Abstract
Background:
Prescription drug monitoring program are designed to reduce harms from prescription opioids; however, little is known about what populations benefit the most from these programs. We investigated how the relationship between implementation of online prescription drug monitoring programs and rates of hospitalizations related to prescription opioids and heroin overdose changed over time, and varied across county levels of poverty and unemployment, and levels of medical access to opioids.
Methods:
Ecologic county-level, spatiotemporal study, including 990 counties within 16 states, in 2001–2014. We modeled overdose counts using Bayesian hierarchical Poisson models. We defined medical access to opioids as the county-level rate of hospital discharges for non-cancer pain conditions.
Results:
In 2010–2014, online prescription drug monitoring programs were associated with lower rates of prescription opioid-related hospitalizations (rate ratio 2014 = 0.74; 95% credible interval: 0.69, 0.80). The association between online prescription drug monitoring programs and heroin-related hospitalization was also negative, but tended to increase in later years. Counties with lower rates of non-cancer pain conditions experienced a lower decrease in prescription opioid overdose, and a faster increase in heroin overdoses. No differences were observed across different county-levels of poverty and unemployment.
Conclusions:
Areas with lower levels of non-cancer pain conditions experienced the smallest decrease in prescription opioid overdose and the faster increase in heroin overdose following implementation of online prescription drug monitoring programs. Our results are consistent with the hypothesis that prescription drug monitoring programs are most effective in areas where people are likely to access opioids through medical providers.
Keywords: Hospital discharges, overdose, prescription opioids, heroin, prescription drug monitoring programs
INTRODUCTION
Drug overdose is the leading cause of injury death in the United States.1 In 2016, fatal opioid-related overdoses accounted for about two-thirds of all US drug overdoses; prescription opioids were involved in approximately half of these events.2 Opioid-related deaths increased four-fold since 2001, from 9,492 to 42,249 in 2016.2 In response, several strategies have been introduced across the United States, including the development and implementation of prescription drug monitoring programs.
Prescription drug monitoring programs are state-level databases into which dispensing prescribers and pharmacists must enter prescription information when controlled medications are dispensed. Authorized users may access these data as permitted by state laws; online prescription drug monitoring programs have been increasingly implemented, providing timely information on dispensing. These programs are expected to reduce prescription opioid-related harm by improving clinical decision-making, identifying patients who might benefit from targeted health interventions, and detecting patients and prescribers engaged in illegal activities (e.g., doctor shopping, pill mills). Their implementation has been associated with safer prescribing practices and lower rates of prescription opioid use and fatal overdose, although evidence is inconsistent.3–5 Only two studies investigating the effect of prescription drug monitoring programs on drug-related overdoses have focused on non-fatal overdoses;6,7 thus, little is known about the potential impact of the programs on these outcomes.
To date, most research on prescription drug monitoring programs has focused on their average effects across populations and time, disregarding important potential sources of heterogeneity. Their impact likely varies by time, as more prescribers and dispensers use the program, and as the complexity of the program evolves. Newer programs tend to incorporate more features likely to affect prescribing and dispensing practices, such as proactive reporting to licensing bodies and prescribers/dispensers, mandatory registration, mandatory consultation of the prescription drug monitoring program, and data sharing across states.8 As newer versions of these programs incorporate additional features, increased benefits from the program may be observed.
Further, the benefit of prescription drug monitoring programs may depend on the source and motives for prescription opioid access in local populations. In particular, areas with a greater concentration of people who are prescribed prescription opioids to treat leading causes of non-cancer related pain might see the greatest benefit from prescription drug monitoring programs, as they are more likely to access prescription opioids through medical providers.9 The prescription drug monitoring program can thus help prescribers identify prescription opioid consumers whose prescription histories suggest misuse, and refer them to evidence-based treatment.10 This will not only reduce the risk of overdose among prescription opioid users, but it may also reduce the dispersion of prescription opioid to families and friends, thus reducing the prescription opioid supply in these areas.11,12
Prescription drug monitoring programs’ impact on heroin-related overdose is also not well understood. The rise in opioid prescriptions, and the subsequent increase in the number of non-medical users of prescription opioids have likely contributed to the rise in people dependent on opioids.13,14 Because the programs may restrict access to prescription opioids through licensed prescribers, people who are dependent on opioids may transition to heroin, which is cheaper and more widely available.15 This can affect low- and high- socioeconomic groups in different ways, for example, depending on their population levels of health coverage that allow access to alternative forms of pain management (e.g., acupuncture, physical therapy), and appropriate opioid discontinuation, including access to medication-assisted treatment for opioid use disorder.16 We hypothesized that in less affluent populations, prescription opioid users identified in health care settings are more likely to be “fired” without referral or referred to a treatment option the patient cannot afford or access.17 Hence, in a context of a restricted prescription opioid supply, less affluent populations may be at greater risk of transition to the cheaper, more widely available heroin.
