Abstract
Purpose
Teleaudiology helps connect patients in rural and underresourced areas to hearing health care providers, minimizing the barrier of geography (Swanepoel et al., 2010). In the United States, teleaudiology is at the initial stages of implementation (Bush, Thompson, Irungu, & Ayugi, 2016). Telehealth researchers recommend conducting a comprehensive planning assessment to optimize implementation and adoption (AlDossary, Martin-Khan, Bradford, Armfield, & Smith, 2017; Alverson et al., 2008; Krupinski, 2015). A geographic analysis of the hearing aid dispensing workforce served as the initial stage of a teleaudiology planning assessment in Arizona.
Method
The analysis used publically available data sets from the U.S. Census, Arizona Department of Health Services, and the U.S. Veterans Administration. Geographic information system tools were used to analyze and visually represent population, potential teleaudiology site data, and hearing aid dispensing workforce (defined as audiologists and hearing instrument specialists licensed to dispense hearing aids in Arizona). ArcGIS was used to generate road networks and travel distance estimations.
Results
The number of audiologists per county ranged from 0 to 216 (average 22.1). Six out of Arizona's 15 counties lacked a single audiologist, and 2 counties lacked a hearing instrument specialist. Potential expansion sites for teleaudiology were located in areas of the state that lacked practice locations for hearing aid services.
Conclusions
There are geographic areas of Arizona that lack licensed hearing aid locations yet are populated by individuals who may need services. Resource availability data inform teleaudiology program expansion. Future research will include data from providers and community members on their perceived needs for services.
A research has shown that a number of health care fields are impacted by disparities in access, including hearing health care (National Academies of Sciences, Engineering, and Medicine, 2016). Such disparities in access to care may occur as differences in utilization of services or, more fundamentally, in terms of the availability of the services themselves. It is known that an individual's geographic proximity to a provider can affect his or her access to health care services (Gulliford et al., 2002). An estimated 20% of the U.S. population lives rurally, yet health care providers are more likely to practice in urbanized areas (Rosenblatt, Andrilla, Curtin, & Hart, 2006). There are currently an estimated 14,600 audiologists nationwide (Bureau of Labor Statistics, U.S. Department of Labor, 2017). According to a supply-and-demand projection, it was estimated that the number of audiologists should double in the next 30 years to meet the needs of the growing patient population (Windmill & Freeman, 2013). Research has also indicated patients in rural areas may receive delayed hearing health care services compared with patients in urban areas (S. Chan, Hixon, Adkins, Shinn, & Bush, 2017; Hixon, Chan, Adkins, Shinn, & Bush, 2016). Improvements in service delivery may lead to more timely intervention for older adults with hearing loss and increase the number of individuals who are fit with hearing aids, a national priority set by Healthy People 2020 (n.d.).
One strategy that has shown to improve access to services for patients living rurally is telehealth (Merrell & Doarn, 2008; Smith & Gray, 2009). A number of medical subspecialties have adopted telehealth, including radiology (Stahl et al., 2017), psychiatry (Yellowlees et al., 2017), and dermatology (Leavitt et al., 2016). Teleaudiology, or the remote delivery of hearing health services, has shown to minimize accessibility barriers related to geography, such as lack of transportation and limited availability of audiologists (Swanepoel et al., 2010). In addition, research has established the validity of a number of audiologic services delivered via teleaudiology as compared with in-person services, including hearing aid fittings (Campos & Ferrari, 2012; Dennis, Gladden, & Noe, 2012). Teleaudiology is in the early stages of implementation in the United States (Bush, Thompson, Irungu, & Ayugi, 2016). The U.S. Veterans Administration (VA) has been at the forefront of the development and implementation of teleaudiology and has demonstrated that it can help lower costs and increase accessibility (Dennis et al., 2012; Gladden, 2013; Gladden, Beck, & Chandler, 2015).
To optimize the implementation of telehealth interventions, it has been recommended to conduct a comprehensive planning assessment (AlDossary, Martin-Khan, Bradford, Armfield, & Smith, 2017; Alverson et al., 2008; Krupinski, 2015; N. Soares, Dewalle, & Marsh, 2017). For example, AlDossary et al. outlined a theory-based telehealth planning framework, based on a survey of the population (potential client base), workforce, transportation systems at local patient sites, and potential opportunities for expansion (AlDossary et al., 2017). In addition, the authors recommend consulting with key stakeholders within the target community to set priorities for a potential intervention.
The purpose of this report is to present results from a geographic analysis of population, workforce, and clinic sites as part of a teleaudiology planning assessment for Arizona. Because professional licensure and hearing aid dispensing laws in the United States are state specific, we focused our analysis at a state level. Previous studies have identified rural/urban differences in workforce distribution across the country in primary care and otolaryngology (Vickery & Cabrera-Muffly, 2016). In addition, a community needs assessment in a rural part of Arizona identified that there is a high need for hearing health care services locally (Ingram et al., 2016). Therefore, we hypothesized that members of the hearing aid dispensing workforce would be concentrated to more densely populated areas of the state. For this planning assessment, the analysis focused on the workforce licensed to dispense hearing aids in Arizona relative to one of the largest populations to access hearing aids, adults over age 65 years (Lin, Thorpe, Gordon-Salant, & Ferrucci, 2011).
Telehealth researchers recommend including a pragmatic selection of local patient sites as a method for optimizing implementation and adoption of the intervention (Van Dyk, 2014; Yellowlees, 2005). There are at least two national community clinic networks known to have wide reach of individuals who live rurally: Community-Based Outpatient Clinics and Federally Qualified Health Centers. First, Community-Based Outpatient Clinics are nonhospital local providers of basic health care for U.S. Veterans (Centers for Medicare & Medicaid Services, 2018; Hedeen et al., 2002). There are over 1,000 Community-Based Outpatient Clinics serving Veterans across the United States, 20% of whom report they live rurally (Holder, 2017). For non-Veterans, an estimated 20 million individuals receive health care services at 6,000 Federally Qualified Health Center sites across the United States (Doty, Abrams, Hernandez, Stremikis, & Beal, 2010). These community clinics are located in federally designated Health Professional Shortage Areas (HPSAs) and are therefore eligible to receive federal reimbursements for delivering health services to all individuals, regardless of ability to pay (Health Resources & Services Administration, 2018). We include these sites in the planning assessment to demonstrate potential opportunities for teleaudiology expansion.
