Abstract
Background
Surgical treatment for shoulder instability generally involves labral repair with a capsular plication or imbrication. Good results are reported in both open and arthroscopic procedures, but there is no consensus on the amount or location of capsular plication that is needed to achieve stability and anatomic anterior, posterior, and inferior translation of the joint.
Questions/purposes
(1) What are the separate and combined effects of increasing plication magnitude and sequential additive plications in the anterior, posterior, and inferior locations of the joint capsule on glenohumeral joint translation in the anterior, posterior, and inferior directions? (2) What plication location and magnitude restores anterior, posterior, and inferior translation to a baseline level?
Methods
Fourteen cadaveric shoulders were dissected down to the glenohumeral capsule and underwent instrumented biomechanical testing. Each shoulder was loaded with 22 N in anterior, posterior, and inferior directions at 60° abduction and neutral rotation and flexion and the resulting translation were recorded. Testing was done over baseline (native), stretched (mechanically stretched capsule to imitate a lax capsule), and 5-mm, 10-mm, and 15-mm plication conditions. Individually, for each of the 5-, 10-, and 15-mm increments, plications were done in a fixed sequential order starting with anterior plication at the 3 o’clock position (Sequence I), then adding posterior plication at the 9 o’clock position (Sequence II), and then adding inferior plication at the 6 o’clock position (Sequence III). Each individual sequence was tested by placing 44 N (10 pounds) of manual force on the humerus directed in an anterior, posterior, and inferior direction to simulate clinical load and shift testing. The effect of plication magnitude and sequence on translation was tested with generalized estimating equation models. Translational differences between conditions were tested with paired t-tests.
Results
Translational laxity was highest with creation of the lax condition, as expected. Increasing plication magnitude had a significant effect on all three directions of translation. Plication location sequence had a significant effect on anterior and posterior translation. An interaction effect between plication magnitude and sequence was significant in anterior and posterior translation. Laxity in all directions was most restricted with 15-mm plication in anterior, posterior, and inferior locations. For anterior translational laxity, at 10-mm and 15-mm plication, there was a progressive decrease in translation magnitude (10-mm plication anterior only: 0.46 mm, plus posterior: 0.29 mm, plus inferior, -0.12 mm; and for 15-mm anterior only: -0.53 mm, plus posterior: -1.00 mm, plus inferior: -1.66 mm). For posterior translational laxity, 10-mm and 15-mm plication also showed progressive decrease in magnitude (10-mm plication anterior only: 0.46 mm, plus posterior: -0.25 mm, plus inferior: -1.94; and for 15-mm anterior only: 0.14 mm, plus posterior: -1.54 mm, plus inferior: -3.66). For inferior translational laxity, tightening was observed only with magnitude of plication (anterior only at 5 mm: 0.31 mm, at 10 mm: -1.39, at 15 mm: -3.61) but not with additional plication points (adding posterior and inferior sequences). To restore laxity closest to baseline, 10-mm AP/inferior plication best restored anterior translation, 15-mm anterior plication best restored posterior translation, and 5 mm posterior with or without inferior plication best restored inferior translation.
Conclusions
Our results suggest that (1) a 10-mm plication in the anterior and posterior or anterior, posterior, and inferior positions may restore anterior translation closest to baseline; (2) 10-mm anterior and posterior or 15-mm anterior plications may restore posterior translation closest to baseline; and (3) 5-mm anterior and posterior or anterior, posterior, and inferior plications may restore inferior translation closest to baseline. Future studies using arthroscopic techniques for plication or open techniques via a true surgical approach might further characterize the effect of plication on glenohumeral translation.
Clinical Relevance
This study found that specific combinations of plication magnitude and location can be used to restore glenohumeral translation from a lax capsular state to a native state. This information can be used to guide surgical technique based on an individual patient’s degree and direction of capsular laxity. In vivo testing of glenohumeral translation before and after capsular plication will be needed to validate these cadaveric results.
Introduction
Glenohumeral instability is generally accompanied by injury to the labrum, capsule, and glenohumeral ligaments [1, 5, 6, 9, 10, 28, 29, 42-44]. Shoulder instability is thought to involve injury to primary and secondary stabilizers of the capsule and capsular ligaments on both sides of the joint, like in the “circle stability concept” reported by Bowen and Warren [7, 9]. In addition to superior and middle glenohumeral ligaments, the anterior and posterior bands of the inferior glenohumeral ligament are important stabilizing structures within the capsule. The anterior band is generally injured in anterior shoulder instability, but the posterior band has been shown to play an equally important role in stabilization [28]. The middle glenohumeral ligament and rotator interval have also been shown to affect the translational and rotational profile of the joint [16, 17, 21, 37, 39]. Many techniques have been developed to treat recurrent shoulder instability; some aim at addressing the labral pathology, some at the capsular/glenohumeral ligament pathology, and some at both. Initially, Neer and Foster [25] reported a humeral-based, open capsular shift technique, and later both Jobe et al. [19] and Altchek et al. [4] reported an open glenoid-based technique incorporating a labral repair.