Through a substantial investment by the US government (>$100 million), all 50 states and the District of Columbia have implemented by 2017 some form of a prescription drug monitoring program, so it is important to know who benefits the most from these programs and whether these programs have unintended consequences. In this study, we investigate whether the association between the implementation of online prescription drug monitoring programs and hospital discharges related to heroin and prescription opioid overdose varied by the concentration of hospital discharges related to non-cancer pain conditions in the county, year of implementation, and county-level socioeconomic conditions (SES).
METHODS
We conducted an ecologic county-level, spatiotemporal study using data from 990 counties in 16 states (Arizona, California, Colorado, Florida, Iowa, Kentucky, Michigan, Nebraska, New Jersey, New York, Oklahoma, North Carolina, Oregon, South Carolina, Vermont, and Washington) from 2001 to 2014, resulting in 13,860 space–time units. There were four counties in Colorado where boundaries changed between 2001 and 2002, thus they were combined into a single geographic unit. Our sample covers all major regions of the United States, and includes counties with low, medium, and high rates of opioid overdose, and states with early, middle, and late implementation of online prescription drug monitoring programs (see eAppendix 1, eTable 1).
Data Sources and Variables
Outcomes.
Annual county-level counts of prescription opioids and heroin-related hospital discharges were obtained from the State Inpatient Databases of the Healthcare Cost and Utilization Project (HCUP). State Inpatient Databases covers approximately 97% of all admissions to community hospitals in the United States18 and includes health, demographic, and administrative information for each admission, including the county of residence. Counts are for each admission, so that one person can have multiple admissions for the same or different diagnoses. Discharge diagnoses are coded according the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). We identified all cases with at least one of the following ICD-9-CM codes as the principal or secondary diagnosis: for heroin overdose, codes 965.01 and E850.0; and for PO overdose, codes 965.00, 965.02, 965.09, E850.1, and E850.2.19,20 Given the low rate of opioid overdose among children, we restricted the analyses to the population aged 12 years and older. The SID dataset also includes cases that had a fatal outcome; between 2001 and 2014, on average, 2.3% of all cases admitted for prescription opioid-related and 4.2% of all cases admitted for heroin-related overdose died during their hospitalization.
Exposure.
The primary exposure was the implementation of an online prescription drug monitoring program, defined as when the program became available online in each state, thus providing real-time information. For our main analyses we treated the online prescription drug monitoring program as a binary variable (presence vs. absence) but considered the fraction of the year in which the program was implemented. We also considered for a secondary analysis eight specific features of prescription drug monitoring programs classified by experts as potentially important determinants of prescribing practices and prescription opioid overdose (see eTable 1 for additional details).8
Effect Modifiers.
To capture variations in the association between presence of a prescription drug monitoring program and opioid overdose over time, we included the interaction of the program with year and year squared. With this we allowed the association between presence of an online program and overdose to vary across years in a non-linear fashion as programs became more robust.
We used the percentage of all hospital discharge diagnoses related to non-cancer pain conditions as a proxy for the local concentration of people who could be prescribed opioids for these diagnoses. Following Sullivan et al.,21 non-cancer pain conditions was defined as a hospitalization related to any of the following conditions: back pain, neck pain, arthritis/joint pain, headache/migrane.21 ICD-9-CM codes and a rationale for the use of this measure is presented in eAppendix 1 (see eTable 2).
Two county-level measures of SES were used as effect modifiers: the percentage of unemployed people and the percentage of families that are below the poverty line22,23. Annual county-level estimates of these variables were supplied by GeoLytics.24
Correlation between non-cancer pain conditions and the SES variable was low to moderate: Pearson’s r = 0.013 for poverty, and r = 0.319 for unemployment.
Other Covariates.
Based on prior studies,25–27 we included several time-varying demographic and health variables at the county level, estimated also annually by GeoLytics using the American Community Survey and census data:24 rate of hospital discharges/100 people; population density, measured as thousands of people/square mile; percentage of the population aged 20–44, 45–64, and >65 years; percentage of white population; percentage of male population; and the percentage of all hospital discharges that included codes for acute pain, following US Centers for Disease Control and Prevention guidelines.20 Studies have reported an association between medical marijuana, naloxone access laws and Good Samaritan Laws, and rates of opioid overdose at the state level.28–30 To account for this, we controlled for the status of these laws and the fraction of the year in which they were implemented at the state level. Finally, during the study period the Affordable Care Act went into effect, which meant that several states expanded Medicaid, including in many cases access to substance use treatment for Medicaid recipients, such as opioid replacement therapies.31 To account for this, we added an indicator at the state level that signals whether Medicaid expansion was in effect in a given year.