This project involves the use of geographic information system (GIS) tools—computer programs used to process, transform, edit, and analyze datasets with spatial components and attributes—to identify the county-level geographic locations of members of the audiology and hearing instrument specialist workforce and older adults with hearing loss. In addition, we calculated the distance an older adult with hearing loss would need to travel to reach the nearest hearing aid dispensing provider. GIS tools have been used previously to describe health care utilization and access (McLafferty, 2003), including in telehealth program planning (Ripley et al., 2014; N. S. Soares, Johnson, & Patidar, 2013). However, this is the first known implementation of GIS tools for a teleaudiology planning assessment.
Method
Data Sources for Population, Workforce, and Clinic Locations
This was a retrospective analysis of population, workforce, and clinic location data. Population data were obtained from the U.S. Census, using population estimates for 2017 (U.S. Census, 2017). The U.S. Census generates annual population estimates based on the most recent U.S. Census (2010). Estimates are created using a number of indicators, including migration patterns, Medicare enrollment data, and tax return data. To demonstrate population geographically, we adopted the U.S. Department of Agriculture's Rural–Urban Continuation Codes (RUCC) classification system. Each county in the United States is assigned one of nine codes based on its metropolitan or nonmetropolitan status and population size. Counties in Arizona fell into six of these nine categories (U.S. Department of Agriculture, 2016). To calculate the estimated population of individuals ≥ 65 years in Arizona who have hearing loss, we interpolated national audiometric prevalence data from the National Health and Nutrition Examination Surveys, published by Lin et al. (2011).
Here, workforce was defined as individuals who hold the state licensure to dispense hearing aids in Arizona: audiologists and hearing instrument specialists. Audiologists are licensed to deliver specialty care, including comprehensive diagnostic audiometry, pediatric care, vestibular rehabilitation, and cochlear implant programming. Arizona audiologists who fit and dispense hearing aids must pursue an additional “dispensing audiologist” license. By contrast, hearing instrument specialists are licensed as “hearing aid dispensers” with a scope of practice that is limited to specific hearing aid services, such as basic hearing tests for the sole purpose of dispensing hearing aids to adults and fit and sell hearing aids. Nationally, there are an estimated 12,000 audiologists and 7,000 hearing instrument specialists (Bureau of Labor Statistics, U.S. Department of Labor, 2017). To identify county-level locations of audiologists and hearing instrument specialists, we used a publicly available dataset maintained by the Arizona Department of Health Services (ADHS, 2017b). Locations were identified as registered practice addresses for individuals holding active dispensing audiology licenses or hearing aid dispenser licenses. Data were accessed on June 17, 2017, and were based on an update made on June 1, 2017. Federally Qualified Health Center locations were obtained from the ADHS Shortage Designation Program Mapper, a publically available online tool used for visualization of health care resources (ADHS, 2017a). Data were accessed on June 17, 2017. Location data for Community-Based Outpatient Clinics were obtained from a publically available facilities directory, accessed on September 8, 2017 (U.S. VA, 2015).
Geographic Analysis of Data and Travel Distance Estimations
To demonstrate the geographic distribution of the population of Arizona, the workforce distribution, and the potential expansion locations for teleaudiology, maps were created using ArcMap (Version 10.5), a GIS software system produced by the Environmental Systems Research Institute (2017). Data from the U.S. Census were tabulated and input into ArcMap. To describe license locations, we exported tabulated ADHS data that contained the longitudinal and latitudinal coordinates of audiologists' and hearing instrument specialists' license locations into ArcMap. For a small subset of licensees, only zip code data were provided (audiologists = 23 and hearing instrument specialists = 7). For these sites, latitude and longitude were approximated to the centerpoint of the corresponding zip code.
We utilized GIS tools and the Arizona road network to estimate average travel distance to the nearest member of the hearing aid workforce. To calculate the travel distance, we used the “Find Nearest Feature” network analyst tool in ArcGIS. Three points are used to identify the shortest path distance between the given origin–destination pair: “origin,” “route,” and “destination.” To generate origin points, we used the estimated population of individuals ≥ 65 years with hearing loss. To fit within the computational power of our analyses, a stratified random selection of 10,000 individuals from the full target population was created. The resulting subsample was proportionally represented in each county as origin points (e.g., Maricopa County has 53.7% of the total estimated population ≥ 65 years with hearing loss and, therefore, received 53.7% of the 10,000 sample points). Origin points were distributed equidistant from each other. Destination points were considered license locations of individual licensed audiologists and hearing instrument specialists (n = 879). The route network was constructed using an up-to-date nationwide road dataset acquired from Environmental Systems Research Institute ArcMap's online database. To demonstrate distance variation within counties, data were shown as a choropleth map, with lighter gradations of color representing further travel distance, using increments of 25 mi.
Results
Population
As shown in Table 1, Arizona has a population of 7,016,270 across 15 counties. Maricopa, where the state's capitol Phoenix is located, is the most densely populated county, with 60% of the state's population (population: 4,307,033). The second most densely populated county is Pima, where 15% of the state's total population lives (population: 1,022,769). Arizona's six metro counties make up 89% of the state's total population, whereas nine nonmetro counties account for just 10% of the total statewide population. The estimated population of individuals ≥ 65 years with unilateral or bilateral hearing loss ranged from 737 (Greenlee) to 414,936 (Maricopa), with a statewide total estimate of 780,829 older adults with hearing loss. The distribution of individuals ≥ 65 years per county ranged from 12% (Coconino) to 38% (La Paz).
Table 1.
