Abstract
Purpose
The smartphone digits-in-noise hearing test, called hearZA, was made available as a self-test in South Africa in March 2016. This study determined characteristics and test performance of the listeners who took the test.
Method
A retrospective analysis of 24,072 persons who completed a test between March 2016 and August 2017 was conducted. User characteristics, including age, English-speaking competence, and self-reported hearing difficulty, were analyzed. Regression analyses were conducted to determine predictors of the speech reception threshold.
Results
Overall referral rate of the hearZA test was 22.4%, and 37% of these reported a known hearing difficulty. Age distributions showed that 33.2% of listeners were ages 30 years and younger, 40.5% were between ages 31 and 50 years, and 26.4% were older than 50 years. Age, self-reported English-speaking competence, and self-reported hearing difficulty were significant predictors of the speech reception threshold.
Conclusions
High test uptake, particularly among younger users, and high overall referral rate indicates that the hearZA app addresses a public health need. The test also reaches target audiences, including those with self-reported hearing difficulty and those with normal hearing who should monitor their hearing ability.
The global burden of hearing loss has been increasing steadily with close to half a billion people estimated to suffer from permanent disabling hearing loss (Vos et al., 2016; Vos et al., 2015; Wilson, Tucci, Merson, & O'Donoghue, 2017). The rise in recreational noise exposure further places an estimated 1.1 billion young people between the ages of 12 to 35 years at risk for acquiring hearing loss (World Health Organization [WHO], 2017). Regardless of high prevalence rates and significant consequences, hearing loss continues to be an undetected and untreated disability that is not adequately positioned or prioritized within many health care systems (Mackenzie & Smith, 2009). This is especially true in low- and middle-income countries (LMICs) where hearing health care is scarce or often unavailable due to the lack of resources and poor awareness among the lay public and health professionals (Mackenzie & Smith, 2009). Consequences of unaddressed hearing loss are far reaching, affecting social participation (Hallam, Ashton, Sherbourne, & Gailey, 2008), psychological well-being (Fellinger, Holzinger, & Pollard, 2012), cognitive function (Livingston et al., 2017), and employment opportunity (Tucci, Merson, & Wilson, 2010; WHO, 2017). With high proportions of occupations dependant on spoken communication (Ruben, 2015), the cumulative effects of hearing loss can have significant economic implications for the individual and society. Recent WHO estimates of the global estimated costs associated with hearing loss equaled 750 billion (WHO, 2017). Emphasis on prevention and treatment of hearing loss is, therefore, important on a global scale with particular focus on LMICs (Wilson et al., 2017).
Although it is well established that timely identification and management could substantially reduce the functional impairment of hearing loss (Cacciatore et al., 1999), most cases remain undiagnosed and untreated, especially in older adults (Pronk et al., 2011). Hearing screening programs have a critical role in monitoring hearing and early detection of hearing difficulty (WHO, 2017). However, implementation and success of these programs are reliant on specific human and technological resources such as trained screening personnel, audiologic equipment, and optimal quiet test environments. In addition, within LMICs, individuals may be required to travel substantial distances for hearing screening as health care providers are severely limited and unequally distributed (Mulwafu et al., 2017). The high costs involved and limited access to population-based hearing screening has led to various initiatives to use telephone- and Internet-based speech-in-noise (SIN) screening tests (Folmer et al., 2017; Jansen, Luts, Wagener, Frachet, & Wouters, 2010; Paglialonga, Tognola, & Grandori, 2014; Sheikh Rashid, Leensen, de Laat, & Dreschler, 2017; Smits, Kapteyn, & Houtgast, 2004; Vlaming, MacKinnon, Jansen, & Moore, 2014; Watson, Kidd, Miller, Smits, & Humes, 2012). Although all these tests measure speech recognition in noise, they vary in terms of speech stimuli, type of background noise, and test procedure. Compared with conventional pure-tone audiometry, SIN tests do not require calibrated equipment and also have the advantage of