Subsequently, arthroscopic techniques for labral repair and/or capsular plication have been reported [11, 18, 20, 23, 32, 49]. Each of these techniques has shown good results, but currently there is controversy over the style and amount of plication needed to restore physiologic rotation and translation of the glenohumeral joint [12, 13, 18, 33]. Concerns about capsule overtightening, limiting ROM, or overconstraining the glenohumeral articulation further complicate decision-making [6, 14, 39, 46]. Previous studies have attempted to quantify capsular volume reduction after plication [15, 22, 24, 31, 36, 47]. These studies show a sequential decrease in volume with plication as expected; however, the clinical correlation is difficult to interpret. Anterior translation has been the focus of studies on the effect of capsular plication, because this is the most common direction of instability [3, 35, 37-39, 45, 46]. Anteroinferior plication is shown to decrease anterior translation as expected [3, 35, 37-39, 45, 46]. However, the effect of posterior plication on anterior translation has not shown consistent results with some studies showing additive benefits on reducing anterior translation and some showing no effect [11, 14, 30, 34], and there are few studies on the evidence of the effect of anterior, posterior, or inferior plication on posterior and inferior translation [8, 26, 34]. Our goal is to add to the literature on the effect of plication in all three locations and directions of translation.
Therefore, we asked: (1) What are the separate and combined effects of increasing plication magnitude and sequential additive plications in the anterior, posterior, and inferior locations of the joint capsule on glenohumeral joint translation in the anterior, posterior, and inferior directions? (2) What plication location and magnitude restores anterior, posterior, and inferior translation to a baseline level?
Materials and Methods
A biomechanical study using cadaveric specimens was conducted. Fourteen shoulder specimens were tested with the same protocol at a single time point. Each specimen served as its own control. The specimens were procured from an anatomic donation organization (Anatomy Gifts Registry, Hanover, MD, USA) as fresh-frozen cadavers and were evaluated structurally with CT and clinically with ROM by an orthopaedic surgeon (SWM). The cohort consisted of shoulders from nine males and five females (12 white and two black) with an average age of 56 ± 11 years (range, 33–66 years).
Experimental Setup
After being fully thawed to room temperature, all pericapsular tissues were dissected from the specimens by a single experienced orthopaedic surgeon (SWM). The rotator cuff tendinous insertions were left intact to keep the capsule unviolated. The rotator interval was then loosely closed with a single suture using Vicryl® 2.0 (Ethicon Inc, Bridgewater, NJ, USA) to act as a ripstop to prevent further stretching or tearing open of the interval during the rotational and translational forces during the creation of a lax state and the subsequent testing. The capsule was then vented with an 18-gauge angiocatheter at the rotator interval to prevent a reseal suction phenomenon during testing. Retroreflective motion tracking marker clusters were rigidly attached to the humerus and scapula. Humerus and scapula bony landmarks were identified and logged in the motion analysis software with a spatial pointer with a calibrated tip. A dynamic 5-second circumduction trial was used to calculate the effective glenohumeral joint center of rotation. The trajectory and distance of movement of each marker, corresponding to the translation of the humerus on the glenoid, was recorded with a calibrated motion analysis system (Motion Analysis Corp, Santa Rosa, CA, USA) accurate to 0.2 mm.
The humerus was cut at the midshaft; the shaft was fixed in a cylindrical tube and the scapula was set in a square frame. Plaster of Paris was poured around each bone and allowed to harden. The humeral and scapular fixtures were attached to a glenohumeral laxity testing device (Fig. 1) designed to allow translational load-response testing in a variety of positions.
Fig. 1.
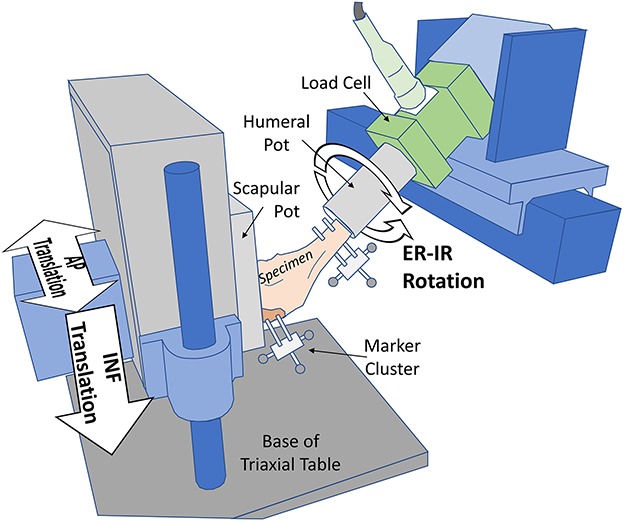
Schematic of the glenohumeral laxity device and testing degrees of freedom from the oblique view is shown. The triaxial base allowed the scapula to translationally float in three directions (only the vertical cylinder bearing is shown). The load cell was mounted in series and aligned with the anatomic humerus long axis. INF = inferior; ER-IR = external rotation–internal rotation. Reprinted from Journal of Shoulder and Elbow Surgery, Kraszewski AP, Mayer SW, Kontaxis A, Hillstrom HJ, Sheikhzadeh A, Russell P, Mapping glenohumeral laxity: effect of capsule tension and abduction in cadaveric shoulders, 2017, with permission from Elsevier.
Each shoulder underwent translational glenohumeral laxity testing in a fixed position of 60° abduction in the scapular plane with neutral axial rotation to represent a common position of load and shift testing clinically. A 44-N (10 pounds) load was applied cyclically five times along three directions (anterior, posterior, and inferior) selected randomly. The load was applied manually to the scapula potting frame with a calibrated spring scale by a single rater (APK) and the joint returned to center after each cycle.
Translational laxity tests were conducted across two experimental factors: capsule state and plication sequence. Capsule state contained five levels: baseline, stretched, 5 mm, 10 mm, and 15 mm. Plication sequence consisted of three levels (anterior; anterior and posterior; and anterior, posterior, and inferior) repeated within the last three capsule state levels (designated I, II, and III, respectively) (Fig. 2).
Fig. 2.
