Abstract
Purpose
Despite advances in cochlear implant and hearing aid technology, many children with hearing loss continue to exhibit poorer language skills than their hearing peers. This randomized pilot trial tested the effects of a parent-implemented communication treatment targeting prelinguistic communication skills in infants and toddlers with hearing loss.
Method
Participants included 19 children between 6 and 24 months of age with moderate to profound, bilateral hearing loss. Children were randomly assigned to the parent-implemented communication treatment group or a “usual care” control group. Parents and children participated in 26, hour-long home sessions in which parents were taught to use communication support strategies. The primary outcome measures were the Communication and Symbolic Behavior Scales (Wetherby & Prizant, 2003), a measure of child prelinguistic skills, and parental use of communication support strategies during a naturalistic play session.
Results
Parents in the treatment group increased their use of communication support strategies by 17%. Children in the treatment group made statistically significant more gains in speech prelinguistic skills (d = 1.09, p = .03) as compared with the control group. There were no statistically significant differences in social and symbolic prelinguistic skills; however, the effect sizes were large (d = 0.78, p = .08; d = 0.91, p = .10).
Conclusions
This study provides modest preliminary support for the short-term effects of a parent-implemented communication treatment for children with hearing loss. Parents learned communication support strategies that subsequently impacted child prelinguistic skills. Although these results appear promising, the sample size is very small. Future research should include a larger clinical trial and child-level predictors of response to treatment.
Although advances in cochlear implant and hearing aid technology have improved spoken language outcomes for many children with hearing loss, there is variability in language outcomes; many children with hearing loss continue to have poorer language skills than their hearing peers (Niparko et al., 2010; Tomblin, Oleson, Ambrose, Walker, & Moeller, 2014; Vohr et al., 2008). Many children with hearing loss produce significantly fewer communicative acts (Nicholas & Geers, 2003), take longer to acquire their first 50 words (Nott, Cowan, Brown, & Wigglesworth, 2009), have poorer vocabulary knowledge (Lund, 2016), have difficulty using grammatical structures in writing and in spoken language (Inscoe, Odell, Archbold, & Nikolopoulos, 2009; Spencer, Barker, & Tomblin, 2003), have poorer narrative skills (Crosson & Geers, 2000), and fail to achieve age-appropriate reading levels in high school (Geers, Tobey, Moog, & Brenner, 2008). These findings suggest that effective language interventions are needed to reduce the variability in spoken language outcomes in children with hearing loss.
Parent–Child Interactions as an Important Context for Early Language Development
Parents and children develop nuanced patterns of interaction from the first weeks of life, which form the basis for how children learn language. Several parent behaviors (communication support strategies) are associated with better language skills in children with hearing loss. Visual support strategies (e.g., using iconic gestures, moving objects into the child's line of sight) facilitate communication outcomes in children with hearing loss (Loots & Devisé, 2003; Loots, Devisé, & Jacquet, 2005). Specifically, parents who use more gestures had higher quality communicative exchanges with their children (Loots et al., 2005). Interactive strategies (e.g., following the child's interest, supporting joint engagement) are also associated with better spoken language outcomes in children with hearing loss (Cejas, Barker, Quittner, & Niparko, 2014). In fact, use of directive rather than interactive strategies at 18 months is negatively predictive of spoken language outcomes at 3 years of age for children with hearing loss (Ambrose, Walker, Unflat-Berry, Oleson, & Moeller, 2015).
Responsive support strategies (e.g., responding to child communication) are also highly associated with spoken language outcomes in children with hearing loss (Quittner et al., 2013). Parent–child conversational turns (Ambrose, VanDam, & Moeller, 2014) and maternal sensitivity (Pressman, Pipp-Siegel, Yoshinaga-Itano, & Deas, 1999) at 2 years predict spoken language outcomes at 3 years for children with hearing loss. Furthermore, maternal responsiveness at age of implant predicts spoken language outcomes at 5 years (Markman et al., 2011).
Linguistically stimulating strategies (e.g., expansions, recasts, number of adult word types, adult utterance length) are also associated with positive communication outcomes in children with hearing loss (DesJardin et al., 2014; DesJardin & Eisenberg, 2007). For example, parental use of expansions and parents' mean length of utterance at 12 months after implantation predict child mean length of utterance 18 months later (Szagun & Schramm, 2016; Szagun & Stumper, 2012). Furthermore, higher level strategies, such as parallel talk (i.e., talking about what the child is doing), expansions, recasts, and the use of open-ended questions are positively associated with growth in both receptive and expressive language outcomes during the 3 years after implantation (Cruz, Quittner, Marker, & DesJardin, 2013). Parent use of communication support strategies at the time of cochlear implantation positively related to spoken language at 5 years of age (Markman et al., 2011), and the magnitude of these effects is similar to those found for age of implantation (Quittner et al., 2013). These results suggest that teaching parents to use communication support strategies is likely to have a positive impact on communication outcomes for children with hearing loss and, as such, should be a critical target of early intervention.
Potential Barriers to Parent–Child Interactions
Hearing loss limits an infant's ability to hear what his or her parent is saying, and a mismatch between the hearing status of the parent and the infant may also impact parent–child interactions. These difficulties may arise from difficulty tailoring interactions to meet the infant's learning strategies. While parents attempt to adapt to their infant's communication needs, they are limited by their own communicative experiences. For example, a parent who learned language primarily through auditory information may use fewer nonauditory (visual, tactile) communicative strategies (Loots & Devisé, 2003), whereas a Deaf parent is more likely to use visual attention strategies than hearing parents (Waxman & Spencer, 1997). Perhaps, to compensate for this mismatch, hearing parents are more directive (i.e., directing the child to do something; Ambrose et al., 2015; Fagan, Bergeson, & Morris, 2014; Vaccari & Marschark, 1997). This increased directive behavior may result in reduced engagement in sustained interactions between children with hearing loss and their hearing parents (Gale & Schick, 2009; Lederberg & Mobley, 1990). Given that 90% of children with hearing loss have hearing parents (Albertini, 2010), providing strategies to overcome the mismatch is essential to maximizing long-term spoken language outcomes for children with hearing loss.
