Abstract
Background
The measurement of native T1 through cardiovascular magnetic resonance (CMR) is a noninvasive method of assessing myocardial fibrosis without gadolinium contrast. No studies so far have evaluated native T1 after renal transplantation. The primary aim of the current study is to assess changes in the myocardium native T1 6 months after renal transplantation.
Methods
We prospectively evaluated 44 renal transplant patients with 3 T CMR exams: baseline at the beginning of transplantation and at 6 months after transplantation.
Results
The native T1 time was measured in the midventricular septum and decreased significantly from 1331 ± 52 ms at the baseline to 1298 ± 42 ms 6 months after transplantation (p = 0.001). The patients were split into two groups through a two-step cluster algorithm: In cluster-1 (n = 30) the left ventricular (LV) mass index and the prevalence of diabetes were lower. In cluster-2 (n = 14) the LV mass index and diabetes prevalence were higher. Decrease in native T1 values was significant only in the patients in cluster-1 (p = 0.001).
Conclusions
The native myocardial T1 time decreased significantly 6 months after renal transplant, which may be associated with the regression of the reactive fibrosis. The patients with greater baseline LV mass index and the diabetic group did not reach a significant decrease in T1.
Electronic supplementary material
The online version of this article (10.1186/s12968-019-0531-x) contains supplementary material, which is available to authorized users.
Keywords: Cardiovascular magnetic resonance imaging, Fibrosis, Kidney transplantation, Native T1
Background
Patients with chronic kidney disease (CKD) are at increased risk for cardiovascular disease (CVD) [1, 2]. Renal transplantation is associated with a reduction in cardiovascular mortality when compared to patients who remain on the transplant waiting list [3]. It is likely that the improvement in cardiac contractility is due to the regression of intermyocardiocytic fibrosis after transplantation [4]. Myocardial fibrosis affects more than 90% of patients with CKD [4] and leads to the accumulation of extracellular matrix (ECM) proteins in the cardiac interstice, which in turn results in increased left ventricle (LV) stiffness. This contributes to reduced diastolic filling, with the development of arrhythmias, heart failure and sudden cardiac death [5–8]. Hence, the extent and severity of myocardial fibrosis are important predictors of death among patients with CKD [4].
Three types of myocardial fibrosis have been reported: reactive interstitial fibrosis, infiltrative interstitial fibrosis and replacement fibrosis [9, 10]. Fibrosis may regress in the reactive type, whilst in the replacement one there is loss of myocytes due to necrosis and/or apoptosis [11–13].
Myocardial fibrosis is confirmed with endomyocardial biopsy, but it is a procedure with high morbidity [14, 15]. Imaging techniques that allow the detection of myocardial fibrosis are noninvasive methods that may improve tissue characterization and stratification of cardiovascular risk. On that account, cardiovascular magnetic resonance (CMR) imaging has been used to quantify myocardial fibrosis and replace endomyocardial biopsy. The measurement of extracellular volume fraction (ECV) by CMR is an efficient method to detect and quantify myocardial fibrosis [16, 17]. Although promising, ECV measurement uses gadolinium contrast, which is contraindicated in patients with a glomerular filtration rate lower than 30 mL/min due to the risk of nephrogenic systemic fibrosis [18].
As an alternative, myocardium native T1 mapping is a resonance method that evaluates myocardial and quantify the fibrosis without the use of gadolinium contrast [19, 20]. The native T1 strong correlates with histological myocardial fibrosis in patients with aortic stenosis [21]. In 2018, a meta-analysis established the reference values of native T1 for nonischemic cardiomyopathies and populations with increased cardiovascular risk [22]. Different types of tissue will have their own normal ranges of values, and a significant departure from the normal range is thought to differentiate between normal and abnormal myocardium.
It has already been demonstrated that in the hemodialysis population, native T1 values are higher in comparison with healthy subjects [20]. However, the values of native T1 after renal transplantation are not yet known.
The primary aim of this study was to evaluate the changing of septal native T1 between baseline and 6 months after renal transplantation.
Patients and methods
This prospective single-center cohort study was performed in a tertiary medical center (Botucatu Medical School - UNESP, Univ Estadual Paulista). A total of 44 patients underwent two CMR examinations. The first exam (baseline) was performed between the 1st and the 10th postoperative days. The second one was performed 6 months after renal transplantation. Changes in the native T1 were evaluated by comparing the first and second exams of the same patient. The protocol was reviewed and approved by the institutional review board (CAAE: 40598414.9.0000.5411). Written informed consent was obtained from the subjects before participation.
Inclusion and exclusion criteria
We included consecutive patients over 18 years of age who received a renal transplant from a living or deceased donor. We excluded patients with a contraindication to CMR (e.g., pacemaker, metal prosthesis, cochlear implant, cerebral aneurysm clip, tattooing, claustrophobia, hemodynamic instability) and inability to perform breath hold.
CMR acquisition
All examinations were performed on the same 3 T CMR system (Magnetom Verio, Siemens AG, Healthineers, Erlangen, Germany) with a phased array chest coil, according to study protocol. A cardiac cine balanced steady-state free precession (bSSFP) sequence was acquired using retrospective cardiac gating. Typically, 25 phases were acquired in 2-, 3-, and 4-chamber long axis views and a stack of short axis views. Scan parameters: field of view (FOV) 37-cm, repetition time 43.54 ms, echo time 1.38 ms, flip angle 50°, slice thickness 6 mm, in-plane image resolution 1.6 × 1.6 mm. Quantitative T1 mapping was performed with a Modified Look-Locker Inversion-Recovery (MOLLI) sequence in mid-cavity short axis slice, without gadolinium (Native T1) following the recommendations of the European Society of Cardiology consensus [23]. Scan parameters: FOV 36-cm, repetition time 316.09 ms, echo time 1.12 ms, flip angle 35°, slice thickness 8 mm, in-plane image resolution 2.1 × 1.4 mm, acquisition in late diastole on every other heartbeat, minimal inversion time 120 ms; increment 80 ms. The T1 mapping scheme included 5 acquisitions after the first inversion pulse, followed by a 3-heartbeat pause and a second inversion pulse followed by 3 acquisitions [5(3)3 scheme].
