Abstract
Background
Approximately one-half of all US surgical procedures, and one-third of orthopaedic procedures, are performed at teaching hospitals. However, the effect of resident participation and their level of training on patient care for TKA postoperative physical function, operative time, length of stay, and facility discharge are unclear.
Questions/purposes
(1) Are resident participation, postgraduate year (PGY) training level, and number of residents associated with absolute postoperative Patient-Reported Outcomes Measurement Information System (PROMIS®-10) global physical function score (PCS), and achieving minimum clinically important difference (MCID) PCS improvement, after TKA? (2) Are resident participation, PGY, and number of residents associated with increased TKA operative time? (3) Are resident participation, PGY, and number of residents associated with increased length of stay after TKA? (4) Are resident participation, PGY, and number of residents associated with higher odds of patients being discharged to another inpatient facility, rather than to their home (facility discharge)?
Methods
We performed a retrospective study using a longitudinally maintained institutional registry of TKAs that included 1626 patients at a single tertiary academic institution from April 2011 through July 2016. All patients who underwent primary, elective unilateral TKA were included with no exclusions. All patients were included in the operative time, length of stay, and facility discharge models. The PCS model required postoperative PCS score (n = 1417; 87%; mean, 46.4; SD, 8.5) and the MCID PCS model required pre- and postoperative PCS (n = 1333; 82%; 55% achieved MCID). Resident participation was defined as named residents being present in the operating room and documented in the operative notes, and resident PGY level was determined by the date of TKA and its duration since the resident entered the program and using the standard resident academic calendar (July – June). Multivariable regression was used to assess PCS scores, operative time, length of stay, and facility discharge in patients whose surgery was performed with and without intraoperative resident participation, accounting for PGY training level and number of residents. We defined the MCID PCS score improvement as 5 points on a 100-point scale. Adjusting variables included surgeon, academic year, age, sex, race–ethnicity, Charlson Comorbidity Index, preoperative PCS, and patient-reported mental function, BMI, tobacco use, alcohol use, and postoperative PCS time for the PCS models. We had postoperative PCS for 1417 (87%) surgeries.
Results
Compared with attending-only TKAs (5% of procedures), no postgraduate year or number of residents was associated with either postoperative PCS or MCID PCS improvement (PCS: PGY-1 = -0.98, 95% CI, -6.14 to 4.17, p = 0.708; PGY-2 = -0.26, 95% CI, -2.01to 1.49, p = 0.768; PGY-3 = -0.32, 95% CI, -2.16 to 1.51, p = 0.730; PGY-4 = -0.28, 95% CI, -1.99 to 1.43, p = 0.746; PGY-5 = -0.47, 95% CI, -2.13 to 1.18, p = 0.575; two residents = 0.28, 95% CI, -1.05 to 1.62, p = 0.677) (MCID PCS: PGY-1 = odds ratio [OR], 0.30, 95% CI, 0.07–1.30, p = 0.108; PGY-2 = OR, 0.86, 95% CI, 0.46–1.62, p = 0.641; PGY-3 = OR, 0.97, 95% CI, 0.49–1.89, p = 0.921; PGY-4 = OR, 0.73, 95% CI, 0.39–1.36, p = 0.325; PGY-5 = OR, 0.71, 95% CI, 0.39–1.29, p = 0.259; two residents = OR, 1.23, 95% CI, 0.80–1.89, p = 0.337). Longer operative times were associated with all PGY levels except for PGY-5 (attending surgeon only [reference] = 85.60 minutes, SD, 14.5 minutes; PGY-1 = 100. 13 minutes, SD, 21.22 minutes, +8.44 minutes, p = 0.015; PGY-2 = 103.40 minutes, SD, 23.01 minutes, +11.63 minutes, p < 0.001; PGY-3 = 97.82 minutes, SD, 18.24 minutes, +9.68 minutes, p < 0.001; PGY-4 = 96.39 minutes, SD, 18.94 minutes, +4.19 minutes, p = 0.011; PGY-5 = 88.91 minutes, SD, 19.81 minutes, -0.29 minutes, p = 0.853) or the presence of multiple residents (+4.39 minutes, p = 0.024). There were no associations with length of stay (PGY-1 = +0.04 days, 95% CI, -0.63 to 0.71 days, p = 0.912; PGY-2 = -0.08 days, 95% CI, -0.48 to 0.33 days, p = 0.711; PGY-3 = -0.29 days, 95% CI, -0.66 to 0.09 days, p = 0.131; PGY-4 = -0.30 days, 95% CI, -0.69 to 0.08 days, p = 0.120; PGY-5 = -0.28 days, 95% CI, -0.66 to 0.10 days, p = 0.145; two residents = -0.12 days, 95% CI, -0.29 to 0.06 days, p = 0.196) or facility discharge (PGY-1 = OR, 1.03, 95% CI, 0.26–4.08, p = 0.970; PGY-2 = OR, 0.61, 95% CI, 0.31–1.20, p = 0.154; PGY-3 = OR, 0.98, 95% CI, 0.48–2.02, p = 0.964; PGY-4 = OR, 0.83, 95% CI, 0.43–1.57, p = 0.599; PGY-5 = OR, 0.7, 95% CI, 0.41–1.40, p = 0.372; two residents = OR, 0.93, 95% CI, 0.56–1.54, p = 0.766) for any PGY or number of residents.
Conclusions
Our findings should help assure patients, residents, physicians, insurers, and hospital administrators that resident participation, after adjusting for numerous patient and clinical factors, does not have any association with key medical and financial metrics, including postoperative PCS, MCID PCS, length of stay, and facility discharge. Future research in this field should focus on whether residents affect knee-specific patient-reported outcomes such as the Knee Injury and Osteoarthritis Score and additional orthopaedic procedures, and determine how resident medical education can be further enhanced without compromising patient care and safety.
Level of Evidence Level III, therapeutic study.
Introduction
Orthopaedic surgery residency programs have the primary responsibility of providing safe, efficacious patient care while encouraging operative procedural training of residents. Orthopaedic surgical residents in the United States aim to generally increase individual competence and independence as their training progresses. Because teaching hospitals, which perform approximately half of all surgeries and a third of all orthopaedic surgeries, strive to balance this educational mission while providing the highest quality patient care, it is important that robust research evaluates the relationship between resident participation and postgraduate year (PGY) training level and any adverse effect of this participation on quality of surgical care [31]. Studies disagree regarding whether resident participation in orthopaedic surgery increases the risk of harm to patients or has any association with patient improvements in pain and function [11, 18-20, 26, 30, 31]. Previous evidence suggested that resident participation in spinal fusion surgeries was associated with increased complications, length of stay (LOS), operative time, and blood transfusion [18-20, 30]. Conversely, a report using the National Surgical Quality Improvement Program (NSQIP) database found a decrease in perioperative complications and mortality in all orthopaedic procedures with resident assistance [11]. TKA and THA may be particularly important to evaluate, because a large-series study showed greater odds for 30-day postoperative complications with resident participation, whereas a higher risk for complications was not found after other orthopaedic procedures [31]. These findings indicated that resident seniority may be associated with LOS, operative time, and postoperative morbidity [26]. However, only short-term complications were evaluated in these studies.