Analysis
We used a spatiotemporal Bayesian model in which we assumed the number of prescription opioids and heroin-related hospital discharges within counties followed a Poisson distribution; the Poisson model assumes that prescription opioids and heroin overdoses are distributed proportionally to each county’s population. To account for spatial autocorrelation of the geographical units, we included a conditional autoregressive random effect that uses the first-order adjacency matrix of counties, weighted as one if counties share a border.32,33 The conditional autoregressive random effect allows to deal with the lack of independence among spatial units, and to avoid biases due to small area effects.34 Models also included a non-spatial county random effect that effectively controlled for over-dispersion that can arise when areas have low or zero counts.35 Results were generated using the Integrated Nested Laplace Approximation package in R (R-INLA), which is a reliable method for generating posterior marginal distributions, avoiding long computational time when using a large number of space–time units, as in more traditional Markov chain Monte Carlo methods for fully Bayesian models.36,37 An example of R-INLA code used on this study is available in eAppendix 2.
We tested different model specifications, including different functions for time, state fixed effects, a county-specific random slope for time, a county-specific random slope for the effect of the prescription drug monitoring program, and spatial lags across counties that share boundaries but have different state policies, to test potential spillover effects of the program’s provisions. Models were compared using the deviance information criterion.38 Final models included a set of time-varying covariates as described previously, a state fixed effect to account for potential endogeneity of prescription drug monitoring program implementation within states (i.e., states with a greater prescription opioid problem may have implemented their program earlier), and linear and quadratic time trends to control for the secular trend of prescription opioid and heroin overdoses. Models also included a county random slope, which allowed counties to have different linear growth, and a random slope for presence of a prescription drug monitoring program; these random effects resulted in a >50-point improvement in the deviance information criterion. We did not include the prescription drug monitoring program spatial lag, as it did not improve model fit and did not have a well-supported coefficient. The mathematical notation of the final model used is presented in eAppendix 1.
To examine potential sources of heterogeneity in the effect of a prescription drug monitoring program, we fit two-way interactions between presence of an online program implementation and year of implementation (and year squared); two-way interactions between online program implementation and the proportion of hospital discharges related to non-cancer pain conditions; two-way interactions between online program implementation and both measures of SES; and three-way interactions between online program implementation, the source of potential heterogeneity, and time. Each source of heterogeneity was examined in a separate model.
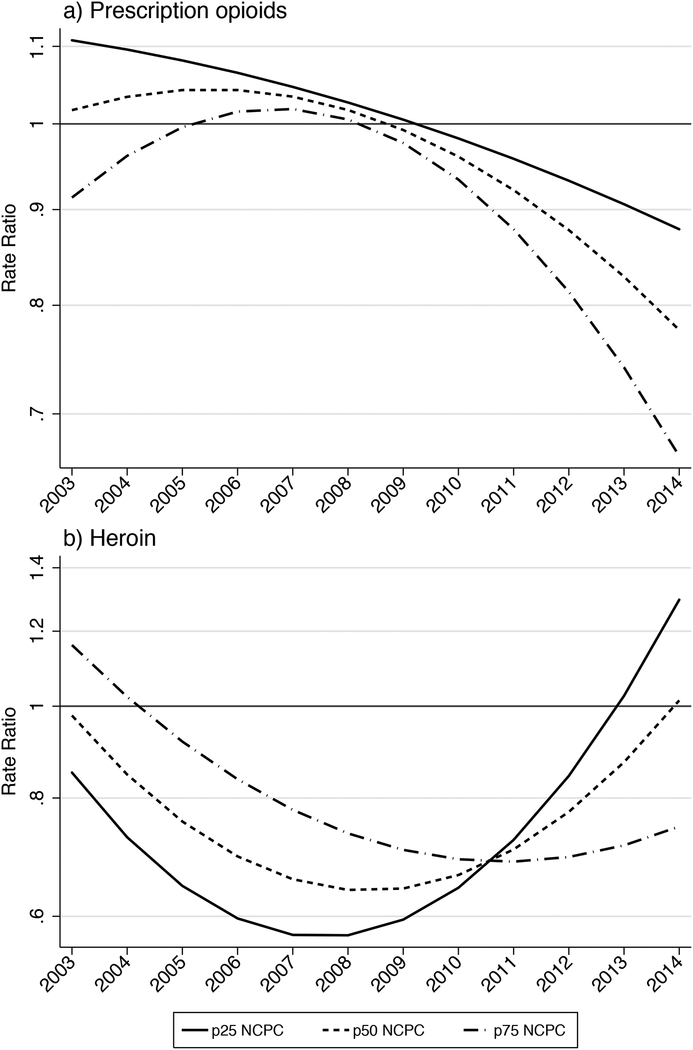
Finally, results in Figures 1 and 2 (and eFigures 2 to 5) were estimated as the linear combination of the coefficient of the presence of a prescription drug monitoring program and its two- and three-way interactions, as described. The SES and level non-cancer pain conditions were set at the 25th, 50th, and 75th percentile for each of those variables.
Figure 1. County-level association between implementation of online prescription drug monitoring programs and hospital discharges related to overdoses of prescription opioids (Panel a) and heroin (Panel b), 2003–2014.
RR: rate ratio; 95% CI: 95% credible interval (shaded area).
