Abstract
Objectives: Nonpharmacologic approaches have been characterized as the preferred means to treat chronic noncancer pain by the Centers for Disease Control and Prevention. There is evidence that mindfulness-based interventions (MBIs) are effective for pain management, yet the typical MBI may not be feasible across many clinical settings due to resource and time constraints. Brief MBIs (BMBIs) could prove to be more feasible and pragmatic for safe treatment of pain. The aim of the present article is to systematically review evidence of BMBI's effects on acute and chronic pain outcomes in humans.
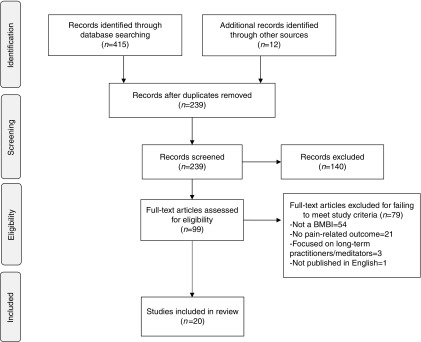
Methods: A literature search was conducted using PubMed, PsycINFO, and Google Scholar and by examining the references of retrieved articles. Articles written in English, published up to August 16, 2017, and reporting on the effects of a BMBI (i.e., total contact time <1.5 h, with mindfulness as the primary therapeutic technique) on a pain-related outcome (i.e., pain outcome, pain affect, pain-related function/quality of life, or medication-related outcome) were eligible for inclusion. Two authors independently extracted the data and assessed risk of bias.
Results: Twenty studies meeting eligibility criteria were identified. Studies used qualitative (n = 1), within-group (n = 3), or randomized controlled trial (n = 16) designs and were conducted with clinical (n = 6) or nonclinical (i.e., experimentally-induced pain; n = 14) samples. Of the 25 BMBIs tested across the 20 studies, 13 were delivered with audio/video recording only, and 12 were delivered by a provider (participant–provider contact ranged from 3 to 80 min). Existing evidence was limited and inconclusive overall. Nevertheless, BMBIs delivered in a particular format—by a provider and lasting more than 5 min—showed some promise in the management of acute pain.
Conclusions: More rigorous large scale studies conducted with pain populations are needed before unequivocally recommending BMBI as a first-line treatment for acute or chronic pain.
Keywords: mindfulness, meditation, brief, pain, systematic review
Introduction
Pain is a common experience; ∼56% of U.S. adults report having at least some pain in the last 3 months, with 11% reporting daily pain and 30% reporting pain that has lasted at least 3 months.1,2 Chronic pain can impair cognition and increases risk for anxiety, depression, and other affective disorders.3–6 Chronic pain has also been linked to increased health care utilization and reduced occupational activity,7,8 costing the United States over $600 billion per year in lost work productivity and medical treatment costs.1
To manage pain and its potential consequences, opioid medications like oxycodone are frequently prescribed. Indeed, over 35% of U.S. adults take prescription opioids in a given year,9 and about 4% receive long-term opioid therapy for chronic noncancer pain,10 although long-term opioid therapy is yet to be established as efficacious and poses significant health risks.11 Among other problems, prescription opioids have contributed to the epidemic of opioid use disorders, affecting an estimated 2 million Americans,12 and opioid-involved mortality, resulting in the overdose death of 90 Americans per day.13
Given that nonpharmacologic interventions can have comparable benefits and do not share the risks of opioid therapy, the Centers for Disease Control and Prevention currently recommends nonpharmacologic intervention as first-line treatment for managing chronic noncancer pain.14 One nonpharmacologic option receiving increased attention is a mindfulness-based approach. Mindfulness refers to a mode of awareness characterized by curiosity, nonjudgment, acceptance, and a present-moment focus.15 Mindfulness can be fostered and strengthened through a variety of mindfulness techniques (e.g., sitting mindfulness of breath, mindful body scan, and open-monitoring practice15). Over recent decades, mindfulness techniques have been incorporated into multiweek, mindfulness-based interventions (MBIs), like Mindfulness-Based Stress Reduction (MBSR15) and Mindfulness-Based Cognitive Therapy (MBCT16). MBIs have been applied and have demonstrated efficacy for a wide range of conditions.17
Extant literature indicates that MBIs may be effective in managing chronic noncancer pain,17–21 including severe, opioid-treated chronic pain.22,23 MBIs are thought to exert analgesic effects through various biobehavioral mechanisms, including improvements in pain catastrophizing, psychological flexibility, acceptance, the capacity to shift from affective to sensory discrimination of pain-evoking sensations, and top–down modulation of ascending nociceptive input.19,23,24
Despite their promise, MBIs are typically time intensive; they usually entail 8 weekly 1–2-h sessions plus daily home practice.15,16 Moreover, MBIs require highly-trained therapists and are usually delivered in specialty settings (e.g., pain clinics). Consequently, standard MBIs are not accessible or feasible for many patients and are difficult to implement in many clinical settings, like primary care and surgery departments. To be feasible across settings, the intervention needs to be brief, and, ideally, delivered at the point-of-care, one-on-one by a nonspecialist. This approach is supported by existing research, which indicates that brief interventions, such as the Screening, Brief Intervention, and Referral to Treatment for substance use disorders, can be effectively implemented in primary care and make a meaningful impact on patient outcomes.25,26 Brief MBIs (BMBIs) could fit well into various clinical settings and offer a safe and inexpensive alternative to opioids. However, the literature on this topic has not been adequately synthesized, presenting a knowledge gap.
Their goal was to systematically review the effects of BMBIs on pain-related outcomes. The authors focused on interventions that employed mindfulness as the primary technique (i.e., techniques designed to foster nonjudgmental awareness of the present moment; e.g., sitting mindfulness of breath, mindful body scan, and open-monitoring practice15) and that were brief enough that they could be implemented in primary care and other clinical settings (e.g., total contact time ≈30 min). Following the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) guidelines,27 the authors focused on the following pain-related outcomes: (1) pain outcomes (e.g., pain intensity and tolerance), (2) pain affect (e.g., pain unpleasantness), (3) function/quality of life (e.g., pain-related interference in social functioning), and (4) medication-related outcomes (e.g., medication use and desire for opioids). In addition to clinical/pain samples, the authors included nonclinical (nonpain) samples, in whom pain was induced experimentally. To maximize the number of potentially relevant articles, the authors did not impose restrictions on study design or comparison conditions.
Methods
The present systematic review was registered with PROSPERO (registration no. CRD42017074524). The PRISMA guidelines28 were followed in writing this report.
Search strategy
Literature searches were conducted by the first and second authors on PubMed, PsycINFO, and Google Scholar through August 16, 2017. Main keywords included the following: mindfulness, meditation, brief, short, abbreviated, minute, pain, acute pain, and chronic pain, in various combinations as needed. Reference sections of identified articles were also examined for additional studies.
The authors initially searched for all mindfulness interventions targeting pain-related outcomes that were shorter than the prototypic 8 weekly sessions, common for MBSR and MBCT.15,16 Based on direct participant–provider contact time, the BMBIs identified from this search generally fell into one of two broad categories: (1) interventions requiring less than 1.5 h of contact or (2) interventions requiring at least 6 h of contact. Given data from primary care settings,29,30 the authors chose through a consensus approach among the authors that interventions in the first—but not the second—category were compatible with primary care service delivery and, thus, focused the systematic review on the BMBIs entailing less than 1.5 h of contact time, regardless of the delivery method (e.g., audio-recording vs. contact with a provider). Because interventions delivered by audio-recording may not have the same efficacy as interventions delivered by a provider, the authors differentiated between these two modes of delivery (although both were included in this systematic review). In addition, because it can take more than a few minutes to fully enter into a mindful state,15 the authors also differentiated BMBIs shorter than 5 min from BMBIs that were 5 min or longer (although both were included in this systematic review).
