Abstract
Objective:
The remarkable progress made in confronting the global HIV epidemic offers a unique opportunity to address the increasing threat of noncommunicable diseases (NCDs). However, questions remain about how to enhance the HIV platforms to deliver integrated HIV and NCD care to people living with HIV (PLHIV) in sub-Saharan Africa (SSA). We aimed to develop a priority research agenda to advance this effort.
Methods:
Researchers, policymakers, and implementers from the United States and SSA conducted three scoping reviews on HIV/NCD prevention and care focused on clinical, health system, and community levels. Based on the review findings and expert inputs, we conducted iterative consensus-development activities to generate a prioritized research agenda.
Results:
Population-level data on NCD prevalence among PLHIV in SSA are sparse. The review identified NCD screening and management approaches that could be integrated into HIV programs in SSA. However, few studies focused on the effectiveness, cost, and best practices for integrated chronic care platforms, making it difficult to derive policy recommendations. To address these gaps, we propose a prioritized research agenda focused on developing evidence-based service delivery models, increasing human capacity through workforce education, generating data through informatics platforms and research, managing the medication supply chain, developing new financing and sustainability models, advancing research-informed policy, and addressing other crosscutting health system issues.
Conclusion:
Based on collaborative, interdisciplinary efforts, a research agenda was developed to provide guidance that advances efforts to adapt the current health system to deliver integrated chronic care for PLHIV and the population at large.
Keywords: chronic care, HIV, noncommunicable disease, research agenda, sub-Saharan Africa
Introduction
There has been remarkable progress in confronting the global HIV epidemic. More than 19.5 million people living with HIV (PLHIV) have received access to antiretroviral therapy, and the number of new HIV infections appears to be decreasing in several countries [1]. Investments in research, particularly in identifying effective HIV prevention and treatment methods, have played a significant role in this success [1]. As the scale-up of HIV treatment has enabled PLHIV to live longer, noncommunicable diseases (NCDs), often referred to as non-AIDS events, have become major causes of morbidity and mortality [2–4]. This new reality is consistent with the overall emerging crisis of NCDs in sub-Saharan Africa (SSA) [5]. In response, global health agencies, such as the WHO and the Joint United Nations Program on HIV/AIDS, have recently called for eliminating parallel health systems and suggested integrating care for NCDs into existing HIV care platforms, and the Council on Foreign Relations suggested that HIV platforms could be expanded to include treatment for NCDs [5–7]. This particular approach to developing an enhanced health system avoids making duplicate platforms by creating one that applies the lessons learned from HIV care and treatment to NCDs. To address the developing threat of NCDs among PLHIV through integrated HIV/NCD care, programs need new evidence-based models and guidance. Little is known about the extent to which NCDs are being managed in HIV care settings and what needs to be done to ensure that such care is delivered. In response, we designed a consensus process to assess current evidence and experience and to establish a research agenda for enhancing NCD management in HIV care settings in SSA.
The Center for Global Health Studies at the US National Institutes of Health’s (NIH) Fogarty International Center (FIC) established an interagency, interdisciplinary team to develop a research agenda focused on the prevention and management of selected, high-burden NCDs in PLHIV in SSA. This effort entitled, ‘Research to Guide Practice: Enhancing HIV/AIDS Platforms to Address NCDs in SSA’ (the HIV/NCD project), was managed through an interagency group and guided by an interdisciplinary, international Steering Committee led by select members of the FIC Advisory Board. More than 40 individuals (project members) involved in global health research, policy development, community engagement, research funding, and program design and management in SSA countries provided input on currently available evidence regarding prevention, care, and treatment for HIV and four selected NCDs in SSA: cardiovascular diseases, cervical cancer, depression, and type 2 diabetes. These NCDs were selected based on the following: available data of the condition or related risk factors in PLHIV; known patho-physiological connection with HIV; association with reported HIV outcomes including morbidity and mortality amongst PLHIV; known costeffective interventions to prevent and treat the selected NCD in low-resource settings [8–16]; and NIH institute interest in and ability to engage specific areas of focus. Although the focus of this effort was on countries in SSA, it was anticipated that the lessons and strategies that emerge from these countries will likely be relevant to other low-resource settings globally.