Figure 2. County-level association between implementation of online prescription drug monitoring programs and hospital discharges related to prescription opioid (Panel a) and heroin overdoses (Panel b), across county levels of non-cancer pain conditions, 2003–2014.
a NCPC = Non-cancer pain conditions. p25, p50 and p75 NCPC: level of NCPC at, respectively, the 25th, 50th, and 75th percentile of the distribution of the proportion of hospital discharges with NCPC diagnoses across the 13,860 county–year observations.
Sensitivity Analyses
As sensitivity analyses we considered: (1) removing Kentucky as a potential influential state to address threats of reverse causation (i.e., that prescription drug monitoring programs were implemented earlier in states with more overdoses); and (2) changing the definition of non-cancer pain conditions to consider alternative expert definition. A more detailed description of these sensitivity analyses is presented in eAppendix 1.
This study was approved by the Institutional Review Board at the University of California, Davis.
RESULTS
The median rate of hospital discharges related to prescription opioid overdose across the 990 counties was 16.8 per 100,000 people (Table 1). For heroin the numbers were much lower, with 75% of the space–time units having a rate of 0.87 per 100,000 people or less. Prescription opioids showed a continuous increase from 2001 to 2011, then stabilized and in most states decreased by 2014 (eFigure 2). The trend in discharges related to heroin overdoses remained stable in most states from 2001 to 2010, and increased thereafter.
Table 1.
Characteristics of 990 counties in 16 US states implementing prescription drug monitoring programs, 2001–2014 (n = 13,860 space-time units).
| Characteristic | |
|---|---|
| Median (interquartile range) | |
| Population aged ≥12 years | 27,024 (10,875 to 78,430) |
| Population density (people per square mile) | 49 (20 to 125) |
| Age (%) | |
| 20–44 | 32 (30 to 34) |
| 45–64 | 25.8 (24.3 to 27) |
| ≥65 | 16 (13 to 19) |
| Sex (%) | |
| Male | 49 (49 to 50) |
| Female | 51 (50 to 51) |
| Race/ethnicity (%) | |
| White | 83 (68 to 93) |
| Black | 1.7 (0.4 to 7.7) |
| Hispanic | 3.3 (1.4 to 8.1) |
| Socioeconomic status (%) | |
| Families living below the poverty line | 11 (8 to 15) |
| Unemployed | 6.6 (4.7 to 9.3) |
| Hospital discharge dataa | |
| Rate/100 people for all hospital discharges | 10 (9 to 12) |
| % discharged with diagnosis of non-cancer pain conditions | 25 (21 to 30) |
| % discharged with diagnosis of acute pain | 13 (12 to 15) |
| No. prescription opioid overdoses | 5 (1 to 18) |
| No. heroin overdoses | 0 (0 to 1) |
| Rate of prescription opioid overdoses/100,000 population | 17 (7 to 29) |
| Rate of heroin overdoses/100,000 population | 0 (0 to 0.87) |
| No. (%) | |
| Counties with medical marijuana lawsb | |
| 2002 | 193 (20) |
| 2008 | 207 (21) |
| 2014 | 326 (33) |
| Counties with Naloxone access lawsb | |
| 2002 | 0 (0.0) |
| 2008 | 62 (6.3) |
| 2014 | 587 (59) |
| Counties with Good Samaritan Lawb | |
| 2008 | 0 (0.0) |
| 2014 | 421 (423) |
| Counties with Medicaid expansionb | |
| 2008 | 0 (0.0) |
| 2014 | 607 (61) |
Restricted to population aged ≥12 years
Counties considered as to having the policy if the policy was effective for 6+ months.
Association of Online Prescription Drug Monitoring Program Implementation with Hospital Discharges Related to Overdoses
Compared with models that averaged the policy effect over the whole period, the overall fit of the models improved substantially when program effects were allowed to vary by time (deviance information criterion reduction for prescription opioids and heroin overdose of 144 and 82 respectively). eTables 2 and 3 show the results for PO and heroin overdoses.
Figure 1 summarizes the association between online prescription drug monitoring program implementation and opioid overdose across the entire study period. For prescription opioids, the implementation of an online prescription drug monitoring program was associated with a small increase in overdose rates in 2005–2007, with a maximum increase of 6% in 2006 (rate ratio [RR] = 1.06; 95% credible interval [CI], 1.01, 1.10). However, implementing a program in the following years was associated with a decrease in the rates of prescription opioids overdose (RR in 2014 = 0.74; 95%CI: 0.69, 0.80). For heroin, the association had a non-linear shape over the years, with the lowest rate ratio observed in 2007 (RR = 0.96; 95%CI: 0.48, 0.79) and the highest in 2014 (RR = 1.30; 0.95, 1.75).
