS population is warranted.
The current study has the advantage of representing a large homogenous sample of Chinese patients with AIS, whereby various confounding variables often found in mixed populations are diminished. Furthermore, the degree of relationship explored in our study suggests that the association of fundamental ethnic and cultural values may not be as strong. That said, evidence should be generated in future studies to address the generalizability of the findings to other populations. Importantly, given the very large sample size of the present study and the use of multiple radiographic parameters and psychosocial factors, robust multivariate analyses were performed to identify key determinants for back pain in adolescents with AIS. Our findings suggest that some modifiable and nonmodifiable factors are closely related to back pain in these adolescents. Clinicians should identify patients who experience back pain alongside insomnia and depression symptoms so that proper treatments can be given to minimize the risk of developing chronic back pain.
The reported prevalence rates of back pain in adolescents with AIS in prior studies range from 23% to 85% [13, 36, 37, 41, 45]. Sato et al. [38] conducted a cross-sectional population-based study to compare the prevalence of back pain in elementary schoolchildren with and without AIS. Their reported point and lifetime prevalence rates of children with AIS were 27.5% and 58.8%, which were much higher than the reported point (9%) and lifetime prevalence (23%) of patients with scoliosis found by Ramirez et al. [37]. In the current study, our point (18.0%) and lifetime prevalences (35.4%) were between the ranges reported by these two studies. The discrepancy might be attributed to differences in data collection methods (population-based research versus consecutive sampling from scoliosis clinics) and sampling populations. Although Sato et al. [38] recruited approximately 44,000 participants, only 55 of them had AIS. Their results should be interpreted with caution. Although both Ramirez et al. [37] and the current study recruited patients from scoliosis clinics, Ramirez et al. included patients aged between 9 months and 22 years. As such, some of their findings were unrelated to adolescents with AIS. Given these results, our findings help clinicians better understand various period prevalence rates of back pain in patients with AIS. Future longitudinal studies should adopt a similar approach to determine trajectories of back pain in teenagers with AIS.
Compared with asymptomatic patients with AIS, those with back pain demonstrated poorer physical function and sleep problems. Although it is known that back pain can cause functional limitations in adolescents, the current study found that these young individuals with back pain were experiencing insomnia and daytime sleepiness, which may affect their learning, back pain perpetuation, and even scoliosis curve progression [3]. Auvinen et al. [3] found that adolescents with insufficient sleep at 16 years old were more likely to experience neck, shoulder, and low back pain at age 18 years (OR range, 2.4–3.2) as compared with those without sleep problems. Given the findings from previous research [3, 35] and ours about the relationship between sleep and pain, it seems important that surgeons should consider referring young patients with AIS and back pain to sleep therapists for sleep hygiene training. Additionally, because the insomnia-related deprivation of melatonin may be related to the curve progression in patients with AIS [19], special attention should be given to the sleep quantity and quality of patients with AIS so that proper interventions can be implemented in these young and vulnerable individuals.
Prior research has reported that certain spinal deformities such as the location of the thoracic curve are related to the corresponding regional pain [40]. Their findings were limited by the lack of adjustment for various physical and psychosocial factors. Because the causes of back pain are multifactorial [6], it is necessary to account for the effects of various potential confounders to clarify the relation between spinal deformity and back pain. For instance, depression, anxiety, or physical activity levels can influence the perception and perpetuation of pain. Thereby, the current study included multiple potential physical and psychosocial factors in the multivariate analyses so as to identify the modifiable and nonmodifiable factors associated with back pain in adolescents with AIS. Our results corroborate previous findings that the severity of the main thoracic curve and older age are related to the presence of back pain in these patients [41]. Interestingly, although Theroux et al. [41] and Smorgick et al. [39] found that braced patients with AIS reported less pain than their nonbraced counterparts, we found that brace wearing is a factor associated with chronic back pain. The discrepancy may be attributed to the fact that patients with a larger spinal curve are prescribed brace treatment. Because larger Cobb angles are found to be a factor associated with pain in the current study, the revelation of brace wearing as a factor associated with chronic back pain further substantiates this notion.
In conclusion, our large-scale study found that the presence of back pain, regardless of whether it was acute or chronic, was associated with decreased sleep quantity and quality in young patients. Importantly, after adjusting for age, sex, and other psychosocial factors, we noted that a main thoracic Cobb angle > 40° was found to increase the odds of having back pain in adolescents with AIS, underscoring the critical implications of a curve magnitude threshold on pain generation. Because an early onset of back pain in adolescents can heighten the risk of recurrence in adulthood [5, 21, 23, 28, 32, 33], future studies should determine if some of the novel factors associated with pain identified in our study can successfully predict back pain and further flag such high-risk individuals. Our study further underscores the need to prospectively and longitudinally assess the implications of such parameters in the development of back pain and its natural history. Additional studies are needed to further replicate our findings in other ethnic populations and assess their implications on quality of life and healthcare-related costs.
Acknowledgments
We thank Mr. Matthew T. H. Chung for help with the literature search and with summarizing relevant information for the preparation of the manuscript.