being less sensitive to ambient noise and transducer type (Jansen et al., 2010). Furthermore, SIN tests measure the functional deficits related to hearing loss as opposed to hearing sensitivity (Smits & Houtgast, 2005).The digits-in-noise (DIN) test is a type of SIN test that measures the speech reception threshold (SRT) where a listener can correctly identify 50% of digit triplets (e.g., 3–2–7) presented in speech noise. Compared with SIN tests that use sentences, English digits are easily understood, even in multilingual populations, making it less dependent on the listener's linguistic skills and suitable for a wide range of users (Smits, Theo Goverts, & Festen, 2013). The DIN was first developed for landline telephone use as Netherland's national hearing test in 2004 (Smits et al., 2004). Several telephone and online versions after that arose in countries such as the United States, Australia, Germany, France, and Poland (Folmer et al., 2017; Jansen et al., 2010; Smits, Merkus, & Houtgast, 2006; Watson et al., 2012; Zokoll, Wagener, Brand, Buschermöhle, & Kollmeier, 2012). A challenge related to telephone DIN tests, however, is insufficient landline coverage in LMICs. In South Africa, for example, only 13.9% of people have access to a landline telephone (Statistics South Africa, 2013). Capitalizing on rapid dispersal of low-cost smartphones with estimated 80% worldwide access by the year 2020 (The Economist, 2015), offering the DIN test as a smartphone application was a suitable alternative to landline testing. The first smartphone DIN test was made available in 2016 as South Africa's national hearing test, called hearZA (Potgieter, Swanepoel, Myburgh, Hopper, & Smits, 2016; Potgieter, Swanepoel, Myburgh, & Smits, 2017). The application can be completed within 3 min, correlates highly with pure-tone average (0.5, 1, 2, and 4 kHz), and has sensitivity and specificity over 90%, sufficient for population-based screening (Potgieter et al., 2016; Potgieter et al., 2017).
As a free downloadable application on Android and iOS app stores, hearZA has been marketed through sponsorships and endorsements by South African celebrities serving as hearing health ambassadors. The hearZA campaign and platform are utilized for several different purposes, of which hearing screening is only one. These purposes include serving as a (a) strategic public awareness tool for hearing health, (b) screening tool for hearing loss, (c) personal hearing profile for tracking hearing health, (d) decision support tool encouraging action on hearing loss developed in collaboration with the Ida Institute, and (e) location-based referral system to connect persons to their closest hearing health providers in partnership with national audiologic societies (Swanepoel, 2017).
Analysis of large-scale hearing screening programs, such as the hearZA national hearing test, can provide indications for test use, considerations for interpretation, and measures of reach. The purpose of the study was, therefore, to determine characteristics and test performance of individuals that have tested themselves with the hearZA national hearing test app.
Method
The study was reviewed and received ethical approval from the Faculty of Humanities Research Ethics Committee, University of Pretoria.
Participants
A retrospective analysis of 30,321 DIN tests completed from March 2016 to August 2017 was conducted. There were 297 listeners who indicated ages of 100 years and older, of which 283 incorrectly indicated ages of 2017 or 2018 years. The remaining 14 subjects had ages 100 up to 117 years. Their data, together with listeners who kept the application's default setting of 27 years, were excluded as incorrect data entries (n = 2175). Furthermore, 4,075 listeners who completed the test without headphones or earbuds were excluded to prevent confounding variables. This resulted in a total of 24,072 tests for analysis. The ages of the remaining sample ranged between 5 and 99 years (average: 39 years; SD = 16.6 years; n = 24,072). Listeners were further divided into two groups based on their self-rated level of English-speaking competence. English-speaking competence is rated on a nonstandardized visual analogue scale of 1 to 10, a lower score indicating poorer competence and a higher score indicating better competence. The two groups were (a) native (N) and nonnative (NN) ≥ 6 and (b) NN ≤ 5 (Potgieter et al., 2017). Pass–fail criteria were based on that of Potgieter et al. (2017), N and NN ≥ 6 with a cutoff of −9.55 dB, and N ≤ 5 with a cutoff of −7.5 dB.