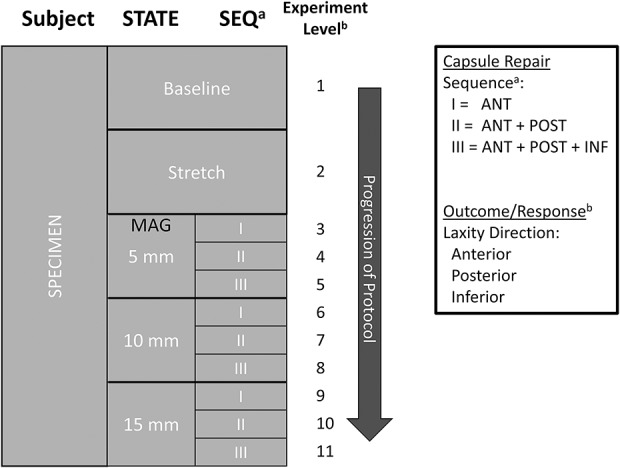
Diagram showing the experimental design and protocol. Each specimen (first column) was tested across two fixed-order within-subject conditions, STATE (second column) and SEQ (third column). The last three levels of STATE were the capsule repairs, MAG. The SEQ levels were repeated within each MAG level, and each SEQ plication was done in a fixed sequence and additively. A total of 11 experimental levels (fourth column) was tested, where the measured outcome per level was glenohumeral translation with laxity direction order randomized. The chronologic progression of testing is depicted by the dark vertical arrow. ANT = anterior; POST = posterior; INF = inferior.
Baseline served as the control condition representing the physically unaltered capsule. Preconditioning was done before testing in the baseline capsule state through 10 cycles in both internal and external rotation at 30° of abduction in the scapular plane, rotating at 5°/s-1 [41]. A complete cycle started at neutral rotation, proceeded until 1.0 N-m torque was reached, and then returned to neutral. The stretched condition was created by applying a constant 5.0-N-m torque for 30 minutes in internal and external rotation separately. The glenohumeral joint was fixed in 40° of abduction in the scapular plane and neutral flexion [3].
The last three levels of state represented conditions of plication repair with incremental magnitude. Plication sutures were first spaced 5 mm apart, then 10 mm, and lastly 15 mm. Within each magnitude level were three plication sequence levels. First was anterior suture of the capsule at the 3:00 position (Sequence I). A second level of plication posteriorly at 9:00 was added (Sequence II). Lastly, a third plication inferiorly at 6:00 was added (Sequence III). Capsular volume was taken up additively such that Sequence II included anterior and posterior plications, and Sequence III included all three plications, until starting the next magnitude level.
Plications were performed on the external capsule with the shoulder in 50° of abduction in the scapular plane and neutral rotation. In each plication region, three parallel sutures were placed starting 10 mm from the glenoid rim, proceeding laterally with 5 mm between each suture. Each plication was performed using a horizontal mattress-type suture configuration with the plication oriented north to south (superior to inferior). Magnitude and spacing were measured with a 1-mm gradation metric ruler. A single experienced orthopaedic surgeon (SWM) performed all repairs using #2 Ethibond-Extra (Ethicon Inc, Somerville, NJ, USA).
Before advancing to the next magnitude, all sutures from the previous round of testing were removed and the location of plication was planned and remeasured such that the new sutures would encompass the location of the holes from previous plications and new suture holes would be created to prevent stretching of any holes and falsely increasing capsular laxity (Fig. 3).
Fig. 3.
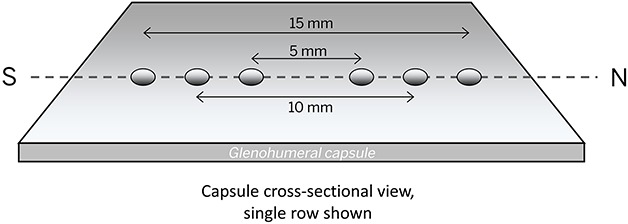
Plication suture hole spacing is shown. Shown is a cross-sectional representation of the glenohumeral capsule and suture holes of a single row. Holes are shown as small shaded circles. The holes shared a common center where previous suture holes were taken up in subsequent plications. The dotted line depicts north-to-south orientation.
Outcome Measures
Recorded marker data were verified and then imported into Visual3D™ software (C-Motion, Germantown, MD, USA) for signal processing. Marker trajectories were smoothed with a low-pass Butterworth filter using a 3.0-Hz cutoff frequency. Bony landmarks taken from CT were used to create specimen-specific scapula and humerus anatomic segment definitions (Fig. 4) [48]. Translational laxity was calculated as the displacement of the humerus center of rotation with respect to the glenoid center of rotation at 44 N force calculated in the scapular anatomic frame: anterior (+X), posterior (-X), and inferior (-Y). Laxity values from the last three cycles of each trial were averaged for analysis.
Fig. 4.
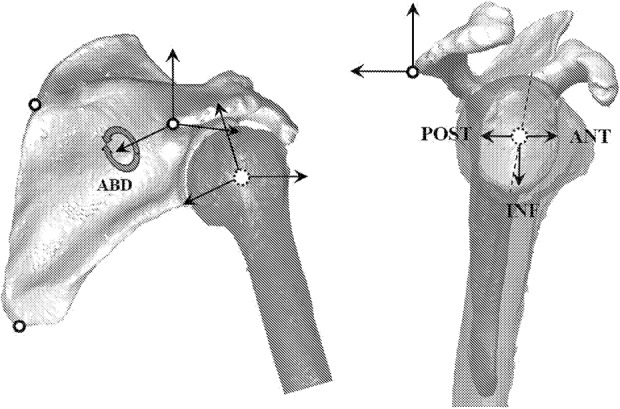
Shoulder segment anatomic coordinate frames and testing degrees of freedom from an oblique view (left) and lateral-to-medial view (right) are shown. The scapular coordinate system was based on bony landmarks (left): acromion angle, root of spine, and inferior angle. Glenohumeral kinematics were calculated as the translational motion of the humeral head center of rotation (COR; dotted circle) with respect to the scapula (right) offset to the glenoid COR. Dotted line indicates the superoinferior axis of the glenoid. ABD = abduction; POST = posterior; ANT = anterior; INF = inferior.