The Prelinguistic Period as a Critical Time for Early Intervention
Before children learn to talk, they use prelinguistic communication skills such as gestures and vocalizations to participate in social interactions. Waving, reaching, and pointing are a primary means of interacting with others before an infant is able to say words (Iverson & Goldin-Meadow, 2005). Early gesture use is particularly important for many children with hearing loss because gesture use in infancy predicts spoken language in toddlerhood (Roberts & Hampton, 2018). Gestures may have a cascading effect on language learning in several ways. Gestures allow children to communicate during a period in which they are unable to communicate using speech. Gestures may elicit more responses from communication partners, and this increased parental linguistic input may subsequently result in increased language skills (Goldin-Meadow, Goodrich, Sauer, & Iverson, 2007).
Vocalizations are also an important precursor to spoken language for children with hearing loss (Moeller et al., 2007). For children with hearing loss, lack of access to sound may disrupt vocal development by altering the quality and quantity of vocalizations. Amount of hearing loss is associated with canonical syllable use and vocalization types (von Hapsburg & Davis, 2006). While many infants with hearing loss may use the same number of total vocalizations as hearing infants, (Iyer & Oller, 2008; Koester, Brooks, & Karkowski, 1998; Moeller et al., 2007; Nathani, Oller, & Neal, 2007), many infants with hearing loss use fewer adult-directed vocalizations than hearing infants (Moeller et al., 2007). Taken together, these findings suggest that prelinguistic skills (gestures, vocalizations) are important targets for early intervention.
A Dearth of Experimental Intervention Studies of Toddlers With Hearing Loss
Despite the variability of language outcomes in children with hearing loss, only a few communication intervention studies have been conducted with children with hearing loss (Luckner & Cooke, 2010). In fact, a recent meta-analysis of auditory–verbal therapy revealed that not a single randomized or quasirandomized controlled trial of auditory–verbal therapy exists despite its widespread use (Brennan-Jones, White, Rush, & Law, 2014). Intervention studies of infants and toddlers with hearing loss have been largely descriptive, following children enrolled in early intervention programs over time (Ching, 2015; Meinzen-Derr, Wiley, & Choo, 2011; Moeller, 2000) or following a convenience sample of children receiving a particular intervention (Jackson & Schatschneider, 2014; Sacks et al., 2014). Findings from these studies suggest that early intervention, in general, is associated with positive language outcomes in children with hearing loss. However, these studies have focused largely on child factors (e.g., age of implantation, degree of hearing loss) rather than specific early intervention approaches. Furthermore, because these studies did not include a control group, it is impossible to determine whether gains were the result of the intervention or maturation alone. Thus, it remains unclear what specific early intervention strategies are most effective for children with hearing loss, illustrating the need for methodologically rigorous studies of early interventions for children with hearing loss.
Purpose of This Study
The proposed research is a pilot study of a parent-implemented communication treatment (PICT) for children with hearing loss. The intervention (a) was implemented during a critical period of prelinguistic language learning (Ruben & Schwartz, 1999); (b) involved the use of visual, interactive, responsive, and linguistically stimulating communication support strategies that are associated with stronger language outcomes in children with hearing loss (Cruz et al., 2013); and (c) included systematic parent training, which has been shown to be effective for increasing parents' use of communication strategies (Roberts & Kaiser, 2015). The objective of the current study was to evaluate the effects of systematically teaching parents to use communication support strategies on child prelinguistic skills. It was hypothesized that (a) parents in the treatment group would use more communication support strategies than parents in the control group, and (b) children in the treatment group would have better prelinguistic communication skills than children in the control group.
Method
Study Design
The PICT study was a single-institution, parallel, randomized, controlled trial (NCT01963468). The study took place in Chicago, Illinois. Northwestern University's Institutional Review Board (STU00081066) approved this study. All participants consented to be part of the research. No adverse events occurred for any study participant.
Participants
Children and their parents were recruited through the Ann & Robert H. Lurie Children's Hospital of Chicago and the Illinois Early Intervention System. Recruitment occurred continuously from October 2013 through June 2015. Eligibility criteria included (a) age between 6 and 24 months; (b) moderate to profound, bilateral, congenital hearing loss; and (c) no known additional disabilities (e.g., Down syndrome, cerebral palsy, seizure disorder, blindness). All children wore bilateral hearing aids, and no children had received a cochlear implant. All parents who participated in the intervention were mothers. See Table 1 for a summary of participant characteristics.
Table 1.
Participant characteristics at baseline.