Procedure
Listeners completed the DIN test by downloading the application on an Android- or iOS-operated smartphone. Individuals were made aware of the app due to marketing campaigns or word-of-mouth recommendations. Before the test, listeners were indicated to complete the test with either earbuds or headphones. Earlier versions of the app did not prevent test execution when earbuds or headphones were not plugged in, which was subsequently changed. The application requires listeners to provide their date of birth and home language and to rate their English-speaking competence on a nonstandardized scale of 1–10. Users were required to indicate whether they experience hearing difficulty by selecting “yes” or “no” on the application. After that, listeners self-select a comfortable listening intensity. Based on the comfort level selected, the application uses a fixed overall level with an adaptive signal-to-noise ratio (SNR; see Potgieter et al., 2016, for details). Masking noise is formed to match the long-term average speech spectrum of the digits. Speech signals are presented diotically. Listeners are expected to enter the digits heard on the smartphone, where a correct response will prompt the application to present the next digit at 2-dB lower SNR. Where the listener is uncertain of the digits heard, they are instructed to guess. When the response is incorrect, the application presents the next triplet at 2-dB higher SNR. The result is calculated by averaging the last 19 SNRs (Potgieter et al., 2016, 2017).
Statistics
Data analysis was completed using SPSS (Version 23.0). Results were analyzed using one-way analysis of variance and analysis of covariance. Post hoc comparisons were made using the Bonferroni adjustment. A p value of ≤ .05 was used to indicate significance. A multiple regression was performed for continuous and categorical variables to determine the predictors of the SRT result. The relationships between percentile SRTs and age were determined by following the procedure as described by Smits et al. (2013). Briefly, percentile values were calculated for 11-year age groups. These age groups were shifted in 1-year steps from 20 to 94 years. The percentile values were calculated for each age group, and a group-size weighted fit to an exponential growth function was performed.
Results
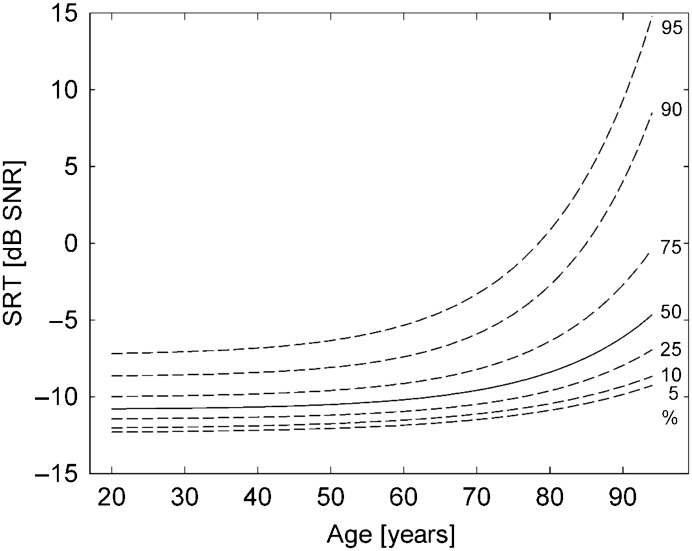
Approximately one in four persons (22.4%) who took the hearZA test (n = 24,072) failed based on normative data by Potgieter et al. (2017). Of persons for whom self-report of hearing status was available (n = 17,611), 37% reported a hearing difficulty of which 30.2% failed the test. Of those who did not self-report a hearing difficulty, 19.7% failed. The age distribution of persons taking the hearZA test (see Figure 1) indicated that 33.2% were 30 years of age and younger, 40.5% were between 31 and 50 years of age, whereas 26.4% were older than 50 years of age. Over 56 years, SRTs became worse, and referral rates rapidly increased (see Figure 2).