CMR analysis
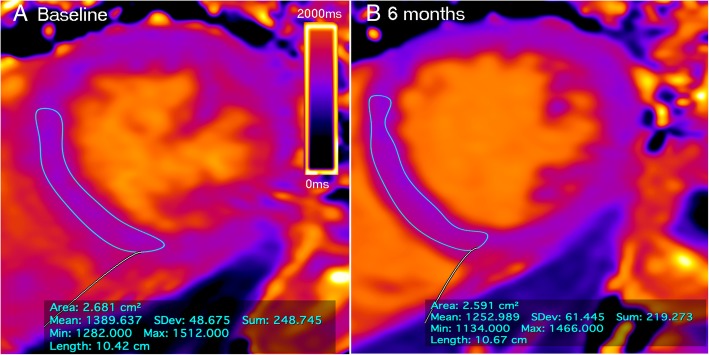
Biventricular ejection fraction, volumes and LV mass were calculated from the short-axis cine images with post-processing using Argus software (Siemens, Healthineers). Endocardial contours were drawn at both end-diastole and end-systole. LV epicardial contours were drawn only at end-diastole to calculate LV mass. This technique was repeated for each short-axis slice and the software calculated the volumes, mass and ejection fraction using the Simpson method. T1 maps were automatically generated on the CMR scanner. A region of interest (ROI) was then drawn in the septal myocardium to obtain T1 value (Fig. 1). The native T1 measurements using midventricular septum approach are recommended as the standardized due to independence of geometrical alterations of cardiac chamber and wall thickness [24]. All the patients underwent the same imaging protocol, analyzed by a single blinded observer, using the same technique of post-processing.
Fig. 1.
Example of T1 septal mapping. The thin line denotes the manually contoured region of interest (ROI) in the midventricular septum. The box shows the measures of T1 value by automatic computer average of the pixels. The color map scale represents the values in milliseconds (blue corresponds to smaller values and yellow to higher values). Data acquired with the modified look-locker inversion recovery (MOLLI) T1 mapping sequence at a field strength of 3 T
Baseline characteristics and other clinical and laboratory parameters
Donor and recipient characteristics and immunosuppressive therapy were evaluated at baseline. Biochemical and renal function parameters and the use of non-immunosuppressive drugs between baseline and 6 months were evaluated. We also evaluated systolic and diastolic blood pressure and heart rate in the two time periods.
Statistical analysis
Sample size calculation
A pilot study was conducted with 11 patients, in which a mean difference in native T1 of 50 ± 52 ms was found. Considering the alpha error of 0.05 and the beta of 0.8, for this study we calculated a number of 38 patients.
Descriptive statistics and comparisons between groups
Categorical variables were expressed in numbers and percentage and compared between the two moments of the study by Fisher’s exact test or chi-square when appropriate. Continuous variables were tested for their normality by the Kolmogorov-Smirnov test and visual inspections of QQ plots. The parametric variables were expressed as mean and standard deviation and compared between the two moments of the study by paired t-test. Non-parametric variables were expressed in median and 25 and 75% percentiles and compared between the two time points by using the Wilcoxon test.
A cluster analysis was conducted using the two-step cluster analysis algorithm with the Schwarz Bayesian criterion for clustering. The number of clusters by automatic selection and the distance were measured with log probability. The TwoStep Cluster Analysis procedure is an exploratory tool designed to reveal natural groupings within a dataset that would otherwise not be apparent. This was used in this study to group the baseline clinical variables into strongly interrelated subgroups (clusters) without prior knowledge of the target variables. We used all baseline clinical variables to build the cluster analysis that automatically resulted in two clusters. This analysis creates groups that are more similar to each other based on the log probability distances (Additional file 1). The methods of cluster analysis in the context of classifying patients in the medical field was described by McLachlan et al. [25] and this approach has been recently utilized to identify clinical variables that was related to disease phenotypes in patients with heart failure [26, 27]. A p value < 0.05 indicated statistical significance. All analyses were performed by using SPSS statistical software, version 20 (International Business Machines, Inc., Armonk, New York, USA). The plots were built with R (R Foundation for Statistical Computing, Vienna, Austria) version 3.4.2 with the ggplot2 package.
Results
There were 44 patients who completed the two CMR evaluations (n = 88 CMR studies). The median time from transplant to the first exam was 5 days and to second exam was 189. The hematocrit was similar for the first CMR exam and preoperative value (mean difference − 0.9% [95%CI -1.437 to 3.237] p = 0.44). The baseline donor and recipient characteristics are detailed in Table 1 and the use of non-immunosuppressive drugs in Table 2. During the study period, no patient has developed a graft loss or a cardiovascular event (acute myocardial infarction, acute coronary syndrome, or arrhythmias). The clinical and biochemical parameters of the patients at the two time points are shown in Table 3.
Table 1.
Donor and recipient characteristics at Baseline of study patients
| Total Patients (n = 44) |
|
|---|---|
| Age (years) | 50 ± 11 |
| Male | 27 (61.4%) |
| Primary renal diagnosis | |
| Hypertension | 11 (25%) |
| Diabetes | 11 (25%) |
| Glomerulonephritis | 8 (18.2%) |
| Unknown cause | 7 (15.9%) |
| Others | 7 (15.9%) |
| Diabetes (n. %) | 14 (31.8%) |
| Prior Transplantation | 2 (4.5%) |
| Length of time on hemodialysis (months) | 29 [15–45] |
| Panel reactive antibody class I (%) | 0 [0–5] |
| Mismatches (n) | 3 [2–3] |
| Donor | |
| Deceased | 37 (84.1%) |
| Living | 7 (15.9%) |
| Donor Age (years) | 39 ± 12 |
| Cause of Donor Death | |
| Cranial trauma | 15 (34%) |
| Cerebrovascular | 15 (34%) |
| Others | 14 (31%) |
| Final donor creatinin (mg/dL) | 1.12 ± 0.6 |
| Cold ischemia time (hours) | 22.3 ± 6.2 |
| Induction therapy | |
| Basiliximab | 12 (27.3%) |
| Thymoglobulin | 32 (72.7%) |
| Immunosuppression | |
| Tacrolimus + mycophenolate + prednisone | 16 (36.4%) |
| 5 (11.4%) | |
| Tacrolimus + sirolimus + prednisone | |
| Tacrolimus + everolimus + prednisone | 23 (52.3%) |
Continuous variables expressed as mean and standard deviation (mean ± standard deviation) or median and 25 and 75% percentiles (median [25th and 75th percentile]). Categorical variables expressed in number and percentage
Table 2.