| Variable | Trial arm |
Pretest comparison | |
|---|---|---|---|
| Intervention (n = 9) | Control (n = 10) | ||
| Child age in months, M (SD) | 10.11 (4.26) | 13.70 (7.77) | d = −0.57 |
| p = .24 | |||
| Degree of hearing loss in better ear, % | |||
| Moderate (41–70 dB hearing loss) | 40 | 33 | p = .82 |
| Severe (71–90 dB hearing loss) | 40 | 33 | |
| Profound (91+ dB HL) | 20 | 33 | |
| Cause of hearing loss, % | |||
| Genetic | 10 | 10 | p = .94 |
| Unknown | 90 | 90 | |
| Hours of speech therapy per month | 3.33 (1.03) | 3.00 (1.41) | d = 0.27 |
| Hours of deaf educator per month | 3.50 (1.00) | 3.50 (1.00) | p = .64 |
| Parent involvement in EI therapy, % | |||
| Did not observe the sessions | 22 | 0 | p = .29 |
| Only observed therapy sessions | 22 | 30 | |
| Observed and general discussion with EI provider | 56 | 70 | |
| Received coaching from an EI provider | 0 | 0 | |
| Male child, % | 67 | 60 | p = .76 |
| Child's ethnicity, % | |||
| Hispanic | 22 | 0 | p = .10 |
| Non-Hispanic | 78 | 100 | |
| Child race, % | |||
| White | 100 | 90 | p = .36 |
| Asian/Pacific Islander | 0 | 10 | |
| Mother's education, % | |||
| Some college | 33 | 30 | p = .96 |
| 4-year degree | 44 | 50 | |
| Graduate degree | 22 | 20 | |
| Baseline scores, M (SD) | |||
| Caregiver use intervention strategies | 0.31 (0.14) | 0.41 (0.18) | d = −0.62 |
| p = .19 | |||
| CSBS: Social weighted raw score | 10.04 (14.19) | 20.01 (11.71) | d = −0.76 |
| p = .11 | |||
| CSBS: Speech weighted raw score | 0.89 (2.67) | 1.90 (4.01) | d = −0.30 |
| p = .53 | |||
| CSBS: Symbolic weighted raw score | 1.89 (3.82) | 2.90 (3.76) | d = −0.27 |
| p = .57 | |||
| Cognitive skills (MSEL) | 50.78 (18.51) | 51.10 (19.07) | d = 0.02 |
| p = .97 | |||
Note. EI = early intervention; CSBS = Communication and Symbolic Behavior Scale Behavior Sample; MSEL = Mullen Scales of Early Learning (Mullen, 1995).
Randomization
Children were randomly assigned equally to treatment or business-as-usual control groups after a review of the inclusion criteria. A computer-generated random number sequence was used to create the allocation sequence. This sequence was only available to Dr. Roberts, not the interventionist. The interventionist enrolled participants, and Dr. Roberts assigned children to experimental conditions. Randomization was stratified based on geographic location (further than 50 mi. from Chicago) due to interventionists' scheduling constraints. Parents in both the intervention and business-as-usual control groups continued to receive early intervention services according to their individualized family service plan. We considered the use of an attentional control group (similar to a pill placebo in drug trials), but we decided against it because the extent to which attention actually affects the outcome or the expectancy of the outcome remains unknown in behavioral randomized trials (Pagoto et al., 2013).
Intervention
Because parents in the intervention group were overtly taught to use specific intervention strategies, parents were not naive to experimental condition. Parents in the control group did not receive the experimental treatment but rather community-based early intervention. Participants provided information about the type and amount of community-based intervention they received. Parents also reported about their level of involvement during their early intervention therapy sessions. Specifically, parents were asked if they were absent during the session (did not observe the sessions), if they observed the session but did not discuss the session with the therapist (observed the session), if they were present and received general strategies from their therapist (observed and general discussion), or if they were present and received specific coaching from their therapist (received coaching). Groups did not differ in terms of the amount or type of early intervention services they received (see Table 1). Although it is possible that the early intervention providers used similar intervention strategies as those included in the experimental intervention, the primary difference between the experimental condition and the business-as-usual early intervention was the inclusion of parents in intervention. No parents in either group received coaching as part of community-based early intervention. The treatment (PICT) included strategies to promote early communication stimulation and parent sensitivity during everyday routines and activities. These strategies are present in many early communication interventions, such as enhanced milieu teaching (Kaiser, 1993), prelinguistic milieu teaching (Yoder & Warren, 2002), and The Hanen Program It Takes Two to Talk (Girolametto, Pearce, & Weitzman, 1996). Parents were taught to encourage and reinforce communication attempts using four types of strategies: visual, interactive, responsive, and linguistically stimulating. Visual strategies included sitting face-to-face with the child, moving objects to the child's attentional focus, pairing spoken words with gestures (pointing), using exaggerated facial expressions, and waiting until the child looks before starting an interaction. Interactive strategies included following the child's lead, choosing interesting and engaging toys, and imitating play actions. Tactile strategies included touching the child to attract or keep attention. Responsive strategies included responding to all child communicative attempts (gestures, vocalizations) and balancing adult–child communicative turns. Linguistically stimulating strategies included expanding child communication by adding spoken words to gestures or vocalizations (e.g., child vocalizes and points to the cup, the parent points to the cup and says, “cup”). These strategies were chosen because they are positively associated with stronger communication skills in children with hearing loss (Quittner et al., 2013; Roberts & Hampton, 2018). See Table 2 for a summary of intervention strategies.
Table 2.
Overview of treatment strategies.
| Strategies | Specific strategies | Measure | Sessions |
|---|---|---|---|
| Visual | • Sit face-to-face with the child, wait until the child looks before starting an interaction, and move objects in the focus of the child's visual attention • Use gestures in the child's line of sight |
• Adult communication that is paired with a gesture in the child's line of sight | 1–6 (6 wks) |
| Interactive | • Follow the child's lead and choose interesting and engaging toys • Imitate the child's nonverbal actions (mirror) and model target language to actions (map) |
• Adult communication that labels the adult's imitation of a child's nonverbal action | 7–12 (6 wks) |
| Responsive | • Respond to communication attempts • Balance turns by responding to each child utterance with only one comment |
• Adult communication that is in response to child communication | 13–18 (6 wks) |
| Linguistically stimulating | • Expand child communication | • Adult communication to which the adult imitates and adds a word | 19–24 (6 wks) |
| All strategies | • Integration of strategies | 25–26 (2 wks) |
Note. wks = weeks.
It is important to distinguish between communication support strategies and mode of communication (sign or spoken language). While there is disagreement in the field regarding the impact that sign language has on spoken language of children with hearing loss (Geers et al., 2017; Mellon et al., 2015), frequently the decision regarding the mode of communication is made by parents (Decker, Vallotton, & Johnson, 2012). Furthermore, these communication support strategies may be used regardless of the mode of communication chosen by the parent (spoken, signed). As such, parents chose the mode in which they wanted to learn and use these strategies; all parents chose spoken language.