Methods
Through a process outlined in Table 1, we performed literature reviews and conducted priority setting meetings and workshops culminating with the writing and publication of the articles in this supplement: Research to Guide Practice: Enhancing HIV/AIDS Platform to Address Non-Communicable Diseases in sub-Saharan Africa. Project members conducted scoping reviews ofwhat is currently being done in the field of NCD prevention, care, and treatment for PLHIV in SSA by examining peer-reviewed and gray literature focused on the four selected NCDs [17]. We searched the bibliographic databases PubMed/MEDLINE and Scopus in February, April, and November of 2015, and March of 2016 to identify peer-reviewed literature, published after 2010, on PLHIV and NCDs in low-income and middle-income countries. Search terms used included controlled vocabulary terms (Medical Subject Headings) and keywords recommended by subject matter experts and by reviewing key articles and included variations of key concepts such as PLHIV, NCDs, SSA, continuum of care, prevalence, health systems, behavior change, and dissemination. In addition to literature searches, the bibliographies of key articles and systematic reviews were examined for relevant literature, and gray literature was identified via searches of Google, Google Scholar, and key organizational websites. Project members reviewed the relevant articles related to the four NCDs of interest among PLHIV. The resulting analysis reported and identified gaps for integration of NCDs into the HIV clinical continuum of care, piloting and scaling-up an integrated chronic care health system, and enhancing HIV/NCD community engagement and health promotion efforts.
Table 1.
Research agenda development stages.
| Stage 1 | Determine parameters of the HIV/NCD project and establish teams for the scoping reviews |
| Stage 2 | Compile and review scoping reviews and prioritize initial research questions |
| Stage 3 | Conduct workshop on HIV/NCD models in lowincome and middle-income countries and outline possible supplement on HIV/NCD integration |
| Stage 4 | Research and draft articles for the Research to Guide Practice: Enhancing HIV/AIDS Platform to Address Non-Communicable Diseases in sub-Saharan Africa supplement |
| Stage 5 | Compile research agendas from stages 1–4 |
NCD, noncommunicable disease.
Project members examined the scoping reviews and identified research gaps that informed the development of the prioritized research agenda presented in this article. Through the analysis and discussion, they identified pilot HIV/NCD programs in SSA that were critically examined at a subsequent workshop as potential scalable models. The result of the reviews, workshop, and supplement planning is a series of 11 articles developed by the project members and their collaborators that articulate the urgent research and capacity-building priorities associated with managing NCDs among PLHIV Each article presents the state of the science, lessons learned, and key research questions pertaining to specific aspects of building and sustaining an integrated chronic care platform [18].
Results
The scoping reviews identified substantial gaps in knowledge and significant opportunities for future research to determine the most effective way to integrate NCD management into existing HIV platforms. One important finding was that data on the prevalence and incidence of NCDs amongst PLHIV in SSA are sparse. Although there are a few published surveys establishing the prevalence of NCDs and related risk factors in the general population [19] and even fewer surveys that have routinely gathered NCD incidence or risk factor prevalence among PLHIV, there is some available information on these NCDs and their risk factors among PLHIV in SSA [20]. Policymakers and implementers reinforced the need for these data to obtain unbiased estimates ofthe magnitude of the NCD threat in PLHIV, without which it is difficult to assess the size of the needed investment in NCD for PLHIV or to determine any progress made once such care is initiated [21].
Members determined that HIV treatment strategies can incorporate NCDs to improve clinical outcomes and primary and secondary prevention for both HIV and NCDs. Although the gradual rise of global NCDs presents a different scenario than the swift and deadly global HIV epidemic, members found that the systems required to address both chronic infections such as HIV and noninfectious chronic diseases have common elements that could leverage existing health system structures heretofore focused solely on HIV prevention and treatment. The review also noted that there were few published studies that described programs that integrated HIV and NCD care which makes it difficult to extrapolate the results to policy recommendations for scale-up. Much research is needed in this area. Recognizing that integrating HIV and NCD services at scale requires leveraging the underlying health system structures, project members further identified the research priorities related to various health system components in SSA including the health workforce [22], supply chain [23], health promotion [24], healthcare delivery models [25], cost and cost-effectiveness [26], and health policy [27].