Use of non-immunosuppressive drugs at baseline and 6 months after transplantation
| Baseline (n = 44) |
6 months (n = 44) |
p | |
|---|---|---|---|
| Aspirin | 20 (45.5%) | 16 (36.4%) | 0.38 |
| Calcium channel blockers | 14 (31.8%) | 16 (36.4%) | 0.65 |
| Beta-blockers | 21 (47.7%) | 27 (61.4%) | 0.19 |
| ARB/ACEi | 26 (60.5%) | 10 (22.7%) | 0.0001 |
| Alpha-blockers | 7 (15.9%) | 8 (18.2%) | 0.77 |
| Spironolactone | 1 (2.3%) | 1 (2.3%) | 1.0 |
| Statin | 5 (11.4%) | 10 (22.7%) | 0.15 |
| Ciprofibrate | 0 (0%) | 3 (6.8%) | 0.09 |
| Furosemide | 17 (38.6%) | 2 (4.5%) | 0.001 |
| Hydrochlorothiazide | 3 (6.8%) | 5 (11.4%) | 0.45 |
| Isosorbide | 2 (4.5%) | 0 (0%) | 0.15 |
ARB angiotensin II receptor blockers, ACEi angiotensin converting enzyme inhibitor
Categorical variables expressed in number and percentage. Comparisons with chi-square test
Table 3.
Clinical and biochemical parameters at baseline and 6 months after transplantation
| Baseline (n = 44) |
6 months (n = 44) |
p | |
|---|---|---|---|
| HR (bmp) | 86 ± 13 | 79 ± 12 | 0.013a |
| DBP (mmHg) | 80 [70–90] | 70 [70–80] | 0.008b |
| SBP (mmHg) | 135 [130–150] | 120 [110–140] | 0.004b |
| Body Weight (Kg) | 71.1 [60.6–78] | 72.6 [62–79.5] | 0.17b |
| Calcium (mg/dL) | 9.3 [8.9–9.6] | 9.6 [9.3–10] | 0.001b |
| Creatinine (mg/dL) | 4.2 [2–7.7] | 1.3 [1–1.8] | 0.001b |
| Phosphate (mg/dL) | 3.9 [3.1–5.4] | 3.5 [3–3.9] | 0.02b |
| Hb (g/dL) | 10.7 ± 1.8 | 12.7 ± 1.7 | 0.001a |
| Ht (%) | 32.7 ± 5.9 | 38.4 ± 4.9 | 0.001a |
| PTH (pg/ml) | 203 [111–483] | 68.8 [44.7–117] | 0.001b |
HR heart rate, Hb hemoglobin, Ht hematocrit, DBP diastolic blood pressure, SBP systolic blood pressure, PTH Parathyroid hormone
Continuous variables expressed as mean and standard deviation (mean ± standard deviation) or median and 25 and 75% percentiles (median [25th and 75th percentile])
aPaired t test; bWilcoxon test
LV mass and function
There was a trend to improved LV function after 6 months, p = 0.07 but no statistical difference in LV mass index (Table 4).
Table 4.
Left ventricular parameters of cardiac magnetic resonance at baseline and 6 months after transplantation
| Baseline (n = 44) |
6 months (n = 44) |
p | |
|---|---|---|---|
| Ejection Fraction (%) | 64 ± 12 | 67 ± 10 | 0.07a |
| EDV (ml) | 155 ± 43 | 152 ± 35 | 0.61a |
| ESV (ml) | 52 [38–69] | 50 [39–63] | 0.49b |
| SV (ml) | 96 ± 21 | 100 ± 20 | 0.27a |
| LVM (g) | 154 ± 40 | 152 ± 35 | 0.76a |
| EDVi (mL/m2) | 88 ± 23 | 85 ± 19 | 0.29a |
| ESVi (mL/m2) | 30 [21–40] | 28 [22–36] | 0.28b |
| SVi (mL/m2) | 55 ± 12 | 56 ± 11 | 0.42a |
| LVMi (g/m2) | 87 ± 20 | 85 ± 16 | 0.36a |
| IS (mm) | 12.9 ± 3.3 | 12.7 ± 3.2 | 0.71a |
| LVPW (mm) | 10.2 ± 2.2 | 9.6 ± 1.8 | 0.07a |
| LVED (mm) | 53 ± 7 | 52 ± 7 | 0.21a |
| LVES (mm) | 34 ± 9 | 33 ± 6 | 0.20a |
BSA body surface area, EDV end-diastolic volume, EDVi end-diastolic volume indexed to BSA, ESV end-systolic volume, ESVi, end-systolic volume index to BSA, LVM left ventricular mass, LVMi left ventricular mass indexed to BSA, SV systolic volume, SVi systolic volume index to BSA, IS interventricular septum, LVPW left ventricular posterior wall, LVED left ventricular end-diastolic diameter, LVES left ventricular end-systolic diameter
Continuous variables expressed as mean and standard deviation (mean ± standard deviation) or median and 25 and 75% percentiles (median [25th and 75th percentile])
apaired t-test; bWilcoxon test
Native T1 times (primary outcome)
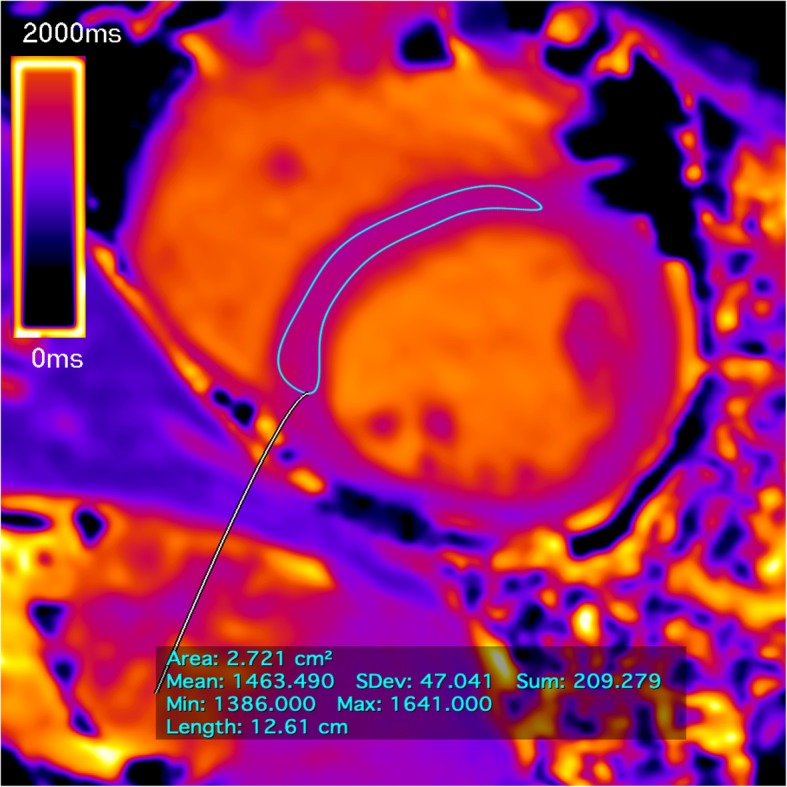
The data analysis revealed a significant reduction in native T1 time 6 months after renal transplantation. The mean T1 decreased from 1331 ± 52 ms to 1298 ± 42 ms at 6 months (p < 0.001) (Fig. 2). The analysis of individual cases of native T1 demonstrated that the majority of the patients reached a reduction in T1 values between baseline and 6 months after transplantation (Additional file 2). Figure 3 display an example of the T1 map at the two time periods in three patients: one patient with native T1 maintenance, one with an increase, and another with a decrease in native T1 times.