A deaf educator or a speech-language pathologist delivered the treatment in the participants' homes. Fidelity did not differ between the deaf educator and speech-language pathologist; fidelity for both exceeded 85% for all sessions. Both interventionists had taken a 3.0-unit course by the author (Dr. Roberts) on early communication interventions for infants and toddlers. This course included direct practice with an infant or toddler and their family. In addition, Dr. Roberts also attended the first six intervention sessions of the first two participants to provide live feedback and support. Hour-long treatment sessions occurred once per week for 6 months. Each session included four segments: (a) The interventionist introduced or reviewed a target treatment strategy (10 min); (b) the interventionist modeled the treatment strategy with the child (20 min); (c) the parent practiced the strategy with her child with coaching from the interventionist (20 min); and (d) the interventionist provided feedback to the parent, summarized the session, and answered the parent's questions (10 min). Intervention strategies were taught sequentially as described in Table 2. During these intervention sessions, the interventionist and parent used toys and materials in the child's home to facilitate generalization. Each session was video-recorded, and fidelity of implementation of the treatment was completed for a random sample of 20% of sessions by an independent rater who watched a video recording of the session and scored a fidelity checklist for the presence of treatment features (e.g., did the interventionist demonstrate the strategy at least six times during the session, did the interventionist provide coaching to the parent at least once every 2 min). The fidelity checklist may be found in the Appendix. On average, treatment fidelity was 92% and was greater than 85% for all sessions.
Outcomes
Parent and child outcomes data were collected in the home at baseline and after the end of treatment (6 months). The home was chosen because young children are typically more comfortable in their home. Because parents were taught to use specific treatment strategies, parents knew the experimental condition to which they were assigned. Pretest and posttest assessments were conducted in the home by a deaf educator or speech-language pathologist. Parents said statements during outcome testing that revealed their experimental condition to the assessor. As such, assessors were not naive to the experimental condition. However, two independent and naive raters scored 20% of all measures. Interobserver agreement was computed for all dependent variables using intraclass correlation coefficients (ICCs), which reflect the proportion of the variability in the reliability sample that is due to among-participant variance in true score estimates of the behavior of interest (Yoder & Symons, 2010). ICC for all dependent variables exceeded .80 and did not differ between experimental conditions, indicating that the potential for experimenter bias was low.
Child prelinguistic communication skills were measured using the Communication and Symbolic Behavior Scale Behavior Sample (Wetherby & Prizant, 2003) at baseline and after intervention. During this 30-min sample, the child was presented with toys and activities designed to elicit prelinguistic communication (e.g., pointing, gesturing, using coordinated eye contact, playing with toys). The interaction was video-recorded and then scored for 20 items (e.g., rate of communication, distal gestures) across seven prelinguistic domains (emotion and eye gaze, communication, gestures, sounds, spoken words, understanding, and object use). These seven domains were then grouped into three clusters: social (emotion and eye gaze, communication, gestures), speech (sounds, spoken words), and symbolic (understanding and object use). The weighted raw scores rather than the standard scores were used because the normative sample only included children between 12 and 24 months of age and many participants were below 12 months of age. ICCs for weighted scores were .82 for social, .95 for speech, and .97 for symbolic.
Parent use of communication strategies was measured by coding the middle 10 min of each parent–child interaction sample using an event-based behavior sampling procedure with Mangold INTERACT (Mangold, 2015), a software that allows frame-by-frame coding of observational data from videos. During the parent–child interaction samples, the parent and child played with a standard set of toys for 20 min. A standard set of toys (e.g., blocks, stacking cups, balls, stuffed animals) was chosen to facilitate the comparison of samples between parent and child dyads over time. Mothers were instructed to play as they usually would. The primary dependent variable was the percentage of adult utterances that included one of the treatment strategies listed in Table 2 during a video-recorded parent–child interaction at home. ICC for adult utterances containing an intervention strategy was .96.
Statistical Analyses
We anticipated 10% attrition and a sample size of 30 children. Assuming an α of .05 with a two-tailed test, 80% power, and a baseline covariate of .70 (based on correlations found in prior studies), a difference of 0.95 SD could be detected with 20 children (10 in each group). Data in both experimental conditions were analyzed using t tests to compare average gain scores between treatment and control groups for child and parent outcomes.
Results
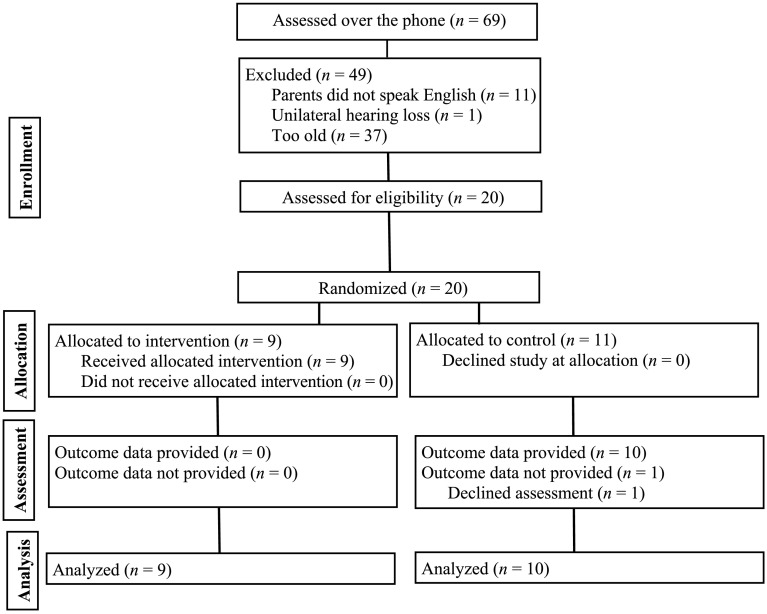
Figure 1 includes a CONSORT flow diagram, summarizing participants by study stage. Table 1 provides a summary of parent and child characteristics. There were no differences at baseline with regard to participant characteristics, as measured by t tests and chi-square tests. It is important to note that the p values for six out of 14 pretest comparisons were less than .50, which is recommended to ensure adequate matching (Mervis & Robinson, 2003). Of the 20 eligible children, nine were assigned to the treatment group, and 11 were assigned to the control group. All children in the treatment group (n = 9) and 91% of children in the control group (n = 10) remained in the study for the duration of intervention. All 19 participants were included in all analyses.