Results for eight individual features of prescription drug monitoring programs are presented in Table 2. For prescription opioids, only “weekly reporting” was associated with reduced rates of overdose-related hospitalizations (RR = 0.92; 95%CI: 0.90, 0.93). For heroin, five out of eight features (“proactive reports to licensing bodies”, “proactive reports to prescribers/dispensers”, “mandatory registration for prescribers”, “mandatory access”, “weekly reporting”, and “all drug schedules reported”) were associated with higher overdose rates. Only “Proactive reports to law enforcement” was associated with lower heroin overdose hospitalizations (RR = 0.82; 95%CI: 0.74, 0.91).
Table 2.
County-level association between selected prescription drug monitoring programs features and hospital discharges related to overdoses of prescription opioids and heroin. 990 counties within 16 US states, 2003–2014
| Prescription Opioids | Heroin | |||
|---|---|---|---|---|
| Median | (95%CI) | Median | (95%CI) | |
| Proactive reports to law enforcement | 1.02 | (0.99, 1.04) | 0.82 | (0.74, 0.91) |
| Proactive reports to licensing bodies | 0.97 | (0.94, 1.00) | 1.29 | (1.13, 1.47) |
| Proactive reports to prescriber/dispenser | 0.99 | (0.97, 1.01) | 1.06 | (0.99, 1.13) |
| Mandatory registration for prescribers | 0.97 | (0.93, 1.01) | 1.12 | (1.00, 1.26) |
| Mandatory access | 0.98 | (0.94, 1.02) | 1.69 | (1.49, 1.90) |
| State shares data | 1.12 | (1.10, 1.15) | 1.01 | (0.95, 1.07) |
| Weekly reporting | 0.92 | (0.90, 0.93) | 1.19 | (1.12, 1.24) |
| All drug schedules reported | 1.08 | (1.06, 1.10) | 1.09 | (1.03, 1.16) |
| Presicion for model hyperparameters | ||||
| Non-spatial random effect | 18.3 | (13.4, 24.9) | 4.6 | (3.3, 6.4) |
| CAR spatial random effect | 5.8 | (4.3, 7.9) | 2.1 | (1.4, 3.1) |
| County-level random trend | 687.5 | (597.5, 790.5) | 152.7 | (125.0, 187.1) |
| Deviance Information Criterion | 66644 | 23112 | ||
Median = Rate ratio, computed as the exp(β) of the median posterior estimates. 95%CI = 95% Credible Interval. CAR = Conditional Autoregressive.
Models adjusted for the following county-level covariates: Rate of total hospital discharges; population density (1000s of people per square mile); % 20–44, 45–64, and 65 plus years of age; % white; % male; proportion of hospital discharges related to acute pain, proportion of hospital discharged related to chronic pain; % poverty, % unemployment. Models were also adjusted for State’s status on medical marijuana law, Naloxone access laws, Good Samaritan Law, Medicaid expansion, state fixed-effect, and a linear and quadratic time trend
The exclusion of Kentucky made no meaningful difference in the estimated results (eFigure 2).
Sources of Heterogeneity
There was a heterogeneous association between online prescription drug monitoring programs and overdose from prescription opioids or heroin across county levels of hospital discharges related to non-cancer pain conditions. Figure 2 presents the association between online prescription drug monitoring program implementation and opioid overdose at three different levels of community concentration of non-cancer pain conditions: (1) 25th percentile of the distribution of these diagnoses across the study population; (2) 50th percentile; and (3) 75th percentile. In counties at the 25th percentile of the non-cancer pain conditions distribution, the association between online prescription drug monitoring program implementation and prescription opioid overdose was fairly linear over time, going from 1.11 (95%CI: 1.03, 1.20) in 2003, when the first program was implemented, to 0.88 in 2014 (95%CI: 0.81, 0.95). In counties at the 75th percentile of the non-cancer pain conditions distribution, this association showed an inverse J-shape, with a RR of 0.91 (95%CI: 0.84, 1.00) in 2003 reaching its highest level in 2007 with an RR of 1.02 (95%CI: 097, 1.07), and a protective association since 2010, reaching its lowest level in 2014 with an RR of 0.66 (95%CI: 0.61, 0.73) (see Figure 2a).
The association between online program implementation and heroin overdose over the years, on the other hand, had a J-shape at the 25th percentile of the non-cancer pain conditions distribution: from 2004 to 2011, the implementation of online programs was associated with lower rates of heroin overdose (lowest RR in 2008 = 0.57; 95%CI: 0.44, 0.73). However, the risk ratio started increasing in 2009, reaching the highest level in 2014 (RR = 1.30; 95%CI: 0.93, 1.78). At the 75th percentile, baseline levels of heroin overdose were higher than those at the 50th and 25th percentiles; however, the implementation of online prescription drug monitoring programs was associated with a consistent decrease in heroin overdose rates across all years.
The proportion of hospital discharges cases involving non-cancer pain conditions under the alternative definition (see eAppendix 1) was highly correlated with our main definition (Pearson’s r = 0.99; p < 0.001), and results showed almost identical patterns as with the first definition (eFigure 3).