Fig. 2.
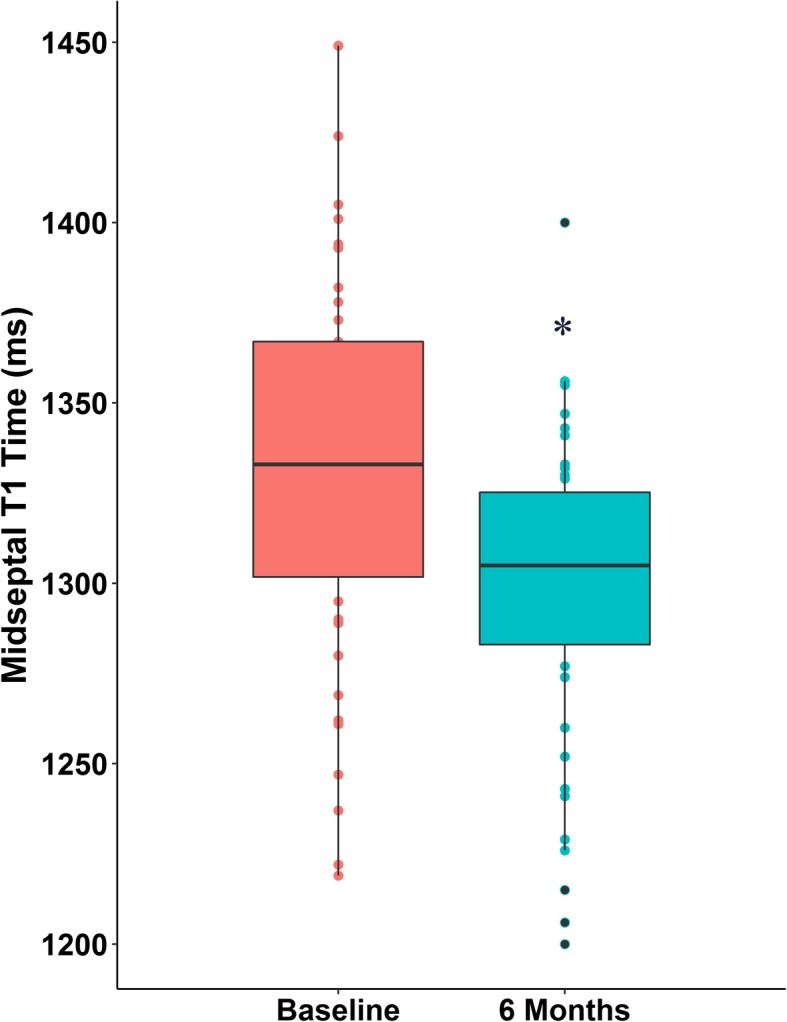
Boxplot comparing midventricular septum T1 time at baseline and 6 months after transplantation.* p < 0.001 x baseline
Fig. 3.
Example of native T1 mapping in a 38-year-old deceased-donor kidney transplant patient. The T1 value changing from 1389 ms (a) to 1252 ms (b) showing a decrease 6 months after transplantation (visual pattern with increased blue staining, patient id = 3).The thin line denotes the manually contoured region of interest (ROI) in the midventricular septum. The box shows the measures of T1 value by automatic computer average of the pixels. The color map scale represents the values in milliseconds (blue corresponds to smaller values and yellow to higher values). Data acquired with the modified look-locker inversion recovery (MOLLI) T1 mapping sequence at field strength of 3 T
Cluster analysis
The 44 patients were divided into 2 groups by two-step cluster algorithm. In cluster-1 (n = 30) there were no patients with diabetes mellitus and in cluster-2 (n = 14), all 14 patients (100%) had diabetes (p < 0.001, Table 5). The LV mass index at baseline was significantly higher in cluster-2 (93 ± 19 g/m2) than in cluster-1 (83 ± 17 g/m2, p = 0.02).
Table 5.
Demographic and clinical characteristics of patients divided in to clusters by Two Step Algorithm
| Cluster-1 (n = 30) |
Cluster-2 (n = 14) |
p | |
|---|---|---|---|
| Age (years) | 48 ± 11 | 54 ± 08 | 0.10 |
| Male | 20 (66.7%) | 7 (50%) | 0.29 |
| Primary renal diagnosis | |||
| Hypertension | 8 (26.7%) | 3 (21.4%) | |
| Diabetes | 0 (0%) | 11 (78.6%) | |
| Glomerulonephritis | 8 (26.7%) | 0 (0%) | 0.001 |
| Unknown cause | 7 (23.3%) | 0 (0%) | |
| Others | 7 (23.3%) | 0 (0%) | |
| Diabetes (n. %) | 0 (0%) | 14 (100%) | 0.0001 |
| Prior Transplant | 2 (6.7%) | 0 (0%) | 0.32 |
| Length of time on hemodialysis (months) | 28 [14–43] | 33 [17–47] | 0.51 |
| Panel reactive antibody class I (%) | 0 [0–15] | 0 [0–0] | 0.33 |
| Mismatches (n) | 3 [2–4] | 3 [2–3] | 0.20 |
| Donor | |||
| Deceased | 24 (80%) | 13 (92.9%) | 0.27 |
| Living | 6 (20%) | 1 (7.1%) | |
| Donor Age (years) | 40 ± 10 | 37 ± 13 | 0.40 |
| Cause of Donor Death | |||
| Cranial trauma | 9 (30%) | 6 (42%) | |
| Cerebrovascular | 9 (30%) | 4 (28.5%) | |
| Others | 7 (40%) | 4 (28.5%) | 0.90 |
| Final donor creatinin (mg/dL) | 1.19 ± 0.6 | 1.14 ± 0.58 | 0.78 |
| Cold ischemia time (hours) | 21.8 ± 7 | 23.2 ± 3.9 | 0.50 |
| Induction therapy | |||
| Basiliximab | 9 (30%) | 3 (21.4%) | 0.55 |
| Thymoglobulin | 21 (70%) | 11 (78.6%) | |
| Immunosuppression | |||
| FK + MFS + PDN | 13 (43.3%) | 3 (21.4%) | |
| FK + SRL + PDN | 4 (13%) | 1 (7.1%) | 0.22 |
| FK + EVR + PDN | 13 (43.3%) | 10 (71.4%) | |
| Use of ARB/ACEi | 17 (56.7%) | 9 (69.2%) | 0.43 |
| Calcium (mg/dL) | 9.39 ± 0.80 | 9.04 ± 0.52 | 0.14 |
| Phosphate (mg/dL) | 4.19 ± 1.78 | 4.5 ± 1.4 | 0.47 |
| PTH (ng/dl) | 199 [117–499] | 211 [68–470] | 0.76 |
| Hb (g/dl) | 10.8 ± 1.9 | 10.6 ± 1.7 | 0.72 |
| SBP (mmHg) | 138 ± 25 | 139 ± 13 | 0.96 |
| DBP (mmHg) | 85 ± 14 | 77 ± 12 | 0.07 |
| LVMi (g/m2) | 83 ± 17 | 93 ± 19 | 0.02 |
FK + EVR + PDN Tacrolimus, everolimus and prednisone, FK + MFS + PDN tacrolimus, mycophenolate and prednisone, FK + SRL + PDN tacrolimus, sirolimus and prednisone, Hb hemoglobin, LVMi left ventricular mass index, DBP diastolic blood pressure, SBP systolic blood pressure, PTH Parathyroid hormone, ARB angiotensin II receptor blockers, ACEi angiotensin converting enzyme inhibitor
Continuous variables expressed as mean and standard deviation (mean ± standard deviation) or median and 25 and 75% percentiles (median [25th and 75th percentile]). Categorical variables expressed in number and percentage
The analysis of LV mass demonstrated that in cluster-1 the LV mass index decreased from 84.5 ± 19.7 g/m2 (baseline) to 81.5 ± 14.1 g/m2 (6 months; p = 0.32). In cluster-2, the LV mass index did not change (93 ± 21.1 g/m2 (baseline) to 92.2 ± 17.2 g/m2 (6 months; p = 0.86). (Additional file 3).
