Abstract
Aims
This study aims to examine the effect of differences in nutritional status on activities of daily living (ADL) and mobility recovery of hospitalized elderly patients with heart failure (HF).
Methods and results
From among 377 consecutive HF patients who underwent rehabilitation at one acute‐care hospital from January 2013 to August 2015, those who were aged ≥ 65 years could walk with assistance before hospitalization and who were hospitalized for the first time were included in this retrospective cohort study. Exclusion criteria were pacemaker surgery during hospitalization, change to other departments, death during hospitalization, and unmeasured ADL. We investigated patient characteristics, basic attributes, Geriatric Nutritional Risk Index (GNRI), ADL [motor Functional Independence Measure (motor FIM)], and Rivermead Mobility Index (RMI). Of these 377 patients, 96 met the inclusion criteria and were divided into the low GNRI group (n = 38, 83.5 ± 8.3 years, 44.7% male) and high GNRI group (n = 58, 81.0 ± 6.6 years, 55.2%). Patient characteristics and the difference between motor ADL and motility recovery and nutrition data were analysed with unpaired t‐test, χ 2 test, and two‐way analysis of covariance. In comparing the two groups, the following parameters were significantly lower in the low GNRI group than in the high GNRI group: body mass index (18.7 ± 2.2 vs. 23.2 ± 2.7 kg/m2, P < 0.01), albumin (3.4 ± 0.4 vs. 3.8 ± 0.4 g/dL, P < 0.01), diabetes mellitus ratio (21.1% vs. 50.0%, P < 0.01), RMI at discharge (6.8 ± 2.6 vs. 8.2 ± 2.2, P = 0.01), and motor FIM at discharge (67.2 ± 19.5 vs. 75.6 ± 13.3, P = 0.02). RMI showed a significant group and term main effect and interaction effect (P < 0.05). Motor FIM showed a significant main effect of group and term (P < 0.05), and no significant interaction effect.
Conclusions
Low nutritional status in hospitalized elderly HF patients affected their recovery of mobility but did not appear to affect the recovery of ADL.
Keywords: Activities of daily living, Elderly, Heart failure, Mobility, Nutritional
Introduction
The number of elderly people is increasing worldwide, and this increase is especially remarkable in Japan, where the elderly make up 27.3% of the population.1, 2, 3 Also, the number of patients with heart failure (HF) is similarly increasing, and their high mortality and rates of readmission and increased medical expenses are becoming a problem.4, 5, 6, 7, 8, 9
In contrast, nutrition10, 11 in HF patients is a reported factor of mortality and readmission. In a report on the nutritional assessment of HF patients, the Geriatric Nutritional Risk Index (GNRI), which is measured using both serum albumin and body mass index (BMI), was shown to have excellent prognostic evaluation ability as compared with the measurement of serum albumin or BMI alone.12, 13, 14, 15 Also, several cross‐sectional studies have shown a relation between mobility and nutrition16, 17 and between activities of daily living (ADL) and nutrition.18
However, it is not clear whether a difference in nutritional status in elderly HF patients affects ADL and motility recovery. The present study aimed to examine the effect of differences in nutritional status on ADL and mobility of elderly patients with HF.
Methods
Study design and participants
From among 377 consecutive HF patients who underwent rehabilitation at one acute‐care hospital from January 2013 to August 2015, those who were aged ≥ 65 years could walk with assistance before hospitalization and who were hospitalized for the first time were included in this retrospective cohort study. Exclusion criteria were pacemaker surgery during hospitalization, change to other departments, death during hospitalization, and unmeasured ADL. The reason for including the criterion of ‘walk with assistance before hospitalization’ is that it affects the mobility and ADL recovery of the patients during hospitalization.
In rehabilitation, if haemodynamics have been stabilized or if HF patients are not experiencing any resting symptoms, on the basis of instructions from a doctor, they can perform exercise therapy (sitting and standing exercises, walking, and aerobic exercise) and ADL training with support from physical therapists.19
Investigation
Patient characteristics and clinical parameters investigated included age; sex; BMI; blood pressure; heart rate; left ventricular ejection fraction; brain natriuretic peptide (BNP) concentration; New York Heart Association (NYHA) class; levels of creatinine, haemoglobin, and albumin; acute management; co‐morbidity; medications; initiation of rehabilitation and of walking exercise; and length of the rehabilitation period and of hospital stay.