Figure 1.
CONSORT participant flowchart for the parent-implemented communication treatment project.
Parent Outcomes
Table 3 shows that parents in the treatment group increased their overall implementation of treatment strategies. The difference in parent use of treatment strategies between the treatment and control groups was large, with an effect size of 1.08 (p = .04). Parents in the treatment group increased their use of communication support strategies by 17%. This increase was substantially more than parents in the control group, whose strategy use increased by 2%.
Table 3.
Outcome comparisons.
| Outcomes | Intervention (n = 9) | Control (n = 10) | p | Effect size (d) a |
|---|---|---|---|---|
| Prelinguistic skills | ||||
| CSBS: Social gain scores | 19.93 (12.70) | 8.90 (13.43) | .08 | 0.78 |
| CSBS: Speech gain scores | 13.11 (12.00) | 3.80 (3.82) | .03 | 1.09 |
| CSBS: Symbolic gain scores | 9.67 (8.61) | 4.40 (3.98) | .10 | 0.91 |
| Caregiver gains in use of intervention strategies | 0.17 (0.10) | 0.02 (0.17) | .04 | 1.03 |
Note. CSBS = Communication and Symbolic Behavior Scale Behavior Sample.
Effect sizes for mean gain scores including pretest and posttest scores correlation were calculated using the Effect Size Determination Program from the Meta-Analysis Toolkit (Lipsey & Wilson, 2000). The pretest and posttest correlations were .412 for social scores, .495 for speech scores, .600 for symbolic scores, and .481 for caregiver use of intervention strategies.
Child Outcomes
Results from this study indicate improvement in prelinguistic skills (see Table 3). The difference in gains in speech prelinguistic skills between treatment and control groups was large with an effect size of 1.09 (p = .03). The differences in gains in social or symbolic prelinguistic skills between the treatment and control groups were not statistically significant (d = 0.78, p = .08; d = 0.91, p = .10). These nonsignificant results are likely due to the small sample size, as the study was only powered to detect an effect size of 0.95 or greater.
Discussion
This is the first randomized clinical trial of a parent-implemented treatment for infants and toddlers with hearing loss. 1 Parent use of treatment strategies led to benefits in child prelinguistic skills. Children in the treatment group had greater speech prelinguistic skills than children in the control group. These results are the first to indicate the potential benefits of providing systematic parent instruction during the prelinguistic period of language development for children with hearing loss. Over time, these stronger prelinguistic skills may facilitate later spoken language skills. Taken together, these preliminary findings suggest that effective early intervention goes beyond just the use of naturalistic communication support strategies with children with hearing loss, but that systematic parent instruction regarding the use of these strategies is critical to changing parent and child behaviors. As such, early interventionists working with children with hearing loss should (a) begin intervention as early as possible, ideally during the prelinguistic period of language development, and (b) include parents in the intervention process by coaching them to use communication support strategies.
Strengths
The elements of the treatment included naturalistic communication support strategies commonly used in early intervention and speech-language therapy. The treatment was standardized such that all parents and children received the same treatment, but also individualized to the developmental level of the infant. The frequency (once per week) is similar to existing early intervention service delivery models. The research design included randomization with minimal attrition. The inclusion of a control group that did not receive coaching enabled a better understanding of the unique effect of coaching on parent and child outcomes. Treatment fidelity was measured for both the interventionist and the parent, which ensured strong experimental control. These methodological strengths support high internal and external validity. As such, it is likely that these results may generalize to similar groups of children with hearing loss.
Limitations
Several limitations should be considered in relation to the current findings. First, randomization favored the control group on all dependent measures at baseline; the control group had higher scores on all Communication and Symbolic Behavior Scale Behavior Sample subscales at baseline. These large differences between groups at baseline may contribute to the lack of statistical significance in some of the dependent variables. Furthermore, the pretest p values indicate that the groups were not adequately matched on six out of 14 variables. Second, given the preliminary nature of this Phase 1 pilot study, the sample size is very small, and these results should be replicated with a greater number of children. Furthermore, the small sample size precludes the use of more sophisticated statistical analyses to control for pretest differences between experimental conditions. Third, parent behavior may have been influenced by their knowledge of the video recording. Fourth, long-term outcomes are needed to assess the impact of the intervention on long-term spoken language skills. Fifth, participant recruitment occurred over 2 years and included several recruitment sources (early intervention referral, self-referral, and physician referral). Families who chose to participate in the clinical trial may have been more motivated and compliant than others from the general population. Sixth, there is a potential for bias because the assessors and parents knew the experimental condition to which they were assigned. Seventh, because most of the participants were from mainstream U.S. cultures, the extent to which findings will generalize to parents and children from other cultures remains unknown.
Conclusions
The results of this study provide preliminary support for a PICT for infants and toddlers with hearing loss that includes teaching parents to use communication support strategies. Systematic instruction resulted in greater parent use of communication support strategies with their children with hearing loss. These strategies in turn had a large effect on speech prelinguistic communication skills. These results indicate that children with hearing loss are likely to benefit from intervention when provided early and when a parent is taught to use specific communication support strategies. This study was a first step in evaluating effective treatments for children with hearing loss who are at great risk for long-term spoken language difficulties. Long-term outcomes of the effects of the treatment is ongoing and will examine spoken language outcomes. While these results appear promising, the sample size is very small. Future research should include a larger clinical trial and include child-level predictors of response to treatment.
Acknowledgments
This study was funded by the National Institutes of Health Grant R03DC012639, awarded to Megan Y. Roberts (PI). All phases of this study were supported by Northwestern University.