Patient-reported outcomes (PROs) assess patient health status directly from the patient’s perspective [36]. The use of PROs dates to the 1980s and has been increasingly reported in research [12, 35]. Traditional hospital-based clinical metrics such as mortality and hospital readmission rates reveal low prevalence measures and may not offer sufficient sensitivity to discern variations for low-risk procedures such as TKA [5]. Integration of these standardized surveys in clinical practice provides a mechanism for monitoring longitudinal changes in symptom severity and patient function, aiding the evaluation of surgical findings [3]. Currently, there is no evidence of which we are aware regarding associations between intraoperative orthopaedic resident participation and postoperative PRO physical function in TKA.
The purpose of our study was to examine the effects of resident participation and their training level on postoperative outcomes among patients undergoing unilateral TKA, including patient-reported physical function. Specifically, we asked: (1) Are resident participation, PGY training level, and number of residents associated with absolute postoperative Patient-Reported Outcomes Measurement Information System (PROMIS®-10) global physical function score (PCS), and achieving minimum clinically important difference (MCID) PCS improvement, after TKA? (2) Are resident participation, PGY, and number of residents associated with increased TKA operative time? (3) Are resident participation, PGY, and number of residents associated with increased TKA LOS? (4) Are resident participation, PGY, and number of residents associated with higher odds of patients being discharged to another inpatient facility, rather than to their home (facility discharge)?
Patients and Methods
We performed an institutional review board-approved study of all patients who underwent unilateral primary TKA from April 2011 through July 2016 at our tertiary academic rural institution in the northeastern United States. Our study received expedited approval with waived consent. All data for this retrospective study were obtained from our longitudinally maintained institutional orthopaedic data repository.
A total of 1626 unilateral primary TKAs were available for analysis from April 2011 through July 2016 (Table 1).
Table 1.
Variable counts
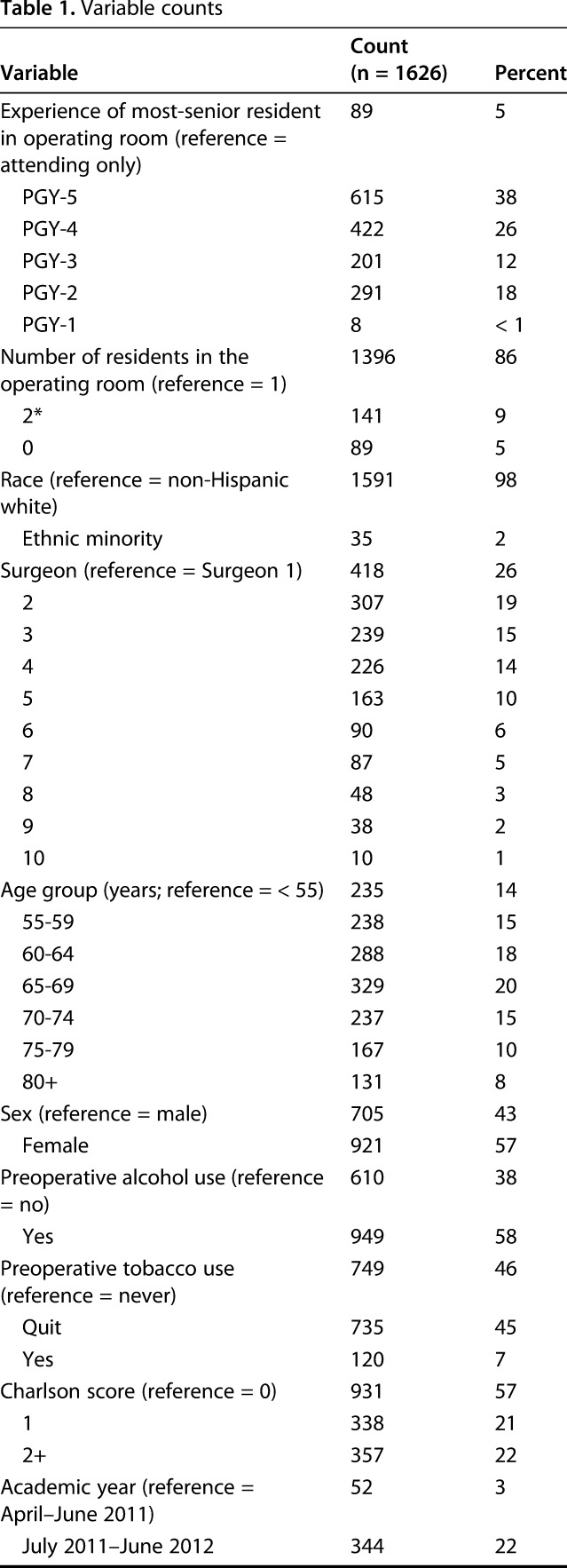
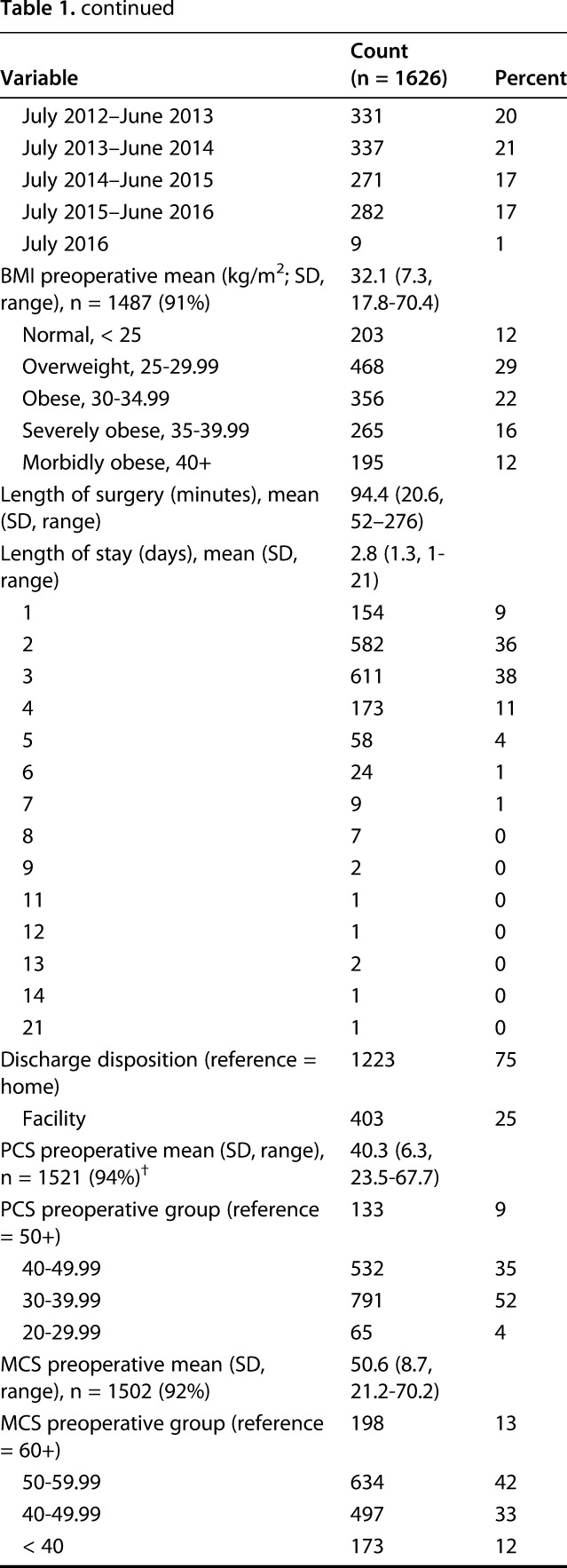