Figure 1.
Age distribution of persons taking the hearZA test (n = 24,072).
Figure 2.
The SRT against age group. Percentiles are shown. SRT = speech reception threshold; SNR = signal-to-noise ratio.
A one-way analysis of variance indicated a significant effect of age groups on the SRT results, F(5, 24066) = 182; p < .001. Listeners were further evaluated according to their level of English-speaking competence (n = 24,072). Most listeners selected English as their first language (n = 17,832). When divided into N and NN ≥ 6 (n = 22,737) and NN ≤ 5 (n = 1,335) groups based on the categories used by Potgieter et al. (2017), significant mean SRT differences between the two groups were found. NN ≤ 5 listeners performed significantly worse than N and NN ≥ 6 listeners (95% CI [1.1 to 1.6]; t(1,410.9) = −11.3; p < .001). Referral rate according to the cutoff criteria by Potgieter et al. (2017) increased with age group, the highest referral rates in the 51- to 60-year and 61- to 99-year groups (see Table 1). After adjustment for age and level of English-speaking competence, there was a statistically significant difference, F(2, 24,067) = 132.89; p < .001; partial η2 = .011, in SRTs between listeners without self-reported hearing difficulty (n = 11,089) and with a self-reported hearing difficulty (n = 6,522). SRTs in listeners with a self-reported hearing difficulty were significantly higher (−9.5 ± 0.04 dB SNR) than in listeners without a reported hearing difficulty (−10.2 ± 0.02 dB SNR), with a mean difference of 0.7 dB SNR (95% CI [0.6 to 0.8]), p < .001.
Table 1.
Mean speech reception thresholds (SRTs) and referral rates of native (N) and nonnative (NN) ≥ 6 and NN ≤ 5 English speakers according to age (referral according to Potgieter et al. [2017] norms).
| Age category in years (n) | Group mean SRT in dB SNR (SD) | Number of N/NN English listeners | Mean SRT in dB SNR (SD) | Referral rate (n) |
|---|---|---|---|---|
| 5–15 (1,441) | −8.5 (4.6) | N and NN ≥ 6: 1,275 | −8.7 (4.4) | No norms |
| NN ≤ 5: 166 | −7.2 (5.4) | |||
| 16–30 (6,543) | −10.2 (2.9) | N and NN ≥ 6: 6,217 | −10.3 (2.8) | 17.3% (1,076) |
| NN ≤ 5: 326 | −9 (4) | 30.7% (100) | ||
| 31–40 (5,893) | −10 (2.8) | N and NN ≥ 6: 5,629 | −10.2 (2.8) | 18.3% (1,030) |
| NN ≤ 5: 264 | −9.1 (3.8) | 31.8% (84) | ||
| 41–50 (3,840) | −9.8 (2.8) | N and NN ≥ 6: 3,662 | −10.1 (2.7) | 19.9% (729) |
| NN ≤ 5: 178 | −9.0 (4.4) | 30.9% (55) | ||
| 51–60 (3,279) | −9.8 (2.8) | N and NN ≥ 6: 3,082 | −9.8 (2.7) | 26.4% (814) |
| NN ≤ 5: 197 | −8.9 (3.4) | 40.6% (80) | ||
| 61–99 (3,670) | −8.7 (3.7) | N and NN ≥ 6: 2,872 | −8.8 (3.6) | 45.6% (1,309) |
| NN ≤ 5: 204 | −7.1 (5) | 57.4% (117) |
Note. SNR = signal-to-noise ratio.