Details of the Arizona population and hearing aid dispensing workforce by county.
| Arizona County | Population a | Estimated population ≥ 65 years with hearing loss b |
Audiologists c | Hearing instrument specialists c | Person-to-provider ratio
d
|
|
|---|---|---|---|---|---|---|
| Audiologists | Hearing instrument specialists | |||||
| Apache | 71,606 | 5,585 | 0 | 2 | — | 2,793:1 |
| Cochise | 124,756 | 17,029 | 6 | 4 | 2,838:1 | 4,257:1 |
| Coconino | 140,776 | 10,981 | 13 | 14 | 845:1 | 784:1 |
| Gila | 53,501 | 9,737 | 0 | 4 | — | 2,434:1 |
| Graham | 37,466 | 3,166 | 0 | 1 | — | 3,166:1 |
| Greenlee | 9,455 | 737 | 0 | 0 | — | — |
| La Paz | 20,601 | 5,088 | 0 | 0 | — | — |
| Maricopa | 4,307,033 | 419,936 | 216 | 335 | 1,944:1 | 1,254:1 |
| Mohave | 207,200 | 39,057 | 3 | 22 | 13,019:1 | 1,775:1 |
| Navajo | 108,956 | 12,040 | 4 | 2 | 3,010:1 | 6,020:1 |
| Pima | 1,022,769 | 126,312 | 77 | 109 | 1,640:1 | 1,159:1 |
| Pinal | 430,237 | 55,931 | 5 | 12 | 11,186:1 | 4,661:1 |
| Santa Cruz | 46,212 | 5,106 | 0 | 2 | — | 2,553:1 |
| Yavapai | 228,168 | 44,493 | 3 | 27 | 14,831:1 | 1,648:1 |
| Yuma | 207,534 | 25,630 | 5 | 13 | 5,126:1 | 1,972:1 |
| State Total | 7,016,270 | 780,829 | 332 | 547 | — | — |
Note. Em dashes indicate zero denominator.
U.S. Census annual estimates of the resident population: April 1, 2010, to July 1, 2017 (U.S. Census, 2017).
Applying National Health and Nutrition Examination Survey estimates for individuals with unilateral or bilateral hearing loss (Lin et al., 2011).
Audiologists and hearing instrument specialists with licenses to dispense hearing aids in Arizona as of June 17, 2017 (Arizona Department of Health Services, 2017b).
Estimated population ≥ 65 with hearing loss per audiologist and per hearing instrument specialist.
Hearing Aid Dispensing Workforce
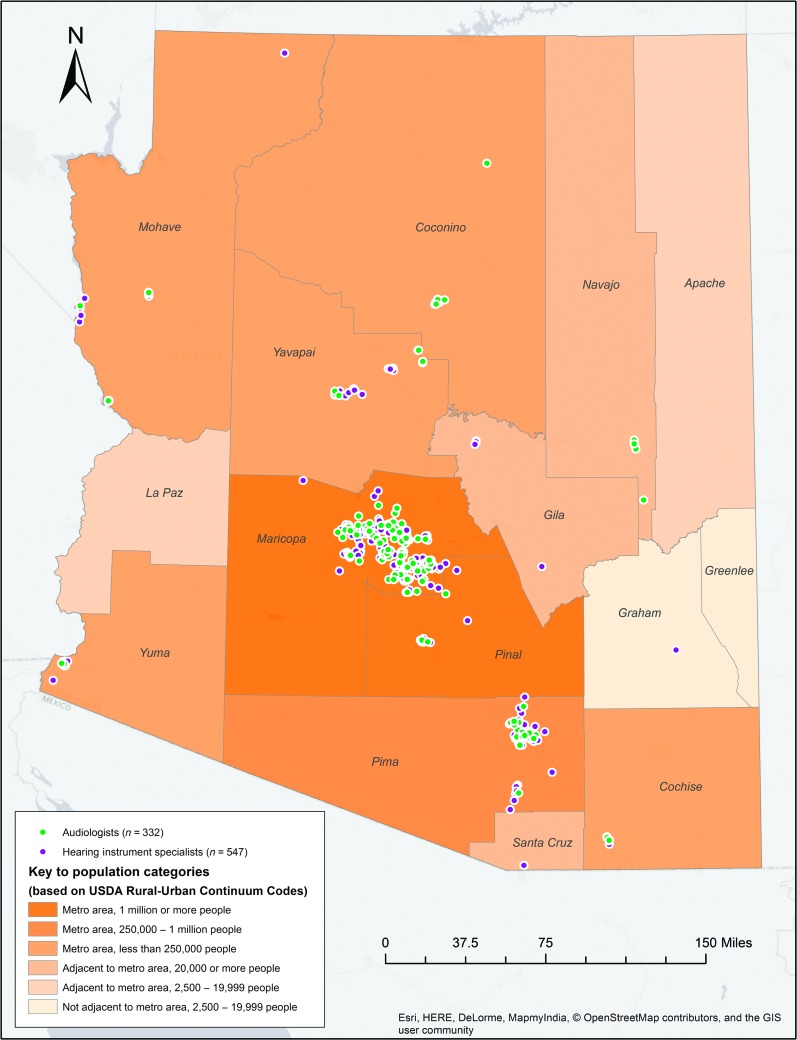
A map of Arizona with the geographic practice locations of audiologists and hearing instrument specialists and population density across Arizona is provided in Figure 1. At the time of the analysis, there were a total of 332 audiologists and 547 hearing instrument specialists licensed to dispense hearing aids in Arizona. There was an average of 22.1 audiologists per county (range: 0 to 216). Most of the audiologists (216) were in the county with the highest population (Maricopa). Six out of the state's 15 counties (40%) had not a single audiologist. The average population in the counties that had 0 audiologists was 39,780 people (range: 8,437 to 53,597). Across Arizona, there was an average of 36.5 hearing instrument specialists per county (range: 0 to 335). The county with the greatest population, Maricopa, also had the greatest number of hearing instrument specialists (335). Two counties had not a single hearing instrument specialist (Greenlee, population: 9,455 and La Paz, population: 20,601). Neither of these counties had an audiologist. Combining audiologists and hearing instrument specialists (n = 879) revealed that 94% (829) were located in Arizona's six metro counties, whereas just 6% were located in Arizona's nine nonmetro counties.
Figure 1.
Practice locations of audiologists and hearing instrument specialists licensed to dispense hearing aids. Total Arizona population is shown, using the U.S. Department of Agriculture's (USDA) Rural–Urban Continuum Code system. Only codes represented in Arizona are illustrated.
Person-to-Provider Ratio
We calculated the ratio of the estimated population ≥ 65 years with hearing loss per audiologist and per hearing instrument specialist. For the nine counties with audiologists, the average ratio was 6,049:1 (SD = 5,119), with a range of 845:1 (Coconino) to 14,831:1 (Yavapai). For the 13 counties with hearing instrument specialists, the average ratio was 2,652:1 (SD = 1,473), with a range of 784:1 (Coconino) to 6,020:1 (Navajo).