Assessment of Geriatric Nutritional Risk Index
We evaluated the GNRI as an index of patient nutrition. Baseline GNRI was calculated from serum albumin and BMI using the following formula20: GNRI = 14.89 × serum albumin (g/dL) + 41.7 × present body weight/[(height)2 (m2) × 22] = 14.89 × serum albumin (g/dL) + 41.7 × BMI/22. The patients were then divided into two groups—the low GNRI (<92) group and high GNRI (≥92) group—on the basis of a previous study.14, 15
Assessment of activities of daily living
We evaluated ADL with the Functional Independence Measure (FIM) at hospital admission and discharge of the patients.13 The FIM was developed to assess rehabilitative aspects of patients with disabilities and consists of two domains, motor and cognitive. A supporting reference for the use of these was published in 1996.21
The motor domain (motor FIM) consists of 13 items: eating; grooming; bathing; dressing upper body; dressing lower body; toileting; bladder and bowel managements; transfer to bed, chair, or wheelchair; transfer to toilet; transfer to tub or shower; walking/wheelchair; and stairs. The cognitive domain (cognitive FIM) consists of five items: comprehension, expression, social interaction, problem solving, and memory.
The FIM is scored on a scale ranging from 1 to 7 points: one point for total assistance, two points for maximal assistance, three points for moderate assistance, four points for minimal contact assistance, five points for supervision, six points for modified independence, and seven points for complete independence. The minimum total FIM score is 18 points, and the maximum score is 126 points, whereas the minimum scores for motor FIM and cognitive FIM were 13 points and five points and the maximum scores were 91 points and 35 points, respectively. We used the motor FIM in this study.22
Assessment of Rivermead Mobility Index
The Rivermead Mobility Index (RMI) is an assessment of mobility originally published in Italy in 1991. This assessment is determined by asking 14 questions related to patient mobility (turning over in bed, lying to sitting, sitting balance, sitting to standing, transfer, walking inside with an aid if needed, climbing stairs, walking outside on even ground, walking inside with no aid, picking something off the floor, walking outside on uneven ground, bathing, walking up and down four steps, and running) and making one observation on the patient's ability to stand unsupported.23, 24 This assessment was performed twice by two physical therapists, at patient hospitalization and at discharge. Also, motor FIM and mobility at admission were evaluated on the day after hospitalization.
Statistical analysis
Patient characteristics and clinical parameters are reported using percentages for categorical variables and mean ± standard deviation for continuous variables. Unpaired t‐test and χ 2 test were used to compare patient characteristics and clinical parameters between the two GNRI groups. To analyse the difference between motor ADL and motility recovery and nutrition, two‐way analysis of covariance (ANCOVA) was used to investigate the interaction between within‐groups factor (term: admission and discharge) and between‐groups factor (group: high GNRI and low GNRI). Those factors with 5% significance in the comparison between the two groups were used as covariates. A P value < 0.05 indicated statistical significance. Statistical analyses were performed with IBM SPSS 25.0 J statistical software (IBM SPSS Japan, Inc., Tokyo, Japan).
Ethical considerations
The Kokura Rehabilitation College Institutional Review Committee on Human Research approved this study (approval number 29‐03), and informed consent was obtained from each patient.
Results
Patient flow
Participant flow in the study is shown Figure 1 . Of the 377 consecutive HF patients who underwent rehabilitation, 109 patients who met the inclusion criteria were originally included in this study. However, 13 patients were later excluded because of pacemaker surgery during hospitalization (nine patients), change to other departments (two patients), death during hospitalization (one patient), or unmeasured ADL (one patient). Therefore, 96 patients were included who were divided into the low GNRI group (n = 38) and high GNRI group (n = 58).
Figure 1.