Study eligibility criteria
Inclusion criteria were as follows: (1) involved human participants; (2) tested effects of a BMBI, defined as total contact time <1.5 h, with mindfulness as the primary therapeutic technique (i.e., techniques designed to foster nonjudgmental awareness of the present moment; e.g., sitting mindfulness of breath, mindful body scan, and open-monitoring practice15); and (3) investigated a pain-related outcome, which following (IMMPACT) guidelines27 included pain outcomes (e.g., pain intensity and tolerance), pain effect (e.g., pain unpleasantness), pain-related function/quality of life (e.g., pain-related interference in social functioning), and medication-related outcomes (e.g., medication use and desire for opioids). Exclusion criteria were as follows: (1) focused on long-term practitioners/meditators; (2) unpublished; or (3) not published in English. Studies were evaluated for eligibility by the first and second authors independently. The studies deemed eligible or potentially eligible by first and second authors were then discussed with the remaining authors to ensure consensus about the suitability of included studies.
Data extraction and risk of bias assessment
The first and second authors independently extracted and summarized the following data from each article included in the systematic review: (1) number of participants enrolled, (2) mean age, (3) percentage of White/Caucasian participants, (4) percentage of female participants, (5) number of study completers, (6) study design, (7) type of mindfulness practice/technique, (8) BMBI duration, (9) BMBI delivery method, (10) nature of control condition (if applicable), (11) methods for measuring mindfulness (if applicable), (12) methods for measuring pain-related outcomes, and (13) main study findings. When a discrepancy in the extracted data was identified, the first and second authors revisited and discussed the relevant article until consensus was reached. The first and second authors used the Cochrane Collaboration tool31 to independently assess risk of bias for the included randomized controlled trials (RCTs); bias risk was rated as high, low, or unclear for each of the following domains: random sequence generation, allocation concealment, blinding (participants and personnel), blinding (assessment of outcomes), attrition, and selective reporting.31 When a discrepancy in risk of bias ratings was identified, the first and second authors revisited and discussed the relevant article until consensus was reached.
Results
Literature search results
Twenty-six independent studies were initially identified. Of those, six studies (six articles) evaluated an MBI shorter than 8 weeks but entailed at least 6 h of direct participant–provider contact; these studies were excluded (see Appendix 1 for summaries of these studies). Twenty studies (19 articles) evaluated BMBIs and met the eligibility criteria (see Fig. 1 for flowchart, Table 1 for summaries).
FIG. 1.
Study selection flowchart. BMBI, brief mindfulness-based intervention.
Table 1.
Studies of Brief Mindfulness-Based Interventions for Pain Management (n = 20)
| Citation | Enrolled | Age (M) | % White | % Female | Completed | Design | Type of practice | Duration/delivery method | Control | Mindfulness measurement | Pain-related measurement | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Evans et al.38 | 63 undergrads | 19 | 74 | 46 | Not found | 3-arm RCT (later collapsed into 2 arms) | Observe or observe, describe, and accept | About 3 min, instructions delivered through computer (text and audio) | Spontaneous coping | Use of observing, describing, and accepting on visual analog scales (0–100) | CPT: pain tolerance | Mindfulness group reported greater use of observing and describing relative to control (ps < 0.05). Mindfulness group exhibited less pain tolerance relative to control (p < 0.05). |
| Feuille and Pargament39 | 107 persons (mostly undergrads) reporting at least two migraines in past month | 20 | 72 | 80 | 74 | 3-arm RCT | (1) Mindfulness of breath (2) spiritualized mindfulness | 7-min group session (with script), instructed to practice 20 min/day for 2 weeks at home (given handout). Practiced 15 min just before CPT | Relaxing | Toronto mindfulness scale state | CPT: pain tolerance and self-reported pain intensity and stress (0–10 scales) | Mindfulness of breath outperformed relaxation on stress during CPT (d = 0.68, p = 0.03). State mindfulness was higher for spiritualized mindfulness relative to mindfulness of breath (d = 0.85, p = 0.02). |
| Forsyth and Hayes40 | 67 persons: 42 undergrads and 25 community members | 29 | not found | 72 | 58 | 3-arm RCT | (1) Mindful acceptance of thoughts (2) mindfulness of breath | About 4 min, delivered with audio-recording | Spontaneous coping | Not found | CPT: pain tolerance and pain threshold | Pain tolerance improvements for acceptance of thoughts (d = 2.83) and mindfulness of breath (d = 3.92) were significantly (ps < 0.05) greater than improvements for control. No between-group effects on pain threshold. |
| Garland et al.41 | 244 inpatients reporting “intolerable pain” or “inadequate pain control” | 51 | 94 | 57 | 240 | 3-arm RCT | Focused attention and open monitoring | Scripted, 15-min session delivered by a social worker | (1) Hypnosis, (2) psychoeducation | Not found | Self-reported pain intensity, unpleasantness, anxiety, and desire for opioids (0–10 scales) | Mindfulness group reported improvements in all four outcomes (ds ranged from 0.17 [desire for opioids] to 0.98 [anxiety], ps < 0.05). Mindfulness outperformed psychoeducation (but not hypnosis) on pain intensity and unpleasantness (ps < 0.01). |
| Howarth et al.42 | 14 chronic illness outpatients (6 with chronic pain) | 55 | Not found | 64 | 14 | Qualitative study (focus groups and interviews) | Body scan | 10-min audio-recording delivered in clinical setting, then instructed to practice at least thrice over 1 week at home | Not found | Focus groups and interviews | Focus groups and interviews | Reductions in pain and medication use identified as key benefits. One patient reported discomfort. Recommendation for 15 min practice (instead of 10 min) |
| Liu et al.43 | 86 undergrads | 20 | Not found | 100 | 60 | 3-arm RCT | Mindfulness of breath, feelings, body sensations, pain | 15-min audio-recording | (1) Imagining a happy or relaxing scene, (2) listening to light music | Not found | CPT: pain tolerance and self-reported pain intensity and distress (0–10 scales) | Mindfulness outperformed light music on pain tolerance and distress and outperformed imagery on distress (ps < 0.05). |
| Petter et al. (2013) 44 | 86 healthy children | 12 | 83 | 44 | 82 | 2-arm RCT | Nonjudgmental awareness of breath, thoughts, body sensations | 10-min audio-recording | Guided imagery | Childhood acceptance and mindfulness measure and direction of attention (1–5 scales) | CPT: pain tolerance and self-reported average and most severe pain (selected from a series of six faces) | Mindfulness group reported greater awareness of thoughts and body sensations during CPT relative to imagery group (ps < 0.01). No significant between-group differences on pain tolerance, average pain, or most severe pain. |
| Petter et al.45 | 198 adolescents | 16 | 87 | 67 | 198 | 2-arm RCT | Nonjudgmental awareness of breath, judgments, and body sensations | 10-min audio-recording | Reading | Mindful attention awareness scale state and awareness of thoughts (1–5 scale) | CPT: pain tolerance and self-reported pain intensity (0–10 scale) | Mindfulness group reported greater awareness of thoughts during CPT relative to reading group (p < 0.05). No significant between-group differences on pain tolerance or intensity. |
| Prins et al.46 | 51 undergraduates | 20 | Not found | 84 | 46 | 2-arm RCT | Open monitoring | 10-min audio-recording | Audio-recording of two fairy tales | Mindful attention awareness scale | Heat stimulation: self-reported pain intensity, affective pain, attention to the pain, and general anxiety (0–10 scales) | No overall group effect, but mindfulness group outperformed control on pain ratings among persons high in pain catastrophizing |