Statistical Analysis
Generalized estimating equations (GEE) with repeated factors were used for analysis. Plication magnitude and sequence were entered as categorical within-subject variables with translation as the dependent variable. A linear link function (analysis of variance model) was used along with an unstructured correlation matrix. Tested model main effects were Magnitude, Sequence, and their interaction, Magnitude x Sequence. Separate models were run for anterior, posterior, and inferior translation. An intercept parameter was included in each model.
Repeated-measures contrasts were also performed separately for anterior, posterior, and inferior translation. Paired comparisons were done across all combinations of capsule state and plication sequence levels including baseline and stretched for 11 experimental levels in all. Baseline and stretched levels, separately, served as references for the contrasts. Statistical significance level was set at α = 0.05. Statistics were done in SPSS software (IBM, Armonk, NY, USA).
Results
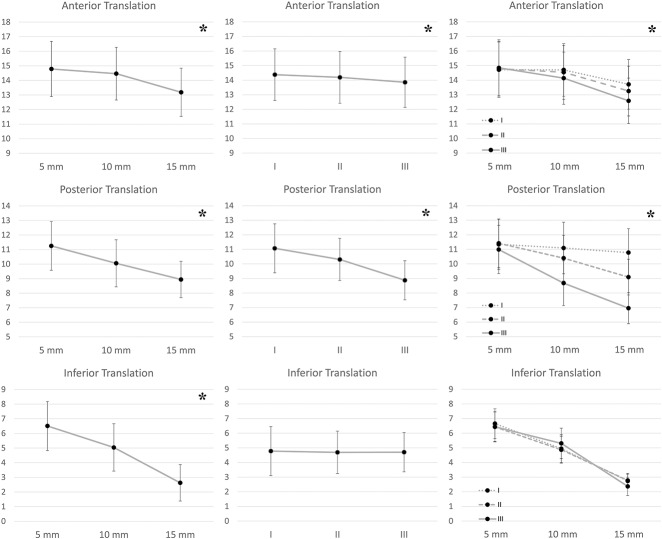
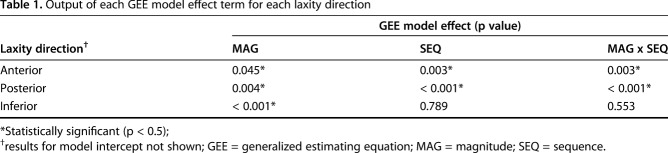
In general, glenohumeral laxity responded similarly across experimental conditions by increasing from intact to lax and then decreasing while progressing in magnitude and plication sequence (Fig. 5). Increasing plication magnitude decreased translation in anterior, posterior, and inferior laxity, but adding to the plication sequence (anterior, plus posterior, plus inferior) decreased anterior and posterior translations but not inferior translation. The interaction effect between plication magnitude and sequence was significant in anterior and posterior translation, but not inferior (Table 1). We observed decreasing laxity across plication magnitudes at different rates: a faster decline that corresponded with added sequence (Fig. 5). For anterior translational laxity, at 10-mm and 15-mm plication, there was a progressive decrease in translation magnitude (10-mm plication anterior only: 0.46 mm, plus posterior: 0.29 mm, plus inferior, -0.12 mm; and for 15-mm anterior only: -0.53 mm, plus posterior: -1.00 mm, plus inferior: -1.66 mm) (Fig. 6). For posterior translational laxity, 10-mm and 15-mm plication also showed progressive decrease in magnitude (10-mm plication anterior only: 0.46 mm, plus posterior: -0.25 mm, plus inferior: -1.94 mm; and for 15-mm anterior only: 0.14 mm, plus posterior: -1.54 mm, plus inferior: -3.66 mm) (Fig. 6). For inferior translational laxity, tightening was observed only with magnitude of plication (anterior only at 5 mm: 0.31 mm, at 10 mm: -1.39, at 15 mm: -3.61) but not with additional plication points (adding posterior and inferior sequences) (Fig. 6).
Fig. 5.
Plots of glenohumeral laxity against each modeled effect are shown. Each row of plots is a separate laxity direction (top = anterior, middle = posterior, bottom = inferior) and each column of plots is a generalized estimating equation (GEE) model effect term (left = MAG, middle = SEQ, right = MAG x SEQ). Within each plot the translational values (vertical axis) are plotted against the effect levels. Values are shown as the marginal mean ± 1.0 standard error. The interaction plots (MAG x SEQ, third column) show three lines instead of one, and their divergence indicates an increasing restriction of plication magnitude across plication sequence. *Statistically significant effect (p < 0.05).
Table 1.