Another key finding is the need for ongoing engagement between research and programs/policies that will ensure that there is adequate knowledge exchange such that studies take into account the concerns and experiences of implementers and policymakers and research results are translated into new care paradigms. In addition, community and patient engagement is critical to ensuring that implemented activities are acceptable to and embraced by the key stakeholder population. Efforts to combat the global HIV epidemic have relied upon collaborative partnerships and provide many lessons learned about how to form and maintain these collaborations [28]. Thus, implementation science, which relies on key stakeholder involvement, provides an opportunity to study HIV/NCD integration activities in real-world settings and at scale [29].
As an outcome of both the scoping reviews and the articles included in the supplement, members developed robust research agendas that outline the fundamental areas for future development (Table 2). This agenda is presented through a modification of WHO’s health system building blocks (Fig. 1) that represents the foci of research activities necessary for developing an integrated chronic care platform.
Table 2.
Research agenda for HIV/noncommunicable disease integration.a
| Service delivery models |
| What are the appropriate NCD diagnostic tests and medications that are available for PLHIV in LMICs? |
| What are the advantages/disadvantages of point-of-care vs. laboratory testing for NCD screening and diagnosis amongst PLHIV? |
| What are the best practices for optimizing linkage to and retention in care of patients with NCDs in HIV programs? |
| Should all patients with NCDs/NCD risk factors be managed in the same way, or should ‘triage’ decisions be made based on risk stratification? |
| What are current evidence-based approaches for NCD management among PLHIV in LMICs? [19] |
| What impact will NCD integration into HIV programs have on visit length, wait times, and workflow? [21] |
| Does integration of NCDs into HIV programs have an impact on HIV treatment, in terms of adherence, retention, quality, patient satisfaction, stigma, or virologic/immunologic outcomes? [21,28] |
| What are the key challenges and best evidence based practices for the screening, treatment, and care of NCDs among PLHIV in LMICs? [19] |
| How can we optimize the delivery of integrated HIV/NCD services (including a robust supply chain) within the HIV care setting? [28] |
| What models of care integration exist across the care continuum in SSA for HIV and NCDs? [24] |
| What are optimal models for the differentiated care of patients with both stable HIV and stable NCDs? [21] |
| Human capacity |
| What training models effectively educate the healthcare work force on HIV and NCDs? |
| How can we build in-country capacity to improve care for NCDs amongst PLHIV? [26] |
| Which clinical cadres should provide screening and diagnostic services, initiate and manage treatment, and dispense and distribute medication for various NCDs? [21] |
| How can we build in-country implementation science research capacity? [28] |
| Information, evaluation, and research |
| What is the impact of innovative technologies and electronic medical records on the clinical management of people with NCDs and HIV? |
| How can local health management information systems be utilized to minimize additional data collection burdens arising from integrated care? [21] |
| At what level should health information systems be updated to facilitate efficient monitoring and evaluation of integrated service delivery? [21] |
| How can we improve population-level data collection of NCDs and their risk factors? [19] |
| Supply chain |
| How do we improve procurement mechanisms to ensure quality medications for NCDs are available and affordable? |
| What is the most effective innovative financing for supply chain resource mobilization? [22] |
| What novel recruitment, training, and employment interventions can be used to fill supply chain workforce gaps? [22] |
| What are some innovative, cost-effective warehouse and transport designs for housing and distributing NCD commodities? [22] |
| What standards and technologies are needed across platforms to ensure quality NCD service and commodity delivery? [22] |
| How can one accurately and reliably forecast commodity needs? [22] |
| Financing and economics |
| What is the financial cost of population-level scale up of NCD prevention, screening, care, and treatment programs? [28] |
| Do current economic assessments and available data support the integration of HIV/NCD programs and care? [25] |
| What is the existing economic evidence for integrated HIV/NCD strategies in LMICs with regards to cost and impact?[25] |
| What are the critical gaps in knowledge on the economics of HIV/NCD integration? [25] |
| What are the gaps in data and how can longitudinal data be used to look at the long-term costs/benefits of NCD treatment? [25] |