| Reiner et al.47 | 40 undergrads | 24 | Not found | 50 | 36 | 2-arm RCT | Mindfulness of breath, thoughts, feelings, and body sensations | 20-min session delivered by instructor and audio-recording, instructed to practice 25 min/day for 2 weeks at home (with audio and handout) | Relaxing | Mindful attention awareness scale | Heat stimulation: pain threshold and self-reported pain intensity (0–100 scale) | Relative to control, mindfulness group showed increased pain threshold (p < 0.001; more pronounced for those high in baseline mindfulness) and more rapid attenuation of pain intensity (p < 0.001). |
| Sharpe et al.48 | 140 undergrads | ∼20 | not found | 72 | 140 | 4-arm RCT | Body scan with (1) threat or (2) no threat | 12-min audio-recording | (1) PMR with threat, (2) PMR without threat | Toronto mindfulness scale state | CPT: pain tolerance and threshold and self-reported pain intensity (0–10 scale) | Under high threat, body scan yielded higher decentering and curiosity than PMR (ps < 0.03). No significant between-group effects on pain outcomes. |
| Swain and Trevena49 | 240 tertiary students | 21 | 76 | 50 | Not found | 4-arm RCT | Mindfulness (type not clear) delivered by (1) therapist or (2) DVD | 3-min script (with therapist or DVD) | (1) Hypnosis with therapist, (2) hypnosis with DVD | Not found | CPT: pain tolerance and self-reported pain intensity (visual analog scale) and anxiety (1–7 scale) | No differences between four conditions on pain tolerance. Hypnosis participants reported less pain intensity and anxiety than mindfulness participants (ps < 0.05). |
| Teixeira50 | 22 older adults with chronic diabetic peripheral neuropathy symptoms (pain and/or numbness) | 75 | 90 | 75 | 20 | 2-arm RCT | Mindfulness (type not clear) | 60-min in-person session, instructed to practice 5 days per week for 4 weeks at home (with audio-recording) | 60-min in-person session on nutrition and food diary for 4 weeks | Not found | Self-reported pain intensity, pain unpleasantness, and quality of life | No significant between-group effects on pain intensity, unpleasantness, or quality of life |
| Ussher et al.51 | 55 chronic pain outpatients (mostly back pain) | ∼60 | 71 | 78 | 55 (clinic)51 (home) | 2-arm RCT | Body scan | 10 min audio-recording, delivered once in clinic and once within 24 h when in pain at home | Audio-recording on natural history | Philadelphia mindfulness scale and measures of acceptance, present focus, decentering | Self-reported pain intensity, pain-related distress, pain social interference, and perceived ability for daily activities (0–10 scales) | No between-group effects on mindfulness outcomes, pain intensity, or perceived ability for daily activities in clinic or at home. In clinic only, body scan outperformed control on pain distress (p = 0.005) and pain social interference (p = 0.036). |
| Warth et al.52 | 84 hospitalized patients in palliative care | 63 | Not found | 71 | 78 | 2-arm RCT | Body scan | 20-min audio-recording | Music therapy | Not found | Self-reported pain intensity and mood with visual analog scales (0–10) | No between-group effects on pain intensity. Music therapy outperformed mindfulness on mood (d = 0.61, p = 0.01). |
| Zeidan et al.53 | 27 undergrads | 19 | 82 | 32 | 22 | Within-group | Focused attention and open monitoring | Three 20-min group trainings (2 delivered by provider, 1 by audio-recording) on 3 consecutive days | (1) Baseline (before and after training), (2) Reading (before training) | Freiburg Mindfulness Inventory | Electrical stimulation: self-reported pain intensity (0–6 scale) and state anxiety measure | Mindfulness increased and anxiety decreased from pre- to post-training (ps < .01). Relative to baseline and reading conditions, a mindfulness condition (after training) resulted in lowest pain intensity ratings (ps ≈ .01). |
| Zeidan et al.53 | 23 undergrads | 21 | 52 | 62 | 21 | Within-group | Focused attention and open monitoring | Three 20-min group trainings (two delivered by provider, one by audio-recording) on three consecutive days | (1) Baseline (before and after training), (2) relaxing (before training), (3) math distraction (before and after training) | Freiburg mindfulness inventory | Electrical stimulation: self-reported pain intensity (0–6 scale) and state anxiety measure | Mindfulness increased and anxiety decreased from pre- to post-training (ps < 0.01). Relative to baseline, relaxing, and math distraction conditions, a mindfulness condition (after training) resulted in lowest pain intensity ratings (ps < 0.05). |
| Zeidan et al.54 | 18 healthy young adults | 26 | 87 | 60 | 15 | Within-group | Focused attention and open monitoring | Four 20-min in-person trainings over 4 days | (1) Rest (before and after training), (2) attention to breath/placebo (before training) | Freiburg mindfulness inventory | Heat stimulation: self-reported pain intensity and unpleasantness with visual analog scales | Mindfulness increased from pre- to post-training (14% increase, p = 0.004). Relative to rest and attention to breath conditions, a mindfulness condition (after training) resulted in lowest pain intensity and unpleasantness ratings (reductions of 40%–57% in pain ratings). |
| Zeidan et al.55 | 80 healthy community members | 27 | 75 | 49 | 75 | 4-arm RCT | Focused attention and open monitoring | Four 20-min in-person trainings over 4 days | (1) Placebo conditioning, (2) sham mindfulness meditation, (3) audio-recording on natural history | Freiburg mindfulness inventory | Heat stimulation: self-reported pain intensity and unpleasantness with visual analog scales | Mindfulness condition increased mindfulness (16%) and reduced pain intensity (27%) and unpleasantness (44%) more than placebo, sham, and audio-recording (ps < 0.05). |
| Zeidan et al.56 | 95 healthy community members | 27 | 73 | 50 | 78 | 4-arm RCT | Focused attention and open monitoring with (1) naloxone or (2) saline | Four 20-min in-person trainings over 4 days | (1) Audio-recording on natural history + naloxone, (2) audio-recording on natural history + saline | Not found | Heat stimulation: self-reported pain intensity and unpleasantness with visual analog scales | Mindfulness conditions outperformed (ps < 0.001) controls on pain intensity and unpleasantness (reductions of 21% to 36%), with no significant differences between mindfulness conditions. |
CPT, cold-pressor task; PMR, progressive muscle relaxation; RCT, randomized controlled trial
Methods of included studies
Designs
One study used qualitative methods, and the other 19 studies used quantitative methods. Of the 19 quantitative studies, 16 were primarily designed to assess intervention efficacy, and the remaining 3 were focused on mechanisms of action. The quantitative studies used within-group (n = 3) or RCT (n = 16) designs. Of the RCTs, eight had two arms, four had three arms, and four had four arms. Fifteen studies evaluated responses to experimentally-induced pain using the cold-pressor task (CPT) (n = 8), heat stimulation (n = 5), or electrical stimulation (n = 2).
Samples
Sample sizes ranged from 14 to 244 participants (total = 1740, M = 87). Fourteen studies were conducted with nonclinical (nonpain) participants, in whom pain was induced experimentally, and six were conducted with clinical samples of individuals with pain-related issues, such as migraine (n = 1), “intolerable pain” (n = 1), chronic diabetic neuropathy (n = 1), chronic noncancer pain (n = 1), palliative status (n = 1), and other chronic illness (n = 1). The included studies focused on children (n = 1), adolescents (n = 1), college students (n = 10), and adults (n = 8); this latter category included one study focused on adults aged 50 years or older. Across the 20 included studies, 63% of the participants were female. Across the 13 studies reporting race/ethnicity data, 81% of the participants were White/Caucasian.