Appendix
Fidelity Checklist
| Initial caregiver training session: TEACH | |
| Therapist reviews the target strategy within the context of the last session. | /5 |
| Therapist checks for understanding and invites caregiver questions before the session. | /5 |
| Therapist practice session: MODEL | |
| Therapist highlights the target strategy at least 10 times (2 points per highlight). | /20 |
| Therapist models the target strategy for 20 min (1 point per minute). | /20 |
| Caregiver practice session: COACH | |
| Therapist gives caregiver positive or training feedback at least once per minute (1 point per feedback). | /20 |
| Parent practices the target strategy for 20 min (1 point per minute). | /20 |
| Ending caregiver training session: REVIEW | |
| Therapist solicits questions/comments about the strategy and the session in general. | /5 |
| Therapist summarizes how the caregiver used the intervention strategy. | /5 |
| Total | /100 |
Funding Statement
This study was funded by the National Institutes of Health Grant R03DC012639, awarded to Megan Y. Roberts (PI). All phases of this study were supported by Northwestern University.
Footnote
Based on a literature search using Scopus on 5/1/2018 using the following search terms: (ABS ( “hearing loss” OR “hearing impaired” OR “deaf” OR “hard of hearing” ) AND ABS ( infant* OR child* OR toddler* ) AND ABS ( intervention* OR treatment* OR therapy ) AND ABS ( random* ) ).
References
- Albertini J. A. (2010). Deafness and hearing loss. In Weiner I. & Craighead W. (Eds.), The Corsini encyclopedia of psychology. Hoboken, NJ: Wiley. [Google Scholar]
- Ambrose S. E., VanDam M., & Moeller M. P. (2014). Linguistic input, electronic media, and communication outcomes of toddlers with hearing loss. Ear and Hearing, 35(2), 139–147. https://doi.org/10.1097/AUD.0b013e3182a76768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrose S. E., Walker E., Unflat-Berry L., Oleson J., & Moeller M. (2015). Quantity and quality of caregivers' linguistic input to 18-month and 3-year old children who are hard of hearing. Ear and Hearing, 36, 48S–59S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan-Jones C. G., White J., Rush R. W., & Law J. (2014). Auditory–verbal therapy for promoting spoken language development in children with permanent hearing impairments. Cochrane Database of Systematic Reviews, 2014(3), Article No. CD010100. https://doi.org/10.1002/14651858.CD010100.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cejas I., Barker D. H., Quittner A. L., & Niparko J. K. (2014). Development of joint engagement in young deaf and hearing children: Effects of chronological age and language skills. Journal of Speech, Language, and Hearing Research, 57(5), 1831–1841. https://doi.org/10.1044/2014_JSLHR-L-13-0262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching T. Y. C. (2015). Is early intervention effective in improving spoken language outcomes of children with congenital hearing loss? American Journal of Audiology, 24(3), 345–348. https://doi.org/10.1044/2015_AJA-15-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosson J., & Geers A. (2000). Structural analysis of narratives produced by a group of young cochlear implant users. The Annals of Otology, Rhinology & Laryngology, 109, 118–119. [DOI] [PubMed] [Google Scholar]
- Cruz I., Quittner A. L., Marker C., & DesJardin J. L. (2013). Identification of effective strategies to promote language in deaf children with cochlear implants. Child Development, 84(2), 543–559. https://doi.org/10.1111/j.1467-8624.2012.01863.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker K. B., Vallotton C. D., & Johnson H. A. (2012). Parents' communication decision for children with hearing loss: Sources of information and influence. American Annals of the Deaf, 157(4), 326–339. https://doi.org/10.1353/aad.2012.1631 [DOI] [PubMed] [Google Scholar]
- DesJardin J. L., Doll E. R., Stika C. J., Eisenberg L. S., Johnson K. J., Ganguly D. H., … Henning S. C. (2014). Parental support for language development during joint book reading for young children with hearing loss. Communication Disorders Quarterly, 35(3), 167–181. https://doi.org/10.1177/1525740113518062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DesJardin J. L., & Eisenberg L. S. (2007). Maternal contributions: Supporting language development in young children with cochlear implants. Ear and Hearing, 28(4), 456–469. https://doi.org/10.1097/AUD.0b013e31806dc1ab [DOI] [PubMed] [Google Scholar]
- Fagan M. K., Bergeson T. R., & Morris K. J. (2014). Synchrony, complexity and directiveness in mothers' interactions with infants pre- and post-cochlear implantation. Infant Behavior & Development, 37(3), 249–257. https://doi.org/10.1016/j.infbeh.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale E., & Schick B. (2009). Symbol-infused joint attention and language use in mothers with deaf and hearing toddlers. American Annals of the Deaf, 153(5), 484–503. https://doi.org/10.1353/aad.0.0066 [DOI] [PubMed] [Google Scholar]
- Geers A. E., Mitchell C. M., Warner-Czyz A., Wang N.-Y., Eisenberg L. S., & the CDaCI Investigative Team. (2017). Early sign language exposure and cochlear implantation benefits. Pediatrics, 140, e20163489 https://doi.org/10.1542/peds.2016-3489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geers A. E., Tobey E., Moog J., & Brenner C. (2008). Long-term outcomes of cochlear implantation in the preschool years: From elementary grades to high school. International Journal of Audiology, 47(Suppl. 2), S21–S30. https://doi.org/10.1080/14992020802339167 [DOI] [PubMed] [Google Scholar]
- Girolametto L., Pearce P. S., & Weitzman E. (1996). Interactive focused stimulation for toddlers with expressive vocabulary delays. Journal of Speech and Hearing Research, 39(6), 1274–1283. Retrieved from https://jslhr.pubs.asha.org/article.aspx?articleid=1781253 [DOI] [PubMed] [Google Scholar]
