Abstract
Splenic cysts are not so common in incidence. Only 800–850 cases have been reported till now in the literature. Splenic cysts can be further classified into parasitic and non-parasitic cysts. Non-parasitic cyst is further subdivided into true and false or pseudocyst. Pseudocysts are those who are lacking any epithelial lining. Splenic pseudocysts are usually a result of trauma, infection or infarction. We present a case of splenic pseudocyst that was diagnosed incidentally on routine check-up, and we managed this case with minimally invasive approach with complete preservation of spleen and only removal of pseudocyst. We used indocyanine green dye that helped us in complete delineation of splenic parenchyma and vascular structure adjacent to it. In our view, as in this study also, adopting a new technique that can be helpful in better treatment of the patient and if it can change the surgical outcome of the disease in favour of the patient, it should be encouraged.
Keywords: Cystectomy, indocyanine green, pseudocyst, splenectomy, splenic cyst
INTRODUCTION
Splenic cysts are not so common in incidence. Only 800–850 cases have been reported till now in the literature. They constitute around <1% of splenectomy specimens or in autopsy cases. Splenic cysts can be further classified into parasitic and non-parasitic cysts. Non-parasitic cyst is further subdivided into true and false or pseudocyst. They can be divided into benign or malignant cyst. True cysts are those that have epithelial lining, while false or pseudocysts are those that lack any epithelial lining, meaning their wall is composed of either fibrous tissue or some subcutaneous tissue. Splenic pseudocysts are usually a result of trauma, infection or infarction. Usually they are asymptomatic. Symptomatic only when either oversized so that compress surrounding viscera or because of some secondary infection or because of rupture. In symptomatology of splenic pseudocyst, it is usually diagnosed incidentally either in splenectomy specimen or in autopsy cases, while in symptomatic cases, it represents as left upper abdominal pain, nausea, vomiting, or if infected secondarily can present with fever, or in cases of rupture, symptoms of abdominal distension or very rarely peritonitis. It is very important to make a diagnosis of splenic pseudocyst and to differentiate mainly between hydatid cysts as the management plan gets changed according to the type of splenic cyst. They are usually managed with splenectomy or very rarely with preservation of spleen either in toto or partial. Indocyanine green (ICG) is a fluorescent dye which is used in medicine as an indicator substance (e.g., for photometric hepatic function diagnostics and fluorescence angiography) in cardiac, circulatory, hepatic and ophthalmic conditions.[1]
CASE REPORT
We report here a very rare case of splenic cyst that was diagnosed incidentally on routine investigation and managed with laparoscopic cystectomy, with preserving the spleen as a whole using ICG dye.
It is a very new modality of treating splenic cysts. The excised cyst which was sent for histopathological examination turned out into a splenic pseudocyst, lacking epithelial lining [Figure 1].
Figure 1.
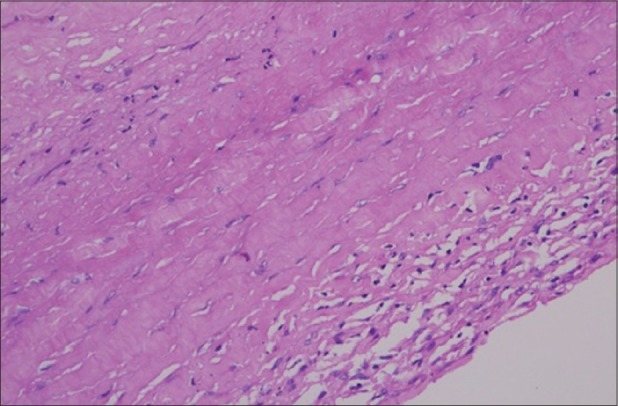
Cyst wall lacking epithelium and made of fibrocollagenous tissue with focal lymphocytic infiltrate (×40)
A 25-year-old gentleman, resident of Haryana, with no comorbid condition, underwent routine investigation and ultrasound abdomen examination for a job interview health check-up. On ultrasound imaging abdomen, it showed a large splenic cyst measuring 120 mm × 140 mm. The patient was further advised for contrast-enhanced computed tomography (CT) which was suggestive of large 130 mm × 140 mm splenic cyst with regular outline and thin wall, with no calcification and CT no. 8–15 HU [Figure 2]. The patient and his relative were discussed with all possible options including exploratory laparotomy, laparoscopy, partial and complete splenectomy and only cystectomy with complete preservation of spleen. As the cyst was not oversized, asymptomatic and not compressing the hilum or adjacent viscera, the plan was complete removal of splenic cyst with complete preservation of spleen or at maximum partial splenectomy, so the minimally invasive approach was chosen, and in addition, ICG dye was also used to help in identifying the splenic parenchyma and adjacent vascular structures including splenic artery and vein. ICG dye helped a lot in identifying and complete delineating of the splenic cyst, normal splenic parenchyma and vascular structure. We were able to manage the patient's disease with minimal invasive approach-laparoscopic cystectomy with complete preservation of spleen by using ICG dye.