The association between implementation of online prescription drug monitoring programs and prescription opioid and heroin overdoses did not vary substantially by county level of socioeconomic conditions (see eFigures 4 and 5, respectively).
DISCUSSION
Prescription drug monitoring programs have been advanced as a key public health intervention to shift the course of the opioid epidemic in the United States. In our study, the implementation of an online program had a non-linear association across time with hospital discharges related to prescription opioid overdoses, showing a negative association at the county level only during the last four years of our study. An online prescription drug monitoring program was also associated with a decreased risk of hospital discharges for heroin overdoses in early years of implementation, but tending to increase in risk in more recent years; these associations varied by a county’s level of hospital discharges related to non-cancer pain conditions. During the study, counties with lower levels of non-cancer pain conditions experienced the least decrease in the rates of prescription opioid overdose and the fastest increase in heroin overdose following implementation of prescription drug monitoring programs.
Our results are somewhat consistent with other studies that have studied changes in population health associated with the implementation of prescription drug monitoring programs,4,27,39–42 although only two of them considered non-fatal overdoses.6,7 These two studies assessed emergency department visits in 11 geographically dispersed metropolitan areas in the United States from 2004 to 2011, one focusing on opioid analgesics and the other on benzodiazepine-related admissions. They found no change in emergency department admissions related to opioid analgesics and benzodiazepines. Our study was able to build on this prior research by investigating the association of implementation of online prescription drug monitoring programs with opioid overdose across a range of rural and urban states, and by accounting for potential heterogeneity of these associations over time.
The variation in the association between implementing an online prescription drug monitoring program and opioid overdose over time has several implications. Averaging the effect of a policy over time can miss important information, including cumulative effects, non-linear trajectories associated with an intervention, and most importantly, the increase in the robustness of these programs that occurred in the latest years. In our study we saw that in the early years of implementation (i.e., 2005–2007), online prescription drug monitoring programs was associated with a small increase in prescription opioid overdose at the county level, while in later years (i.e., 2010–2014), it was associated with up to a 25% reduction in prescription opioid overdoses. For heroin overdoses, the association showed a non-linear pattern, but in the opposite direction, so that as the robustness of prescription drug monitoring programs increased, implementation of online programs tended to be associated with increased risk of heroin overdoses.
We found that the association between implementation of online prescription drug monitoring programs and prescription opioid- and heroin-related overdoses varied by county-level concentration of hospital discharges related to non-cancer pain conditions. Counties with a higher concentration of people treated for these conditions experienced the largest reductions in prescription opioid overdose, and the lowest increases in heroin overdose, following implementation of on-line prescription drug monitoring programs. This finding suggests that prescription drug monitoring programs may be more effective at regulating access to prescription opioids in areas where the local population has more access to the prescription opioid supply through the medical system. However, in places with lower levels of medical treatment for non-cancer pain conditions, the implementation of a prescription drug monitoring program may decrease the overall availability of prescription opioids, but without a concurrent increase in referrals of opioid-dependent patients to substance dependence treatment. Restricting the prescription opioid supply may induce susceptible people who access opioids through non-medical routes to shift to other opioids, such as heroin.
We hypothesized a similar mechanism regarding effect modification of the association between prescription drug monitoring programs and opioid-related hospital discharges across socioeconomic levels, positing that support for adequate tapering of opioids, and access to treatment for opioid use disorders would be less available in less affluent areas. In our study, however, the relationship between online prescription drug monitoring programs and opioid overdose-related hospitalizations did not vary across county levels of poverty and unemployment, suggesting that the county-level SES measurement used may not adequately capture known financial barriers to accessing addiction treatment.43 It is also possible that the hypothesized mechanism is not strong enough to influence population levels of opioid overdose across areas of different socioeconomic conditions.
Our findings are consistent with the hypothesis that prescription drug monitoring programs are effective in reducing hospitalizations for overdoses from prescription opioids, but also highlight the need to think about strategies to mitigate unintended consequences of interventions that restrict the supply of prescription opioids.
This study makes several novel contributions to understanding the impact of prescription drug monitoring programs on opioid-related harm. We examined the association between online prescription drug monitoring program implementation and non-fatal opioid overdoses, considering both prescription opioid and heroin overdoses, and in counties rather than at the state level. Moreover, we sought to examine sources of heterogeneity in the associations, in order to highlight the particular benefits that prescription drug monitoring programs may provide to populations that access prescription opioids through health care providers. We tested for multiple model specification and conducted several sensitivity analyses, such as looking at individual features of prescription drug monitoring programs and removing a potentially influential state. In most cases estimates were similar to those generated in our main analysis.