Mindfulness interventions
Of the 20 included studies, 15 evaluated 1 BMBI and 5 evaluated 2 BMBIs. Of the 25 BMBIs in total, 13 were delivered with audio/video recording only (duration ranged from 3 to 20 min), and 12 were delivered by a provider (direct participant–provider contact ranged from 3 to 80 min). Five BMBIs were shorter than 5 min. Participants were instructed to practice mindfulness at home in six BMBIs, with the requested practice ranging from once to 5 days/week for 4 weeks.
A number of mindfulness techniques were represented. Two BMBIs used mindfulness of breath training, during which the practitioner is trained to focus and sustain attention on the changing sensations of the breath.15 Five BMBIs used body scan, which involves mindfully attending to sensations in different body parts, noticing when attention drifts from the meditative object (e.g., sensations in the left foot), and then returning attention back to the meditative object.15 One BMBI used mindful acceptance of thoughts/pain (i.e., emphasized being fully present, rather than avoiding unpleasant experiences), and another used “spiritualized” mindfulness (i.e., emphasized concept of wholeness and one's connection with all living beings). Thirteen BMBIs used a combination of mindfulness techniques, including open monitoring/vipassana. While mindfulness of breath and body scan foster a sharp focus on a specific meditative object, open-monitoring practices promote a wider field of awareness, in which any arising cognitive, emotional, or sensory event can be observed nonjudgmentally.15,57 The specific type of mindfulness practice was not clear for three BMBIs.
Control conditions
Thirty control conditions were identified across the 20 included studies. Eight control conditions were relatively inactive: 4 rest/relaxing, 2 spontaneous coping, and 2 baseline/no intervention, and 21 were more active: 8 education-based, 3 hypnotic suggestion, 3 imagery/distraction, 2 progressive muscle relaxation, 2 music-based, 2 sham mindfulness practice, and 1 placebo cream-conditioning interventions.
Outcomes
All outcomes were assessed immediately or soon after the intervention (no longer term follow-ups). Mindfulness level was assessed with the Freiburg Mindfulness Inventory58 in four studies, the State Version of the Toronto Mindfulness Scale59 in two studies, the Trait Version of the Mindful Attention Awareness Scale60 in two studies, the State Version of the Mindful Attention Awareness Scale60 in one study, the Childhood Acceptance and Mindfulness Measure61 in one study, the Philadelphia Mindfulness Scale62 in one study, and several nonvalidated, study-specific measures.
Regarding pain-related outcomes, pain outcomes (e.g., pain intensity, tolerance, and threshold) were assessed in all studies, pain-related effect (e.g., pain unpleasantness, stress/distress, and anxiety) was assessed in 13 studies, function/quality of life (e.g., perceived ability for daily activities and social interference) was assessed in 2 studies, and medication needs (e.g., medication use and desire for opioids) were assessed in 2 studies.
Risk of bias
See Table 2 for risk of bias ratings for included RCTs (n = 16). Regarding random sequence generation, 37.5% of studies had unclear risk, 56.3% had low risk, and 6.3% had high risk. Regarding allocation concealment, 37.5% of studies had unclear risk, 50.0% had low risk, and 12.5% had high risk. Regarding blinding (participants and personnel), 68.8% had unclear risk, 0.0% had low risk, and 31.3% had high risk. Regarding blinding (outcome assessment), 75.0% had unclear risk, 25.0% had low risk, and 0.0% had high risk. Regarding attrition, 12.5% had unclear risk, 68.8% had low risk, and 18.8% had high risk. Regarding selective reporting, 100.0% had unclear risk, 0.0% had low risk, and 0.0% had high risk.
Table 2.
Risk of Bias for Included Randomized Controlled Trials (n = 16) Using Cochrane Collaboration Tool
| Citation | Random sequence generation | Allocation concealment | Blinding (participants and personnel) | Blinding (outcome assessment) | Attrition | Selective reporting |
|---|---|---|---|---|---|---|
| Evans et al.38 | Unclear | Unclear | High risk | Unclear | Unclear | Unclear |
| Feuille and Pargament39 | High risk | High risk | Unclear | Low risk | High risk | Unclear |
| Forsyth and Hayes40 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear |
| Garland et al.41 | Low risk | Low risk | High risk | Unclear | Low risk | Unclear |
| Liu et al.43 | Low risk | Low risk | Unclear | Low risk | High risk | Unclear |
| Petter et al.44 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear |
| Petter et al.45 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear |
| Prins et al.46 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear |
| Reiner et al.47 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear |
| Sharpe et al.48 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear |
| Swain and Trevena49 | Unclear | High risk | Unclear | Unclear | Unclear | Unclear |
| Teixeira50 | Low risk | Low risk | High risk | Unclear | Low risk | Unclear |
| Ussher et al.51 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear |
| Warth et al.52 | Unclear | Low risk | High risk | Unclear | Low risk | Unclear |
| Zeidan et al.55 | Unclear | Low risk | Unclear | Unclear | Low risk | Unclear |
| Zeidan et al.56 | Low risk | Low risk | Unclear | Low risk | High risk | Unclear |
Cochrane Collaboration Tool: Higgins et al.31
Results of included studies (N = 20)
Findings of the 20 included studies are presented systematically below. The authors first review findings obtained with BMBIs shorter than 5 min, given that very short practices may be insufficient for producing a state of heightened mindfulness. Next, the authors review findings obtained with audio-delivered BMBIs because these interventions may not have the same efficacy as ones delivered by a provider. Regarding provider-led BMBIs lasting more than 5 min, findings are organized by sample type (i.e., nonclinical vs. clinical/pain) and then further organized by research design (i.e., qualitative, within-group, or RCT).
BMBI shorter than 5 min (n = 3)
Three studies evaluated BMBIs shorter than 5 min. In a three-arm RCT (N = 67), Forsyth and Hayes40 reported that two ∼4-min audio-recorded BMBIs (acceptance of thoughts and mindfulness of breath) yielded greater improvements in pain tolerance (d = 2.83 and d = 3.92, respectively; ps < 0.05) but not in pain threshold on the CPT relative to a spontaneous coping condition with healthy undergrads and community members. In contrast, Evans et al.38 found that an ∼3-min computer-delivered mindfulness practice resulted in less cold-pressor pain tolerance than a spontaneous coping condition with healthy undergrads, and Swain and Trevena49 found that 3-min mindfulness interventions, delivered by provider or DVD, did not outperform similarly-delivered hypnosis interventions on cold-pressor induced pain intensity ratings with healthy tertiary students. In summary, very short BMBIs (i.e., <5 min) have yielded mixed results with nonclinical samples.
BMBI longer than 5 min, delivered by audio only (n = 7)
Seven studies evaluated BMBIs longer than 5 min that were delivered by audio-recording only. Of these seven studies, five were conducted with nonclinical participants, and two were conducted with clinical/pain participants. Regarding the nonclinical research, Liu et al.43 determined, in a sample of 86 undergraduates, that 15 min of audio-recorded instruction in mindfulness of breath, body sensations, and pain led to significantly more cold-pressor pain tolerance than a music condition and significantly less cold-pressor induced distress compared to a pleasant imagery condition. The other four nonclinical studies did not reveal significant between-group differences when comparing the effects of 12-min audio-recorded body scan to progressive muscle relaxation48 or when comparing the effects of 10-min audio-recorded mindfulness practice to guided imagery,44 reading,45 or an audio-recording of fairy tales.46
Two studies evaluated audio-recorded BMBIs longer than 5 min with clinical participants. In a sample of patients with chronic noncancer pain (n = 55; 47.3% taking opioids), Ussher et al.51 found that a 10-min audio-recorded body scan outperformed a natural history recording on ratings of pain distress (p = 0.005) and perceived likelihood of pain interfering with social relations (p = 0.036) when delivered in a clinical setting (no significant differences when completed at home). Warth et al.52 reported that, relative to music therapy, a 20-min audio-recorded body scan was no more effective on pain intensity (p > 0.05) and was less effective on mood ratings (d = 0.61, p = 0.01) for 84 patients in palliative care. In summary, BMBIs delivered through audio-recording have yielded mostly disappointing results with clinical and nonclinical samples.