A multiple regression was conducted to determine if English-speaking competence, self-reported hearing difficulty, and age were significant predictors of the SRT result. Data of 6,461 listeners who did not select whether they had a known hearing problem were excluded. In the remaining sample (n = 17,611), all the variables contributed significantly to the prediction, F(3, 17067) = 219.55, p < .001; adj. R2 = .04. Linear regression analysis for N and NN ≥ 6 (n = 19,430) and NN ≤ 5 (n = 1,413) listeners were conducted for the same variables. For N and NN ≥ 6 listeners, the model was significant, F(3, 16705) = 146.79, p < .001; adj. R2 = .02, with age (B = 0.02; 95% CI [0.016 to 0.021]; p < .001) and self-reported hearing difficulty (B = −0.53; 95% CI [−0.62 to −0.44]; p < .001) contributing significantly to the prediction. Overall, the model was also significant for NN ≤ 5 listeners, F(3, 898) = 13.66, p < .001; adj. R2 = .04, with age (B = 0.02; 95% CI [0.01 to 0.03]; p < .001), self-reported English-speaking competence rating (B = −0.47; 95% CI [−0.67 to −0.28]; p < .001), and self-reported hearing difficulty (B = −0.91; 95% CI [−1.46 to −0.35]) contributing significantly to the prediction.
Discussion
The hearZA national hearing test app had 30,321 persons tested from March 3, 2016, to August 14, 2017. Overall, the test had a referral rate of 22.4%. Compared with the 81% referral rate of the U.S. national hearing test (Watson et al., 2015), the referral rate of hearZA was low. It is possible that hearZA targets a younger population group, where the prevalence of hearing loss is still low, explaining the overall low SRTs across age groups. In the tests for which self-report of a hearing problem was available, 37% reported a known hearing difficulty. Most persons who took the test (40.5%) were between 31 and 50 years of age, and 27.2% were 30 years of age and younger. The median age of the listeners was 37 years. Compared with the Dutch National Hearing Test (Smits, Merkus et al., 2006), the median age in this analysis was lower than both the Internet (40 years) and telephone versions (54 years) of the test, suggesting the hearZA app is reaching a younger population. Over 50 years of age, test uptake dropped with less than a third (26.4%) of the sample in this category. The same pattern was seen for the Dutch National Hearing Test (Smits, Merkus et al., 2006). A study by Moore, Rothpletz, and Preminger (2015) linked poorer computer literacy with age among the elderly population. Although computer literacy does not necessarily relate to smartphone use, it reflects general digital literacy and limited ability and, perhaps, willingness to take self-testing using Internet technology. Physical restrictions, such as visual impairment and limited upper extremity dexterity, typical in the aging population, were also suggested contributors to the limited use of Internet-based health provision (Moore et al., 2015; Or et al., 2011). Of course, the hearZA marketing efforts, mostly on digital media, also bias the sample to younger populations.
Referral rates remained constant for N and NN English-speaking listeners between the ages of 16 and 50 years. Over the age of 50 years, however, hearing deteriorates quickly (Smits, Kramer, & Houtgast, 2006), and referral rates rapidly increase. In South Africa, a multilingual country with 11 official languages, N English speakers comprise only 9.6% of the population (Statistics South Africa, 2011). It was therefore interesting that the majority of listeners in this analysis selected English as their first language. One apparent reason for the high rate of listeners designated as N English speakers in the data set is the fact that it was the default setting on the hearZA app (changed subsequently). Mantonakis, Rodero, Lesschaeve, and Hastie (2009) investigated how the order of choices affects selection and found that most individuals are likely to select the first option in a sequence. Another possibility could be attributed to the fact that the test is reaching mostly N English speakers because marketing campaigns were conducted and distributed in an English medium. In line with the study of Potgieter et al. (2017), self-rated English-speaking competence was a significant predictor of the SRT. Even though some listeners may have kept the default selection of English as the first language, N and NN listeners with English-speaking competence equal or better than 6 still performed significantly better than NN listeners with ratings equal or lower than 5. The self-reported English-speaking competence rating was also a significant predictor in NN listeners with English-speaking competence ≤ 5, poorer scores showing poorer SRTs.