Footnotes
The authors received a grant from the General Research Fund of the Research Grants Council reference # 17156416 (JPYC).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Asher M, Min Lai S, Burton D, Manna B. Discrimination validity of the Scoliosis Research Society-22 Patient Questionnaire: relationship to idiopathic scoliosis curve pattern and curve size. Spine (Phila Pa 1976) . 2003;28:74-78. [DOI] [PubMed] [Google Scholar]
- 2.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the Scoliosis Research Society-22 Patient Questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) . 2003;28:63-69. [DOI] [PubMed] [Google Scholar]
- 3.Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Jarvelin MR, Taanila AM, Karppinen JI. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J . 2010;19:641-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balague F, Skovron ML, Nordin M, Dutoit G, Pol LR, Waldburger M. Low back pain in schoolchildren. A study of familial and psychological factors. Spine (Phila Pa 1976) . 1995;20:1265-1270. [DOI] [PubMed] [Google Scholar]
- 5.Brattberg G. Do pain problems in young school children persist into early adulthood? A 13-year follow-up. Eur J Pain . 2004;8:187-199. [DOI] [PubMed] [Google Scholar]
- 6.Burton AK, Balague F, Cardon G, Eriksen HR, Henrotin Y, Lahad A, Leclerc A, Muller G, van der Beek AJ; COST B13 Working Group on European Guidelines for Prevention in Low Back Pain. How to prevent low back pain. Best Pract Res Clin Rheumatol . 2005;19:541-555. [DOI] [PubMed] [Google Scholar]
- 7.Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr . 2013;13:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheung JPY, Cheung PWH, Law K, Borse V, Lau YM, Mak LF, Cheng A, Samartzis D, Cheung KMC. Postoperative rigid cervical collar leads to less axial neck pain in the early stage after open-door laminoplasty--a single-blinded randomized controlled trial. Neurosurgery . 2018. Aug 3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 9.Cheung KM, Senkoylu A, Alanay A, Genc Y, Lau S, Luk KD. Reliability and concurrent validity of the adapted Chinese version of Scoliosis Research Society-22 (SRS-22) questionnaire. Spine (Phila Pa 1976) . 2007;32:1141-1145. [DOI] [PubMed] [Google Scholar]
- 10.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) . 2005;30:1331-1334. [DOI] [PubMed] [Google Scholar]
- 11.Chung KF, Kan KK, Yeung WF. Assessing insomnia in adolescents: comparison of Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index. Sleep Med . 2011;12:463-470. [DOI] [PubMed] [Google Scholar]
- 12.Clark EM, Tobias JH, Fairbank J. The impact of small spinal curves in adolescents who have not presented to secondary care: a population-based cohort study. Spine (Phila Pa 1976) . 2016;41:E611-E617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dickson JH, Erwin WD, Rossi D. Harrington instrumentation and arthrodesis for idiopathic scoliosis. A twenty-one-year follow-up. J Bone Joint Surg Am . 1990;72:678-683. [PubMed] [Google Scholar]
- 14.Eich E, Reeves JL, Jaeger B, Graff-Radford SB. Memory for pain: relation between past and present pain intensity. Pain . 1985;23:375-380. [DOI] [PubMed] [Google Scholar]
- 15.Eyvazov K, Samartzis D, Cheung JP. The association of lumbar curve magnitude and spinal range of motion in adolescent idiopathic scoliosis: a cross-sectional study. BMC Musculoskelet Disord . 2017;18:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fong DY, Cheung KM, Wong YW, Wan YY, Lee CF, Lam TP, Cheng JC, Ng BK, Luk KD. A population-based cohort study of 394,401 children followed for 10 years exhibits sustained effectiveness of scoliosis screening. Spine J . 2015;15:825-833. [DOI] [PubMed] [Google Scholar]
- 17.GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet . 2016;388:1603-1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gendreau M, Hufford MR, Stone AA. Measuring clinical pain in chronic widespread pain: selected methodological issues. Best Pract Res Clin Rheumatol . 2003;17:575-592. [DOI] [PubMed] [Google Scholar]
- 19.Girardo M, Bettini N, Dema E, Cervellati S. The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis (AIS). Eur Spine J . 2011;20(Suppl 1):S68-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goodman JE, McGrath PJ. The epidemiology of pain in children and adolescents: a review. Pain . 1991;46:247-264. [DOI] [PubMed] [Google Scholar]
- 21.Harreby M, Neergaard K, Hesselsoe G, Kjer J. Are radiologic changes in the thoracic and lumbar spine of adolescents risk factors for low back pain in adults? A 25-year prospective cohort study of 640 school children. Spine (Phila Pa 1976) . 1995;20:2298-2302. [DOI] [PubMed] [Google Scholar]
- 22.Jamison RN, Sbrocco T, Parris WC. The influence of physical and psychosocial factors on accuracy of memory for pain in chronic pain patients. Pain . 1989;37:289-294. [DOI] [PubMed] [Google Scholar]
- 23.Jeffries LJ, Milanese SF, Grimmer-Somers KA. Epidemiology of adolescent spinal pain: a systematic overview of the research literature. Spine (Phila Pa 1976) . 2007;32:2630-2637. [DOI] [PubMed] [Google Scholar]