Provider-led BMBI longer than 5 min, nonclinical sample (n = 6)
Six studies evaluated provider-led BMBIs longer than 5 min with nonclinical participants. Of these six studies, three were conducted with within-group methodology. Zeidan et al.53 conducted two studies in which healthy participants completed control tasks before and after a 60-min training in mindfulness meditation. The mindfulness training significantly reduced pain intensity ratings (ps < 0.05) during noxious electrical stimulation of the arm compared to a reading condition (see Study 1) and compared to math distraction and relaxation conditions (see Study 3). In a study of 18 healthy participants undergoing functional magnetic resonance imaging (fMRI) to assess the possible brain mechanisms of mindfulness-based analgesia, Zeidan et al.54 found that four 20-min mindfulness meditation training sessions reduced pain intensity (40% reduction) and pain unpleasantness (57% reduction) in response to noxious heat compared to other conditions completed by the same group of participants (i.e., rest and placebo/“attention to breath” conditions). Zeidan et al.54 also identified the neural correlates of mindfulness-induced analgesia; reductions in pain intensity were associated with the activation of regions involved in top–down executive control (e.g., anterior cingulate cortex) and interoceptive awareness (e.g., right anterior insula), and reductions in plain unpleasantness were associated with the activation of regions involved in the cognitive reappraisal of sensory information (e.g., orbitofrontal cortex) and the deactivation of regions involved in low-level nociceptive processing (e.g., thalamus).
Three nonclinical studies evaluated provider-led BMBIs longer than 5 min with RCT methodology. In a RCT with 40 undergraduates, Reiner et al.47 showed that 20 min of mindfulness practice, followed by relatively intensive home practice (i.e., 25 min/day for 2 weeks), led to significantly higher pain threshold (p < 0.001) and more rapid attenuation of pain intensity (p < 0.001) during thermal stimulation compared to a relaxation condition. Two mechanistic RCTs were conducted by Zeidan et al. to determine if mindfulness-based analgesia engages: (1) endogenous opioidergic systems56 and (2) distinct neural mechanisms compared to two placebos: placebo-cream and sham mindfulness meditation.55 Across both studies, brief mindfulness training (i.e., four 20-min in-person sessions over 4 days) reduced experimentally-induced pain intensity (21%–27%) and pain unpleasantness (33%–44% reductions) ratings more than comparison conditions (i.e., placebo-cream, sham mindfulness meditation, and listening to an audio-recording on natural history). Zeidan et al.56 discovered that the analgesic effects of brief mindfulness training were not reversed by intravenous administration of naloxone, an opioid antagonist, demonstrating that brief mindfulness training does not engage endogenous opioidergic pathways to reduce experimentally-induced pain in nonclinical samples. Consistent with their previous neuroimaging study,54 Zeidan et al.55 reported that mindfulness-based analgesia engaged neural mechanisms (e.g., activation of the orbitofrontal cortex, perigenual anterior cingulate cortex, right anterior insula, and secondary somatosensory cortices; deactivation of the thalamus) that were distinct from those associated with placebo-cream and sham mindfulness meditation (e.g., activation of the thalamus and periaqueductal gray matter; deactivation of the posterior insula and secondary somatosensory cortices). Moreover, while sham mindfulness meditation-based pain relief was associated with lower respiration rate, mindfulness-based pain relief was not, suggesting that BMBIs may relieve pain through top–down modulation of ascending nociceptive input, rather than through the bottom–up mechanisms that characterize placebo/relaxation. In summary, provider-led BMBIs longer than 5 min have demonstrated beneficial effects on pain intensity and pain affect in nonclinical samples in both within-group and RCT studies.
Provider-led BMBI longer than 5 min, clinical/pain sample (n = 4)
Four studies evaluated provider-led BMBIs longer than 5 min with clinical/pain participants. Of these four studies, one was conducted with qualitative methodology, and three were conducted with RCT methodology. Using qualitative methods, Howarth et al.42 examined the effects of a 10-min, audio-recorded body scan, delivered in a clinical setting, and then practiced at least thrice over a 1-week period at home, with 14 outpatients with heterogeneous chronic illness conditions. Patients expressed high degree of satisfaction with the intervention and identified reductions in pain and medication use as key benefits. One patient suggested that a 10-min practice may be insufficient for alleviating pain, and many agreed that a 15-min practice would have been preferable.
Regarding the RCTs evaluating provider-led BMBIs longer than 5 min with clinical participants, Feuille and Pargament39 reported that mindfulness of breath and spiritualized mindfulness (i.e., emphasizing one's connection with all living beings), both of which involved 22 min of in-person practice and relatively intensive at-home practice (20 min/day for 2 weeks), led to lower cold-pressor stress relative to a relaxation condition (e.g., d = 0.68, p = 0.03) with 107 individuals with history of migraines (80% female). Of note, although the mindfulness conditions did not significantly differ on pain-related outcomes, spiritualized mindfulness produced significantly higher levels of state mindfulness relative to mindfulness of breath (d = 0.85, p = 0.02). Garland et al.41 randomized 244 inpatients (94% White) experiencing “intolerable pain” or “inadequate pain control” from an array of painful diseases and surgeries to 15 min of mindfulness practice (i.e., focused attention and open monitoring), psychoeducation, or hypnotic suggestion, all of which were delivered by social workers. The mindfulness condition led to improvements in pain intensity (d = 0.43, p < 0.001), unpleasantness (d = 0.58, p < 0.001), anxiety (d = 0.98, p < 0.001), and desire for opioids (d = 0.17, p < 0.05); the improvements in pain intensity and unpleasantness were significantly greater than improvements observed for psychoeducation (ps < 0.01) but not for hypnosis. Finally, Teixeira50 randomized 22 older adults with chronic pain and/or numbness caused by diabetic peripheral neuropathy to either: (1) BMBI, which entailed a 60-min session of mindfulness practice plus relatively intensive home practice (i.e., 5 days per week for 4 weeks), or (2) a 60-min nutrition education session with at-home diet monitoring; this small RCT did not show significant between-group differences on pain intensity, unpleasantness, or quality-of-life outcomes. In summary, provider-led BMBIs longer than 5 min have demonstrated encouraging results in a qualitative study and relative efficacy in two of three RCTs conducted with clinical/pain samples.
Discussion
To their knowledge, this is the first systematic review of the impact of BMBIs on outcomes relevant to acute and chronic pain. Findings on the efficacy of BMBIs were mixed; BMBIs were found to outperform a comparison condition on at least one pain-related outcome (e.g., pain intensity and pain unpleasantness) in only 11 of the 19 quantitative studies (8/14 conducted with nonclinical samples and 3/5 conducted with clinical/pain samples).