- Goldin-Meadow S., Goodrich W., Sauer E., & Iverson J. (2007). Young children use their hands to tell their mothers what to say. Developmental Science, 10(6), 778–785. https://doi.org/10.1111/j.1467-7687.2007.00636.x [DOI] [PubMed] [Google Scholar]
- Inscoe J. R., Odell A., Archbold S., & Nikolopoulos T. (2009). Expressive spoken language development in deaf children with cochlear implants who are beginning formal education. Deafness & Education International, 11(1), 39–55. https://doi.org/10.1002/dei.252 [Google Scholar]
- Iverson J. M., & Goldin-Meadow S. (2005). Gesture paves the way for language development. Psychological Science, 16(5), 367–371. https://doi.org/10.1111/j.0956-7976.2005.01542.x [DOI] [PubMed] [Google Scholar]
- Iyer S. N., & Oller D. K. (2008). Prelinguistic vocal development in infants with typical hearing and infants with severe-to-profound hearing loss. Volta Review, 108(2), 115–138. [PMC free article] [PubMed] [Google Scholar]
- Jackson C. W., & Schatschneider C. (2014). Rate of language growth in children with hearing loss in an auditory–verbal early intervention program. American Annals of the Deaf, 158(5), 539–554. https://doi.org/10.1353/aad.2014.0006 [DOI] [PubMed] [Google Scholar]
- Kaiser A. P. (1993). Parent-implemented language intervention: An environmental system perspective. In Kaiser A. & Gray D. (Eds.), Enhancing children's communication: Research foundations for intervention (pp. 63–84). Baltimore, MD: Brookes. [Google Scholar]
- Koester L. S., Brooks L. R., & Karkowski A. M. (1998). A comparison of the vocal patterns of deaf and hearing mother-infant dyads during face-to-face interactions. Journal of Deaf Studies and Deaf Education, 3(4), 290–301. https://doi.org/10.1093/oxfordjournals.deafed.a014357 [DOI] [PubMed] [Google Scholar]
- Lederberg A. R., & Mobley C. E. (1990). The effect of hearing impairment on the quality of attachment and mother-toddler interaction. Child Development, 61(5), 1596–1604. Retrieved from https://www.jstor.org/stable/1130767?seq=1#page_scan_tab_contents [DOI] [PubMed] [Google Scholar]
- Lipsey M., & Wilson S. (2000). Practical meta-analysis. Thousand Oaks, CA: Sage. [Google Scholar]
- Loots G., & Devisé I. (2003). The use of visual-tactile communication strategies by deaf and hearing fathers and mothers of deaf infants. Journal of Deaf Studies and Deaf Education, 8(1), 31–42. https://doi.org/10.1093/deafed/8.1.31 [DOI] [PubMed] [Google Scholar]
- Loots G., Devisé I., & Jacquet W. (2005). The impact of visual communication on the intersubjective development of early parent–child interaction with 18- to 24-month-old deaf toddlers. Journal of Deaf Studies and Deaf Education, 10(4), 357–375. https://doi.org/10.1093/deafed/eni036 [DOI] [PubMed] [Google Scholar]
- Luckner J. L., & Cooke C. (2010). A summary of the vocabulary research with students who are deaf or hard of hearing. American Annals of the Deaf, 155(1), 38–67. Retrieved from http://muse.jhu.edu/article/380119 [DOI] [PubMed] [Google Scholar]
- Lund E. (2016). Vocabulary knowledge of children with cochlear implants: A meta-analysis. Journal of Deaf Studies and Deaf Education, 21(2), 107–121. https://doi.org/10.1093/deafed/env060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangold P. (2015). INTERACT 14 user guide. Arnstorf, Germany: Mangold International. [Google Scholar]
- Markman T. M., Quittner A. L., Eisenberg L. S., Tobey E. A., Thal D., Niparko J. K., & Wang N.Y. (2011). Language development after cochlear implantation: An epigenetic model. Journal of Neurodevelopmental Disorders, 3(4), 388–404. https://doi.org/10.1007/s11689-011-9098-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzen-Derr J., Wiley S., & Choo D. I. (2011). Impact of early intervention on expressive and receptive language development among young children with permanent hearing loss. American Annals of the Deaf, 155(5), 580–591. https://doi.org/10.1353/aad.2011.0010 [DOI] [PubMed] [Google Scholar]
- Mellon N. K., Niparko J. K., Rathmann C., Mathur G., Humphries T., Napoli D. J., … Lantos J. D. (2015). Should all deaf children learn sign language? Pediatrics, 136(1), 170–176. https://doi.org/10.1542/peds.2014-1632 [DOI] [PubMed] [Google Scholar]
- Mervis C., & Robinson B. (2003). Methodological issues in cross-group comparisons of language and/or cognitive development. In Levy Y. & Schaeffer J. (Eds.), Language competence across populations: Toward a definition of specific language impairment (pp. 71–79). Mahwah, NJ: Erlbaum. [Google Scholar]
- Moeller M. P. (2000). Early intervention and language development in children who are deaf and hard of hearing. Pediatrics, 106(3), e43–e43. https://doi.org/10.1542/peds.106.3.e43 [DOI] [PubMed] [Google Scholar]
- Moeller M. P., Hoover B., Putman C., Arbataitis K., Bohnenkamp G., Peterson B., … Stelmachowicz P. (2007). Vocalizations of infants with hearing loss compared with infants with normal hearing: Part II—Transition to words. Ear and Hearing, 28(5), 628–642. https://doi.org/10.1097/AUD.0b013e31812564c9 [DOI] [PubMed] [Google Scholar]
- Mullen E. (1995). Mullen Scales of Early Learning. San Antonio, TX: Pearson. [Google Scholar]
- Nathani S., Oller D. K., & Neal A. R. (2007). On the robustness of vocal development: An examination of infants with moderate-to-severe hearing loss and additional risk factors. Journal of Speech, Language, and Hearing Research, 50(6), 1425–1444. https://doi.org/10.1044/1092-4388(2007/099) [DOI] [PubMed] [Google Scholar]
- Nicholas J. G., & Geers A. E. (2003). Hearing status, language modality, and young children's communicative and linguistic behavior. Journal of Deaf Studies and Deaf Education, 8(4), 422–437. https://doi.org/10.1093/deafed/eng029 [DOI] [PubMed] [Google Scholar]