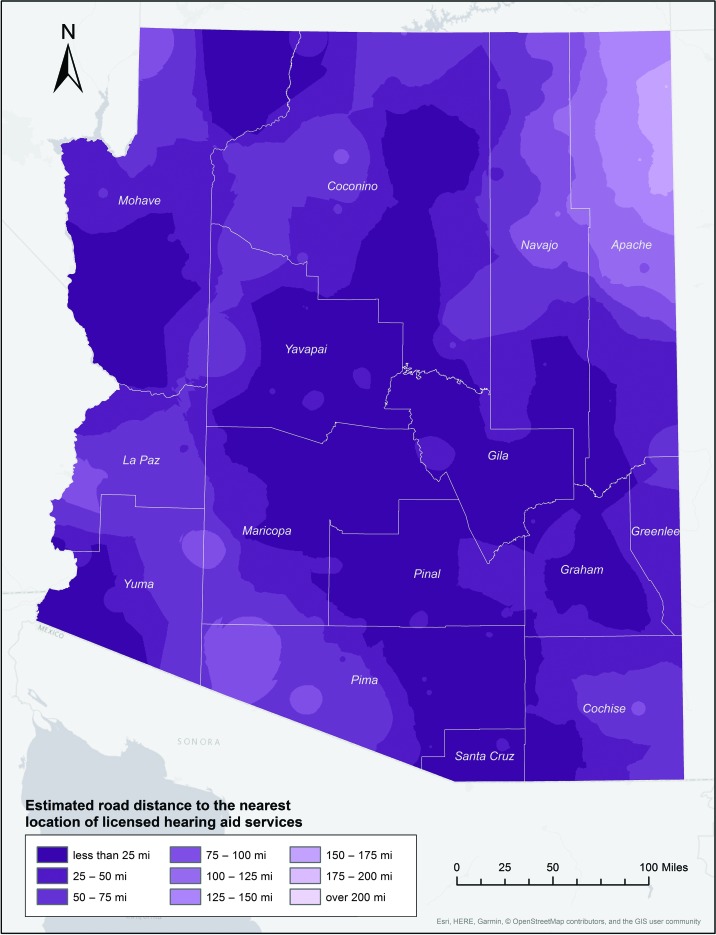
Estimated Travel Distance
Road travel distances were calculated for the estimated population of individuals ≥ 65 years with hearing loss to the nearest hearing aid dispensing provider. Average travel distance results are represented in Figure 2 as a graduated color (choropleth) map. Travel distance calculations were first performed for audiologists and hearing instrument specialists separately. Across Arizona's 15 counties, the average travel distance was 46.1 mi to an audiologist and 36.34 mi to a hearing instrument specialist. A two-tailed independent-samples t test of the difference between groups was not significant (p = .2308). We then calculated the average travel distance a potential patient would need to travel to reach either an audiologist or hearing instrument specialists (closest of the two). Results revealed that the average travel distance was 23.84 mi across Arizona's 15 counties. Travel distances were calculated to be as short as 2.30 mi (Maricopa) and as long as 118.90 mi (Apache). Six out of Arizona's 15 counties had average travel distances greater than 20 mi.
Figure 2.
Estimated road travel distances for the estimated population of individuals age ≥ 65 years with hearing loss to the nearest location of licensed hearing aid services.
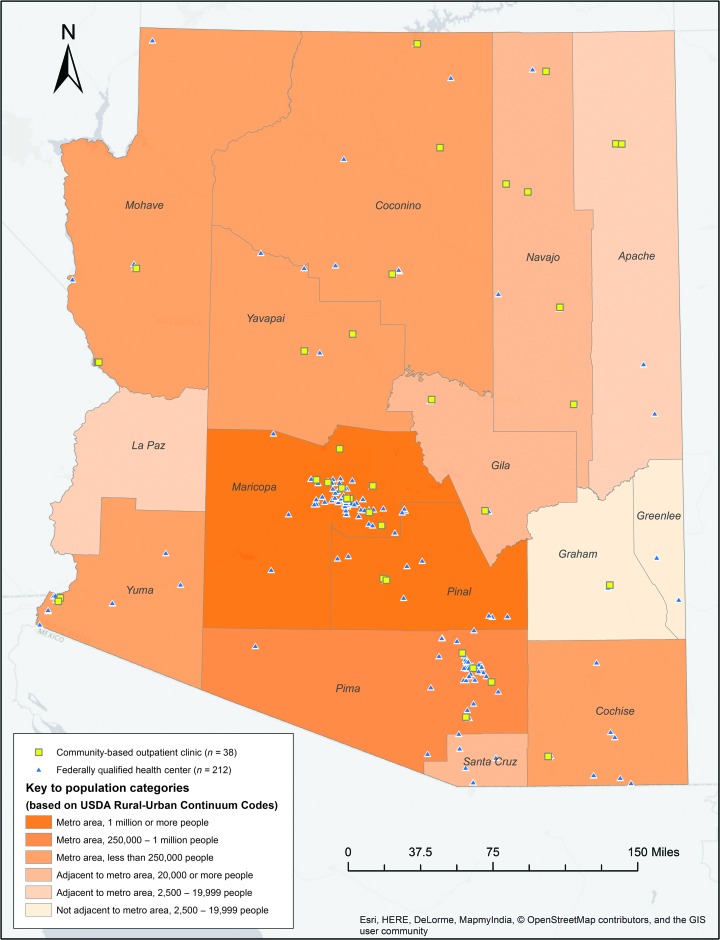
Potential Expansion for Hearing Aid Services Using Teleaudiology
A map is provided in Figure 3 showing the locations of Arizona's 38 Community-Based Outpatient Clinics and 212 Federally Qualified Health Center sites and the population density for the state of Arizona. We calculated the estimated travel distance for the estimated population of individuals ≥ 65 years with hearing loss to these sites. To community-based outpatient clinics, travel distances were calculated to be as short as 7.11 mi (Graham) and as far as 63.89 mi (La Paz). Travel distances to Federally Qualified Health Centers were calculated to be as short as 3.46 mi (Santa Cruz) and as far as 69.86 mi (Apache). In addition, in three counties (Apache, Cochise, Coconino) the average travel distance to a Community-Based Outpatient Clinic was shorter than to a hearing aid dispensing location. In 11 out of 15 counties, the average estimated travel distance to a Federally Qualified Health Center was shorter than to a hearing aid dispensing location. Average travel distances by county can be found in Table 2.