Limitations
Our results should be interpreted in light of the following limitations. First, as in all ecologic studies, ours is not exempt of bias from aggregation of measurements at the county-level. Although this is one of the first studies to examine the impact of prescription drug monitoring programs in smaller geographic areas, thus reducing the possibility of aggregation bias, counties are still a large unit in terms of area and population. Second, we included only 16 states in our study because they had complete county-level data for the duration of the study when we conducted the analyses. Generalizability concerns are somewhat mitigated because our sample includes states in all major regions in the country, states of different sizes and with different sociodemographic characteristics, opioid problems, and times at which the prescription drug monitoring programs were implemented. Third, although we used fixed effects to account for state baseline differences, we accounted for multiple observed time-varying characteristics, and conducted several sensitivity analyses, there still may be residual confounding due to co-occurring changes in state policies. For example, a deterrent reformulation of OxyContin in 2010 affected the overdose potential of this drug across all states. This may have contributed to the stabilization or the decrease in prescription opioid overdose rates around the same time, and to the rise of the heroin epidemic.44 The differential effect of these changes across states, as well as other policy differences/changes within smaller areas (e.g., city-level prevention programs) is still not well known. Fourth, the classification of opioid overdose (and drugs in general) is based most times on patient’s (or relatives and friends) self-reports, or the report conducted by the health team based on the evidence observed at the time of admission (e.g., presence of medication, needles, and physical symptoms). The lack of toxicologic examination can cause miscoding of the actual cause of admission. Additionally, ICD-9 does not have a specific code for synthetic or semi-synthetic opioid that can be used to identify, for example, admissions likely due to fentanyl overdose as in the ICD-10 system. Finally, an inherent limitation of ecologic studies is that associations are at the area level, thus study findings cannot be used to make inferences at the individual level.
Within 990 counties in 16 US states, the implementation of online prescription drug monitoring programs was associated with reductions in hospital discharges related to prescription opioid overdoses. The largest benefit associated with these programs was observed in counties with greater concentration of hospital discharges related to non-cancer pain conditions, which may indicate greater access to prescription opioids through the medical system.
Supplementary Material
Acknowledgments:
We thanks Dr. Stephen G. Henry for his contributions to this article
Funding: This study was supported by grants from the US National Institute on Drug Abuse (R01DA039962, primary investigator, Dr. Cerdá; T32DA031099, Fink). Dr. Castillo-Carniglia was supported by Becas Chile as part of the National Commission for Scientific and Technological Research (CONICYT) and a Robertson Fellowship in Violence Prevention Research.
Footnotes
Conflict of Interests: None.
Example of R-INLA code used is available in eAppendix 2.
REFERENCES
- 1.CDC. Ten Leading Causes of Death and Injury, United States, 2016. https://www.cdc.gov/injury/wisqars/LeadingCauses.html Accessed 05/04, 2018.
- 2.CDC. Wide-ranging online data for epidemiologic research (WONDER). http://wonder.cdc.gov Accessed 05/04, 2018.
- 3.Rutkow L, Chang HY, Daubresse M, Webster DW, Stuart EA, Alexander GC. Effect of Florida’s Prescription Drug Monitoring Program and Pill Mill Laws on Opioid Prescribing and Use. JAMA Intern Med 2015;175(10):1642–9. [DOI] [PubMed] [Google Scholar]
- 4.Pardo B Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction 2016. [DOI] [PubMed] [Google Scholar]
- 5.Patrick SW, Fry CE, Jones TF, Buntin MB. Implementation Of Prescription Drug Monitoring Programs Associated With Reductions In Opioid-Related Death Rates. Health Aff (Millwood) 2016;35(7):1324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bachhuber MA, Maughan BC, Mitra N, Feingold J, Starrels JL. Prescription monitoring programs and emergency department visits involving benzodiazepine misuse: Early evidence from 11 United States metropolitan areas. Int J Drug Policy 2016;28:120–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maughan BC, Bachhuber MA, Mitra N, Starrels JL. Prescription monitoring programs and emergency department visits involving opioids, 2004–2011. Drug Alcohol Depend 2015;156:282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis CS, Pierce M, Dasgupta N. Evolution and convergence of state laws governing controlled substance prescription monitoring programs, 1998–2011. Am J Public Health 2014;104(8):1389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription. Clin J Pain 2014;30(7):557–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA 2016;315(15):1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seamans MJ, Carey TS, Westreich DJ, Cole SR, Wheeler SB, Alexander GC, Pate V, Brookhart MA. Association of Household Opioid Availability and Prescription Opioid Initiation Among Household Members. JAMA Intern Med 2018;178(1):102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health 2014;104(2):e52–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cicero TJ, Kuehn BM. Driven by prescription drug abuse, heroin use increases among suburban and rural whites. JAMA 2014;312(2):118–9. [DOI] [PubMed] [Google Scholar]
- 14.Muhuri P, Gfroerer J, Davies M. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States CBHSQ Data Review; SAMHSA, August. 2013. [Google Scholar]
- 15.Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. “Every ‘never’ I ever said came true”: transitions from opioid pills to heroin injecting. Int J Drug Policy 2014;25(2):257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moonesinghe R, Zhu J, Truman BI. Health Insurance Coverage — United States, 2004 and 2008. MMWR Morb Mortal Wkly Rep. Suppl 2011;60(1):35–7 [PubMed] [Google Scholar]
- 17.Wu LT, Zhu H, Swartz MS. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend 2016;169:117–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Healthcare Cost and Utilization Project (HCUP). Overview of the State Inpatient Databases (SID). http://www.hcup-us.ahrq.gov/sidoverview.jsp Accessed 07/27, 2017.