The LV ejection fraction (EF) changed from 64.1 ± 13.5% (baseline) to 66.3 ± 8.5% (6 months) in cluster-1, p = 0.24. In cluster-2, the EF changed from 65.3 ± 9.8% (baseline) to 68.6 ± 12.2% (6 months), p = 0.09.
In cluster-1, native T1 values decreased from 1337 ± 54.8 ms (baseline) to 1293 ± 38.7 ms (6 months; p = 0.001). In cluster-2, the native T1 was similar at baseline and at 6 months (p = 0.50, Fig. 4). The analysis of individual cases demonstrates that only the patients in Cluster-1 reached a reduction in T1 values between baseline and 6 months after transplantation (Additional file 4).
Fig. 4.

Boxplot comparing midventricular septum T1 time at baseline and 6 months after transplantation splitted into two groups. The groups were wrapped by a cluster analysis designed to reveal natural groupings within a dataset that would otherwise not be apparent. The majority of patients in cluster-2 were diabetics and the patients with greater baseline left ventricular mass index. * p = 0.001 x baseline
Discussion
To our knowledge, this is the first prospective study to evaluate the change in myocardial native T1 after renal transplantation. We demonstrated that native T1 significantly decreased 6 months after transplantation.
Use of non-immunosuppressive drugs
The inhibition of the renin-angiotensin-aldosterone system, induced by angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs), reduces myocardial fibrosis, regardless of its hypotensive action [28]. In addition, the selective AT1 angiotensin II antagonist prevents myocyte hypertrophy and interstitial fibrosis [29]. Most patients use ARBs or ACEIs during the dialysis period. In the early postoperative period after transplantation, however, these medications are frequently discontinued since they impair renal graft function, perpetuate anemia, and leads to hyperkalemia. In the present study, 6 months after transplantation, the use of ARBs/ACEIs decreased significantly; thus, the use of these medications was not the main factor to the improvement in native T1 after transplantation. Additionally there was no correlation between using ACEIs/ARBs and change in native T1 (data not shown).
Clinical and biochemical parameters
We found that at 6 months after renal transplantation, heart rate and systolic and diastolic blood pressures decreased significantly. This finding probably resulted from inactivation of the sympathetic system and the renin-angiotensin-aldosterone system after transplantation. Both systems, when activated, stimulate intracellular signaling pathways, with consequent increase in protein synthesis in myocytes and fibroblasts leading to cellular hypertrophy and fibrosis [30]. Other effects are the activation of growth factors, activation of metalloproteinases, hemodynamic overload by vasoconstriction and water retention, increase in oxidative stress, and direct cytotoxic effect, leading to cell death due to necrosis or apoptosis [31–33]. Blockade of these systems plays an important role in preventing or attenuating the developmental process for replacement fibrosis.
CMR
In the CMR evaluation, considering ventricular function, volume and mass, we did not find differences at 6 months, similar to Patel [34] and Prasad et al. [35]. Patel performed the first study to serially evaluate the LVs of patients who have undergone kidney transplantation using CMR. Prasad results showed a result deriving from an adjustment of LV parameters using a gender-specific method.
In contrast, improved CMR derived LV parameters have been demonstrated in children within 6 months after transplantation [36], indicating that gender adjustment assumes particular importance in adults. The pediatric patients also had a short time on dialysis (median = 6 months), perhaps explaining lower abnormalities in cardiac structure and function. Additionally, different CMR technology, distinct reference populations and diverse study design might be the reason for this discrepancy.
In a different way from the ventricular function and mass, the native T1 was significantly reduced 6 months after renal transplantation. The native T1 time is a sensitive marker of myocardial fibrosis [19, 37–39] and we associated the decrease of native T1 with the reduction of reactive fibrosis after renal transplantation. Reactive fibrosis is secondary to neurohumoral activation that was triggered by the cellular mediators angiotensin II, aldosterone and endothelin I, [40–42] which stimulate the myofibroblasts to increase the production and deposition of collagen in the ECM. At this time, no cardiomyocyte necrosis is detected and the fibrosis can be discontinued. Thus, renal transplantation has the potential to inhibit this neurohumoral activation by improving volume overload and pressure control and thereby contribute to the regression of reactive fibrosis and prevent the progression to irreversible replacement fibrosis.
To date, no prior studies have evaluated native T1 in renal transplant recipients. Using 3 T CMR and measuring T1 times in the midventricular septum, Rutherford and Graham-Brown et al. found lower native T1 values in hemodialysis patients than the baseline values of the present study [20, 38]. An explanation for these differences may be that in the present study the mean dialysis time was longer (38 months) than that in Rutherford and Grahan-Brown’s studies (5 and 21 months, respectively) [20, 38]. There is still no standardization of native T1 values for the normal population that can differentiate between disease states and normality [43, 44], although Weingärtner et al., using a protocol similar to that of the present study (MOLLI with 3 T CMR) in 20 healthy subjects, found a native T1 of 1183 ± 47 ms [44]. We also observed that T1 values after 6 months of transplantation was not similar to normal healthy population. One explanation is that it would take a longer time to achieve values similar to those in a healthy population. Finally, it is likely that transplantation may not be able to fully reverse the myocardial fibrosis.