Figure 3.
Locations of potential teleaudiology expansion sites. Total Arizona population is shown, using the U.S. Department of Agriculture's (USDA) Rural–Urban Continuum Code system. Only codes represented in Arizona are illustrated.
Table 2.
Mean and standard deviation road distance estimates (in miles) to the nearest licensed hearing aid services and to potential teleaudiology expansion sites.
| Arizona County | Licensed hearing aid services
a
|
Potential teleaudiology expansion site |
||||
|---|---|---|---|---|---|---|
| Community-Based Outpatient Clinic
b
|
Federally Qualified Health Center
c
|
|||||
| M | SD | M | SD | M | SD | |
| Apache | 118.90 | (36.97) | 39.59 | (17.66) | 69.86 | (28.01) |
| Cochise | 21.60 | (21.29) | 23.30 | (19.94) | 6.72 | (8.79) |
| Coconino | 17.34 | (23.09) | 13.65 | (20.17) | 14.99 | (19.97) |
| Gila | 8.86 | (9.32) | 11.79 | (9.88) | 10.41 | (9.61) |
| Graham | 6.83 | (7.89) | 7.11 | (8.89) | 6.58 | (8.00) |
| Greenlee | 41.56 | (4.13) | 42.55 | (2.80) | 5.72 | (2.77) |
| La Paz | 58.16 | (17.29) | 63.89 | (16.09) | 58.02 | (13.29) |
| Maricopa | 2.30 | (3.29) | 7.71 | (23.68) | 3.74 | (9.22) |
| Mohave | 7.68 | (13.16) | 27.09 | (47.02) | 10.48 | (18.44) |
| Navajo | 35.75 | (33.11) | 19.03 | (12.41) | 24.44 | (26.48) |
| Pima | 4.11 | (7.05) | 7.34 | (25.27) | 3.50 | (12.94) |
| Pinal | 7.89 | (7.68) | 17.48 | (12.67) | 5.28 | (10.24) |
| Santa Cruz | 6.75 | (5.82) | 33.59 | (7.76) | 3.46 | (4.99) |
| Yavapai | 8.05 | (11.38) | 13.68 | (17.61) | 10.47 | (15.44) |
| Yuma | 6.47 | (9.83) | 9.26 | (17.05) | 4.11 | (8.76) |
Note. Travel distances calculated for estimated population of individuals age ≥ 65 years with hearing loss in Arizona.
Audiologists and hearing instrument specialists who held active licenses to dispense hearing aids in Arizona as of June 17, 2017 (Arizona Department of Health Services, 2017b).
Community-Based Outpatient Clinics are health centers that serve as the providers of basic health services to Veterans who live far from a larger health center (Centers for Medicare & Medicaid Services, 2018).
Federally Qualified Health Centers are health centers that operate in Health Professional Shortage Areas and are eligible to receive reimbursements under the Centers for Medicare and Medicaid Services for providing primary and preventative care to all individuals, regardless of ability to pay (Health Resources & Services Administration, 2018).
Discussion
The aim of this project was to describe the geographic distribution of the population and hearing aid workforce across Arizona as the first phase of a comprehensive teleaudiology planning assessment. This aim is aligned with an ongoing program of research related to reducing disparities in access to hearing health care. GIS mapping techniques were used to demonstrate the distribution of the workforce in relation to the estimated population of individuals ≥ 65 years with hearing loss. We analyzed population data relative to workforce population and estimated differences in travel burden from areas across the state using road travel distance. A similar methodology has been used to plan interventions in other health care professions, including in telehealth (N. Soares et al., 2017; N. S. Soares et al., 2013). The novel contribution of this study is the application of GIS tools for teleaudiology resource planning.
Our results revealed that the majority (94%) of the hearing aid workforce in Arizona practiced in metro counties, and six counties had not a single audiologist. These findings are consistent with previous geographic analyses that described urban/rural variations in the otolaryngology workforce. A recent geographic analysis of otolaryngologists across the United States demonstrated that 92.8% of providers practiced in counties with populations greater than 75,000 individuals. In addition, authors of the study estimated that nearly two thirds of the country lacked sufficient access to an otolaryngologist (Vickery & Cabrera-Muffly, 2016). The authors concluded that there is a high need for increased funding for educational programs and a need for strategies that increase access to counties with small populations. Similar arguments have been made in the field of audiology (Windmill & Freeman, 2013).
Arizona's statewide average is consistent with the national average of four audiologists per 100,000 people (American Speech-Language-Hearing Association, 2017). The methodology used in this study also allowed us to capture county-level distributions of audiologists, which ranged from 1.33 (Pinal) to 9.67 (Coconino) per 100,000 population, indicating potential areas of maldistribution within the state. Such data may help inform policy for future state and federal designation and reimbursement guidelines. For example, in the United States, areas with too few primary medical care, dental, or mental health care providers can receive federal designation as HPSAs. These areas are eligible to receive federal funding to support health programs (Health Resources & Services Administration, 2018). Currently, hearing health care provider availability data are not represented in HPSA determination criteria. However, the current study can contribute information that helps aid policy makers in advocating for crucial hearing health care resources.
Travel Distance
The current study contributes to the literature by using GIS tools to demonstrate the anticipated road distance for the estimated population of individuals ≥ 65 years with hearing loss to the nearest location of licensed hearing aid services. County-level results indicated that individuals located in more densely populated areas may have shorter travel distances compared with their more rural counterparts. These results are supported by previous research from primary care and other areas of specialty health care that have demonstrated rural/urban differences in travel to health services. For example, a retrospective chart review by Chan et al. (2006) investigated the travel distances for Medicare patients to reach specialty health care appointments. Results showed that individuals who lived in areas of less than 25,000 people traveled two to three times further to see medical and surgical specialists than individuals who lived in more densely populated areas of more than 25,000 people (L. Chan, Hart, & Goodman, 2006). In addition, they found that patients living in more sparsely populated areas had fewer number of visits to a specialist. The authors speculated that rural patients may limit health care visits as a result of transportation challenges (L. Chan et al., 2006).