| What is the ideal minimum economic dataset and what variables should be captured in an economic evaluation of integrated care? [25] |
| How can cost-effectiveness analyses be used to evaluate the integration of HIV/NCD care? [25] |
| What information is needed to assess the interactions of multiple NCDs, including interactions between CVD, cancer, and mental health risks over time? [25] |
| Is it feasible to harmonize and standardize HIV and NCD economic models, and their methods, data sources, and assumptions? [25] |
| Policy, governance, leadership |
| What are the policy changes (e.g., taxation of tobacco) necessary for population-wide NCD prevention among PLHIV? Are they different from those applied to the general population? [26] |
| What constitutes a ‘mandatory minimum’ level of top-down guidance to catalyze sub-national action to integrate services (e.g., national directive; national directive+guidelines; national directive+guidelines+training; etc.)? [21] |
| What are policy level opportunities and challenges for NCD and HIV care integration and scale-up? [26,28] |
| What are the evidence needs and evidence generation activities that would support decisions surrounding HIV/NCD policies? [26] |
| How can the HIV/NCD integration policy development process be adequately supported by funding mechanisms? [26] |
| What are best practices for science-informed HIV/NCD integration policy that can lead to scale-up? [26] |
| What governance models can inform a national and subnational approach to integrated care? [21] |
| What is the political economy of HIV/NCD integration – and what strategies can be employed to minimize barriers to planning and implementation? [21] |
| Health promotion |
| What is the impact of community engagement and awareness campaigns on NCD prevention for PLHIV? |
| How can coordination of community engagement campaigns be synergistic in lowering individual NCD risk and enhancing NCD care and its outcomes? How can this be evaluated? |
| What are the best practices for community engagement to provide support for existing HIV and NCD prevention, care, and treatment interventions? How can evidence-based NCD prevention interventions be integrated into HIV prevention initiatives without undermining HIV prevention outcomes? |
| How do we effectively reach marginalized communities and vulnerable populations? How do population differences (e.g., gender and urbanization) inform NCD prevention strategies? [23,28] |
| What HIV communication for behavior change strategies have developed and how have they been successfully leveraged to support health promotion activities in SSA? [23] |
| What communication for behavior change strategies have been applied to individuals with HIV, also at risk of NCDs in SSA? [23] |
| How does the integration of HIV and NCD communication interventions improve service provision and service demand? [23] |
| How do we create understanding and appeal of engaging in health practices – including prevention, care seeking, and self-management – that address both NCD and HIV? [28] |
| What are effective strategies and methods for NCD behavioral interventions in PLHIV? [23] |
| Partnerships |
| What roles do the various stakeholders play in care integration and how can sustainable mutually beneficial private public partnerships be established? [24] |
| Cross-cutting |
| How do we assess organizational, site, and community capacity for integration of NCD diagnosis and treatment strategies into current healthcare structures? |
| What are the major research gaps regarding implementation of integrated models of care and their scale up in SSA? [24] Is there an optimal model of integrated HIV and NCD care? [24] |
| What is the morbidity and mortality impact of population-level scaling up of NCD prevention, screening, care, and treatment programs? [28] |
| What are the prevalence of NCDs and their risk factors in HIV populations in SSA? [19] |
| What are key challenges and viable approaches to integrated comprehensive care? [24] |
| How do we enhance health systems to provide integrated HIV/NCD prevention care and treatment? [26] |
| What has already been done to incorporate NCD care into existing HIV care systems and programs in LMICs? For PLHIV? For the general public? Key challenges? [24] |
| What are the clinical and process outcomes of various integrated care models? [24] |
| What are the most common challenges facing national health program efforts to integrate HIV and NCDs treatment and care? [25] |
| How can we improve the fidelity of integrated HIV/NCD services? [28] |
| How do we culturally adapt integrated HIV/NCD services for different countries and contexts within SSA? [28] |
| How can qualitive improvement initiatives from other chronic care and integration programs inform HIV/NCD services? [21] |
LMIC, low-income and middle-income country;PLHIV, people living with HIV;SSA, sub-Saharan Africa.
Research questions developed through scoping reviews, project member discussions and each article in the supplement.