The discrepancies between ventricular mass/function and fibrosis in the present study are related to the specificity of the method. Thus, the studies that demonstrated a reduction of ventricular mass in post-transplant were performed using transthoracic echocardiography, which may be influenced by volume overload [45]. Furthermore, echocardiography assumes an approximately cubic LV shape when calculating the LV mass index [46]. On the other hand, the myocardial fibrosis in patients with advanced CKD [4] is better accessed by CMR, using the native T1 measurement [38, 39]. Thus, native T1 may be better correlated to morphological abnormalities in the myocardium of chronic renal patients [11, 20].
In order to explore hidden patterns in the data, we performed a cluster analysis, and a group showed no improvement of native T1. The main finding of this group was the greater rate of diabetes. Previous studies have demonstrated that high glucose concentrations can lead to pathological changes in the myocardium, including the accumulation of ECM proteins. Mechanisms responsible for these alterations may include overproduction, decreased degradation, and / or chemical modifications of ECM proteins [47]. Consequently, in diabetic patients the transplantation cannot interrupt these mechanisms that can explain the lack of decrease in native T1. In addition to diabetes, another characteristic of this cluster group is the greater baseline LV mass index. Patients with higher LV mass index also did not reach a decrease in T1 and myocardial fibrosis, possibly because these patients achieved such a striking change in cardiac structure that it became unlikely to be reversed.
Study limitations
Although native T1 time has demonstrated a positive correlation with biopsy-proven fibrosis in diseases with pressure overload [21], we could not perform histological confirmation in this study. Thus, in the absence of confirmatory biopsy, a direct inference between native T1 and myocardial fibrosis is not allowed. Another limitation was the baseline CMR at the time of transplantation. Although performing the pre-transplant CMR would be more appropriate, this is not possible with deceased donors due to long waiting list times. Then, we performed the first CMR as close to the transplant surgery as possible. Native T1 is more stable than blood T1 for variations in hematocrit and heart rate [48]. Furthermore, we conduced additional analyzes controlled for these factors and the results of native T1 were not affected by these confounders (Additional file 5). Although of sensitivity analysis, the decrease of hematocrit in the postoperative period may interfere with the analysis of native T1 resulting in lower T1 values. Additional studies with longer observation time are needed to evaluate the sequential changes of native T1 and parameters of left ventricular mass and function. However, this work is the first to evaluate the myocardium of renal transplant patients using native T1 time. The images were performed in the same apparatus, with the same magnetic field (3 T), and all the patients underwent the same imaging protocol and analyzed by a single blinded observer.
In conclusion, myocardial native T1 decreased significantly 6 months after renal transplantation. Patients that do not achieve a significant decrease in native T1 include those with diabetes and those with highest baseline LV mass index. The measurement of native T1 time by CMR may be considered an appropriate complementary method to evaluate myocardial fibrosis in renal transplant patients without using contrast.
Additional files
Statistical analysis of Two-Step Cluster. Cluster sizes and importance of the predictors. (DOCX 38 kb)
Analysis of individual cases of native T1 map at baseline and 6 months after transplantation (n = 44 before and n = 44, 6 months after transplantation). (TIFF 439 kb)
A Boxplot comparing left ventricular mass index (LVMi) at baseline and 6 months after transplantation. B: Analysis of individual cases of LVMi at baseline and 6 months after transplantation. C: Boxplot comparing Left Ventricular Mass index (LVMi) at baseline and 6 months after transplantation split into two groups (clusters). D: Analysis of individual cases of native T1 map at baseline and 6 months after transplantation splitted into two groups by Cluster analysis. (TIF 1406 kb)
Analysis of individual cases of native T1 map at baseline and 6 months after transplantation splitted into two groups by Cluster analysis. (n = 44 before and n = 44, 6 months after transplantation). (TIFF 268 kb)
Additional statistical analyzes for native T1 adjusted for confounding factors. (DOCX 20 kb)
Acknowledgments
Funding
This study was funded by the kidney transplant service UNESP, Univ Estadual Paulista through to clinical research grant.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACEi
Angiotensin-converting enzyme inhibitor
- ARB
Angiotensin II receptor blockers
- CKD
Chronic kidney disease
- CMR
Cardiovascular magnetic resonance
- CVD
Cardiovascular disease
- DM
Diabetes mellitus
- ECM
Extracellular matrix
- ECV
Extracellular volume fraction
- EF
Ejection fraction
- FOV
Field of view
- HD
Hemodialysis
- LV
Left ventricle/left ventricular
- MOLLI
Modified look-locker inversion recovery
- ROI
Region of interest
Authors’ contributions
MMC: Participated in the performance of the research and conception and design. MFB: Analysis and interpretation of data. ACVM: Analysis and interpretation of data. HSN: Participated in the performance of the research. MFV: Participated in the performance of the research. HMT: Participated in the performance of the research. AMB: Participated in the performance of the research. LGMA: Interpreted results; edited and revised manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The protocol was reviewed and approved by the institutional review board (CAAE: 40598414.9.0000.5411).
Consent for publication
Written informed consent was obtained from the patients before participation.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mariana Moraes Contti, Email: mmcontti@gmail.com.
Maurício Fregonesi Barbosa, Email: maufbarbosa@gmail.com.
Alejandra del Carmen Villanueva Mauricio, Email: alvima88@hotmail.com.
Hong Si Nga, Email: honguinha2@gmail.com.
Mariana Farina Valiatti, Email: marianavaliatti@gmail.com.
Henrique Mochida Takase, Email: henriquetakase@gmail.com.
Ariane Moyses Bravin, Email: arianemoyses@hotmail.com.
Luis Gustavo Modelli de Andrade, Phone: 55 (14) 3811-6547, Email: gustavomodelli@yahoo.com.br.