Output of each GEE model effect term for each laxity direction
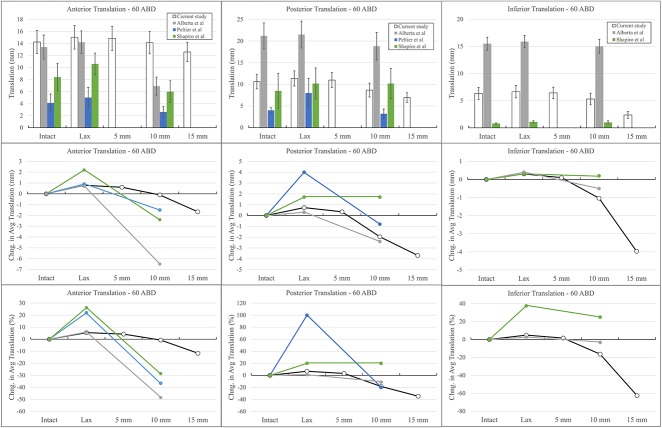
Fig. 6.
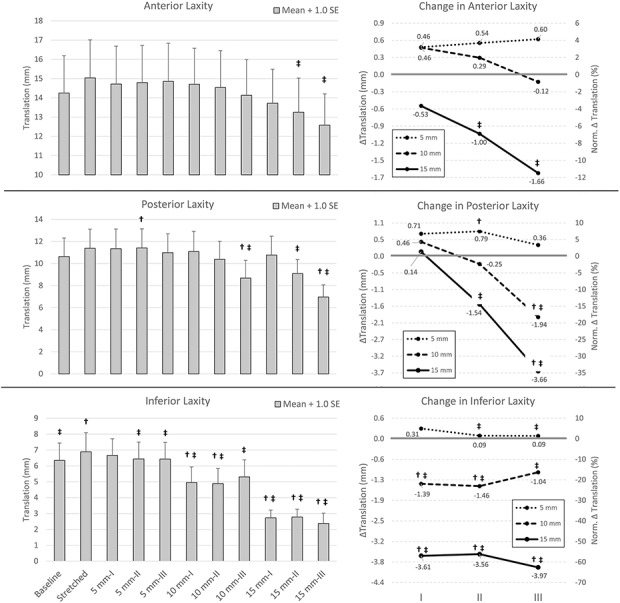
Glenohumeral laxity is demonstrated. The left bar graphs are the average translation laxity values + 1.0 standard error per STATE level. The right line graphs are the average (left vertical axis) and normalized average (right vertical axis) change (Δ) in laxity with respect to baseline; values are given per plication sequence (I, II, and III) on the horizontal axis; plication magnitudes are shown with different lines: small dash = 5 mm, large dash = 10 mm, and solid line = 15 mm. Single dagger (†) and double dagger (‡) indicate significant differences with respect to baseline and stretched conditions.
To restore laxity closest to baseline, 10-mm AP/inferior plication best restored anterior translation (to -0.12 mm of baseline), 15-mm anterior plication best restored posterior translation (to 0.14 mm of baseline), and 5-mm posterior with or without inferior plication best restored inferior translation (to 0.09 mm of baseline) (Fig. 6). Laxity in all directions was most restricted with 15-mm anterior, posterior, and inferior plication. Conditions having a substantial observed difference from either baseline or lax conditions occurred least frequently in the anterior direction, followed by posterior, and lastly inferior.
Discussion
The role of the glenohumeral ligaments in joint stability is well explained [6-10, 17, 27-29, 40, 43, 44]. In cases of atraumatic shoulder instability, capsular plication is often performed to restore the native mechanical stability of the joint. Clinical studies have shown good results with both open and arthroscopic techniques; however, it is difficult to determine if anatomic joint mechanics are restored [2, 3, 12]. Given the potential for recurrent instability with too little plication or overconstraint of the glenohumeral joint with too great a plication, a plication level that restores the native joint mechanics as closely as possible is ideal. Our study aimed to determine the effect of sequentially larger plications in three locations along the capsule on translation of the humeral head as well as the most advantageous combination of plications from among those tested to restore anatomic joint translation.
We recognize several limitations to this study. First, many of the specimens were advanced in age with possible unknown previous injuries to the shoulder and capsule not detectable with CT or dissection. Second, we did not simulate dynamic muscular forces across the shoulder, which may change translation compared with in vivo. Next, we are not able to draw conclusions about the effect of a single location of plication other than the anterior position as a result of the sequential and additive nature of the study design. Testing was also performed in a single position and plane, possibly limiting the applicability our conclusions to this glenohumeral position. Additionally, our methodology did not include testing of rotational changes, which is another important part of decision-making when performing a capsular plication. Our results are limited to time zero analysis and we are unable to provide information on the role of capsular healing or further changes over time. We chose a capsular-based plication technique for this study, which is less common than other described techniques. The rotator interval was closed in all specimens for homogeneity but may have produced translational consequences. We expected that these changes would be similar across specimens.
This study is comparable to others in specimen age, sample size, and technique of translational testing. Dynamic stability through muscular contraction is minimal during routine clinical laxity tests. Despite time zero analysis, this information could be used clinically to decide the best plication for individual patterns of instability from among those tested. Rotator interval closure created more homogeneity of capsule morphology and was performed before any translational testing. Additionally, previously collected pilot data suggested interval closure had no effect on translation in our model. Our capsular-based plication was chosen to isolate capsular effect without confounding factors of labral repair. As such, we feel that this study provides additional insight into the systematic effect of plication magnitude and location sequence on translation. To our knowledge this has not been previously reported.