Fig. 1.
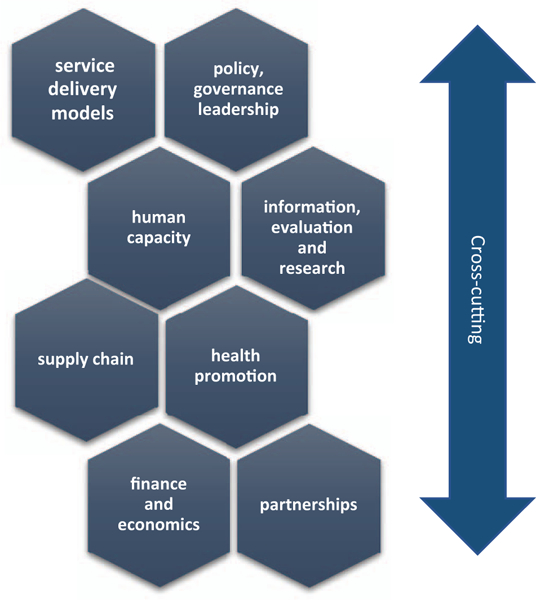
Mapping the research article.
The identified research questions map across these health system building blocks and include questions that are cross-cutting in nature. Table 2 outlines the research agenda initially developed through the scoping reviews and project member discussions and the set of research questions from each article in the supplement. These questions fall into four thematic areas:
-
(1)
Burden of disease data of NCDs among PLHIV to understand the magnitude of the current and ongoing chronic care needs and make the case for integrated screening and treatment.
-
(2)
Implications of effective chronic care integration across the health system, including evidence for point-of-care NCD prevention, care, and treatment, implementation and scaleup of services, modifying underlying health system structures, and policy initiatives to enhance sustainability.
-
(3)
Implementation science advances and capacity to answer research questions related to integration and assess effective approaches to evolving NCD care for PLHIV.
-
(4)
Partnership and stakeholder engagement, especially national government agencies, in the research agenda to ensure responsive and continuous services for integrated chronic care.
Discussion
As countries seek to address the growing NCD epidemic in SSA, new evidence to address gaps in knowledge is urgently needed. If implemented, the research agenda we propose aims to generate this evidence across critical areas of the health system to enable evidence-informed scale up of HIV/NCD care services for PLHIV. We believe that this research will also be relevant to and inform chronic care for the general population beyond PLHIV For instance, the development of a reliable supply chain that can accommodate diagnostic and treatment supplies for a myriad of conditions beyond HIV could be scaled up to the general population. Likewise, a health workforce capable of caring for NCDs among PLHIV could also address chronic diseases in the general population.
The diversity of research questions identified through the HIV/NCD Project requires the engagement of a wide range of scientific disciplines, including clinical research, healthcare management science, health economics, behavioral and communications science, health systems research, policy research, information technology, and epidemiology and surveillance. Implementation science will play a key role in informing efforts to effectively integrate known services and bring such innovations to scale.
There are encouraging signs of efforts to address some of the questions identified in the research agenda. Several NIH institutes and centers, including the National Institute of Mental Health, the National Cancer Institute, the National Heart, Lung and Blood Institute, and the FIC, all members of this project, have established funding announcements and notices that provide support to answer the key questions in the research agenda [30–32].
Additional engagement and support from all relevant stakeholders, including funding agencies, researchers, program implementers, the community, multilateral organizations, and policymakers are needed to systematically answer the many critical questions that stand in the way of moving the integration efforts forward. Timely dissemination of the research results will promote quick uptake of the evidence to inform policies and programs. At all levels – national, international, and multilateral – partnerships need to be established to address the dual challenges of HIV and NCDs. Many of the innovative partnerships developed for the HIV epidemic provide opportunities to evaluate lessons learned that could be applicable to NCD care. Other partnerships may need to be re-envisioned for NCDs and new mechanisms may need to be established.
Conclusion
As efforts continue to address the threat of NCDs among PLHIV, much can be done to build upon the investments to date in strengthening the HIV platform. Implementation of integrated chronic care is critical to sustain the public health gains made through investments in HIV prevention and care. This holistic approach has potential benefits for both HIV and NCD prevention and treatment. However, many gaps in knowledge stand in the way of progress, and policymakers need a solid evidence base to inform their decision-making. The research agenda developed by this HIV/NCD project offers a pathway forward that can serve as a roadmap for funders, policymakers and researchers.