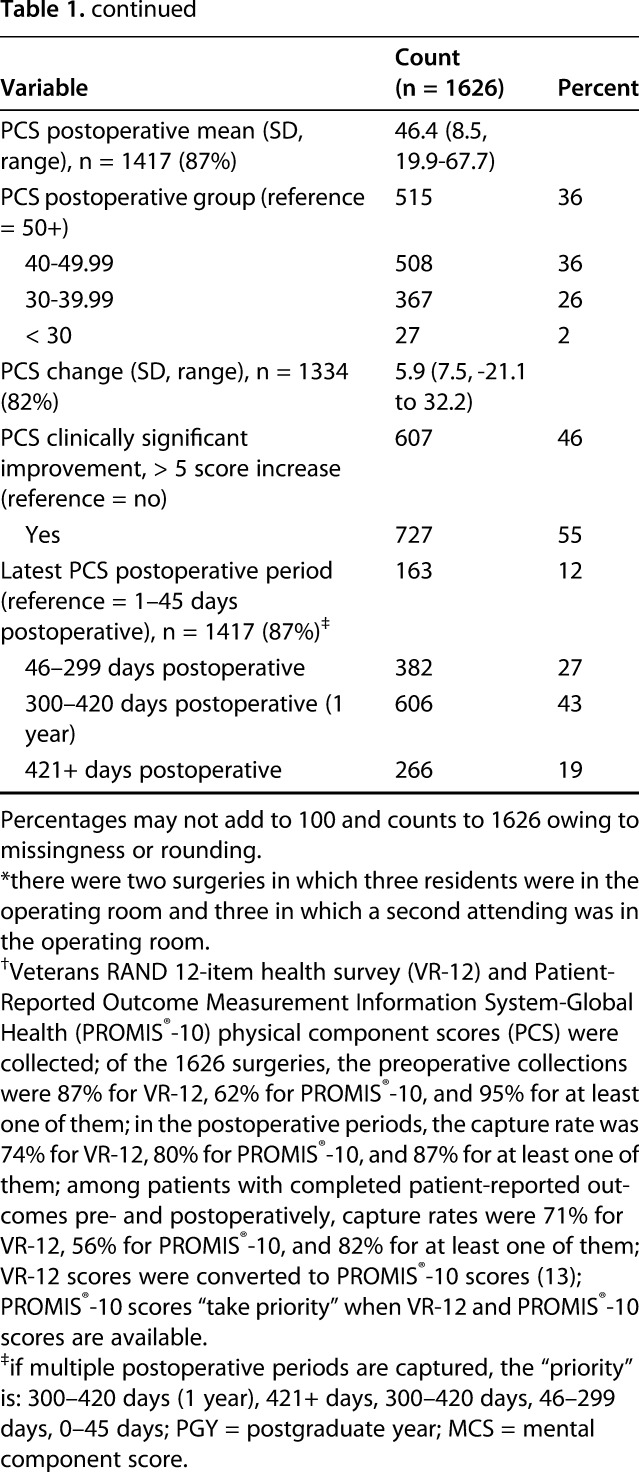
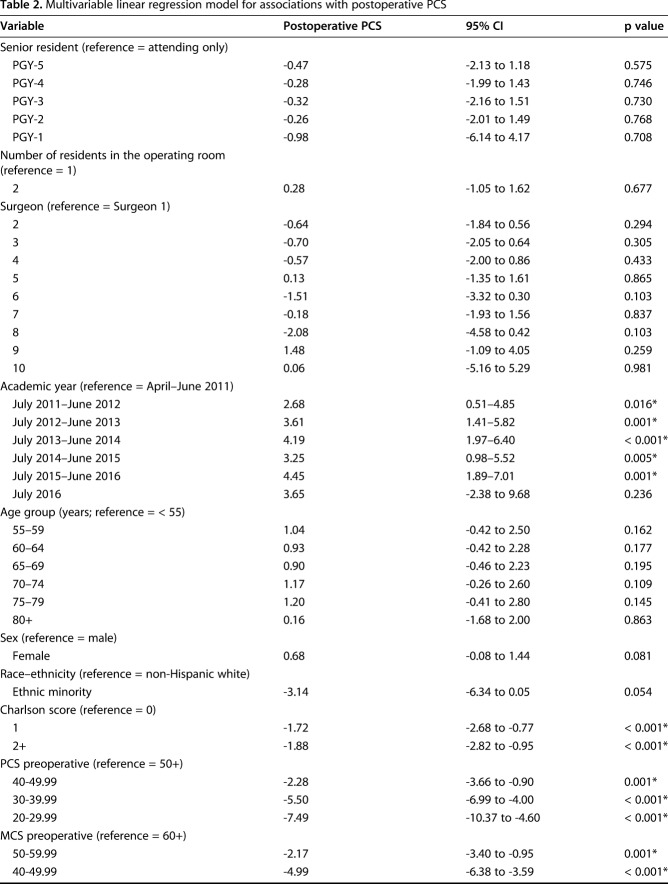
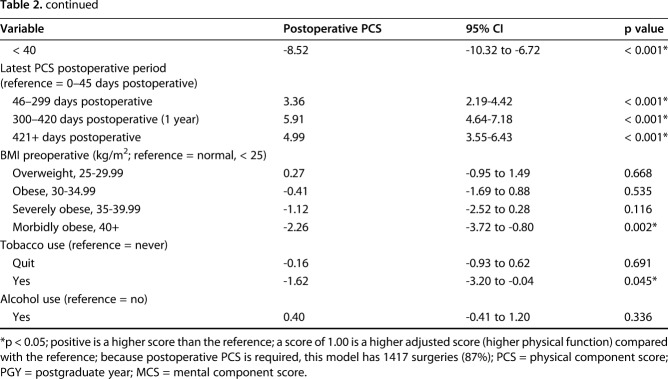
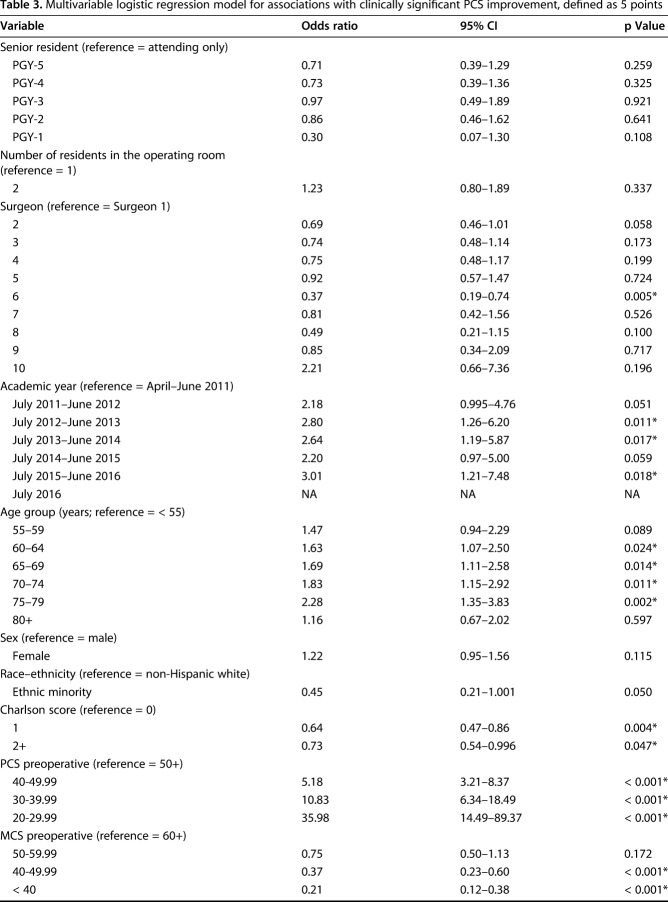
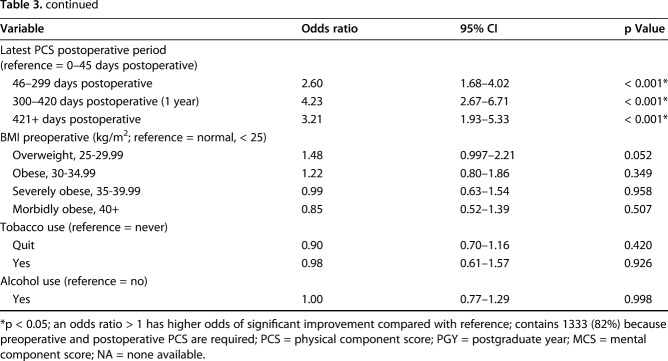
We excluded bilateral TKAs (n = 531) because our database did not record the extent of resident participation for each knee and repeat primary TKA on the contralateral knee (n = 151). Because the PCS postoperative model requires postoperative PCS and the MCID PCS change model requires pre- and postoperative PCS, those models include 1417 (87%) (Table 2) and 1333 (82%) (Table 3) TKAs, respectively. Among the postoperative PCS scores, 43% were captured at approximately 1-year postoperative (defined as 10–14 months, or 300–420 days), 19% after 1 year (421+ days), 27% between 46 to 299 days postoperative (between our department’s standard 1-month and 1-year followups), and 12% at the patient’s first followup (between 1 and 45 days postoperative) (Table 1). This period is included as an adjusting variable in the PCS models (Tables 2 and 3). There were some preoperative differences between patients who did or did not have a postoperative PCS, including surgeon (p = 0.009); alcohol use (62% of patients with postoperative PCS drank alcohol versus 50% of patients with no postoperative PCS, p = 0.003); Charlson Comorbidity Index (46% versus 21% with at least one comorbidity, p < 0.001); resident year (p < 0.001); PCS (40.6 [SD, 6.3] versus 38.2 [SD, 5.6], p < 0.001); and mental component score (MCS) (50.9 [SD, 8.7] versus 48.3 [SD, 8.7], p < 0.001) (data not shown). All of these factors were adjusting variables in our multivariable statistical models. There were no differences by postoperative PCS capture rates by resident PGY, number of residents, race, age, sex, tobacco use, and BMI (data not shown).
Table 2.
Multivariable linear regression model for associations with postoperative PCS
Table 3.
Multivariable logistic regression model for associations with clinically significant PCS improvement, defined as 5 points
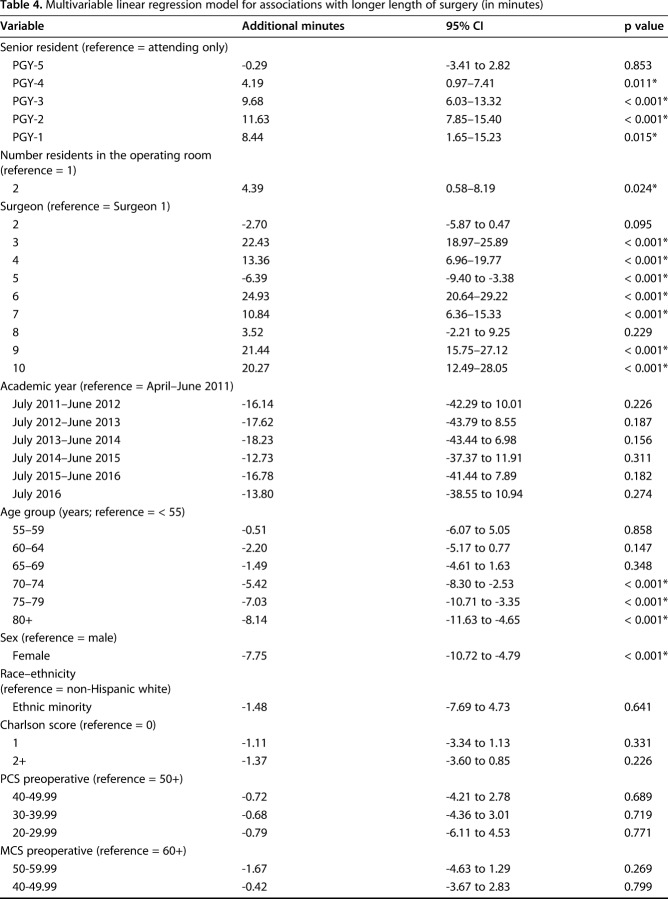
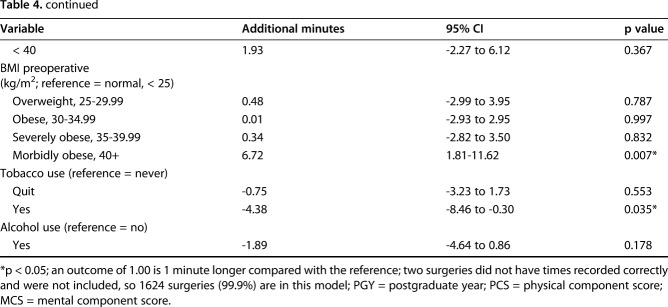
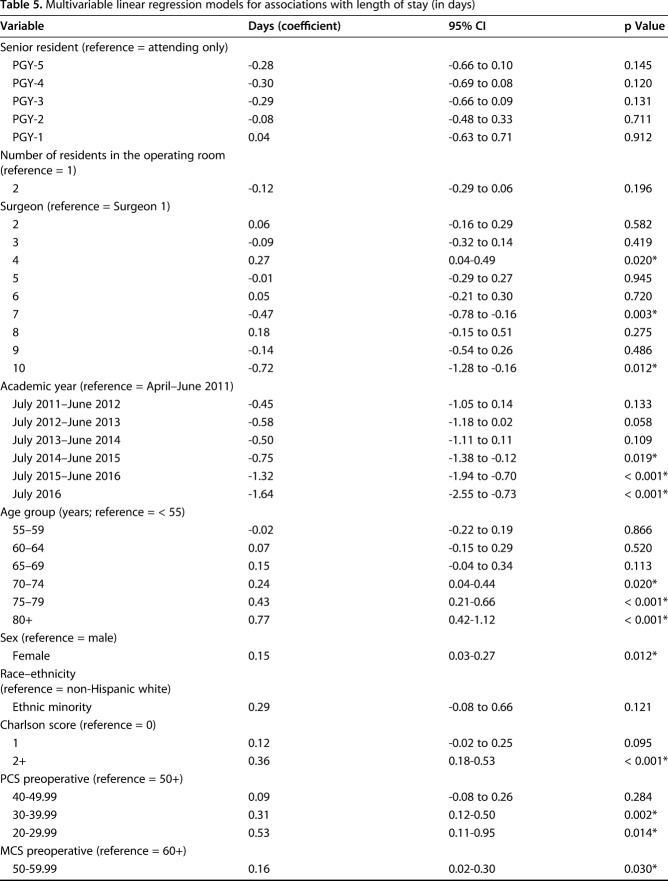
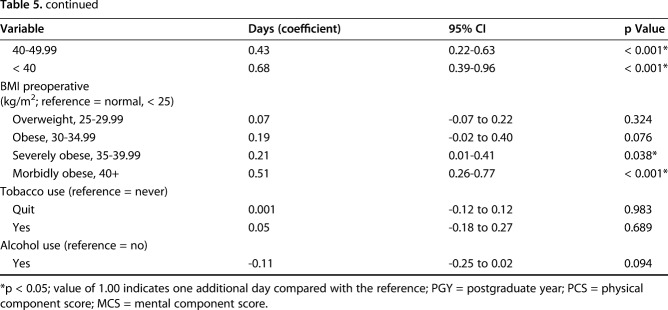
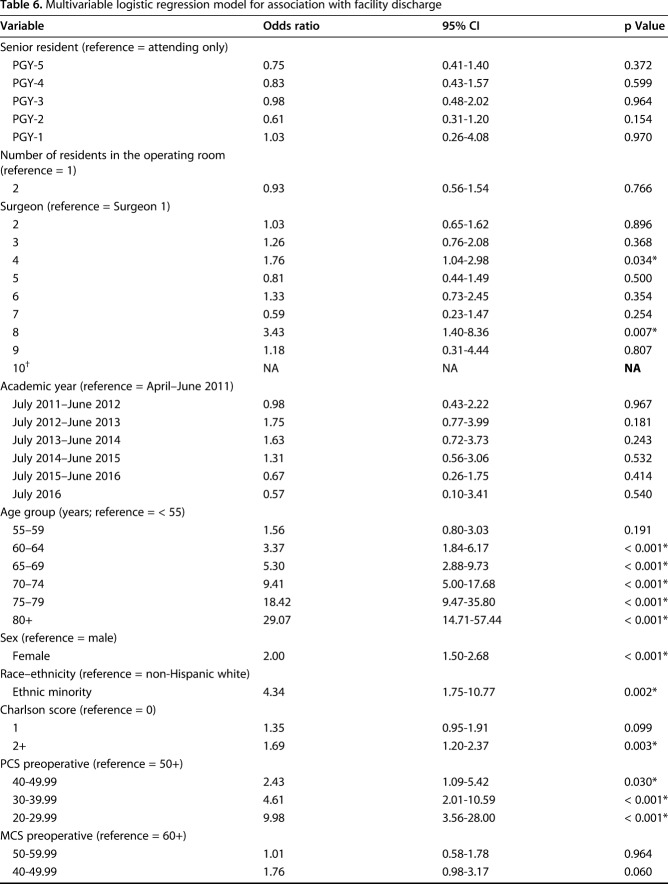
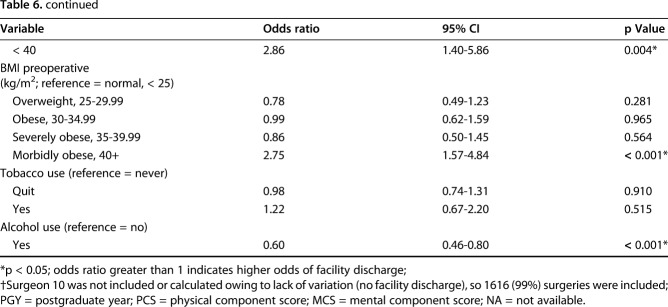