We found translation decreased in all three directions with increasing magnitude of plication although each direction responded to a different degree (Fig. 5). Additionally, there was an interaction between magnitude and plication location for anterior and posterior translation, but not inferior. Compared with previous studies, we found it required anterior and posterior or anterior, posterior, and inferior 15-mm plication to decrease anterior translation, whereas two other studies each found that anterior translation was decreased with two anteriorly based 10-mm capsular or capsulolabral plications. We also found 10-mm anterior, posterior, and inferior plications or 15-mm anterior/posterior or anterior/posterior/inferior plication decreased posterior translation, whereas both other studies reported posterior translation had not decreased [30, 38]. A third study performed two anterior 10-mm capsulolabral plications and found anterior and posterior translation decreased below the lax state, again dissimilarly to our results [3]. This study also evaluated inferior translation, which did not decrease, unlike our study in which inferior translation decreased with 5-mm anterior/posterior or anterior/posterior/inferior translation and all 10- and 15-mm plication. Peltier et al. was the only previous report, which included the effect of a two-level (ANT and ANT + POST) sequence on anterior and posterior translation. Similar to our results, the addition of posterior plication decreased anterior translation further than anterior plication alone [30]. Dissimilarly, neither location decreased posterior translation. Each of these three studies utilized similar positioning of the glenohumeral joint (60° of abduction and neutral rotation), but they report plications of 10 mm, whereas our study included plications of 5, 10, and 15 mm. Each study utilized a different type, location, and number of plications, which may account for differing results (Fig. 7). These results support the circle stability concept, which states that an injury to both the anterior and posterior capsular structures occurs with anterior shoulder instability, and thus injury on both sides of the joint is necessary to produce instability, and repair of both sides may be necessary to restore stability [9]. Interestingly, plication magnitude and sequence progression showed an interdependent (covariate) change; increased loss of translational laxity was observed with progression in the plication sequence for a given magnitude. A lack of covariate change in inferior translation may be the result of the fixed plication sequence order with inferior sutures performed last. This information is important to consider in preoperative planning where knowledge of this multiplicative effect between plication magnitude and number of sites may improve the desired decrease of glenohumeral translation and may aid in decreasing the risk of joint overtightening. It is unknown if our observations would change with a different sequence order; thus, this remains open to future investigation.
Fig. 7.
Comparison of glenohumeral laxity across comparable studies is shown. Shown are the laxity results from this study and three others that tested laxity in 60° elevation per capsule condition. Each direction is in a separate column, and in rows top to bottom are the average raw translation, change in translation, and normalized change in translation. As a result of the range in experimental methodologies among our work and comparable studies, incremental steps of capsular plication magnitude past the stretched (lax) condition are Level 1, Level 2, and Level 3. ABD = abduction.
Addressing our second objective, our study found anterior translation was restored closest to baseline with 10 mm in anterior/posterior (+0.29 mm) or anterior/posterior/inferior (-0.12 mm) plication. Posterior translation was restored closest to baseline with 10-mm anterior/posterior (-0.25 mm) and 15-mm anterior plication (+0.14 mm). Posterior translation decreased furthest below baseline with 10-mm anterior/posterior/inferior (-1.94 mm) and 15-mm anterior/posterior (-1.54 mm) or anterior/posterior/inferior (-3.66 mm) plications. Finally, inferior translation was restored using 5-mm anterior/posterior (+0.09 mm) or anterior/posterior/inferior (+0.09 mm) plications. All 10-mm and 15-mm plications decreased inferior translation compared with baseline (-1.04 mm to -3.97 mm). Alberta et al. found less anterior translation than baseline (6.9 mm with 20-N force) with two 10-mm anterior plications [3]. However, Shapiro et al. also used two 10-mm anterior plications and found no decrease in anterior translation [38]. Peltier et al. also reported two 10-mm anterior plications did not decrease anterior translation with 25-N force. Addition of posterior plications also did not decrease anterior translation [30]. Compared with previous studies, conflicting results are also seen among those examining the ability of plication to restore baseline posterior translation. One study reported that posterior translation remained 5 to 6 mm greater than baseline after two 10-mm anterior plications [38]. However, another reported that posterior translation decreased 2.2 to 2.4 mm below baseline with the same plication configuration [3]. Peltier et al. reported posterior translation was not different than baseline, even with posterior plication added [30]. Shapiro et al. was the only study to quantify inferior translation and reported restoration 0.4 mm above baseline with two 10-mm anterior plications [38].
Based on our results, 10-mm plication in the combined AP or AP/inferior positions may restore anterior translation closest to baseline; 10-mm combined AP or 15-mm anterior plications may restore posterior translation closest to baseline; and 5-mm combined AP or AP/inferior plications may restore inferior translation closest to baseline. Our results may be used to help guide surgeons in individualizing surgical plans based on the direction of translational instability of each patient. Future studies that may expand on these findings could utilize arthroscopic or open surgical approaches with intact musculature or test translation and rotation of specimens in multiple degrees of glenohumeral abduction and rotation as well as follow clinical outcomes in patients after utilization of these individualized techniques.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Hospital for Special Surgery, New York, NY, USA.