The high test uptake, especially among younger population groups, and the high overall referral rate (22.4%) indicate that the hearZA app is addressing a public health need. Although developed for adult users, there was a substantial sample (n = 1,275) of listeners under 15 years of age. The ability to understand speech in noise is an intrinsic attribute of the auditory system that matures with age (Talarico et al., 2007). Koopmans, Goverts, and Smits (2018) demonstrated the effect of age on the Dutch DIN test SRT for a group of more than 100 children with normal hearing. It will, therefore, be essential to determine age-specific norms of the test for the users between the ages of 5 and 15 years because it is clear that parents want to use it for this purpose. Age, self-reported English-speaking competence, and hearing difficulty were all significant factors influencing test outcomes. A limitation of this analysis, however, was that results assumed that listeners correctly entered personal information, such as date of birth, self-reported hearing problem, N language, and NN language English-speaking competence rating, over which researchers had no control. Furthermore, between the two groups with and without self-reported listening difficulty, although statistically different, the difference was small (0.7 dB). Large distributions of SRTs in both groups likely shifted the means of the two groups, another limitation of field testing. Moreover, Pronk, Deeg, and Kramer (2018) found that the self-report of hearing disability is influenced by other factors, such as demographics, personality, mood, and social situation, causing discrepancies between self-report and DIN test results. This could also possibly account for the small difference between the two groups. Lastly, considering the effect of self-reported English-speaking competence, the SRT cutoff criteria set out for N and NN speakers in Potgieter et al. (2017) are appropriate.
Overall, this study demonstrated widespread uptake of the hearZA app across age groups with a substantial number of persons self-reporting hearing problems (37%) and failing the test (22.4%). This means it is reaching an important target audience, those who think they have hearing loss. Conversely, it also reaches a high proportion of persons not yet presenting with a clear hearing problem but, having taken the test, are aware of their hearing status and can then track it through the app's personal profile (Swanepoel, 2017). Users are also reminded annually (via in-app notifications) to conduct follow-up tests allowing for longitudinal tracking and the possibility of early detection of hearing problems. A failed DIN test result has demonstrated positive influence on uptake of interventions (Smits & Houtgast, 2005; Watson et al., 2015). This method of self-testing should therefore promote increased self-efficacy and accessible hearing health behaviors among users.
Acknowledgments
Research reported in this publication was supported by the National Institute of General Medical Sciences Award 5R21DC016241-02, awarded to David R. Moore and De Wet Swanepoel. Portions of this article were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation.
Funding Statement
Research reported in this publication was supported by the National Institute of General Medical Sciences Award 5R21DC016241-02, awarded to David R. Moore and De Wet Swanepoel.
References
- Cacciatore F., Napoli C., Abete P., Marciano E., Triassi M., & Rengo F. (1999). Quality of life determinants and hearing function in an elderly population: Osservatorio Geriatrico Campano Study Group. Gerontology, 45(6), 323–328. [DOI] [PubMed] [Google Scholar]
- Fellinger J., Holzinger D., & Pollard R. (2012). Mental health of deaf people. The Lancet, 379(9820), 1037–1044. [DOI] [PubMed] [Google Scholar]