References
- 1.Baigent C, Burbury K, Wheeler D. Premature cardiovascular disease in chronic renal failure. Lancet. 2000;356:147–152. doi: 10.1016/S0140-6736(00)02456-9. [DOI] [PubMed] [Google Scholar]
- 2.Cavalcante LG, Ricardo de Souza C, Kochi AC. Left ventricular mass behaviour in hemodialysis patients during 17 years. J Bras Nefrol. 2014;37:341–348. doi: 10.5935/0101-2800.20150054. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe RA, Ashby VB, Milford EL. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 4.Mall G, Huther W, Schneider J, Lundin P, Ritz E. Diffuse intermyocardiocytic fibrosis in uraemic patients. Nephrol Dial Transpl. 1990;5:39–44. doi: 10.1093/ndt/5.1.39. [DOI] [PubMed] [Google Scholar]
- 5.Ter Maaten JM, Damman K, Verhaar MC, Paulus WJ, Duncker DJ, Cheng C, et al. Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail. 2016;18:588–598. doi: 10.1002/ejhf.497. [DOI] [PubMed] [Google Scholar]
- 6.Ritz E. Left ventricular hypertrophy in renal disease: beyond preload and afterload. Kidney Int. 2009;75:771–773. doi: 10.1038/ki.2009.35. [DOI] [PubMed] [Google Scholar]
- 7.Ritz E, Wanner C. The challenge of sudden death in dialysis patients. Clin J Am Soc Nephrol. 2008;3:920–929. doi: 10.2215/CJN.04571007. [DOI] [PubMed] [Google Scholar]
- 8.Glassock RJ, Pecoits-Filho R, Barberato SH. Left ventricular mass in chronic kidney disease and ESRD. Clin J Am Soc Nephrol. 2009;4:79–91. doi: 10.2215/CJN.04860709. [DOI] [PubMed] [Google Scholar]
- 9.Berk BC, Fujiwara K, Lehoux S. ECM remodeling in hypertensive heart disease. J Clin Invest. 2007;117:568–575. doi: 10.1172/JCI31044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radenkovic D, Weingärtner S, Ricketts L, Moon JC, Captur G. Heart Fail Rev. 2017;22:415–30. Published online 2017 Jun 16. 10.1007/s10741-017-9627-2. [DOI] [PMC free article] [PubMed]
- 11.Graham-Brown MP, Patel AS, Stensel DJ, March DS, Marsh AM, McAdam J, et al. Imaging of myocardial fibrosis in patients with end-stage renal disease: current limitations and future possibilities. Biomed Res Int. 2017;5453606. 10.1155/2017/5453606. [DOI] [PMC free article] [PubMed]
- 12.Weidemann F, Herrmann S, Störk S, Niemann M, Frantz S, Lange V, et al. Impact of myocardial fibrosis in patients with symptomatic severe aortic stenosis. Circulation. 2009;120:577–584. doi: 10.1161/CIRCULATIONAHA.108.847772. [DOI] [PubMed] [Google Scholar]
- 13.Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiac magnetic resonance. J Am Coll Cardiol. 2011;57:891–903. doi: 10.1016/j.jacc.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becker AE, Heijmans CD, Essed CE. Chronic non-ischaemic congestive heart disease and endomyocardial biopsies. Worth the extra? Eur Heart J. 1991;12:218–223. doi: 10.1093/oxfordjournals.eurheartj.a059872. [DOI] [PubMed] [Google Scholar]
- 15.Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, et al. Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation. 2010;122:138–144. doi: 10.1161/CIRCULATIONAHA.109.930636. [DOI] [PubMed] [Google Scholar]
- 16.Sado DM, Flett AS, Moon JC. Novel imaging techniques for diffuse myocardial fibrosis. Futur Cardiol. 2011;7:643–650. doi: 10.2217/fca.11.45. [DOI] [PubMed] [Google Scholar]
- 17.Kellman P, Wilson JR, Xue H, Ugander M, Arai AE. Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J Cardiovasc Magn Reson. 2012;14:63. doi: 10.1186/1532-429X-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomsen HS, Morcos SK, Almén T, Bellin MF, Bertolotto M, Bongartz G, et al. Nephrogenic systemic fibrosis and gadolinium-based contrast media: updated ESUR contrast medium safety committee guidelines. Eur Radiol. 2013;23:307–318. doi: 10.1007/s00330-012-2597-9. [DOI] [PubMed] [Google Scholar]
- 19.Małek ŁA, Werys K, Kłopotowski M, Śpiewak M, Miłosz-Wieczorek B, Mazurkiewicz Ł, et al. Native T1-mapping for non-contrast assessment of myocardial fibrosis in patients with hypertrophic cardiomyopathy - comparison with late enhancement quantification. Magn Reson Imaging. 2015;33:718–724. doi: 10.1016/j.mri.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 20.Rutherford E, Talle MA, Mangion K, Bell E, Rauhalammi SM, Roditi G, et al. Defining myocardial tissue abnormalities in end-stage renal failure with cardiac magnetic resonance imaging using native T1 mapping. Kidney Int. 2016;90:845–852. doi: 10.1016/j.kint.2016.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alqahtani F, Aljohani S, Almustafa A, Alhijji M, Ali O, Holmes DR, et al. Human non-contrast T1 values and correlation with histology in diffuse fibrosis. Heart. 2013;99:932–937. doi: 10.1136/heartjnl-2012-303052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van den Boomen M, Slart RHJA, Hulleman EV, Dierckx RAJO, Velthuis BK, van der Harst P, et al. Native T1 reference values for nonischemic cardiomyopathies and populations with increased cardiovascular risk: a systematic review and meta-analysis. J Magn Reson Imaging. 2018;47:891–912. doi: 10.1002/jmri.25885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, et al. Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR working Group of the European Society of cardiology consensus statement. J Cardiovasc Magn Reson. 2013;15:92. doi: 10.1186/1532-429X-15-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogers T, Dabir D, Mahmoud I, Voigt T, Schaeffter T, Nagel E, et al. Standardization of T1 measurements with MOLLI in differentiation between health and disease – the ConSept study. J Cardiovasc Magn Reson. 2013;15:78. doi: 10.1186/1532-429X-15-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLachlan GJ. Cluster analysis and related techniques in medical research. Stat Methods Med Res. 1992;1:27–48. doi: 10.1177/096228029200100103. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad T, Pencina MJ, Schulte PJ, O'Brien E, Whellan DJ, Piña IL, et al. Clinical implications of chronic heart failure phenotypes defined by cluster analysis. J Am Coll Cardiol. 2014;64:1765–1774. doi: 10.1016/j.jacc.2014.07.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horiuchi Y, Tanimoto S, Latif AHMM, Urayama KY, Aoki J, Yahagi K, et al. Identifying novel phenotypes of acute heart failure using cluster analysis of clinical variables. Int J Cardiol. 2018;262:57–63. doi: 10.1016/j.ijcard.2018.03.098. [DOI] [PubMed] [Google Scholar]
- 28.Díez J, Querejeta R, López B, González A, Larman M, Martínez Ubago JL. Losartan-dependent regression of myocardial fibrosis is associated with reduction of left ventricular chamber stiffness in hypertensive patients. Circulation. 2002;105:2512–2517. doi: 10.1161/01.CIR.0000017264.66561.3D. [DOI] [PubMed] [Google Scholar]