- 19.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid Prescribing After Nonfatal Overdose and Association With Repeated Overdose: A Cohort Study. Ann Intern Med 2016;164(1):1–9. [DOI] [PubMed] [Google Scholar]
- 20.CDC Prescription Drug Overdose Team. Guide to ICD-9-CM and ICD-10 code related to poisoning and pain. National Center for Injury Prevention and Control, 2013. [Google Scholar]
- 21.Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain 2008;138(2):440–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev Sci 2002;3(2):125–33. [DOI] [PubMed] [Google Scholar]
- 23.Karb RA, Subramanian SV, Fleegler EW. County Poverty Concentration and Disparities in Unintentional Injury Deaths: A Fourteen-Year Analysis of 1.6 Million U.S. Fatalities. PLoS One 2016;11(5):e0153516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.GeoLytics Inc. GeoLytics Estimates Premium. East Brunswick, NJ, 2017. [Google Scholar]
- 25.Cerda M, Gaidus A, Keyes KM, Ponicki W, Martins S, Galea S, Gruenewald P. Prescription opioid poisoning across urban and rural areas: identifying vulnerable groups and geographic areas. Addiction 2017;112(1):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305(13):1315–21. [DOI] [PubMed] [Google Scholar]
- 27.Paulozzi LJ, Kilbourne EM, Desai HA. Prescription drug monitoring programs and death rates from drug overdose. Pain Med 2011;12(5):747–54. [DOI] [PubMed] [Google Scholar]
- 28.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern Med 2014;174(10):1668–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi Y Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend 2017;173:144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McClellan C, Lambdin BH, Ali MM, Mutter R, Davis CS, Wheeler E, Pemberton M, Kral AH. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav 2018. March 19 [Epub ahead of print]. doi: 10.1016/j.addbeh.2018.03.014. [DOI] [PubMed] [Google Scholar]
- 31.Sharp A, Jones A, Sherwood J, Kutsa O, Honermann B, Millett G. Impact of medicaid expansion on access to opioid analgesic medications and medication-assisted treatment. Am J Public Health 2018;108(5):642–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernardinelli L, Clayton D, Pascutto C, Montomoli C, Ghislandi M, Songini M. Bayesian analysis of space–time variation in disease risk. Stat Med 1995;14(21–22):2433–43. [DOI] [PubMed] [Google Scholar]
- 33.Carlin B, Louis T. Bayes and Empirical Bayes Methods for Data Analysis, (2nd ed). New York: Chapman & Hall; 2000. [Google Scholar]
- 34.Waller L, Gotway C. Applied Spatial Statistics for Public Health Data. Wiley Publishers; 2004. [Google Scholar]
- 35.Lord D, Washington SP, Ivan JN. Poisson, Poisson-gamma and zero-inflated regression models of motor vehicle crashes: balancing statistical fit and theory. Accident; Analysis and Prevention 2005;37(1):35–46. [DOI] [PubMed] [Google Scholar]
- 36.Schrodle B, Held L. Spatio-temporal disease mapping using INLA. Environmetrics 2011;22(6):725–734. [Google Scholar]
- 37.Ugarte MD, Adin A, Goicoa T, Militino AF. On fitting spatio-temporal disease mapping models using approximate Bayesian inference. Stat Methods Med Res 2014;23(6):507–30. [DOI] [PubMed] [Google Scholar]
- 38.Spiegelhalter DJ, Best NG, Carlin BR, van der Linde A. Bayesian measures of model complexity and fit. Journal of the Royal Statistical Society Series B-Statistical Methodology 2002;64:583–616. [Google Scholar]
- 39.Delcher C, Wagenaar AC, Goldberger BA, Cook RL, Maldonado-Molina MM. Abrupt decline in oxycodone-caused mortality after implementation of Florida’s Prescription Drug Monitoring Program. Drug Alcohol Depend 2015;150:63–8. [DOI] [PubMed] [Google Scholar]
- 40.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood) 2016;35(10):1876–1883. 10.1377/hlthaff.2016.0448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim M The impact of prescription drug monitoring programs on opioid-related poisoning deaths. Johns Hopkins University, 2013. [Google Scholar]
- 42.Radakrishnan S Essays in the Economics of Risky Health Behaviors. Cornell University, 2015. [Google Scholar]
- 43.Saloner B, Lê Cook. Blacks and Hispanics are less likely than whites to complete addiction treatment, largely due to socioeconomic factors. Health Aff (Millwood) 2013; 32(1): 135–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cicero TJ, Ellis MS, Surratt HL. Effect of abuse-deterrent formulation of OxyContin. N Engl J Med 2012;367:187–189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.