- Folmer R. L., Vachhani J., McMillan G. P., Watson C., Kidd G. R., & Feeney M. P. (2017). Validation of a computer-administered version of the digits-in-noise test for hearing screening in the United States. Journal of the American Academy of Audiology, 28(2), 161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallam R., Ashton P., Sherbourne K., & Gailey L. (2008). Persons with acquired profound hearing loss (APHL): How do they and their families adapt to the challenge? Health, 12(3), 369–388. [DOI] [PubMed] [Google Scholar]
- Jansen S., Luts H., Wagener K. C., Frachet B., & Wouters J. (2010). The French digit triplet test: A hearing screening tool for speech intelligibility in noise. International Journal of Audiology, 49(5), 378–387. [DOI] [PubMed] [Google Scholar]
- Koopmans W. J., Goverts S. T., & Smits C. (2018). Speech recognition abilities in normal-hearing children 4 to 12 years of age in stationary and interrupted noise. Ear and Hearing. Epub ahead of print. https://doi.org/10.1097/AUD.0000000000000569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston G., Sommerlad A., Orgeta V., Costafreda S. G., Huntley J., Ames D., … Cooper C. (2017). Dementia prevention, intervention, and care. The Lancet, 390(10113), 2673–2734. [DOI] [PubMed] [Google Scholar]
- Mackenzie I., & Smith A. (2009). Deafness—The neglected and hidden disability. Annals of Tropical Medicine and Parasitology, 103(7), 565–571. [DOI] [PubMed] [Google Scholar]
- Mantonakis A., Rodero P., Lesschaeve I., & Hastie R. (2009). Order in choice: Effects of serial position on preferences. Psychological Science, 20(11), 1309–1312. [DOI] [PubMed] [Google Scholar]
- Moore A. N., Rothpletz A. M., & Preminger J. E. (2015). The effect of chronological age on the acceptance of Internet-based hearing health care. American Journal of Audiology, 24(3), 280–283. [DOI] [PubMed] [Google Scholar]
- Mulwafu W., Ensink R., Kuper H., & Fagan J. (2017). Survey of ENT services in sub-Saharan Africa: Little progress between 2009 and 2015. Global Health Action, 10(1), 1289736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Or C. K., Karsh B. T., Severtson D. J., Burke L. J., Brown R. L., & Brennan P. F. (2011). Factors affecting home care patients' acceptance of a web-based interactive self-management technology. Journal of the American Medical Informatics Association, 18(1), 51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paglialonga A., Tognola G., & Grandori F. (2014). A user-operated test of suprathreshold acuity in noise for adult hearing screening: The SUN (Speech Understanding in Noise) test. Computers in biology and medicine, 52, 66–72. [DOI] [PubMed] [Google Scholar]
- Potgieter J. M., Swanepoel D. W., Myburgh H. C., Hopper T. C., & Smits C. (2016). Development and validation of a smartphone-based digits-in-noise hearing test in South African English. International Journal of Audiology, 55, 405–411. [DOI] [PubMed] [Google Scholar]
- Potgieter J. M., Swanepoel D. W., Myburgh H. C., & Smits C. (2017). The South African English Smartphone Digits-in-Noise Hearing Test: Effect of age, hearing loss and speaking competence. Ear and Hearing, 39(4), 656–663. [DOI] [PubMed] [Google Scholar]
- Pronk M., Deeg D. J., & Kramer S. E. (2018). Explaining discrepancies between the Digit Triplet Speech-in-Noise Test Score and self-reported hearing problems in older adults. Journal of Speech, Language, and Hearing Research, 1–14. [DOI] [PubMed] [Google Scholar]
- Pronk M., Kramer S. E., Davis A. C., Stephens D., Smith P. A., Thodi C., … Grandori F. (2011). Interventions following hearing screening in adults: A systematic descriptive review. International Journal of Audiology, 50(9), 594–609. [DOI] [PubMed] [Google Scholar]
- Ruben R. J. (2015). How did otolaryngology-head & neck surgery become an essential medical discipline for the 21st century? International Journal of Pediatric Otorhinolaryngology, 79(6), 783–785. [DOI] [PubMed] [Google Scholar]
- Sheikh Rashid M., Leensen M. C., de Laat J. A., & Dreschler W. A. (2017). Laboratory evaluation of an optimised Internet-based speech-in-noise test for occupational high-frequency hearing loss screening: Occupational earcheck. International Journal of Audiology, 56(11), 844–853. [DOI] [PubMed] [Google Scholar]