References
- 1.Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002;400:48–57. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad CS, Wang VM, Sugalski MT, Levine WN, Bigliani LU. Biomechanics of shoulder capsulorrhaphy procedures. J Shoulder Elbow Surg. 2005;14(Suppl S):12S-18S. [DOI] [PubMed] [Google Scholar]
- 3.Alberta FG, Elattrache NS, Mihata T, McGarry MH, Tibone JE, Lee TQ. Arthroscopic anteroinferior suture plication resulting in decreased glenohumeral translation and external rotation. Study of a cadaver model. J Bone Joint Surg Am. 2006;88:179–187. [DOI] [PubMed] [Google Scholar]
- 4.Altchek DW, Warren RF, Skyhar MJ, Ortiz G. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am. 1991;73:105–112. [PubMed] [Google Scholar]
- 5.Bankart AS. Recurrent or habitual dislocation of the shoulder-joint. BMJ. 1923;2:1132–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability. Biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;330:13–30. [PubMed] [Google Scholar]
- 7.Blasier RB, Guldberg RE, Rothman ED. Anterior shoulder stability: contributions of rotator cuff forces and the capsular ligaments in a cadaver model. J Shoulder Elbow Surg. 1992;1:140–150. [DOI] [PubMed] [Google Scholar]
- 8.Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am. 1997;79:433–440. [PubMed] [Google Scholar]
- 9.Bowen MK, Warren RF. Ligamentous control of shoulder stability based on selective cutting and static translation experiments. Clin Sports Med. 1991;10:757–782. [PubMed] [Google Scholar]
- 10.Burkart AC, Debski RE. Anatomy and function of the glenohumeral ligaments in anterior shoulder instability. Clin Orthop Relat Res. 2002;400:32–39. [DOI] [PubMed] [Google Scholar]
- 11.Castagna A, Borroni M, Delle Rose G, Markopoulos N, Conti M, Vinci E, Garofalo R. Effects of posterior-inferior capsular plications in range of motion in arthroscopic anterior Bankart repair: a prospective randomized clinical study. Knee Surg Sports Traumatol Arthrosc. 2009;17:188–194. [DOI] [PubMed] [Google Scholar]
- 12.Castagna A, Markopoulos N, Conti M, Delle Rose G, Papadakou E, Garofalo R. Arthroscopic bankart suture-anchor repair: radiological and clinical outcome at minimum 10 years of follow-up. Am J Sports Med. 2010;38:2012–2016. [DOI] [PubMed] [Google Scholar]
- 13.Chalmers PN, Mascarenhas R, Leroux T, Sayegh ET, Verma NN, Cole BJ, Romeo AA. Do arthroscopic and open stabilization techniques restore equivalent stability to the shoulder in the setting of anterior glenohumeral instability? A systematic review of overlapping meta-analyses. Arthroscopy. 2015;31:355–363. [DOI] [PubMed] [Google Scholar]
- 14.DeAngelis JP, Hertz B, Wexler MT, Patel N, Walley KC, Harlow ER, Manoukian OS, Masoudi A, Vaziri A, Ramappa AJ, Nazarian A. Posterior capsular plication constrains the glenohumeral joint by drawing the humeral head closer to the glenoid and resisting abduction. Orthop J Sports Med. 2015;3:2325967115599347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flanigan DC, Forsythe T, Orwin J, Kaplan L. Volume analysis of arthroscopic capsular shift. Arthroscopy. 2006;22:528–533. [DOI] [PubMed] [Google Scholar]
- 16.Frank RM, Taylor D, Verma NN, Romeo AA, Mologne TS, Provencher MT. The rotator interval of the shoulder: implications in the treatment of shoulder instability. Orthop J Sports Med. 2015;3:2325967115621494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Itoi E, Hsu HC, An KN. Biomechanical investigation of the glenohumeral joint. J Shoulder Elbow Surg. 1996;5:407–424. [DOI] [PubMed] [Google Scholar]
- 18.Jacobson ME, Riggenbach M, Wooldridge AN, Bishop JY. Open capsular shift and arthroscopic capsular plication for treatment of multidirectional instability. Arthroscopy. 2012;28:1010–1017. [DOI] [PubMed] [Google Scholar]
- 19.Jobe FW, Giangarra CE, Kvitne RS, Glousman RE. Anterior capsulolabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med. 1991;19:428–434. [DOI] [PubMed] [Google Scholar]
- 20.Jones KJ, Kahlenberg CA, Dodson CC, Nam D, Williams RJ, Altchek DW. Arthroscopic capsular plication for microtraumatic anterior shoulder instability in overhead athletes. Am J Sports Med. 2012;40:2009–2014. [DOI] [PubMed] [Google Scholar]
- 21.Kuhn JE, Huston LJ, Soslowsky LJ, Shyr Y, Blasier RB. External rotation of the glenohumeral joint: ligament restraints and muscle effects in the neutral and abducted positions. J Shoulder Elbow Surg. 2005;14(Suppl S):39S-48S. [DOI] [PubMed] [Google Scholar]
- 22.Lubowitz J, Bartolozzi A, Rubinstein D, Ciccotti M, Schweitzer M, Nazarian L, Lombardi J, Dellose S, Landsdorf A, Miller L. How much does inferior capsular shift reduce shoulder volume? Clin Orthop Relat Res. 1996;328:86–90. [DOI] [PubMed] [Google Scholar]
- 23.Marcacci M, Zaffagnini S, Petitto A, Neri MP, Iacono F, Visani A. Arthroscopic management of recurrent anterior dislocation of the shoulder: analysis of technical modifications on the Caspari procedure. Arthroscopy. 1996;12:144–149. [DOI] [PubMed] [Google Scholar]
- 24.Miller MD, Larsen KM, Luke T, Leis HT, Plancher KD. Anterior capsular shift volume reduction: an in vitro comparison of 3 techniques. J Shoulder Elbow Surg. 2003;12:350–354. [DOI] [PubMed] [Google Scholar]