However, not all of the BMBIs were of equal rigor; some were very short (i.e., <5 min), and others were delivered through audio-recording. When focusing on provider-led BMBIs that were longer than 5 min, the authors found that these interventions demonstrated consistent efficacy. Indeed, excluding the small and likely underpowered study by Teixeira50 (n = 22), there were eight quantitative studies that tested a provider-led BMBI involving more than 5 min of mindfulness training, and all found that BMBI outperformed a comparison condition on at least one pain-related outcome (six conducted with nonclinical samples, and two conducted with clinical/pain samples). This may suggest that the delivery of BMBI in a particular format—by a provider and lasting more than 5 min—may hold some promise in the management of pain. The potential benefits associated with this format are in keeping with clinical experience. That is, the development of mindfulness skills may be facilitated by sufficient practice time and the presence of a therapist or other provider, who can answer questions and lend emotional and instrumental support. Nevertheless, more rigorous scrutiny, using well-designed clinical trials, is needed to answer questions about the effectiveness and “active ingredients” of BMBIs, especially in clinical samples.
Following the IMMPACT guidelines,27 the authors reviewed BMBI's effects on four types of pain-related outcomes: (1) pain outcomes, (2) pain affect, (3) function/quality of life, and (4) medication-related outcomes. Of the 19 quantitative studies, BMBI's relative efficacy was demonstrated for pain (n = 9), pain affect (n = 7), and function/quality of life (n = 1) outcomes. The only quantitative study investigating BMBI's effects on medication-related outcomes41 found that the desire for opioids significantly decreased from pre- to post-BMBI, although this reduction was not significantly greater than the reductions observed for comparison conditions. It is also worth noting that this study examined the desire for opioids, rather than opioid use; the latter might be a more important and consequential outcome for pain patients. Clearly, the current evidence base is insufficient for determining whether BMBIs improve medication-related outcomes or enhance function/quality of life.
The aforementioned effects of BMBIs on pain affect are noteworthy, considering the role that affective processes play in the pain experience.63 Indeed, some researchers have argued that pain relief can be mediated by improvements in pain affect.63 The reviewed findings, particularly those reported by Zeidan et al.,54,55 suggest that this hypothetical pathway from mindfulness training to pain relief through improved affect might itself be mediated by reduced activity in neural regions involved in low-level nociceptive processing (e.g., thalamus) and increased activity in neural regions involved in interoceptive awareness (e.g., right anterior insula), top–down executive control (e.g., anterior cingulate cortex), and the cognitive reappraisal of sensory information (e.g., orbitofrontal cortex). Importantly, these mechanisms associated with BMBIs might be distinct from those associated with placebo, sham mindfulness meditation, distraction, and relaxation.54–56 However, the precise effects and mechanisms may depend on the nature of the pain (e.g., clinical vs. nonclinical pain), the specific mindfulness technique employed (e.g., focused attention vs. open monitoring), and the practitioner's experience level. For instance, there are some data indicating that open monitoring (vipassana) practice alleviates pain unpleasantness but not pain intensity57 and that mindfulness-based analgesia is associated with activation of the orbitofrontal cortex in novices and deactivation of the prefrontal cortex in long-term meditators.64 This might imply that, while BMBIs may modulate pain-related appraisals in novices, long-term training may employ “non-appraisal” mechanisms, indicating that the mechanisms of mindfulness-based analgesia may evolve with increasing meditation expertise.
The reviewed literature has several shortcomings that should be addressed in future research. First, their risk of bias assessment showed that key information (e.g., details about randomization procedure) was often missing from articles and that blinding of participants and personnel was not consistently implemented (i.e., 31.3% of studies had high risk of bias in this domain). Specifically, blinding can be compromised when inactive controls are used (e.g., resting); participants asked to “wait quietly” or “rest” might deduce that they are in the nonexperimental condition, which could introduce various forms of bias, like demand characteristics and expectancy effects.
A second limitation of the reviewed literature is that many studies were conducted with small samples and were, therefore, likely underpowered for assessing efficacy. Using a between-group, medium effect size (d = 0.5), a sample size of at least 51 participants per group would be required to have an 80% chance of detecting an effect (assuming an effect exists). Yet, of the 14 RCTs designed to assess intervention efficacy, only 3 had this group size, raising the possibility that Type II errors were committed.
Third, because some studies relied on audio-recorded interventions and/or induced pain in nonclinical participants, the associated findings may have limited generalizability to clinical practice. Experimentally-induced pain is delivered under controlled conditions and is typically anticipated, and can be terminated at any time, by the participant. Despite some clinical situations in which pain is expected and its delivery controlled (e.g., procedural pain), clinical pain is unique because it can involve unpredictable flare-ups that are of variable intensity/duration and that can substantially impact the patient's lifestyle and behavioral functioning. The authors identified only six studies evaluating BMBIs with clinical/pain samples; of these, only one was conducted exclusively with chronic pain patients,51 and none was conducted exclusively with patients with opioid-treated chronic pain. Patients with chronic pain, especially severe pain requiring opioid therapy, tend to have complex co-occurring medical and mental health problems3–5 that can present clinical challenges65,66 and impact treatment response.67,68 Caution is therefore advised before generalizing the reviewed findings, based primarily on nonchronic pain samples, to the treatment of chronic pain, especially in opioid-treated populations. Although BMBIs could possibly be efficacious for these targets, multiweek MBIs might be required to produce therapeutic change; early stage RCTs suggest efficacy of 8-week MBIs for reducing pain severity, aberrant opioid-use related behaviors, and the use of opioids among patients with opioid-treated chronic pain.22,23
Fifth, longer term follow-ups are absent in this literature. That is, improvements in pain attributable to BMBIs have only been observed immediately or soon after the intervention, which indicates little about the sustainability of these improvements. Empirical data underscore the importance of continued mindfulness practice following MBIs,69 and so it stands to reason that BMBIs could have longer term efficacy, provided that participants continue to practice.
The limitations of past research implicate specific paths forward. Future studies should consider employing: (1) provider-led interventions entailing more than 5 min of mindfulness practice, (2) larger samples to sufficiently power the study for efficacy testing, (3) rigorous assessment of pain, function/quality of life, and medication/opioid use, and (4) longer term follow-ups, as consistent with the IMMPACT guidelines on clinical trials in chronic pain.27 Research procedures also need to be described in sufficient detail so that the quality of the resulting evidence can be ascertained. In addition, because some studies included multiple types of mindfulness practice in the same BMBI, future research might investigate whether the effects and mechanisms vary by practice type (e.g., focused attention vs. open monitoring). Furthermore, because past work in this area has primarily relied on female, Caucasian, and young adult participants, a top priority for future investigations is to test BMBIs with other groups (e.g., males, persons of color, and older adults), so that the authors could elucidate for whom BMBIs are most effective. Research with males may be especially important, as there is some evidence that they respond differently to noxious stimuli than females.44,70
Given that prescription opioids have contributed to an epidemic of opioid misuse and opioid-involved fatalities,71 it is imperative that primary care physicians and other medical providers have nonopioid interventions at their disposal that are safe, feasible at the point of care, and effective. This systematic review, which focused on a safe and easy to administer intervention (BMBI), yielded some encouraging findings on its potential efficacy, yet the evidence is still limited and inconsistent and, as such, inconclusive. While more rigorous, large scale research is needed before unequivocally recommending BMBI as a first-line treatment for acute or chronic pain, the clinical implications of employing a brief form of mental training to attenuate acute and chronic pain are of unique practicality to clinicians and attractiveness to patients seeking safe pain relief.
Acknowledgments
A.S.M. was supported by research fellowship T32HP10010, E.L.G. was supported by grants R01DA042033 and R61AT009296 from the National Institutes of Health, and F.Z. was supported by grant R00-AT008238 from the National Institutes of Health.
Appendix Table 1.