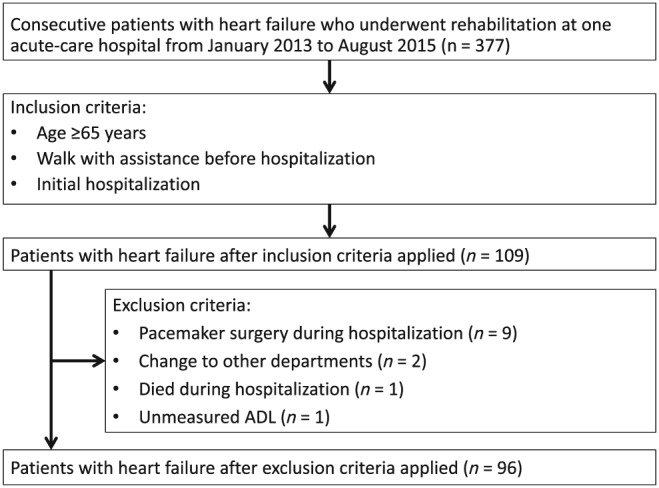
Patient flow during the study. ADL, activities of daily living.
Patient characteristics
A comparison of the clinical characteristics between the low GNRI group and high GNRI group of elderly hospitalized HF patients is shown in Table 1. There were significant differences between the two groups with regard to BMI, albumin level, diabetes mellitus (DM), RMI score, and motor FIM score at discharge (P < 0.05).
Table 1.
Patient characteristics
| Low GNRI n = 38 | High GNRI n = 58 | F or χ 2 value | P value | |
|---|---|---|---|---|
| Age, years | 83.5 ± 8.3 | 81.0 ± 6.6 | 1.71a | 0.10 |
| Sex, male, % | 44.7 | 55.2 | 1.00 | 0.32 |
| BMI at admission, kg/m2 | 18.7 ± 2.2 | 23.2 ± 2.7 | 1.47a | <0.001 |
| Clinical parameters at admission | ||||
| Systolic blood pressure, mmHg | 141.7 ± 32.1 | 146.9 ± 36.6 | 0.03a | 0.47 |
| Diastolic blood pressure, mmHg | 77.7 ± 14.9 | 82.4 ± 28.8 | 1.54a | 0.50 |
| Heart rate, beats/min | 88.8 ± 24.1 | 88.1 ± 24.7 | 0.41a | 0.89 |
| LVEF, % | 49.7 ± 15.0 | 45.4 ± 15.8 | 0.29a | 0.19 |
| BNP level, pg/mL | 1045.6 ± 761.7 | 803.0 ± 600.4 | 4.54a | 0.10 |
| NYHA class I/II/III/IV, % | 2.6/18.4/50.0/28.9 | 1.7/19.0/43.1/36.2 | 0.70 | 0.874 |
| Creatinine level, mg/dL | 1.3 ± 0.9 | 1.3 ± 1.1 | 0.04 | 0.83 |
| eGFR, mL/min/1.73 m2 | 45.2 ± 21.2 | 49.5 ± 19.3 | 0.61a | 0.31 |
| Haemoglobin level, g/dL | 11.0 ± 2.4 | 12.0 ± 2.5 | 0.04a | 0.06 |
| Albumin level, g/dL | 3.4 ± 0.4 | 3.8 ± 0.4 | 0.51a | <0.001 |
| GNRI | 86.0 ± 5.9 | 101.2 ± 7.4 | 1.35a | <0.001 |
| Acute management, % | 23.7 | 27.6 | 0.18 | 0.67 |
| Co‐morbidity at admission, % | ||||
| Hypertension | 97.4 | 87.9 | 2.68 | 0.10 |
| DM | 21.1 | 50.0 | 8.12 | 0.004 |
| Ischaemic heart disease | 39.5 | 55.2 | 2.26 | 0.13 |
| Valvular disease | 50.0 | 34.5 | 2.29 | 0.13 |
| Atrial fibrillation | 23.7 | 43.1 | 3.79 | 0.052 |
| Orthopaedic disease | 42.1 | 39.7 | 0.06 | 0.81 |
| Neurological disease | 15.8 | 25.9 | 1.36 | 0.24 |
| Respiratory disease | 31.6 | 15.5 | 3.47 | 0.06 |
| Medications at admission | ||||
| Diuretic | 100.0 | 93.1 | 2.74 | 0.10 |
| Beta‐blockers | 63.2 | 79.3 | 3.03 | 0.08 |
| ACEI/ARB | 73.7 | 60.3 | 1.81 | 0.18 |
| Rehabilitation progress | ||||
| Initiation of walking exercise, days | 8.4 ± 8.2 | 6.4 ± 4.8 | 5.31a | 0.18 |
| Rehabilitation start, days | 2.2 ± 3.0 | 2.6 ± 2.7 | 0.52a | 0.50 |
| Length of hospital stay, days | 22.2 ± 11.0 | 19.8 ± 7.0 | 4.08a | 0.25 |
| Rehabilitation period, days | 19.9 ± 11.3 | 17.2 ± 6.4 | 6.29a | 0.13 |
| RMI score on admission | 2.6 ± 1.7 | 2.5 ± 2.1 | 1.50a | 0.81 |
| RMI score at discharge | 6.8 ± 2.6 | 8.2 ± 2.2 | <0.01a | 0.01 |
| Motor FIM score on admission | 33.1 ± 16.4 | 36.5 ± 15.6 | 0.15a | 0.31 |
| Motor FIM score at discharge | 67.2 ± 19.5 | 75.6 ± 13.3 | 4.87a | 0.02 |
Values are presented as mean ± standard deviation or %.
ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; BMI, body mass index; BNP, brain natriuretic peptide; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; FIM, Functional Independence Measurement; GNRI, Geriatric Nutritional Risk Index; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; RMI, Rivermead Mobility Index.
F value.
Mobility and activities of daily living
The results of two‐way ANCOVA showed a significant group and term main effect and interaction effect for the RMI score (P < 0.05), indicating that nutrition had an effect on mobility recovery. There was no significant interaction effect for the motor FIM score. There was also a significant main effect of group and term (P < 0.05) (Table 2), which showed that nutrition did not affect ADL recovery.
Table 2.
Two‐way analysis of covariancea
| Mean square | F value | P value | |
|---|---|---|---|
| RMI | |||
| Term | 1146.7 | 246.1 | <0.001 |
| GNRI group | 19.1 | 4.1 | 0.04 |
| Interaction | 30.4 | 6.5 | 0.01 |
| Motor FIM | |||
| Term | 61486.1 | 252.3 | <0.001 |
| GNRI group | 1669.7 | 6.8 | <0.001 |
| Interaction | 347.5 | 1.4 | 0.23 |
FIM, Functional Independence Measure; GNRI, Geriatric Nutritional Risk Index; RMI, Rivermead Mobility Index.
Adjusted for diabetes mellitus.
Discussion
This is the first study, to our knowledge, to report that the nutritional status of elderly hospitalized HF patients is related to the recovery of mobility. The results showed that recovery of mobility in the low GNRI group was poor in comparison with that in the high GNRI group of elderly inpatients with HF.
Characteristics of the low Geriatric Nutritional Risk Index group of elderly heart failure patients
Compared with the low GNRI group, the high GNRI group had a higher BMI and higher DM ratio. In the elderly, high BMI is a known risk factor for developing diabetes.25 In a previous study, characteristics of a high co‐morbidity rate of DM were shown to be related to malnutrition in patients with HF.26 Therefore, in the patients with HF and a high GNRI in this study, the co‐morbidity rate of DM may also be high.
However, there was no significant difference in severity of HF between the two groups. A previous study showed a relationship between nutritional status and severity in HF.25 We set ‘walk with assistance’ and ‘hospitalized for the first time’ as inclusion criteria in the present study. It was reported that ADL and NYHA in HF patients were correlated.27 There is a relation between cardiovascular disease history and the severity of risk factors in HF.28 In the present study, it appeared that nutritional status did not reflect severity because it was possible that owing to inclusion criteria that we chose, not so many cases of severe HF were included.
Recovery of mobility and activities of daily living
Mobility of the elderly HF patients in the low GNRI group was low at discharge, and this finding has been reported as a potential prognostic indicator for frailty and malnutrition.16, 17 The decline in mobility at discharge in the present study supports the findings of these previous studies.16, 17 We also found that nutritional status was related to the recovery of mobility in the hospitalized patients. HF patients and community‐dwelling elderly with malnutrition are known to have decreased muscle mass,29, 30 and decreased mobility was shown to be associated with the reduced muscle mass of HF patients.31 It was also reported that elderly people require more protein than do younger adults, that the reduction in protein associated with malnutrition may reduce muscle mass,32 and that the combination of protein intake and exercise therapy increases the muscle mass of elderly people.33 Therefore, in the present study, we surmise that the HF patients in low GNRI group may have had a poor recovery of mobility from exercise therapy. Also, the results suggested that the evaluation of muscle mass related to mobility and the necessity for nutrition intervention were necessary. However, it was also possible that HF patients with cachexia were included in the low GNRI group.34 The effect of exercise therapy on cachexia is not known.35 Mobility in the HF patients with cachexia in the low GNRI group may have been poor because it is difficult to obtain positive effects of exercise therapy in these patients.