Figure 2.
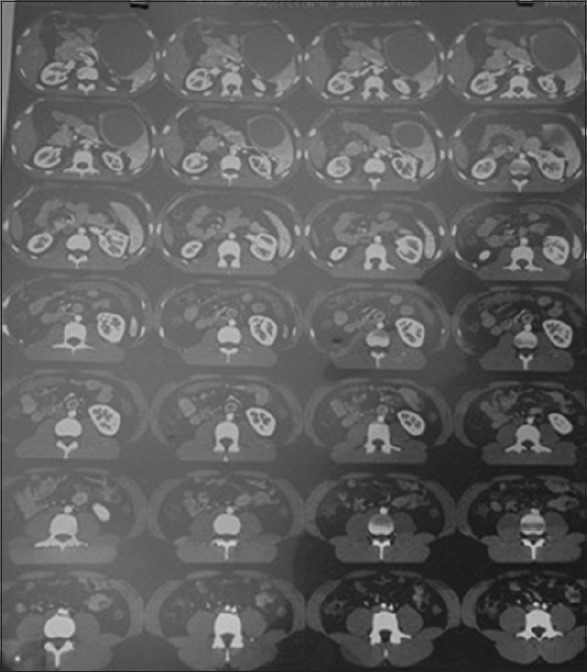
Computed tomography scan showing large splenic cyst
Pre-operative preparation and the port position [Figure 3] were exactly the same as in any standard procedure of laparoscopic cystectomy or splenectomy, the only difference was that we used ICG dye while operating. 2 ml of ICG dye was diluted with 8 ml of normal saline and injected intravenously after creating pneumoperitoneum that helped us identifying splenic parenchyma. After completing diagnostic laparoscopy, we injected another 2 ml of ICG dye intravenously that further added up in delineating splenic pseudocyst. After injecting the ICG dye, splenic parenchyma and the surrounding vessels were clearly identified [Figure 4], and a gross difference could be elicited. Using ICG dye helped us to identify the cyst and its wall very clearly, and we were able to manage this case only with cystectomy and preserving the whole spleen.
Figure 3.

Standard port position of laparoscopic splenic cystectomy
Figure 4.

Indocyanine green dye showing clear delineation of splenic viscera and the pseudocyst
The patient tolerated the procedure well and he was discharged and sent home on post-operative day 2 in stable condition tolerating normal diet.