- 29.Epifanio HB, Zornoff LA, Matsubara BB. Myocardial remodeling after experimental acute myocardial infarction in rats. Effect of renin-angiotensin-aldosterone blockade. Arq Bras Cardiol. 2005;84:10–14. doi: 10.1590/S0066-782X2005000100003. [DOI] [PubMed] [Google Scholar]
- 30.Azevedo PS, Polegato BF, Minicucci MF, Paiva SA, Zornoff LA. Cardiac remodeling: concepts, clinical impact, pathophysiological mechanisms and pharmacologic treatment. Arq Bras Cardiol. 2016;106:62–69. doi: 10.5935/abc.20160005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sayer G, Bhat G. The renin-angiotensin-aldosterone system and heart failure. Cardiol Clin. 2014;32:21–32. doi: 10.1016/j.ccl.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 32.Albuquerque FN, Brandão AA, Silva DA, Mourilhe-Rocha R, Duque GS, Gondaret AFP, et al. Angiotensin-converting enzyme genetic polymorphism: its impact on cardiac remodeling. Arq Bras Cardiol. 2014;102:70–79. doi: 10.5935/abc.20130229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Florea VG, Cohn JN. The autonomic nervous system and heart failure. Circ Res. 2014;114:1815–1826. doi: 10.1161/CIRCRESAHA.114.302589. [DOI] [PubMed] [Google Scholar]
- 34.Patel RK, Mark PB, Johnston N, McGregor E, Dargie HJ, Jardine AG. Renal transplantation is not associated with regression of left ventricular hypertrophy: a magnetic resonance study. Clin J Am Soc Nephrol. 2008;3:1807–1811. doi: 10.2215/CJN.01400308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prasad GVR, Yan AT, Nash MM, Kim SJ, Wald R, Wald R. Determinants of left ventricular characteristics assessed by cardiac magnetic resonance imaging and cardiovascular biomarkers related to kidney transplantation. Can J Kidney Health Dis. 2018;5:2054358118809974. doi: 10.1177/2054358118809974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schaefer B, Rusai K, Toth A, Pasti K, Ujszaszi A, Kreko M, et al. Cardiac magnetic resonance imaging in children with chronic kidney disease and renal transplantation. Pediatr Transplant. 2012;16:350–356. doi: 10.1111/j.1399-3046.2012.01672.x. [DOI] [PubMed] [Google Scholar]
- 37.Graham-Brown MP, Rutherford E, Levelt E, March D, Churchward DR, Stensel DJ, et al. Native T1 mapping: inter-study, inter-observer and inter-center reproducibility in hemodialysis patients. J Cardiovasc Magn Reson. 2017;19:21. doi: 10.1186/s12968-017-0337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graham-Brown MP, March DS, Churchward DR, Stensel DJ, Singh A, Arnold R, et al. Novel cardiac nuclear magnetic resonance method for noninvasive assessment of myocardial fibrosis in hemodialysis patients. Kidney Int. 2016;90:835–844. doi: 10.1016/j.kint.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 39.Everett RJ, Stirrat CG, Semple SI, Newby DE, Dweck MR, Mirsadraee S. Assessment of myocardial fibrosis with T1 mapping MRI. Clin Radiol. 2016;71:768–778. doi: 10.1016/j.crad.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 40.Willenheimer R. Left ventricular remodelling and dysfunction. Can the process be prevented? Int J Cardiol. 2000;72:143–150. doi: 10.1016/s0167-5273(99)00182-5. [DOI] [PubMed] [Google Scholar]
- 41.Florea VG, Mareyev VY, Samko AN, Orlova IA, Coats AJS, Belenkov YN. Left ventricular remodelling: common process in patients with different primary myocardial disorders. Int J Cardiol. 1999;68:281–287. doi: 10.1016/S0167-5273(98)00362-3. [DOI] [PubMed] [Google Scholar]
- 42.Yoshiyama M, Nakamura Y, Omura T, Izumi Y, Matsumoto R, Oda S, et al. Angiotensin converting enzyme inhibitor prevents left ventricular remodelling after myocardial infarction in angiotensin II type 1 receptor knockout mice. Heart. 2005;91:1080–1085. doi: 10.1136/hrt.2004.035618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goebel J, Seifert I, Nensa F. Can native T1 mapping differentiate between healthy and diffuse diseased myocardium in clinical routine cardiac MR imaging? PLoS One. 2016;11:e0155591. doi: 10.1371/journal.pone.0155591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weingärtner S, Meßner NM, Budjan J, Loßnitzer D, Mattler U, Papavassiliu T, et al. Myocardial T1-mapping at 3T using saturation-recovery: reference values, precision and comparison with MOLLI. J Cardiovasc Magn Reson. 2017;18:84. doi: 10.1186/s12968-016-0302-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hunold P, Vogt FM, Heemann UW, Zimmermann U, Barkhausen J. Myocardial mass and volume measurement of hypertrophic left ventricles by MRI--study in dialysis patients examined before and after dialysis. J Cardiovasc Magn Reson. 2003;5:553–561. doi: 10.1081/JCMR-120025230. [DOI] [PubMed] [Google Scholar]
- 46.Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55:613–618. doi: 10.1161/01.CIR.55.4.613. [DOI] [PubMed] [Google Scholar]
- 47.Asbun J, Villarreal FJ. The pathogenesis of myocardial fibrosis in the setting of diabetic cardiomyopathy. J Am Coll Cardiol. 2006;47:693–700. doi: 10.1016/j.jacc.2005.09.050. [DOI] [PubMed] [Google Scholar]
- 48.Piechnik SK, Ferreira VM, Lewandowski AJ, Ntusi NA, Banerjee R, Holloway C. Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson. 2013;15:13. doi: 10.1186/1532-429X-15-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Statistical analysis of Two-Step Cluster. Cluster sizes and importance of the predictors. (DOCX 38 kb)
Analysis of individual cases of native T1 map at baseline and 6 months after transplantation (n = 44 before and n = 44, 6 months after transplantation). (TIFF 439 kb)
A Boxplot comparing left ventricular mass index (LVMi) at baseline and 6 months after transplantation. B: Analysis of individual cases of LVMi at baseline and 6 months after transplantation. C: Boxplot comparing Left Ventricular Mass index (LVMi) at baseline and 6 months after transplantation split into two groups (clusters). D: Analysis of individual cases of native T1 map at baseline and 6 months after transplantation splitted into two groups by Cluster analysis. (TIF 1406 kb)
Analysis of individual cases of native T1 map at baseline and 6 months after transplantation splitted into two groups by Cluster analysis. (n = 44 before and n = 44, 6 months after transplantation). (TIFF 268 kb)
Additional statistical analyzes for native T1 adjusted for confounding factors. (DOCX 20 kb)
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.