Activities of daily living at discharge was low in the HF patients in the low GNRI group. This supports the findings of a previous study.18 However, nutritional status did not show any apparent effects on the recovery of ADL. A previous study showed that each ADL varies in difficulty.36 For example, the difficulty and physical load of performing self‐care such as grooming, bathing, and dressing are low, whereas they are high when performing transfer actions and locomotion. ADL associated with the high loads of locomotion and transfer may be difficult to recover owing to malnutrition. In addition, because locomotion and transfer are just one part of the total FIM score, we considered that the influence of nutrition on the ADL index of the FIM to be small. In high and low GNRI groups in the future, it will be necessary to investigate ADL items with different rates of recovery and to determine which ADL items are difficult to recover through rehabilitation. It is possible that ADL was evaluated as being low owing to the ceiling effect of the FIM evaluation. For a more accurate evaluation of ADL recovery, we may need to select more sensitive indicators of ADL and to investigate the physical functions associated with ADL. Longitudinal studies that include nutritional interventions will be necessary in the future to evaluate the effects of malnutrition on the recovery of mobility and ADL in hospitalized elderly HF patients.
Strengths
As result of two‐way ANCOVA using the factors of nutrition and mobility, low nutritional status as evaluated by the GNRI was a factor related to recovery of mobility in elderly HF patients. This finding suggests that improvement of nutrition during hospitalization may be important in improving patient mobility at discharge.
Limitations
This study was conducted at a single facility and with a small sample size. Primarily, the patients were in their 80s, thus making it difficult to report findings for patients in their 70s or 90s. Also, we did not consider difference in the sexes. We also did not investigate physical function (muscle strength, handgrip, skin fold thickness, and gait speed) as related to ADL and mobility before or during hospitalization, nor did we evaluate the nutrition index at discharge, and ADL after discharge. These need to be considered in a future study.
Conclusions
We showed that low nutritional status affected the recovery of mobility in elderly hospitalized HF patients but that it might not affect the recovery of ADL. These findings suggest the need for muscle mass measurement and nutritional intervention studies.
Conflict of interest
None declared.
Funding
This work was supported by JSPS KAKENHI (grant number JP17K01500) and by the MEXT‐Supported Program for the Strategic Research Foundation at Private Universities, 2015–19, the Japan Ministry of Education, Culture, Sports, Science and Technology (grant number S1511017) to K.O. Neither the authors nor their associated institutions report any financial relationships with industry relevant to this study.
Acknowledgements
This study benefitted from the support and encouragement of Masashi Kanai, Masato Ogawa, Koudai Ishihara, Asami Ogura, Daisuke Nakamura, Takayuki Shimogai, Ikkou Kubo, Yuji Kanejima, and Hiroto Ogi, all of Kobe University Graduate School of Health Sciences. We also thank Hiroki Taniue, Department of Rehabilitation, Kenwakai Otemachi Hospital, for investigative support in the present study.
Kitamura M., Izawa K. P., Yaekura M., Mimura Y., Nagashima H., and Oka K. (2019) Differences in nutritional status and activities of daily living and mobility in elderly hospitalized patients with heart failure, ESC Heart Failure, 6, 344–350. 10.1002/ehf2.12393.
All work was performed in the Department of Rehabilitation, Shinyukuhashi Hospital, Yukuhashi, Japan.