The current study's travel distance estimates may provide context for previous study results, indicating that rural individuals experience delayed hearing health care treatment. In a recent study by S. Chan et al. (2017), survey data from hearing aid users in Kentucky revealed that respondents from rural areas experienced longer times between receiving a hearing loss diagnosis and a hearing aid fitting when compared with individuals living in urban areas (25.7 years vs. 19.1 years, p = .024). Rural treatment delays were also found by Bush et al. (2014) among a cohort of children receiving hearing aid rehabilitation and among an adult cochlear implant cohort (Hixon et al., 2016), although these studies lacked an analysis of workforce distribution. Additional research is needed to identify how workforce distribution and hearing aid service utilization are related.
Increasingly, medical specialty services have begun to include a telemedicine service delivery model in an effort to improve accessibility for geographically isolated patients (e.g., Heath, Salerno, Hopkins, Hertzig, & Caputo, 2009). In audiology, timely diagnosis and intervention are considered necessary for successful rehabilitation. However, due to an overall shortage of audiologists and trend for providers across all health fields to practice in urbanized areas, patients in less populated communities may be at risk for delays in care based on where they live.
Potential Expansion for Teleaudiology
Internationally, teleaudiology has been shown to be an effective strategy to expand service access by decreasing transportation burden for patients living far from a clinic (Swanepoel et al., 2010). Our results indicated that travel distance to a hearing aid provider may be reduced by utilizing community clinics as a hub for teleaudiology. For example, in Apache County, travel distance to a Federally Qualified Health Center was 50.04 mi closer than to a hearing aid dispensing provider, and travel to a Community-Based Outpatient Clinic was 39.59 mi closer than to a hearing aid dispensing provider. Previously, Chu et al. (2015) demonstrated that VA patients saved 290 min in travel time by receiving treatment via telemedicine at community-based clinics compared to if they had visited larger hospital-based clinics. In addition, previous research supports the expansion of health services to community clinics as an effective method for decreasing transportation barriers. Barrett, Dziak, and Kaboli (2011) demonstrated a pilot project in which VA audiology services were expanded to five Community-Based Outpatient Clinics in rural Iowa using teleaudiology. Results showed bringing services closer to the patients' home led to an estimated 5,417 hr in saved drive time (Barrett et al., 2011). Many Community-Based Outpatient Clinics and Federally Qualified Health Centers across the United States have active telemedicine programs in primary care and areas of specialty health care to connect patients with providers located in other areas. In addition, Federally Qualified Health Center sites are authorized to receive reimbursements under the Centers for Medicare and Medicaid for qualified services delivered via telemedicine (Centers for Medicare & Medicaid Services, 2018). However, at the time of analysis, Arizona's 38 Community-Based Outpatient Clinics or 212 Federally Qualified Health Centers did not offer teleaudiology services.
Our geographic analysis indicated that many areas of Arizona may benefit from local licensed hearing aid services. For example, Cochise County, with a population of 124,756, lacked a single audiologist and had only one hearing instrument specialist. We estimated that Cochise County is home to 17,029 individuals aged 65 years and older with hearing loss. Due to the number of potential persons with hearing loss and the relatively low number of local hearing aid providers, this area may benefit from a local teleaudiology program. One of the county's seven Federally Qualified Health Centers may serve as a potential local teleaudiology hub. The average road distance for a person with hearing loss to one of Cochise County's Federally Qualified Health Centers is an estimated 6.72 mi (compared with 21.60 mi to the nearest hearing instrument specialist). Audiologists in nearby urban areas (e.g., Maricopa County, 216 audiologists) may connect via teleaudiology with a patient and a trained technician located at a Federally Qualified Health Center to perform remote hearing aid fittings. As a next step, it is recommended to survey the needs and priorities of prospective patients and local providers using a community-based needs assessment (AlDossary et al., 2017).
However, our geographic analysis indicated that these resources may still not be available in all areas. For example, in La Paz County (population: 20,601), there was not a single audiologist, hearing instrument specialist, Federally Qualified Health Center, or Community-Based Outpatient Clinic. Our analysis indicated that individuals ≥ 65 years estimated to have hearing loss in La Paz County may need to drive an average of 58 mi to reach the nearest licensed hearing aid services. Teleaudiology may improve access, yet additional research is needed to identify the local sites and resources that are available. If community clinics are not available, hospitals, community gathering places, or a patient's own home may serve as the local teleaudiology site. In addition, such variation in resource availability demonstrates the value of conducting strategic planning assessments.
Study Limitations and Opportunities for Future Research
Data Sources
To perform analyses for this study, we used a publically available data set that included locations for audiologists and hearing instrument specialists holding active licenses to dispense hearing aids in Arizona. Interpreting these data must be taken with several precautions. First, the ADHS data set does not provide data on audiologists' subspecialties. Therefore, our analyses do not account for pediatric or itinerant audiologists, for example. For this data set, it is the responsibility of individual licensees to maintain up-to-date practice addresses. There was a small subset of licensees with practice locations listed outside of Arizona (audiologists, n = 52; hearing instrument specialists, n = 33). It was thought that these licensees may have entered an out-of-state address as a placeholder while seeking employment. These data were omitted from our analyses.
For the purpose of this workforce distribution analysis, we defined the population of hearing aid dispensers as licensed audiologists and licensed hearing instrument specialists. Alternative methods for the acquisition of hearing aids (e.g., online sales) were omitted from the current study's analyses. Further research is still needed to understand the population's use of alternative methods of acquiring hearing aids. Finally, to calculate travel distance estimates for this study, origin points were distributed across each county representing the target population. The methodology in this study prevented us from generating travel distance estimations for individual patients or for special cohorts, such as the Veteran population. Future research may incorporate actual patient locations for more precise travel distance estimates. Previous research has accomplished this through retrospective chart review (Bruner, Pugh, Yeager, Bruner, & Curran, 2015).
Generalizability of Outcomes
We chose to limit our analyses to Arizona, and therefore, results may not be generalizable across other regions. However, by concentrating within Arizona, we were able to define the hearing aid workforce as it is available to state residents. State-specific data help to inform policy makers and help identify areas of high need. The generalizability of our study outcomes is improved by the use of national community health clinic networks and a nationally recognized rural classification scheme (Rural–Urban Continuation Codes). Specifically, each of these strategies could be applied nationally as patient site locations for teleaudiology. In addition, the methodology presented in this study may be adopted by researchers elsewhere for the purposes of planning assessments, regardless of geographic region or topic area. Future research at a national level appears warranted based on our results from Arizona. However, state-specific analyses will continue to be necessary due to professional licensure regulations and policy regulating the dispensing of hearing aids.