- Niparko J. K., Tobey E. A., Thal D. J., Eisenberg L. S., Wang N.Y., Quittner A. L., & Fink N. E. (2010). Spoken language development in children following cochlear implantation. Journal of the American Medical Association, 303(15), 1498–1506. https://doi.org/10.1001/jama.2010.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nott P., Cowan R., Brown P. M., & Wigglesworth G. (2009). Early language development in children with profound hearing loss fitted with a device at a young age: Part I—The time period taken to acquire first words and first word combinations. Ear and Hearing, 30(5), 526–540. https://doi.org/10.1097/AUD.0b013e3181a9ea14 [DOI] [PubMed] [Google Scholar]
- Pagoto S., McDermott M. M., Reed G., Greenland P., Mazor K. M., Ockene J. K., … Ockene I. (2013). Can attention control conditions have detrimental effects in behavioral medicine randomized trials? Psychosomatic Medicine, 75(2), 137–143. https://doi.org/10.1097/PSY.0b013e3182765dd2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman L. J., Pipp-Siegel S., Yoshinaga-Itano C., & Deas A. (1999). Maternal sensitivity predicts language gain in preschool children who are deaf and hard of hearing. Journal of Deaf Studies and Deaf Education, 4(4), 294–304. https://doi.org/10.1093/deafed/4.4.294 [DOI] [PubMed] [Google Scholar]
- Quittner A. L., Cruz I., Barker D. H., Tobey E., Eisenberg L. S., & Niparko J. K. (2013). Effects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users' language development over four years. The Journal of Pediatrics, 162(2), 343–348. https://doi.org/10.1016/j.jpeds.2012.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M., & Hampton L. (2018). Exploring cascading effects of multimodal communication skills in infants with hearing loss. Journal of Deaf Studies and Deaf Education, 23, 95–105. https://doi.org/10.1093/deafed/enx041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M., & Kaiser A. (2015). Early intervention for toddlers with language delays: A randomized controlled trial. Pediatrics, 135, 686–693. https://doi.org/10.1542/peds.2014-2134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruben R. J., & Schwartz R. (1999). Necessity versus sufficiency: The role of input in language acquisition. International Journal of Pediatric Otorhinolaryngology, 47(2), 137–140. https://doi.org/10.1016/S0165-5876(98)00132-3 [DOI] [PubMed] [Google Scholar]
- Sacks C., Shay S., Repplinger L., Leffel K. R., Sapolich S. G., Suskind E., … Suskind D. (2014). Pilot testing of a parent-directed intervention (Project ASPIRE) for underserved children who are deaf or hard of hearing. Child Language Teaching and Therapy, 30(1), 91–102. https://doi.org/10.1177/0265659013494873 [Google Scholar]
- Spencer L. J., Barker B. A., & Tomblin J. B. (2003). Exploring the language and literacy outcomes of pediatric cochlear implant users. Ear and Hearing, 24(3), 236–247. https://doi.org/10.1097/01.AUD.0000069231.72244.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szagun G., & Schramm S. A. (2016). Sources of variability in language development of children with cochlear implants: Age at implantation, parental language, and early features of children's language construction. Journal of Child Language, 43(3), 505–536. https://doi.org/10.1017/S0305000915000641 [DOI] [PubMed] [Google Scholar]
- Szagun G., & Stumper B. (2012). Age or experience? The influence of age at implantation and social and linguistic environment on language development in children with cochlear implants. Journal of Speech, Language, and Hearing Research, 55(6), 1640–1654. https://doi.org/10.1044/1092-4388(2012/11-0119) [DOI] [PubMed] [Google Scholar]
- Tomblin J. B., Oleson J. J., Ambrose S. E., Walker E., & Moeller M. P. (2014). The influence of hearing aids on the speech and language development of children with hearing loss. JAMA Otolaryngology–Head & Neck Surgery, 140(5), 403–409. https://doi.org/10.1001/jamaoto.2014.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaccari C., & Marschark M. (1997). Communication between parents and deaf children: Implications for social-emotional development. Journal of Child Psychology and Psychiatry and Allied Disciplines, 38(7), 793–801. https://doi.org/10.1111/j.1469-7610.1997.tb01597.x [DOI] [PubMed] [Google Scholar]
- Vohr B., Jodoin-Krauzyk J., Tucker R., Johnson M. J., Topol D., & Ahlgren M. (2008). Early language outcomes of early-identified infants with permanent hearing loss at 12 to 16 months of age. Pediatrics, 122(3), 535–544. https://doi.org/10.1542/peds.2007-2028 [DOI] [PubMed] [Google Scholar]
- von Hapsburg D., & Davis B. L. (2006). Auditory sensitivity and the prelinguistic vocalizations of early-amplified infants. Journal of Speech, Language, and Hearing Research, 49(4), 809–822. https://doi.org/10.1044/1092-4388(2006/057) [DOI] [PubMed] [Google Scholar]
- Waxman R., & Spencer P. (1997). What mothers do to support infant visual attention: Sensitivities to age and hearing status. Journal of Deaf Studies and Deaf Education, 2(2), 104–114. https://doi.org/10.1093/oxfordjournals.deafed.a014311 [DOI] [PubMed] [Google Scholar]
- Wetherby A., & Prizant B. M. (2003). Communication and Symbolic Behavior Scales. Baltimore, MD: Brookes. [Google Scholar]
- Yoder P. J., & Symons F. (2010). Observational measurement of behavior. New York, NY: Springer. [Google Scholar]
- Yoder P. J., & Warren S. F. (2002). Effects of prelinguistic milieu teaching and parent responsivity education on dyads involving children with intellectual disabilities. Journal of Speech, Language, and Hearing Research, 45(6), 1158–1174. https://doi.org/10.1044/1092-4388(2002/094) [DOI] [PubMed] [Google Scholar]