Excluded Studies that Investigated Mindfulness-Based Interventions Shorter than 8 Weeks but that Entailed at Least 6 H of Training Time (n = 6)
| Citation | Enrolled | Age (M) | % White | % Female | Completed | Design | Type of practice | Duration/delivery method | Control | Mindfulness measurement | Pain-related measurement | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cathcart et al.32 | 58 community members with chronic tension-type headaches | ∼45 | Not found | 62 | 42 | 2-arm RCT | Based on mindfulness-based stress reduction and mindfulness-based cognitive therapy | 6, 2-h group sessions over 3 weeks | Waitlist | Five facet mindfulness questionnaire | Self-reported headache intensity, frequency, and duration over 2-weeks and measures of depression, anxiety, and stress | Mindfulness condition outperformed control on headache frequency (p = 0.04) and observed facet of mindfulness (p = 0.01). |
| Duncan et al.33 | 30 healthy pregnant women | Not found | 59 | 100 | 29 | 2-arm RCT | Adapted from mindfulness-based stress reduction | 2.5 days of intensive training (about 18 h total) | Standard childbirth education | Five facet mindfulness questionnaire | Pain catastrophizing, perceived labor pain, use of pain medication during labor, and depression | Mindfulness condition outperformed control on depression (p < 0.04). |
| Esch et al.34 | 32 healthy adults | ∼26 | Not found | ∼75 | 31 | 2-arm RCT | Body scan, attention to breath and sensations, open monitoring, walking meditation | 5, 1.5-h group sessions over five consecutive days | Passive control | Freiburg mindfulness inventory | Tourniquet test: pain tolerance | No significant between-group differences. |
| Kingston et al.35 | 45 undergrads | 23 | Not found | 79 | 42 | 2-arm RCT | Body scan, mindfulness of breath, sounds, thoughts, and body sensations | 6, 1-h group sessions over 3 weeks | Guided imagery | Kentucky inventory of mindfulness skills | Positive effect, negative effect, and CPT: tolerance and self-reported pain intensity (1–10 scale) | Mindfulness scores increased over the mindfulness intervention (p < 0.005). Mindfulness intervention outperformed control on pain tolerance (p = 0.042) and intensity (p = 0.047). |
| Su et al.36 | 18 adults with moderate or severe pain, and 16 adults with mild or no pain | 39 | Not found | 73 | 34 | Within-group | Based on mindfulness-based stress reduction | 6 weekly 2.5-h sessions and 8-h session in fourth week | N/A | Kentucky inventory of mindfulness skills | Pain intensity and pain-related impairment | Significant improvements in mindfulness (p < 0.001), pain intensity (p = 0.005), and pain-related impairment (p = 0.016). |
| Tekur et al.37 | 91 patients with chronic low-back pain | ∼48 | Not found | 46 | 80 | 2-arm RCT | Mindful yoga | 1-week intensive residential yoga program (about 119 h total) | Exercise, education, breathing technique | Not found | Pain intensity, pain-related disability, and spinal flexibility | Mindfulness condition outperformed control on pain intensity (p < 0.001), pain-related disability (p < 0.001), and spinal flexibility (ps ranged from 0.002 to 0.059). |
RCT, randomized controlled trial; CPT, cold-pressor task.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Acadamies Press, 2011 [PubMed] [Google Scholar]
- 2. Nahin RL, Boineau R, Khalsa PS, et al. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clinic Proc 2016;91:1292–1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berryman C, Stanton TR, Bowering KJ, et al. Evidence for working memory deficits in chronic pain: A systematic review and meta-analysis. Pain 2013;8:1181–1196 [DOI] [PubMed] [Google Scholar]
- 4. Bushnell MC, Ceko M, Low LA. Cognitive and emotional control of pain and its disruption in chronic pain. Nat Rev Neurosci 2013;14:502–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bushnell MC, Case LK, Ceko M, et al. Effect of environment on the long-term consequences of chronic pain. Pain 2015;156:42–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol 2014;69:197–207 [DOI] [PubMed] [Google Scholar]
- 7. Gerdle B, Bjork J, Henriksson C, Bengtsson A. Prevalence of current and chronic pain and their influences upon work and healthcare-seeking: A population study. J Rheumatol 2004;31:1399–1406 [PubMed] [Google Scholar]
- 8. Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada-prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag 2002;7:179–184 [DOI] [PubMed] [Google Scholar]
- 9. Han B, Compton WM, Blanco C, et al. Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med 2017;167:293–301 [DOI] [PubMed] [Google Scholar]
- 10. Boudreau D, Von Korff M, Rutter CM, et al. Trends in long‐term opioid therapy for chronic non‐cancer pain. Drug Safety 2009;18:1166–1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: A systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med 2015;162:276–286 [DOI] [PubMed] [Google Scholar]
- 12. Schuchat A, Houry D, Guy GP. New data on opioid use and prescribing in the United States. JAMA 2017;318:425–426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. Understanding the epidemic. Online document at: www.cdc.gov/drugoverdose/epidemic/index.html, accessed 2017
- 14. Dowell D, Heagerich TM, Chou R. CDC guidelines for prescribing opioids for chronic pain—Unites States, 2016. JAMA 2016;315:1624–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kabat-Zinn J. Full Catastrophe Living (revised edition): Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Bantam Books, 2013. [Google Scholar]
- 16. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. New York: Guilford Press, 2012. [Google Scholar]
- 17. Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med 2014;174:357–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs. cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA 2016;315:1240–1249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Greeson J, Eisenlohr-Moul T. Mindfulness-based stress reduction for chronic pain. In: Baer R, ed. Mindfulness-Based Treatment Approaches: Clinician's Guide to Evidence Base and Applications. Burlington: Elsevier, 2014:269–292 [Google Scholar]
- 20. Hilton L, Hempel S, Ewing BA, et al. Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Ann Behav Med 2017;51:199–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Morone NE, Greco CM, Moore CG, et al. A mind-body program for older adults with chronic low back pain: A randomized clinical trial. JAMA Intern Med 2016;176:329–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zgierska A, Burzinski JC, Cox JC, et al. Mindfulness meditation and cognitive behavioral therapy intervention reduces pain severity and sensitivity in opioid-treated chronic low back pain: Pilot findings from a randomized controlled trial. Pain Med 2016;17:1865–1881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Garland EL, Manusov EG, Froeliger B, et al. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. J Consult Clin Psychol 2014;82:448–459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zeidan F, Vago DR. Mindfulness meditation-based pain relief: A mechanistic account. Ann N Y Acad Sci 2016;1373:114–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Angerwala SM, McCane-Katz F. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: A brief review. J Psychoactive Drugs 2012;44:307–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug Alcohol Depend 2009;99:280–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19 [DOI] [PubMed] [Google Scholar]
- 28. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6:E1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Forrest CB, Nutting PA, von Schrader S, et al. Primary care physician specialty referral decision making: Patient, physician, and health care system determinants. Med Decis Making 2006;26:76–85 [DOI] [PubMed] [Google Scholar]
- 30. Stange KC, Zyzanski SJ, Jaen CR, et al. Illuminating the “black box”: A description of 4454 patient visits to 138 family physicians. J Fam Pract 1998;46:377–390 [PubMed] [Google Scholar]
- 31. Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cathcart S, Galatis N, Immink M, et al. Brief mindfulness-based therapy for chronic tension-type headache: A randomized controlled pilot study. Behav Cogn Psychother 2014;42:1–15 [DOI] [PubMed] [Google Scholar]