References
- 1. World Health Organization . World Health Statistics 2018. http://www.who.int/gho/publications/world_health_statistics/en/ (1 August 2018). [Google Scholar]
- 2. Cabinet Office Japan . Annual Report on the Aging Society: 2017—Section 1 Situation on Aging. http://www8.cao.go.jp/kourei/english/annualreport/2017/pdf/c1‐1.pdf (1 August 2018). [Google Scholar]
- 3. Santulli G, Ciccarelli M, Trimarco B, Iaccarino G. Physical activity ameliorates cardiovascular health in elderly subjects: the functional role of the β adrenergic system. Front Physiol 2013; 124: 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ministry of Health, Labour and Welfare Japan . Vital Statistics—Trends in Leading Causes of Death. https://www.mhlw.go.jp/english/database/db‐hw/populate/dl/03.pdf (1 August 2018). [Google Scholar]
- 5. Yasuda S, Nakao K, Nishimura K, Miyamoto Y, Sumita Y, Shishido T, Shishido T, Anzai T, Tsutsui H, Ito H, Komuro I, Saito Y, Ogawa H, on the behalf of JROAD . The current status of cardiovascular medicine in Japan—analysis of a large number of health records from a nationwide claim‐based database, JROAD‐DPC. Circ J 2016; 80: 2327–2335. [DOI] [PubMed] [Google Scholar]
- 6. Roger VL, Go AS, Lloyd‐Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie‐Rosett J, American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123: e18–e209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kannel WB, Belanger AJ. Epidemiology of heart failure. Am Heart J 1991; 121: 951–957. [DOI] [PubMed] [Google Scholar]
- 8. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006; 355: 251–259. [DOI] [PubMed] [Google Scholar]
- 9. Santulli G, Iaccarino G. Adrenergic signaling in heart failure and cardiovascular aging. Maturitas 2016; 93: 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tsutsui H, Tsuchihashi‐Makaya M, Kinugawa S, Goto D, Takeshita A, JCARE‐CARD Investigators . Clinical characteristics and outcome of hospitalized patients with heart failure in Japan. Circ J 2006; 70: 1617–1623. [DOI] [PubMed] [Google Scholar]
- 11. Agra Bermejo RM, González Ferreiro R, Varela Román A, Gómez Otero I, Kreidieh O, Conde Sabarís P, Rodríguez‐Mañero M, Moure González M, Seoane Blanco A, Virgós Lamela A, García Castelo A, González Juanatey JR. Nutritional status is related to heart failure severity and hospital readmissions in acute heart failure. Int J Cardiol 2017; 230: 108–114. [DOI] [PubMed] [Google Scholar]
- 12. Jones CH, Smye SW, Newstead CG, Will EJ, Davison AM. Extracellular fluid volume determined by bioelectric impedance and serum albumin in CAPD patients. Nephrol Dial Transplant 1998; 13: 393–397. [DOI] [PubMed] [Google Scholar]
- 13. Aziz EF, Javed F, Pratap B, Musat D, Nader A, Pulimi S, Alivar CL, Herzog E, Kukin ML. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: an ACAP‐HF data analysis. Heart Int 2011; 6: e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Narumi T, Arimoto T, Funayama A, Kadowaki S, Otaki Y, Nishiyama S, Takahashi H, Shishido T, Miyashita T, Miyamoto T, Watanabe T, Kubota I. Prognostic importance of objective nutritional indexes in patients with chronic heart failure. J Cardiol 2013; 5: 307–313. [DOI] [PubMed] [Google Scholar]
- 15. Yoshihisa A, Kanno Y, Watanabe S, Yokokawa T, Abe S, Miyata M, Sato T, Suzuki S, Oikawa M, Kobayashi A, Yamaki T, Kunii H, Nakazato K, Suzuki H, Ishida T, Takeishi Y. Impact of nutritional indices on mortality in patients with heart failure. Open Heart 2018; 1: e000730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Izawa KP, Watanabe S, Oka K, Mogamiya T, Tada M, Nakata S, Nitobe S, Yoshizawa K, Hirano Y, Osada N, Omiya K, Shimizu H. Differences in physical performance based on the Geriatric Nutritional Risk Index in elderly female cardiac patients. Aging Clin Exp Res 2015; 27: 195–200. [DOI] [PubMed] [Google Scholar]
- 17. Izawa KP, Watanabe S, Oka K. Relationship of thresholds of physical performance to nutritional status in older hospitalized male cardiac patients. Geriatr Gerontol Int 2015; 15: 189–195. [DOI] [PubMed] [Google Scholar]
- 18. Kinugasa Y, Kato M, Sugihara S, Hirai M, Yamada K, Yanagihara K. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ J 2013; 77: 705–711. [DOI] [PubMed] [Google Scholar]