Conclusion
This was the first step in a comprehensive teleaudiology planning assessment for the state of Arizona. We demonstrated variations in the geographic distribution of the hearing aid dispensing workforce. Data indicated there were areas of the state that may benefit from increased access through teleaudiology services. In addition, our results may help provide context for previous research that has indicated rural delays in treatment. However, increased distance from a provider cannot be equated to reduced use of services. Therefore, as the next step, we will evaluate certain patient-related factors, including access to a vehicle, motivation for intervention, and a patient's financial situation, that are thought to influence service utilization among rural individuals (Blazer, Landerman, Fillenbaum, & Horner, 1995). Results of this teleaudiology planning assessment may encourage hearing aid providers and hearing health care researchers to consider how rural areas are affected by maldistribution of resources and how strategies, such as teleaudiology, can help expand accessibility.
Acknowledgments
Research in this publication was supported by the National Institute on Deafness and Other Communication Disorders Grant R33DC013681 (PI: Nicole Marrone). The authors thank Jay Griffin at the Arizona Department of Health Services for his assistance in accessing health workforce data for this project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Portions of this research were presented at the 3rd International Internet & Audiology Meeting, Louisville, KY, July 2017, which was funded by National Institute on Deafness and Other Communication Disorders (NIDCD) Grant 1R13DC016547 and the Oticon Foundation, and at the Association for Research in Otolaryngology in San Diego, CA, on February 10, 2018.
Funding Statement
Research in this publication was supported by the National Institute on Deafness and Other Communication Disorders Grant R33DC013681 (PI: Nicole Marrone).
References
- AlDossary S., Martin-Khan M. G., Bradford N. K., Armfield N. R., & Smith A. C. (2017). The development of a telemedicine planning framework based on needs assessment. Journal of Medical Systems, 41(5), 74. [DOI] [PubMed] [Google Scholar]
- Alverson D. C., Holtz B., D'Iorio J., DeVany M., Simmons S., & Poropatich R. K. (2008). One size doesn't fit all: Bringing telehealth services to special populations. Telemedicine and e-Health, 14(9), 957–963. [DOI] [PubMed] [Google Scholar]
- American Speech-Language-Hearing Association. (2017). ASHA-certified personnel-to-population ratios. Retrieved from https://www.asha.org/uploadedFiles/Personnel-to-Population-Ratios-State.pdf
- Arizona Department of Health Services. (2017. a). Arizona Designation Mapper. Retrieved from https://www.azdhs.gov/prevention/health-systems-development/shortage-designation/designation-mapper/index.php
- Arizona Department of Health Services. (2017b). Public health licensing provider and facility databases. Retrieved from http://azdhs.gov/licensing/index.php#databases
- Barrett D., Dziak K., & Kaboli P. (2011). Expanding audiology services to CBOCs: Bringing care closer to Veterans. Veterans Rural Health Resource Center Issue Brief # 5. Retrieved from https://www.ruralhealth.va.gov/docs/issue-briefs/BARRETT_Audiology_Services_FINAL_3-6-11.pdf
- Blazer D. G., Landerman L. R., Fillenbaum G., & Horner R. (1995). Health services access and use among older adults in North Carolina: Urban vs. rural residents. American Journal of Public Health, 85(10), 1384–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruner D. W., Pugh S. L., Yeager K. A., Bruner J., & Curran W. (2015). Cartographic mapping and travel burden to assess and develop strategies to improve minority access to national cancer clinical trials. International Journal of Radiation Oncology Biology Physics, 93(3), 702–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics, U.S. Department of Labor. (2017). Occupational outlook handbook: Audiologists. Retrieved from https://www.bls.gov/ooh/healthcare/audiologists.htm
- Bush M. L., Osetinsky M., Shinn J. B., Gal T. J., Ding X., Fardo D. W., & Schoenberg N. (2014). Assessment of Appalachian region pediatric hearing healthcare disparities and delays. The Laryngoscope, 124(7), 1713–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush M. L., Thompson R., Irungu C., & Ayugi J. (2016). The role of telemedicine in auditory rehabilitation: A systematic review. Otology & Neurotology, 37(10), 1466–1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos P. D., & Ferrari D. V. (2012). Teleaudiology: Evaluation of teleconsultation efficacy for hearing aid fitting. Journal da Sociedade Brasileira de Fonoaudiologia, 24(4), 301–308. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. (2018). Federally Qualified Health Center. Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/fqhcfactsheet.pdf
- Chan L., Hart L. G., & Goodman D. C. (2006). Geographic access to health care for rural Medicare beneficiaries. The Journal of Rural Health, 22(2), 140–146. [DOI] [PubMed] [Google Scholar]
- Chan S., Hixon B., Adkins M., Shinn J. B., & Bush M. L. (2017). Rurality and determinants of hearing healthcare in adult hearing aid recipients. The Laryngoscope, 127(10), 2362–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu S., Boxer R., Madison P., Kleinman L., Skolarus T., Altman L., … Shelton J. (2015). Veterans Affairs telemedicine: Bringing urologic care to remote clinics. Urology, 86(2), 255–261. [DOI] [PubMed] [Google Scholar]
- Dennis K. C., Gladden C. F., & Noe C. M. (2012). Telepractice in the Department of Veterans Affairs: An overview of the VA telehealth and pilot teleaudiology programs. Hearing Review, 19(11), 44–50. [Google Scholar]
- Doty M. M., Abrams M. K., Hernandez S. E., Stremikis K., & Beal A. C. (2010). Enhancing the capacity of community health centers to achieve high performance: Findings from the 2009 Commonwealth Fund national survey of Federally Qualified Health Centers. New York, NY: The Commonwealth Fund. [Google Scholar]
- Environmental Systems Research Institute. (2017). ArcMap (Version 10.5) [Computer software]. Retrieved from http://desktop.arcgis.com/en/arcmap/
- Gladden C. (2013). The current status of VA audiology. Veterans Health Administration. Retrieved from http://www.ncrar.research.va.gov/Education/Conf_2013/Documents/Gladden.pdf
- Gladden C., Beck L., & Chandler D. (2015). Tele-audiology: Expanding access to hearing care and enhancing patient connectivity. Journal of the American Academy of Audiology, 26(9), 792–799. [DOI] [PubMed] [Google Scholar]