- 33. Duncan LG, Cohn MA, Chao MT, et al. Benefits of preparing for childbirth with mindfulness training: A randomized controlled trial with active comparison. BMC Pregnancy Childbirth 2017;17:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Esch T, Winkler J, Auwarter V, et al. Neurobiological aspects of mindfulness in pain autoregulation: Unexpected results from a randomized-controlled trial and possible implications for meditation research. Front Hum Neurosci 2017;10:674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kingston J, Chadwick P, Meron D, Skinner C. A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. J Psychosom Res 2007;62:297–300 [DOI] [PubMed] [Google Scholar]
- 36. Su IW, Wu FW, Liang KC, et al. Pain perception can be modulated by mindfulness training: A resting-state fMRI study. Front Hum Neurosci 2016;10:570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tekur P, Singphow C, Negendra HR, Raghuram N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med 2008;14:637–644 [DOI] [PubMed] [Google Scholar]
- 38. Evans DR, Elsenlohr-Mohl TA, Button DF, et al. Self‐regulatory deficits associated with unpracticed mindfulness strategies for coping with acute pain. J Appl Soc Psychol 2014;44:23–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Feuille M, Pargament K. Pain, mindfulness, and spirituality: A randomized controlled trial comparing effects of mindfulness and relaxation on pain-related outcomes in migraineurs. J Health Psychol 2015;20:1090–1106 [DOI] [PubMed] [Google Scholar]
- 40. Forsyth L, Hayes LL. The effects of acceptance of thoughts, mindful awareness of breathing, and spontaneous coping on an experimentally induced pain task. Psychol Record 2014;64:447–455 [Google Scholar]
- 41. Garland EL, Baker AK, Larsen P, et al. Randomized controlled trial of brief mindfulness training and hypnotic suggestion for acute pain relief in the hospital setting. J Gen Intern Med 2017;32:1106–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Howarth A, Perkins-Porras L, Copland C, Ussher M. Views on a brief mindfulness intervention among patients with long-term illness. BMC Psychol 2016;4:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Liu X, Wang S, Chang S, et al. Effect of brief mindfulness intervention on tolerance and distress of pain induced by cold-pressor task. Stress Health 2013;29:199–204 [DOI] [PubMed] [Google Scholar]
- 44. Petter M, Chambers CT, Chorney JM. The effects of mindful attention on cold pressor pain in children. Pain Res Manag 2013;18:39–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Petter M, McGrath PJ, Chambers CT, Dick BD. The effects of mindful attention and state mindfulness on acute experimental pain among adolescents. J Pediatr Psychol 2014;39:521–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Prins B, Decuypere A, Van Damme S. Effects of mindfulness and distraction on pain depend upon individual differences in pain catastrophizing: An experimental study. Eur J Pain 2014;18:1307–1315 [DOI] [PubMed] [Google Scholar]
- 47. Reiner K, Granot M, Soffer E, Lipsitz JD. A brief mindfulness meditation training increases pain threshold and accelerates modulation of response to tonic pain in an experimental study. Pain Med 2016;17:628–635 [DOI] [PubMed] [Google Scholar]
- 48. Sharpe L, Perry KN, Rogers P, et al. A comparison of the effect of mindfulness and relaxation on responses to acute experimental pain. Eur J Pain 2013;17:742–752 [DOI] [PubMed] [Google Scholar]
- 49. Swain NR, Trevena J. A comparison of therapist-present or therapist-free delivery of very brief mindfulness and hypnosis for acute experimental pain. N Z J Psychol 2015;16:22–28 [Google Scholar]
- 50. Teixeira E. The effect of mindfulness meditation on painful diabetic peripheral neuropathy in adults older than 50 years. Holistic Nurs Pract 2010;24:277–283 [DOI] [PubMed] [Google Scholar]
- 51. Ussher M, Spatz A, Copland C, et al. Immediate effects of a brief mindfulness-based body scan on patients with chronic pain. J Behav Med 2014;37:127–134 [DOI] [PubMed] [Google Scholar]
- 52. Warth M, Kebler J, Hillecke TK, Bardenheuer HJ. Music therapy in palliative care: A randomized controlled trial to evaluate effects on relaxation. Dtsch Arztebl Int 2015;112:788–794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zeidan F, Gordon NS, Merchant J, Goolkasian P. The effects of brief mindfulness meditation training on experimentally induced pain. J Pain 2010;11:199–209 [DOI] [PubMed] [Google Scholar]
- 54. Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci 2011;31:5540–5548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zeidan F, Emerson NM, Farris SR, et al. Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. J Neurosci 2015;35:15307–15325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zeidan F, Adler-Neal AL, Wells RE, et al. Mindfulness-meditation-based pain relief is not mediated by endogenous opioids. J Neurosci 2016;36:3391–3397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Perlman DM, Salomons TV, Davidson RJ, Lutz A. Differential effects on pain intensity and unpleasantness of two meditation practices. Emotion 2010;10:65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Walach HB, Buttenmuller N, Kleinknecht V, Schmidt NS. Measuring mindfulness- the Freiburg Mindfulness Inventory (FMI). Pers Individ Differ 2006;40:1543–1555 [Google Scholar]
- 59. Lau MA, Bishop SR, Segal ZV, et al. The toronto mindfulness scale: Development and validation. J Clin Psychol 2006;12:1445–1467 [DOI] [PubMed] [Google Scholar]
- 60. Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol 2003;84:822–848 [DOI] [PubMed] [Google Scholar]
- 61. Greco LA, Baer RA, Smith GT. Assessing mindfulness in children and adolescents: Development and validation of the child and adolescent mindfulness measure (CAMM). Psychol Assess 2011;23:606–614 [DOI] [PubMed] [Google Scholar]
- 62. Cardaciotto L, Herbert JD, Forman EM, et al. The assessment of present-moment awareness and acceptance: The Philadelphia Mindfulness Scale. Assessment 2008;15:204–223 [DOI] [PubMed] [Google Scholar]
- 63. Edwards RR, Dworkin RH, Sullivan MD, et al. The role of psychosocial processes in the development and maintenance of chronic pain. J Pain 2016;17:70–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Zeidan F, Grant JA, Brown CA, et al. Mindfulness meditation-related pain relief: Evidence for unique brain mechanisms in the regulation of pain. Conscious Cogn 2012;19:597–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Esquibel AY, Borkan J. Doctors and patients in pain: Conflict and collaboration in opioid prescription in primary care. Pain 2014;155:2575–2582 [DOI] [PubMed] [Google Scholar]
- 66. Zgierska A, Miller M, Rabago D. Patient satisfaction, prescription drug abuse, and potential consequences. JAMA 2012;307:1377–1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jamison RN, Edwards RR, Liu X, et al. Relationship of negative affect and outcome of an opioid therapy trial among low back pain patients. Pain Pract 2013;13:173–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wasan AD, Michna E, Edwards RR, et al. Psychiatric comorbidity is associated prospectively with diminished opioid analgesia and increased opioid misuse in patients with chronic low back pain. Anesthesiology 2015;123:861–872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Morgan LP, Graham JR, Hayes-Skelton SA, et al. Relationships between amount of post-intervention mindfulness practice and follow-up outcome variables in an acceptance-based behavior therapy for generalized anxiety disorder: The importance of informal practice. J Contextual Behav Sci 2014;3:173–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Edwards RR, Haythornthwaite JA, Sullivan MJ, Filligim RB. Catastrophizing as a mediator of sex differences in pain: Differential effects for daily pain versus laboratory-induced pan. Pain 2004;111:335–341 [DOI] [PubMed] [Google Scholar]
- 71. Atluri S, Sudarshan G, Manchikanti L. Assessment of the trends in medical use and misuse of opioid analgesics from 2004 to 2011. Pain Physician 2014;17:119–128 [PubMed] [Google Scholar]