Other outcomes had minor exclusions. Two (0.1%) patients are not included in the operative time model owing to incorrect capture of recorded times in the electronic medical record (Table 4). All patients are included in the LOS model (Table 5). Ten (0.6%) patients were not included in the facility discharge because their surgeon, who had a low-volume of TKAs, did not have any variation in the model (all 10 were discharged to home) and therefore could not be calculated (Table 6).
Table 4.
Multivariable linear regression model for associations with longer length of surgery (in minutes)
Table 5.
Multivariable linear regression models for associations with length of stay (in days)
Table 6.
Multivariable logistic regression model for association with facility discharge
Residents present during the TKA were identified in individual chart reviews and their PGY level was based on the date of surgery compared with their entry in the resident program (Table 1). TKAs were performed by 10 orthopaedic attending surgeons with or without the assistance of residents. Orthopaedic surgery residents present during surgery represent all levels of training from PGY-1 to -5. In cases in which multiple residents were present (n = 141; 9%), the more-senior resident was assumed to be the first assistant. During the study period, there were 37 orthopaedic surgery residents at our institution. Intraoperative complications were documented in four cases (three tibia fractures and one medial collateral ligament injury), but the intraoperative complication rate was too low to discern any relationship to year of training or resident participation and these were not explored further.
All model variables were recorded preoperatively and obtained from our longitudinally maintained institutional repository (Table 1). Our primary variables were the PGY level of the senior resident (with a reference category of “attending surgeon only”) and the number of residents present in the operating room. Adjusting factors included age [23, 28, 38], sex [23, 28, 38], race–ethnicity (non-Hispanic white versus ethnic minority) [13, 14], surgeon [28], alcohol use [21], tobacco use [21, 34], Charlson Comorbidity score [28], academic year (July-June), clinically recorded BMI [8, 28], PCS [28, 32, 33], and MCS [16]. Our models included postoperative PCS and a conservative MCID PCS improvement of 5 points or greater [4, 15, 33], operative time, LOS, and facility discharge. We used the established, standardized PROMIS-10 and Veterans