- Gulliford M., Figueroa-Munoz J., Morgan M., Hughes D., Gibson B., Beech R., & Hudson M. (2002). What does ‘access to health care’ mean? Journal of Health Services Research & Policy, 7(3), 186–188. [DOI] [PubMed] [Google Scholar]
- Healthy People 2020. (n.d.) Topics and objectives: Hearing and other sensory or communication disorders. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/hearing-and-other-sensory-or-communication-disorders/objectives
- Health Resources & Services Administration. (2018). Federally Qualified Health Centers. Retrieved from https://www.hrsa.gov/opa/eligibility-and-registration/health-centers/fqhc/index.html
- Heath B., Salerno R., Hopkins A., Hertzig J., & Caputo M. (2009). Pediatric critical care telemedicine in rural underserved emergency departments. Pediatric Critical Care Medicine, 10(5), 588–591. [DOI] [PubMed] [Google Scholar]
- Hedeen A. N., Heagerty P. J., Fortney J. C., Borowsky S. J., Walder D. J., & Chapko M. K. (2002). VA Community-Based Outpatient Clinics: Quality of care performance measures. Medical Care, 40(7), 570–577. [DOI] [PubMed] [Google Scholar]
- Hixon B., Chan S., Adkins M., Shinn J. B., & Bush M. L. (2016). Timing and impact of hearing healthcare in adult cochlear implant recipients: A rural–urban comparison. Otology & Neurotology, 37(9), 1320–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder K. A. (2017). Veterans in Rural America: 2011–2015 [ACS-36]. Retrieved from https://www.census.gov/content/dam/Census/library/publications/2017/acs/acs-36.pdf
- Ingram M., Marrone N., Sanchez D. T., Sander A., Navarro C., de Zapien J. G., … Harris F. (2016). Addressing hearing health care disparities among older adults in a US–Mexico border community. Frontiers in Public Health, 4, 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupinski E. A. (2015). Innovations and possibilities in connected health. Journal of the American Academy of Audiology, 26(9), 761–767. [DOI] [PubMed] [Google Scholar]
- Leavitt E. R., Kessler S., Pun S., Gill T., Escobedo L. A., Cockburn M., … Crew A. B. (2016). Teledermatology as a tool to improve access to care for medically underserved populations: A retrospective descriptive study. Journal of the American Academy of Dermatology, 75(6), 1259–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F. R., Thorpe R., Gordon-Salant S., & Ferrucci L. (2011). Hearing loss prevalence and risk factors among older adults in the United States. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 66(5), 582–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLafferty S. L. (2003). GIS and health care. Annual Review of Public Health, 24(1), 25–42. [DOI] [PubMed] [Google Scholar]
- Merrell R. C., & Doarn C. R. (2008). Is it time for a telemedicine breakthrough? Telemedicine and e-Health, 14(6), 505–506. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2016). Hearing health care for adults: Priorities for improving access and affordability. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Ripley D. C. C., Litt E. R., Jia H., Vogel W. B., Wang X., Wilson L. K., … Graham G. D. (2014). Using GIS to plan specialty health services for Veterans: The example of acute stroke care. Journal of Geographic Information System, 6(3), 177–184. [Google Scholar]
- Rosenblatt R. A., Andrilla C. H. A., Curtin T., & Hart L. G. (2006). Shortages of medical personnel at community health centers: Implications for planned expansion. Journal of the American Medical Association, 295(9), 1042–1049. [DOI] [PubMed] [Google Scholar]
- Smith A. C., & Gray L. C. (2009). Telemedicine across the ages. Medical Journal of Australia, 190(1), 15–29. [DOI] [PubMed] [Google Scholar]
- Soares N., Dewalle J., & Marsh B. (2017). Utilizing patient geographic information system data to plan telemedicine service locations. Journal of the American Medical Informatics Association, 24(5), 891–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares N. S., Johnson A. O., & Patidar N. (2013). Geomapping telehealth access to developmental-behavioral pediatrics. Telemedicine and e-Health, 19(8), 585–590. [DOI] [PubMed] [Google Scholar]
- Stahl I., Dreyfuss D., Ofir D., Merom L., Raichel M., Hous N., … Haddad E. (2017). Reliability of smartphone-based teleradiology for evaluating thoracolumbar spine fractures. The Spine Journal, 17(2), 161–167. [DOI] [PubMed] [Google Scholar]
- Swanepoel D. W., Clark J. L., Koekemoer D., Hall J. W. III., Krumm M., Ferrari D. V., … Barajas J. J. (2010). Telehealth in audiology: The need and potential to reach underserved communities. International Journal of Audiology, 49(3), 195–202. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2010). QuickFacts. Retrieved from http://purl.access.gpo.gov/GPO/LPS33913
- U.S. Census Bureau. (2017). Annual estimates of the resident population: April 1, 2010 to July 1, 2017. Retrieved from https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk
- U.S. Department of Agriculture. (2016). Rural–urban continuum codes. Retrieved from https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- U.S. Department of Veterans Affairs. (2015). Locations: Arizona. Retrieved from http://www.va.gov/directory/guide/state.asp?dnum=ALL&STATE=AZ
- Van Dyk L. (2014). A review of telehealth service implementation frameworks. International Journal of Environmental Research and Public Health, 11(2), 1279–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Health Administration. Restoring trust in Veterans health care, fiscal year 2016 annual report. Retrieved from https://www.va.gov/HEALTH/docs/ VHA_AR16.pdf
- Vickery T. W., & Cabrera-Muffly C. (2016). Geographic distribution of otolaryngologists in the United States. Ear, Nose, & Throat Journal, 95(6), 218–223. [PubMed] [Google Scholar]
- Windmill I. M., & Freeman B. A. (2013). Demand for audiology services: 30-yr projections and impact on academic programs. Journal of the American Academy of Audiology, 24(5), 407–416. [DOI] [PubMed] [Google Scholar]
- Yellowlees P. M. (2005). Successfully developing a telemedicine system. Journal of Telemedicine and Telecare, 11(7), 331–335. [DOI] [PubMed] [Google Scholar]
- Yellowlees P., Burke Parish M., González Á., Chan S., Hilty D., Iosif A.M., … Shore J. (2017). Asynchronous telepsychiatry: A component of stepped integrated care. Telemedicine and e-Health, 24(5), 375–378. https://doi.org/10.1089/tmj.2017.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]