- 19. JCS Joint Working Group . Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012). Circ J 2014; 78: 2022–2093. [DOI] [PubMed] [Google Scholar]
- 20. Yamada K, Furuya R, Takita T, Maruyama Y, Yamaguchi Y, Ohkawa S, Kumagai H. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr 2008; 87: 106–113. [DOI] [PubMed] [Google Scholar]
- 21. Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the Functional Independence Measure: a quantitative review. Arch Phys Med Rehabil 1996; 77: 1226–1232. [DOI] [PubMed] [Google Scholar]
- 22. Kitamura M, Izawa KP, Taniue H, Mimura Y, Imamura K, Nagashima H, Brubaker PH. Relationship between activities of daily living and readmission within 90 days in hospitalized elderly patients with heart failure. Biomed Res Int 2017; 2017: 7420738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Collen FM, Wade DT, Robb GF, Bradshaw CM. The Rivermead Mobility Index: a further development of the Rivermead Motor Assessment. Int Disabil Stud 1991; 13: 50–54. [DOI] [PubMed] [Google Scholar]
- 24. Scimia F, Casadei I, Cerquetani E, Piccoli M, Villa A, La Carrubba S, Salustri A. Functional evaluation of ultra‐octogenarian patients undergoing cardiac rehabilitation: correlation between six minute walking test and Rivermead mobility index [in Italian]. Monaldi Arch Chest Dis 2010; 74: 159–163. [DOI] [PubMed] [Google Scholar]
- 25. Gray N, Picone G, Sloan F, Yashkin A. Relation between BMI and diabetes mellitus and its complications among US older adults. South Med J 2015; 1: 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sze S, Zhang J, Pellicori P, Morgan D, Hoye A, Clark AL. Prognostic value of simple frailty and malnutrition screening tools in patients with acute heart failure due to left ventricular systolic dysfunction. Clin Res Cardiol 2017; 106: 533–541. [DOI] [PubMed] [Google Scholar]
- 27. Norberg EB, Boman K, Löfgren B. Activities of daily living for old persons in primary health care with chronic heart failure. Scand J Caring Sci 2008; 22: 203–210. [DOI] [PubMed] [Google Scholar]
- 28. O'Connor M, Murtaugh CM, Shah S, Barrón‐Vaya Y, Bowles KH, Peng TR, Zhu CW, Feldman PH. Patient characteristics predicting readmission among individuals hospitalized for heart failure. Med Care Res Rev 2016; 73: 3–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gao L, Jiang J, Yang M, Hao Q, Luo L, Dong B. Prevalence of sarcopenia and associated factors in Chinese community‐dwelling elderly: comparison between rural and urban areas. J Am Med Dir Assoc 2015; 16: 1003,e1–e6. [DOI] [PubMed] [Google Scholar]
- 30. Htun NC, Ishikawa‐Takata K, Kuroda A, Tanaka T, Kikutani T, Obuchi SP, Hirano H, Iijima K. Screening for malnutrition in community dwelling older Japanese: preliminary development and evaluation of the Japanese Nutritional Risk Screening Tool (NRST). J Nutr Health Aging 2016; 20: 114–120. [DOI] [PubMed] [Google Scholar]
- 31. Coats AJ, Clark AL, Piepoli M, Volterrani M, Poole‐Wilson PA. Symptoms and quality of life in heart failure: the muscle hypothesis. Br Heart J 1994; 72: S36–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy‐Westphal A, Cederholm T, Cruz‐Jentoft A, Krznariç Z, Nair KS, Singer P, Teta D, Tipton K, Calder PC. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 2014; 33: 929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tieland M, Dirks ML, van der Zwaluw N, Verdijk LB, van de Rest O, de Groot LC, van Loon LJ. Protein supplementation increases muscle mass gain during prolonged resistance‐type exercise training in frail elderly people: a randomized, double‐blind, placebo‐controlled trial. J Am Med Dir Assoc 2012; 13: 713–719. [DOI] [PubMed] [Google Scholar]
- 34. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016; 18: 891–975. [DOI] [PubMed] [Google Scholar]
- 35. von Haehling S, Anker SD. Treatment of cachexia: an overview of recent developments. J Am Med Dir Assoc 2014; 15: 866–872. [DOI] [PubMed] [Google Scholar]
- 36. Dunlay SM, Manemann SM, Chamberlain AM, Cheville AL, Jiang R, Weston SA, Roger VL. Activities of daily living and outcomes in heart failure. Circ Heart Fail 2015; 8: 261–267. [DOI] [PMC free article] [PubMed] [Google Scholar]