RAND 12-item health survey to determine PCS and MCS with time. We collected both, sometimes concurrently, during the study period, prioritizing the PROMIS-10. If PROMIS-10 scores were not available, the Veterans RAND-12 PCS and MCS were converted to the PROMIS-10 scale using a recent validated crosswalk [29]. Operative time was defined as the elapsed minutes from the initiation of skin incision to completed wound closure. LOS was captured in days. Discharge disposition was dichotomized in home versus facility [28]. There were no changes in pre- and postoperative protocols during the study period.
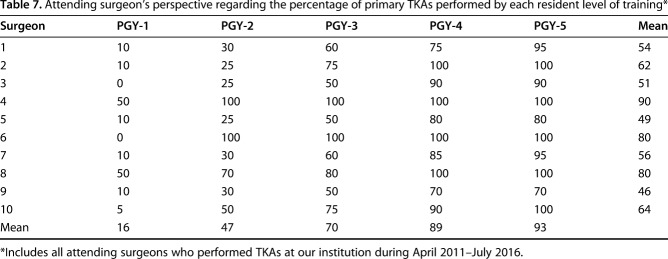
There were no differences in patient demographics by resident participation. Residents assisted in 95% of cases, including 9% of total cases in which at least two residents were involved. Although it was impossible to quantify the exact percentage of resident involvement in any given case, we polled all of our attending surgeons performing TKAs during the study period (April 2011 – July 2016) to gain a sense of graduated resident involvement as they progressed through residency (Table 7). PGY-5 residents had the most-frequent senior training level present in the operating room (38%) compared with PGY-4 (26%), PGY-3 (12%), PGY-2 (18%), and PGY-1 (< 1%). The mean age for our patient sample was 65.5 years (SD, 10.1 years), with a mean preoperative PCS of 40.3 (SD, 6.3) and MCS of 50.6 (SD, 8.7). Fifty-seven percent of patients were female and 98% were classified as white, which reflects the local older population [25]. Although there was a mean MCID-achieved PCS improvement (5.89 score improvement, SD, 7.50), 46% did not achieve MCID PCS improvement of 5 points or greater (Table 1) and 16% had lower PCS scores postoperatively (data not shown).
Table 7.
Attending surgeon’s perspective regarding the percentage of primary TKAs performed by each resident level of training*
We collected additional postoperative data that are not reflected in the analytic models (Table 1). The PCS change score was measured as the latest available postoperative recorded PCS subtracted by the latest preoperative score; a positive change score indicates PCS improvement. The period captured by the postoperative PCS was included in the PCS change models. We also documented any additional all-cause same-knee surgery (“reoperations”) within 90 days of the primary TKA.