- 24.Joncas J, Labelle H, Poitras B, Duhaime M, Rivard CH, Le Blanc R. [Dorso-lumbal pain and idiopathic scoliosis in adolescence] [in French]. Ann Chir . 1996;50:637-640. [PubMed] [Google Scholar]
- 25.Le MTH, Tran TD, Holton S, Nguyen HT, Wolfe R, Fisher J. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLoS One . 2017;12:e0180557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am . 2001;83:1169-1181. [PubMed] [Google Scholar]
- 27.Makino T, Kaito T, Kashii M, Iwasaki M, Yoshikawa H. Low back pain and patient-reported QOL outcomes in patients with adolescent idiopathic scoliosis without corrective surgery. Springerplus . 2015;4:397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mikkelsson M, El-Metwally A, Kautiainen H, Auvinen A, Macfarlane GJ, Salminen JJ. Onset, prognosis and risk factors for widespread pain in schoolchildren: a prospective 4-year follow-up study. Pain . 2008;138:681-687. [DOI] [PubMed] [Google Scholar]
- 29.Milanese S, Grimmer-Somers K. What is adolescent low back pain? Current definitions used to define the adolescent with low back pain. J Pain Res . 2010;3:57-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am . 1969;51:223-229. [PubMed] [Google Scholar]
- 31.Negrini S, Hresko TM, O'Brien JP, Price N; SOSORT Boards; SRS Non-Operative Committee. Recommendations for research studies on treatment of idiopathic scoliosis: consensus 2014 between SOSORT and SRS non-operative management committee. Scoliosis . 2015;10:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Sullivan P, Beales D, Jensen L, Murray K, Myers T. Characteristics of chronic non-specific musculoskeletal pain in children and adolescents attending a rheumatology outpatients clinic: a cross-sectional study. Pediatr Rheumatol Online J . 2011;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Sullivan PB, Beales DJ, Smith AJ, Straker LM. Low back pain in 17 year olds has substantial impact and represents an important public health disorder: a cross-sectional study. BMC Public Health . 2012;12:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21): further examination of dimensions, scale reliability, and correlates. J Clin Psychol . 2012;68:1322-1338. [DOI] [PubMed] [Google Scholar]
- 35.Pakpour AH, Yaghoubidoust M, Campbell P. Persistent and developing sleep problems: a prospective cohort study on the relationship to poor outcome in patients attending a pain clinic with chronic low back pain. Pain Pract . 2018;18:79-86. [DOI] [PubMed] [Google Scholar]
- 36.Pratt RK, Burwell RG, Cole AA, Webb JK. Patient and parental perception of adolescent idiopathic scoliosis before and after surgery in comparison with surface and radiographic measurements. Spine (Phila Pa 1976). 2002;27:1543-1550; discussion 1551-1552. [DOI] [PubMed] [Google Scholar]
- 37.Ramirez N, Johnston CE, Browne RH. The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am . 1997;79:364-368. [DOI] [PubMed] [Google Scholar]
- 38.Sato T, Hirano T, Ito T, Morita O, Kikuchi R, Endo N, Tanabe N. Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J . 2011;20:274-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Smorgick Y, Mirovsky Y, Baker KC, Gelfer Y, Avisar E, Anekstein Y. Predictors of back pain in adolescent idiopathic scoliosis surgical candidates. J Pediatr Orthop . 2013;33:289-292. [DOI] [PubMed] [Google Scholar]
- 40.Theroux J, Le May S, Fortin C, Labelle H. Prevalence and management of back pain in adolescent idiopathic scoliosis patients: a retrospective study. Pain Res Manag . 2015;20:153-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Theroux J, Le May S, Hebert JJ, Labelle H. Back pain prevalence is associated with curve-type and severity in adolescents with idiopathic scoliosis: a cross-sectional study. Spine (Phila Pa 1976) . 2017;42:E914-E919. [DOI] [PubMed] [Google Scholar]
- 42.Theroux J, Stomski N, Hodgetts CJ, Ballard A, Khadra C, Le May S, Labelle H. Prevalence of low back pain in adolescents with idiopathic scoliosis: a systematic review. Chiropr Man Therap . 2017;25:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tully PJ, Zajac IT, Venning AJ. The structure of anxiety and depression in a normative sample of younger and older Australian adolescents. J Abnorm Child Psychol . 2009;37:717-726. [DOI] [PubMed] [Google Scholar]
- 44.Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet . 2008;371:1527-1537. [DOI] [PubMed] [Google Scholar]
- 45.Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am . 1981;63:702-712. [PubMed] [Google Scholar]
- 46.Wong AY, Parent EC, Prasad N, Huang C, Chan KM, Kawchuk GN. Does experimental low back pain change posteroanterior lumbar spinal stiffness and trunk muscle activity? A randomized crossover study. Clin Biomech (Bristol, Avon) . 2016;34:45-52. [DOI] [PubMed] [Google Scholar]
- 47.Yu DS. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs . 2010;66:2350-2359. [DOI] [PubMed] [Google Scholar]