- 25.Neer CS, II, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 26.Nho SJ, Frank RM, Van Thiel GS, Wang FC, Wang VM, Provencher MT, Verma NN. A biomechanical analysis of shoulder stabilization: posteroinferior glenohumeral capsular plication. Am J Sports Med. 2010;38:1413–1419. [DOI] [PubMed] [Google Scholar]
- 27.O'Brien SJ, Neves MC, Arnoczky SP, Rozbruck SR, Dicarlo EF, Warren RF, Schwartz R, Wickiewicz TL. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449–456. [DOI] [PubMed] [Google Scholar]
- 28.O'Brien SJ, Schwartz RS, Warren RF, Torzilli PA. Capsular restraints to anterior-posterior motion of the abducted shoulder: a biomechanical study. J Shoulder Elbow Surg. 1995;4:298–308. [DOI] [PubMed] [Google Scholar]
- 29.O'Connell PW, Nuber GW, Mileski RA, Lautenschlager E. The contribution of the glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med. 1990;18:579–584. [DOI] [PubMed] [Google Scholar]
- 30.Peltier KE, McGarry MH, Tibone JE, Lee TQ. Effects of combined anterior and posterior plication of the glenohumeral ligament complex for the repair of anterior glenohumeral instability: a biomechanical study. J Shoulder Elbow Surg. 2012;21:902–909. [DOI] [PubMed] [Google Scholar]
- 31.Ponce BA, Rosenzweig SD, Thompson KJ, Tokish J. Sequential volume reduction with capsular plications: relationship between cumulative size of plications and volumetric reduction for multidirectional instability of the shoulder. Am J Sports Med. 2011;39:526–531. [DOI] [PubMed] [Google Scholar]
- 32.Privitera DM, Bisson LJ, Marzo JM. Minimum 10-year follow-up of arthroscopic intra-articular Bankart repair using bioabsorbable tacks. Am J Sports Med. 2012;40:100–107. [DOI] [PubMed] [Google Scholar]
- 33.Reinold MM, Gill TJ, Wilk KE, Andrews JR. Current concepts in the evaluation and treatment of the shoulder in overhead throwing athletes, part 2: injury prevention and treatment. Sports Health. 2010;2:101–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Remia LF, Ravalin RV, Lemly KS, McGarry MH, Kvitne RS, Lee TQ. Biomechanical evaluation of multidirectional glenohumeral instability and repair. Clin Orthop Relat Res. 2003;416:225–236. [DOI] [PubMed] [Google Scholar]
- 35.Schneider DJ, Tibone JE, McGarry MH, Grossman MG, Veneziani S, Lee TQ. Biomechanical evaluation after five and ten millimeter anterior glenohumeral capsulorrhaphy using a novel shoulder model of increased laxity. J Shoulder Elbow Surg. 2005;14:318–323. [DOI] [PubMed] [Google Scholar]
- 36.Sekiya JK, Willobee JA, Miller MD, Hickman AJ, Willobee A. Arthroscopic multi-pleated capsular plication compared with open inferior capsular shift for reduction of shoulder volume in a cadaveric model. Arthroscopy. 2007;23:1145–1151. [DOI] [PubMed] [Google Scholar]
- 37.Shafer BL, Mihata T, McGarry MH, Tibone JE, Lee TQ. Effects of capsular plication and rotator interval closure in simulated multidirectional shoulder instability. J Bone Joint Surg Am. 2008;90:136–144. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro TA, Gupta A, McGarry MH, Tibone JE, Lee TQ. Biomechanical effects of arthroscopic capsulorrhaphy in line with the fibers of the anterior band of the inferior glenohumeral ligament. Am J Sports Med. 2012;40:672–680. [DOI] [PubMed] [Google Scholar]
- 39.Sodl JF, McGarry MH, Campbell ST, Tibone JE, Lee TQ. Biomechanical effects of anterior capsular plication and rotator interval closure in simulated anterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2016;24:365–373. [DOI] [PubMed] [Google Scholar]
- 40.Soslowsky LJ, Malicky DM, Blasier RB. Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J Shoulder Elbow Surg. 1997;6:371–379. [DOI] [PubMed] [Google Scholar]
- 41.Southgate DF, Hill AM, Alexander S, Wallace AL, Hansen UN, Bull AM. The range of axial rotation of the glenohumeral joint. J Biomech. 2009;42:1307–1312. [DOI] [PubMed] [Google Scholar]
- 42.Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25:306–311. [DOI] [PubMed] [Google Scholar]
- 43.Terry GC, Hammon D, France P, Norwood LA. The stabilizing function of passive shoulder restraints. Am J Sports Med. 1991;19:26-34. [DOI] [PubMed] [Google Scholar]
- 44.Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–1217. [PubMed] [Google Scholar]
- 45.Wang VM, Sugalski MT, Levine WN, Pawluk RJ, Mow VC, Bigliani LU. Comparison of glenohumeral mechanics following a capsular shift and anterior tightening. J Bone Joint Surg Am. 2005;87:1312–1322. [DOI] [PubMed] [Google Scholar]
- 46.Werner CM, Nyffeler RW, Jacob HA, Gerber C. The effect of capsular tightening on humeral head translations. J Orthop Res. 2004;22:194–201. [DOI] [PubMed] [Google Scholar]
- 47.Wiater JM, Vibert BT. Glenohumeral joint volume reduction with progressive release and shifting of the inferior shoulder capsule. J Shoulder Elbow Surg. 2007;16:810–814. [DOI] [PubMed] [Google Scholar]
- 48.Wu G, van der Helm FCT, Veeger HEJ, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. [DOI] [PubMed] [Google Scholar]
- 49.Zaffagnini S, Marcheggiani Muccioli GM, Giordano G, Bonanzinga T, Grassi A, Nitri M, Bruni D, Ravazzolo G, Marcacci M. Long-term outcomes after repair of recurrent post-traumatic anterior shoulder instability: comparison of arthroscopic transglenoid suture and open Bankart reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:816–821. [DOI] [PubMed] [Google Scholar]