Statistical Analysis
We used multivariable regression techniques for all analytic models and robust standard errors to account for the observational study. Linear regression was used for the postoperative PCS, length of surgery, and LOS models, whereas dichotomous logistic regression was used for determining the MCID PCS improvement and discharge status. Because all surgeries were done at one tertiary academic institution, and all second primary TKAs were excluded, there were no repeat patients and no clustering. Statistical significance was set at a probability less than 0.05. All analyses used Stata 12 MPTM (StataCorp, College Station, TX, USA).
Results
After accounting for other factors like BMI, surgeon, and preoperative PCS, resident PGY level and number of residents were not associated with postoperative PCS (Table 2). Compared with attending-only TKAs, no PGY had different postoperative PCS (PGY-5: -0.47 points, 95% CI, -2.13 to 1.18, p = 0.575; PGY-4: -0.28 points, 95% CI, -1.99 to 1.43, p = 0.746; PGY-3: -0.32 points, 95% CI, -2.16 to 1.51, p = 0.730; PGY-2: -0.26 points, 95% CI, -2.01 to 1.49, p = 0.768; PGY-1: -0.98 points, 95% CI, -6.14 to 4.17, p = 0.708). No differences were found for postoperative PCS between having two residents compared with one (0.28 points, 95% CI, -1.05 to 1.62; p = 0.677).
There also were no associations between resident PGY level and number of residents and the likelihood of achieving an equal or greater improvement than the MCID for PCS improvement (Table 3). Compared with attending-only TKAs, no PGY had different postoperative MCID PCS improvement (PGY-5: odds ratio [OR] of MCID improvement, 0.71, 95% CI, 0.39–1.29, p = 0.259; PGY-4: OR, 0.73, 95% CI, 0.39–1.36, p = 0.325; PGY-3: OR, 0.97, 95% CI, 0.49–1.89, p = 0.921; PGY-2: OR, 0.86, 95% CI, 0.46–1.62, p = 0.641; PGY-1: OR, 0.30, 95% CI, 0.07–1.30, p = 0.108). Additionally, no difference was found by having multiple residents in the operating room compared with one (OR, 1.23, 95% CI, 0.80–1.89, p = 0.337).
All PGY training levels except for the PGY-5 group were associated with longer operative times compared with mean attending-only surgery of 86 minutes (SD, 15 minutes) (PGY-1 = +8.44 minutes, 95% CI, 1.65–15.23 minutes, p = 0.015; PGY-2 = +11.63 minutes, 95% CI, 7.85–15.40, p < 0.001; PGY-3 = +9.68 minutes, 95% CI, 6.03–13.32, p < 0.001; PGY-4 = +4.19 minutes, 95% CI, 0.97–7.41, p = 0.011; PGY-5 = -0.29 minutes, 95% CI, -3.41 to 2.82, p = 0.853), as was participation of more than one resident during surgery (+4.39 minutes, 95% CI, 0.58–8.19, p = 0.024, compared with one resident) (Table 4). However, there was greater variation in operative time among individual attending orthopaedic surgeons (range, -6.39 to 24.93 minutes, compared with Surgeon 1). Older patients and female sex were associated with shorter operative times.
No difference in hospital LOS was found between different levels of resident training or the presence of two residents (Table 5) (PGY-5: -0.28 days, 95% CI, -0.66 to 0.10 days, p = 0.145; PGY-4: -0.30, 95% CI, -0.69 to 0.08, p = 0.120; PGY-3: -0.29, 95% CI, -0.66 to 0.09, p = 0.131; PGY-2: -0.08, 95% CI -0.48 to 0.33, p = 0.711; PGY-1: 0.04, 95% CI, -0.63 to 0.71, p = 0.912). Older patients and female patients were associated with longer LOS as were higher Charlson Comorbidity Index and BMI and lower preoperative PCS and MCS.
Similarly, no difference in odds of facility discharge, defined as discharge to anywhere but the patient’s home [28], was found among different levels of resident training or the presence of two residents (Table 6) (PGY-5: OR, 0.75 of facility discharge compared with attending-only TKA, 95% CI, 0.41–1.40, p = 0.372; PGY-4: OR, 0.83, 95% CI, 0.43–1.57, p = 0.599; PGY-3: OR, 0.98, 95% CI, 0.48–2.02, p = 0.964; PGY-2: OR, 0.61, 95% CI, 0.31–1.20, p = 0.154; PGY-1: OR, 1.03, 95% CI, 0.26–4.08, p = 0.970). In an adjusted multivariable model, older patients, female patients, higher Charlson Comorbidity Index, higher BMI, lower PCS, and lower MCS were all associated with facility discharge.
Using the data repository and patient charts, we identified 11 known cases of a patient returned to the operating room for a knee-specific additional surgery within 90 days of the primary unilateral TKA (0.7%). These 11 cases included four infections, two cases of hemarthrosis, one case of avascular necrosis, a wound dehiscence with likely patellar tendon injury, dehiscence of the incision, revision to correct patellar subluxation, and revision for instability and clunk. There was no discernible pattern for individual residents or PGY level and we did not have the counts to investigate reoperations further. In the attending-only group, there were no cases of intraoperative complications or additional 90-day knee-specific surgery.
Discussion
Although approximately one-third of all orthopaedic procedures in the United States are performed at teaching hospitals, the effect of resident participation and their level of training on patient care for TKA outcomes is currently unclear [31]. We investigated this clinical question using PROs, operative time, LOS, and facility discharge as adjunctive measures to the current knowledge of clinical metrics and postoperative mortality data. Previous studies examining the intraoperative effects of residents have largely analyzed them as a homogenous unit without accounting for level of training [11, 18-20, 30, 31]. To further elucidate the role of resident participation in orthopaedic surgery, we examined the effects of resident experience according to PGY level. We examined the relationships between resident year of training and its effects on PROs, operative time, LOS, and discharge disposition in 1626 patients who underwent primary TKA. In this study, no associations were found between the training level of orthopaedic surgery residents and PROs assessed when compared with surgery without resident participation after applying numerous adjusting variables.
This study has numerous limitations. First, although we had complete or more than 99% inclusion rates for our operative time, LOS, and facility discharge outcomes, we had significant missingness for postoperative PCS in our unfunded pragmatic study. However, these capture rates are quite good in a pragmatic unfunded observational dataset and are similar to the funded American Joint Replacement, Function and Outcomes Research for Comparative Effectiveness in Total Joint Replacement, and California Joint Replacement registries [2, 15]. Those missing postoperative PCS differed in some ways. These differences might be explained in additional analyses outside the scope of the current study. For example, later years such as 2015 and 2016 may have lower followup rates because less time has passed, particularly for followups at least 1 year after the TKA (our analyses and followup dates go through July 2016); patients with higher Charlson Comorbidity Index scores may be more likely to have more clinical visits and thus more opportunities to record PCS; and some surgeons were in the dataset only during earlier years before capturing scores were more emphasized in our department. However, our data allow for inclusion of variables rarely available in previous studies, such as physical and mental function and clinic-measured BMI, and we statistically adjusted for the time in which postoperative PCS was captured. Second, it was not possible to determine the degree of involvement each resident had during surgery, and it may have varied by surgeon and other operating room and logistic factors that could not be measured or controlled. Additionally, we queried all 10 of the surgeons in our dataset regarding the degree of resident involvement they typically encouraged and found, as expected, graduated responsibility mirrored resident training level (Table 7). There also might be variations in resident skill level, confidence, and perceived difficulty and complexity of the case. Additionally, although we presented a large study cohort that drew data from a longitudinally maintained institutional registry, our patients were not randomly assigned and were from a single institution in a rural area. Although the geographic area does not have much racial and ethnic diversity, it presents much diversity for other socioeconomic status measures, including employment, education, income, and living alone status [15, 28]. Finally, although we attempted to adjust for patient differences using multivariable analyses, there were potentially other factors not captured by our database that may affect a pragmatic dataset. For example, we did not capture measures of case complexity beyond Charlson Comorbidity Index and BMI: measures such as Current Procedural Terminology codes and Relative Value Units may show additional complexities of the TKA that might affect resident participation [26].