DISCUSSION
Splenic pseudocysts are not so common in incidence and are very difficult to diagnose preoperatively; they usually remain asymptomatic (30%–60% cases). Usually, they are a result of previous trauma, or some infection or infarction or it can be associated with acute or chronic pancreatitis. When symptomatic, they present as left upper abdominal pain, nausea or vomiting. Whenever some benign cyst is suspected preoperatively, the spleen should be preserved so that the risk of overwhelming post-splenectomy infection can be avoided or minimised, particularly in children or young patients.[2] Some non-surgical treatment modalities such as percutaneous drainage with or without injection of a chemical agent can reduce the size of large cysts, but it is usually associated with a high rate of recurrence.[3] Total splenectomy is usually indicated only in cases of oversized cyst, or splenic hilum cyst or cysts covered with splenic parenchyma.[4] In an attempt of preserving the spleen, close observation, percutaneous drainage, marsupialization of splenic cyst with decapuslarization or complete cystectomy with partial splenectomy have been tried in the past. Somehow, these procedures did not get so much of success and splenectomy is still considered the standard treatment of choice, particularly in the above-mentioned criteria.[5] Verma et al. in their study reported two cases of splenic pseudocyst post-abdominal trauma cases, in which they managed with exploratory laparotomy, preserving spleen in one case, while doing splenectomy and cystectomy in another case.[6] Shresthaand Shrestha also reported a case of splenic pseudocyst that was initially treated as hydatid cyst of spleen with anthelmintics and later on treated with exploratory laparotomy and splenectomy.[7] In our case, on complete medical history, no history of trauma could be elicited, totally incidental finding in a young asymptomatic patient. We managed the case with minimally invasive approach (laparoscopic complete cystectomy), but with complete preservation of the spleen. In this case, we used ICG dye as an adjunctive tool to identify and delineate splenic parenchyma and splenic vasculature. With the use of this dye, we were able to manage this case with complete separation and removal of cyst and cyst wall from splenic parenchyma with very minimal bleeding. To the best of our knowledge and by going through the previous literatures in PubMed, we could not find any article publishing this new technique of treatment.
CONCLUSION
Splenic cysts are usually asymptomatic. Although very rare in incidence, still if a pre-operative diagnosis of benign cyst is made, the surgeon's attempt should be to preserve the spleen as much as possible. In today's era of minimally invasive technique, using an adjunct such as ICG dye can reduce the operating time, minimise the intraoperative bleeding, and can help in the delineation of viscera and preservation of spleen, without any side effects. In our view, as in this study also, adopting a new technique that can be helpful in better treatment of the patient and if it can change surgical outcome of the disease in favour of the patient, it should be encouraged. However, still, long-term data on more number of patients and few more studies are needed before labelling it (laparoscpic cystectomy using ICG dye)as standard or routine way of treating splenic psuedocyst.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Indocyanine Green Solution. NIH. National Cancer Institute. [Last retrieved on 2012 Dec 01]. Available from: https://en.wikipedia.org/wiki/Indocyanine_green .
- 2.Eraklis AJ, Kevy SV, Diamond LK, Gross RE. Hazard of overwhelming infection after splenectomy in childhood. N Engl J Med. 1967;276:1225–9. doi: 10.1056/NEJM196706012762203. [DOI] [PubMed] [Google Scholar]
- 3.Moir C, Guttman F, Jequier S, Sonnino R, Youssef S. Splenic cysts: Aspiration, sclerosis, or resection. J Pediatr Surg. 1989;24:646–8. doi: 10.1016/s0022-3468(89)80711-0. [DOI] [PubMed] [Google Scholar]
- 4.Stoidis CN, Spyropoulos BG, Misiakos EP, Fountzilas CK, Paraskeva PP, Fotiadis CI, et al. Spontaneous regression of a true splenic cyst: A case report and review of the literature. Cases J. 2009;2:8730. doi: 10.4076/1757-1626-2-8730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu HM, Kortbeek JB. Management of splenic pseudocysts following trauma: A retrospective case series. Am J Surg. 2006;191:631–4. doi: 10.1016/j.amjsurg.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Verma A, Yadav A, Sharma S, Saini D, Om P, Khoja H, et al. A rare splenic pseudocyst. J Surg Case Rep 2013. 2013 doi: 10.1093/jscr/rjt086. pii: rjt086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shrestha AL, Shrestha P. A rare encounter with an expanding pseudocyst of the spleen. Case Rep Gastrointest Med. 2017;2017:9896856. doi: 10.1155/2017/9896856. [DOI] [PMC free article] [PubMed] [Google Scholar]