- Smits C., & Houtgast T. (2005). Results from the Dutch Speech-in-Noise Screening Test by telephone. Ear and Hearing, 26(1), 89–95. [DOI] [PubMed] [Google Scholar]
- Smits C., Kapteyn T. S., & Houtgast T. (2004). Development and validation of an automatic speech-in-noise screening test by telephone. International Journal of Audiology, 43(1), 15–28. [DOI] [PubMed] [Google Scholar]
- Smits C., Kramer S. E., & Houtgast T. (2006). Speech reception thresholds in noise and self-reported hearing disability in a general adult population. Ear and Hearing, 27(5), 538–549. [DOI] [PubMed] [Google Scholar]
- Smits C., Merkus P., & Houtgast T. (2006). How we do it: The Dutch functional hearing–screening tests by telephone and Internet. Clinical Otolaryngology, 31(5), 436–440. [DOI] [PubMed] [Google Scholar]
- Smits C., Theo Goverts S., & Festen J. M. (2013). The digits-in-noise test: Assessing auditory speech recognition abilities in noise. The Journal of the Acoustical Society of America, 133(3), 1693–1706. [DOI] [PubMed] [Google Scholar]
- Statistics South Africa. (2011). Census in brief, South Africa. Retrieved from http://www.statssa.gov.za/publications/P03014/P030142011.pdf
- Statistics South Africa. (2013). General Household Survey. Retrieved from: http://www.statssa.gov.za/publications/P0318/P03182013.pdf
- Swanepoel D. W. (2017). Smartphone-based National Hearing Test launched in South Africa. The Hearing Journal, 70(1), 14–16. [Google Scholar]
- Talarico M., Abdilla G., Aliferis M., Balazic I., Giaprakis I., Stefanakis T., … Paolini A. G. (2007). Effect of age and cognition on childhood speech in noise perception abilities. Audiology and Neurotology, 12(1), 13–19. [DOI] [PubMed] [Google Scholar]
- The Economist. (2015). Planet of the phones. Retrieved from http://www.economist.com/news/leaders/21645180-smartphone-ubiquitous-addictive-and-transformative-planet-phones
- Tucci D. L., Merson M. H., & Wilson B. S. (2010). A summary of the literature on global hearing impairment: Current status and priorities for action. Otology & Neurotology, 31(1), 31–41. [DOI] [PubMed] [Google Scholar]
- Vlaming M. S., MacKinnon R. C., Jansen M., & Moore D. R. (2014). Automated screening for high-frequency hearing loss. Ear and Hearing, 35(6), 667–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T., Allen C., Arora M., Barber R. M., Bhutta Z. A., … Murray C. J. (2016). Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet, 389(10064), 1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T., Barber R. M., Bell B., Bertozzi-Villa A., Biryukov S., Bolliger I., … Dicker D. (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet, 386(9995), 743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson C. S., Kidd G. R., Miller J. D., Smits C., & Humes L. E. (2012). Telephone screening tests for functionally impaired hearing: Current use in seven countries and development of a US version. Journal of the American Academy of Audiology, 23(10), 757–767. [DOI] [PubMed] [Google Scholar]
- Watson C. S., Kidd G. R., Preminger J. E., Miller J. D., Maki D. P., & Crowley A. (2015). Benefits of a telephone-administered national screening test. Audiology Online, 27(6), 1–8. [Google Scholar]
- Wilson B. S., Tucci D. L., Merson M. H., & O'Donoghue G. M. (2017). Global hearing health care: New findings and perspectives. The Lancet, 309(10111), 2503–2515. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Deafness and Hearing Loss Factsheet. Retrieved from http://www.who.int/mediacentre/factsheets/fs300/en/
- Zokoll M. A., Wagener K. C., Brand T., Buschermöhle M., & Kollmeier B. (2012). Internationally comparable screening tests for listening in noise in several European languages: The German digit triplet test as an optimization prototype. International Journal of Audiology, 51(9), 697–707. [DOI] [PubMed] [Google Scholar]