Intraoperative participation of orthopaedic surgery residents and their PGY level were not associated with changes in long-term physical function, as measured by either postoperative PCS change or MCID PCS improvement of 5 points or greater [4, 15, 33]. These findings may speak to the ability of a residency program to uphold its educational mission toward residents of all training levels without compromising patient care. To our knowledge, this is the first study to evaluate resident involvement with postoperative PRO PCS; other published studies investigated only short-term clinical measures of intraoperative resident participation, with varying conclusions [11, 18-20, 26, 30, 31, 39]. The goals of most patients undergoing TKA and other orthopaedic procedures are pain relief and improved physical function; therefore we propose PROs as an equally important metric in evaluating resident-related surgical measures. Interestingly, and in agreement with previous studies [15, 28], we showed that patients with the lowest preoperative PCS reported the greatest PCS improvement from TKA, whereas those with the lowest preoperative MCS reported the least clinical benefit. Moreover, in our patients undergoing TKA, the presence of multiple residents in the operating room was not associated with a difference in postoperative PROs. Although not a focus of our research questions, it is interesting that no attending-only TKA had an intraoperative complication or an additional 90-day knee-specific surgery in our unilateral TKA dataset. However, the small sample size of this group renders any comparisons challenging.
Among the models we examined, intraoperative resident participation had the greatest effect on operative duration. Consistent with previous reports on spinal surgery and minimally invasive THA, TKAs with resident participation were associated with longer operative times [19, 20, 39]. In our resident sublevel analysis, compared with cases without a resident, all PGY levels (except PGY-5) and cases with multiple residents had longer operative times. Longer durations of surgery may be a result of resident inexperience and/or time devoted to teaching by the attending surgeon. From PGYs-2 to -5, there was a steady decline in the duration of surgery, which is supported by previous studies that increasing experience is linked to shorter operative times in orthopaedic procedures [6, 40]. Shorter lengths of surgery also may be related to a greater observational role and minimal hands-on operating experience for PGY-1 residents, whereas orthopaedic trainees participate in greater procedural roles starting at PGY-2 at our institution, as self-reported by our attending surgeons (Table 7). Longer operative times potentially can lead to an increased risk of infection, postoperative transfusion, readmissions, and reoperations in total joint arthroplasties, but the significance of the addition of a mean 11.6 minutes, after adjustment for other factors, in the longest group (PGY-2) is unclear (Table 4) [10,17, 25, 27]. However, individual attending surgeons were associated with much greater variations in operative duration compared with resident training level, even after adjustment for resident and patient characteristics. Our results are in contrast with the NSQIP primary knee and hip arthroplasty population reported by Pugely et al. [26], which showed that operative times were not affected by resident PGY level, despite having the same definition of operative time as we used, although their findings were inconsistent between different orthopaedic procedures. This topic has been explored more extensively in general surgery procedures with controversial results [1, 7, 9, 22, 24, 37].
As supported in other studies, we did not find any differences in LOS based on resident participation [7, 22, 24, 37]. However, Pugely et al. [26] reported increasing durations of hospital stay with higher PGY levels. Our study and data differ in numerous ways from their work. Pugely et al. [26] used the NSQIP dataset and had access to multicenter claims data; however, they did not capture several key variables that are available in our electronic medical records data, including Charlson Comorbidity Index, preoperative PCS and MCS, and individual surgeon. Additionally, we used individual PGYs while Pugely et al. dichotomized residents into “junior” and “senior” residents, and also included fellows [26]. Their findings also were inconsistent among different orthopaedic procedures assessed.
We also found no differences in odds of facility discharge between residents at various training levels participating in surgery. Other studies have noted no differences in similar 30-day outcomes [7, 22, 24, 37].
Although largely confirmatory, our study is notable for several reasons. We have postoperative PCS as an outcome and a preoperative adjusting variable, which, to the best of our knowledge, has not been used previously for resident participation study for TKAs, although it has become increasingly important to payers and the government. We provide contrasting evidence regarding any association resident participation may have on operative times, complications, and LOS [26]. Further study should attempt to have the counts of previous claims studies while including electronic medical records and PRO variables similar to our study.
Our findings should serve to assuage concerns from patients, surgeons, residents, and hospital administrators regarding resident participation in TKAs. Despite modestly longer operative times with junior residents, there were no differences in physical function, LOS, or discharge disposition among patients undergoing primary unilateral TKA with surgical participation of residents at any training level. The effect of intraoperative resident participation in orthopaedic surgeries on long-term patient function and additional surgeries would benefit from further investigation with the intention of improving resident education without compromising patient care.
Acknowledgments
We thank Robin L. Hemingway (Department of Orthopaedics, Dartmouth-Hitchcock Medical Center) for assistance in performing chart reviews.
Footnotes
One of the authors (BJK) has received funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (P60-AR048094 and P60-AR062799).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA.
References
- 1.Advani V, Ahad S, Gonczy C, Markwell S, Hassan I. Does resident involvement effect surgical times and complication rates during laparoscopic appendectomy for uncomplicated appendicitis? An analysis of 16,849 cases from the ACS-NSQIP. Am J Surg. 2012;203:347–351. [DOI] [PubMed] [Google Scholar]
- 2.Ayers DC, Franklin PD. Joint replacement registries in the United States: a new paradigm. J Bone Joint Surg Am. 2014;96:1567–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayers DC, Zheng H, Franklin PD. Integrating patient-reported outcomes into orthopaedic clinical practice: proof of concept from FORCE-TJR. Clin Orthop Relat Res. 2013;471:3419–3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ. Can preoperative patient-reported outcome measures be used to predict meaningful improvement in function after TKA? Clin Orthop Relat Res. 2017;475:149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birkmeyer JD, Dimick JB, Birkmeyer NJ. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg. 2004;198:626–632. [DOI] [PubMed] [Google Scholar]
- 6.Bjorgul K, Novicoff WM, Saleh KJ. Learning curves in hip fracture surgery. Int Orthop. 2011;35:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatterjee A, Pyfer B, Chen L, Czerniecki B, Tchou J, Fisher C. Resident and fellow participation in breast surgery: an American College of Surgeons NSQIP clinical outcomes analysis. J Am Coll Surg. 2015;221:988–994. [DOI] [PubMed] [Google Scholar]
- 8.D’Apuzzo MR, Novicoff WM, Browne JA. The John Insall Award: Morbid obesity independently impacts complications, mortality, and resource use after TKA. Clin Orthop Relat Res. 2015;473:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis SS, Jr, Husain FA, Lin E, Nandipati KC, Perez S, Sweeney JF. Resident participation in index laparoscopic general surgical cases: impact of the learning environment on surgical outcomes. J Am Coll Surg. 2013;216:96–104. [DOI] [PubMed] [Google Scholar]
- 10.Duchman KR, Pugely AJ, Martin CT, Gao Y, Bedard NA, Callaghan JJ. Operative time affects short-term complications in total joint arthroplasty. J Arthroplasty. 2017;32:1285–1291. [DOI] [PubMed] [Google Scholar]
- 11.Edelstein AI, Lovecchio FC, Saha S, Hsu WK, Kim JY. Impact of resident involvement on orthopaedic surgery outcomes: an analysis of 30,628 patients from the American College of Surgeons National Surgical Quality Improvement Program Database. J Bone Joint Surg Am. 2014;96:e131. [DOI] [PubMed] [Google Scholar]
- 12.Gartland JJ. Orthopaedic clinical research: deficiencies in experimental design and determinations of outcome. J Bone Joint Surg Am. 1988;70:1357–1364. [PubMed] [Google Scholar]
- 13.Goodman SM, Mandl LA, Parks ML, Zhang M, McHugh KR, Lee YY, Nguyen JT, Russell LA, Bogardus MH, Figgie MP, Bass AR. Disparities in TKA outcomes: census tract data show interactions between race and poverty. Clin Orthop Relat Res. 2016;474:1986–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katz JN. Persistence of racial and ethnic differences in utilization and adverse outcomes of total joint replacement. J Bone Joint Surg Am. 2016;98:1241–1242. [DOI] [PubMed] [Google Scholar]
- 15.Keeney BJ, Koenig KM, Paddock NG, Moschetti WE, Sparks MB, Jevsevar DS. Do aggregate socioeconomic status factors predict outcomes for total knee arthroplasty in a rural population? J Arthroplasty. 2017;32(12):3583–3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khatib Y, Madan A, Naylor JM, Harris IA. Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthop Relat Res. 2015;473:2630–2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS, Jr, Stock MC, Gust MJ, Mahvi DM. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015;150:110–117. [DOI] [PubMed] [Google Scholar]
- 18.Kim RB, Garcia RM, Smith ZA, Dahdaleh NS. Impact of resident participation on outcomes after single-level anterior cervical diskectomy and fusion: an analysis of 3265 patients from the American College of Surgeons National Surgical Quality Improvement Program database. Spine (Phila Pa 1976). 2016;41:E289–296. [DOI] [PubMed] [Google Scholar]
- 19.Kothari P, Lee NJ, Lakomkin N, Leven DM, Shin JI, Guzman JZ, Skovrlj B, Steinberger J, Cho SK. Impact of resident involvement on morbidity in adult patients undergoing fusion for spinal deformity. Spine (Phila Pa 1976). 2016;41:1296–1302. [DOI] [PubMed] [Google Scholar]
- 20.Lee NJ, Kothari P, Kim C, Leven DM, Skovrlj B, Guzman JZ, Steinberger J, Cho SK. The impact of resident involvement in elective posterior cervical fusion. Spine (Phila Pa 1976). 2016. Feb 1. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 21.Maradit Kremers H, Kremers WK, Berry DJ, Lewallen DG. Social and behavioral factors in total knee and hip arthroplasty. J Arthroplasty. 2015;30:1852–1854. [DOI] [PubMed] [Google Scholar]
- 22.McMillan DT, Viera AJ, Matthews J, Raynor MC, Woods ME, Pruthi RS, Wallen EM, Nielsen ME, Smith AB. Resident involvement and experience do not affect perioperative complications following robotic prostatectomy. World J Urol. 2015;33:793–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ong PH, Pua YH. A prediction model for length of stay after total and unicompartmental knee replacement. Bone Joint J. 2013;95:1490–1496. [DOI] [PubMed] [Google Scholar]
- 24.Papandria D, Rhee D, Ortega G, Zhang Y, Gorgy A, Makary MA, Abdullah F. Assessing trainee impact on operative time for common general surgical procedures in ACS-NSQIP. J Surg Educ. 2012;69:149–155. [DOI] [PubMed] [Google Scholar]
- 25.Peersman G, Laskin R, Davis J, Peterson MG, Richart T. Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS J. 2006;2:70–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pugely AJ, Gao Y, Martin CT, Callaghan JJ, Weinstein SL, Marsh JL. The effect of resident participation on short-term outcomes after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:2290–2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844–850. [DOI] [PubMed] [Google Scholar]
- 28.Rissman CM, Keeney BJ, Ercolano EM, Koenig KM. Predictors of facility discharge, range of motion, and patient-reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis. J Arthroplasty. 2016;31:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schalet BD, Rothrock NE, Hays RD, Kazis LE, Cook KF, Rutsohn JP, Cella D. Linking physical and mental health summary scores from the Veterans RAND 12-Item Health Survey (VR-12) to the PROMIS(R) Global Health scale. J Gen Intern Med. 2015;30:1524–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoenfeld AJ, Carey PA, Cleveland AW, 3rd, Bader JO, Bono CM. Patient factors, comorbidities, and surgical characteristics that increase mortality and complication risk after spinal arthrodesis: a prognostic study based on 5,887 patients. Spine J. 2013;13:1171–1179. [DOI] [PubMed] [Google Scholar]
- 31.Schoenfeld AJ, Serrano JA, Waterman BR, Bader JO, Belmont PJ., Jr The impact of resident involvement on post-operative morbidity and mortality following orthopaedic procedures: a study of 43,343 cases. Arch Orthop Trauma Surg. 2013;133:1483–1491. [DOI] [PubMed] [Google Scholar]
- 32.Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, Kazis LE. Updated U.S. population standard for the Veterans RAND 12-Item Health Survey (VR-12). Qual Life Res. 2009;18:43–52. [DOI] [PubMed] [Google Scholar]
- 33.SooHoo NF, Li Z, Chenok KE, Bozic KJ. Responsiveness of patient reported outcome measures in total joint arthroplasty patients. J Arthroplasty. 2015;30:176–191. [DOI] [PubMed] [Google Scholar]
- 34.Sørensen LT. Wound healing and infection in surgery: the clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg. 2012;147:373–383. [DOI] [PubMed] [Google Scholar]
- 35.Tarlov AR, Ware JE, Jr, Greenfield S, Nelson EC, Perrin E, Zubkoff M. The medical outcomes study: an application of methods for monitoring the results of medical care. JAMA. 1989;262:925–930. [DOI] [PubMed] [Google Scholar]
- 36.U.S. Food and Drug Administration. Guidance for Industry: Patient Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. Available at: https://www.fda.gov/downloads/drugs/guidances/ucm193282.pdf. Accessed September 11, 2017.
- 37.Venkat R, Valdivia PL, Guerrero MA. Resident participation and postoperative outcomes in adrenal surgery. J Surg Res. 2014;190:559–564. [DOI] [PubMed] [Google Scholar]
- 38.Weaver F, Hynes D, Hopkinson W, Wixson R, Khuri S, Daley J, Henderson WG. Preoperative risks and outcomes of hip and knee arthroplasty in the Veterans Health Administration. J Arthroplasty. 2003;18:693–708. [DOI] [PubMed] [Google Scholar]
- 39.Weber M, Benditz A, Woerner M, Weber D, Grifka J, Renkawitz T. Trainee surgeons affect operative time but not outcome in minimally invasive total hip arthroplasty. Sci Rep. 2017;7:6152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Witjes S, Smolders JM, Beaulé PE, Pasker P, Van Susante JL. Learning from the learning curve in total hip resurfacing: a radiographic analysis. Arch Orthop Trauma Surg. 2009;129:1293–1299. [DOI] [PubMed] [Google Scholar]