Acknowledgements
W.M.E-S. and L.K. provided initial conceptualization; S.V, P.P., and L.K. drafted the article; S.V, P.P., and B.B. provided the chart of research questions; P.P., N.A., W.M.T., and R.F. along with all other authors reviewed the article and approved the final version.
Thank you to Alicia Livinski, from the NIH Library, for conducting the literature review searches.
Special thanks to all who gave valued input to the HIV/ NCD project by participating in one or more products or meetings: James Alaro, Charles Ajayi, Ashley Antoine, Moses Bateganya, Kevin Brady, Pim Brouwers, Gene Bukhman, Hannah Cooper, Amisha Gandhi, Berhanu Molla Gedefaw, Roger Glass, Peter Godfrey-Faussett, Chris Gordon, Maureen Goodnow, Greg Greenwood, Joon Ha, Diane Havlir, Mark Hawkin, Degu Jerene, Jill Kanaley, Ben Kasdan, Peter Kilmarx, Elke Konings, Jeremiah Laktabai, Peter Lamptey, Fleetwood Loustalot, Carol Macera, Ellis McKenzie, Kathleen Michels, Collins Mitambo, Kibachio Jose Mwangi, Denis Nash, Funmi Olopade, Oyere Onuma, Nancy Padian, Gloria Sangiwa, Mona Saraiya, Virginia Senkomago, Arthur Sherman, George Siberry, Abraham Siika, Michael Smalky, Shelley Smith, Jason Sreedhar, Lindsay Templin, Marco Vitoria, David Watkins, Jessica Wilkinson, May Wong, and Emily Wroe.
Source of support: this article as part of the Research to Guide Practice: Enhancing HIV/AIDS Platform to Address Non-Communicable Diseases in sub-Saharan Africa was supported by the US National Institutes of Health Fogarty International Center.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US government.
Footnotes
HIV/NCD Project Members: Melanie Bacon, Joshua Berman, Rick Berzon, Pido Bongomin, Andrew Bremer, Delivette Castor, Pamela Collins, Rebecca Dirks, Geraldina Dominguez, Atalay Alem Ejigu, Michael Engelgau, Mychelle Farmer, John Flanigan, Eric Goosby, Rebecca Henry, Meghan Huchko, Michael Johnson, Kenneth Juma, Carol Langley, Naomi Levitt, George Mensah, Beatrice Matanje-Mwagomba, Helen McGuire, Paolo Miotti, Bernardo Nuche-Berenguer, Rachel Nugent, Paul Park, Sonak Pastakia, Emmanuel Peprah, Miriam Rabkin, Doreen Ramogola-Masire, Dianne Rausch, Michael Reid, Vikrant Sahasrabuddhe, Carolyn Williams, Makeda Williams, Deborah von Zinkernagel, Gerald Yonga.
Conflicts of interest
There are no conflicts of interest.
References
- 1.UNAIDS. Ending AIDS: progress towards the 90–90–90 targets. Geneva: UNAIDS;2017. [Google Scholar]
- 2.Deeks SG, Phillips AN. HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ 2009;338:a3172. [DOI] [PubMed] [Google Scholar]
- 3.Goulet JL, Fultz SL, Rimland D, Butt A, Gibert C, Rodriguez-Barradas M, et al. Aging and infectious diseases: do patterns of comorbidity vary by HIV status, age, and HIV severity? Clin Infect Dis 2007;45:1593–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smit M, Olney J, Ford NP, Vitoria M, Gregson S, Vassall A, et al. The growing burden of noncommunicable disease among persons living with HIV in Zimbabwe. AIDS 2018;32:773–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels MEDT, Bollyky TJ The emerging global health crisis: noncommunicable diseases in low- and middle-income countries. New York: Council on Foreign Relations; 2014. [Google Scholar]
- 6.Joint United Nations Programmeon HIV/AIDS (UNAIDS). Global report: UNAIDS report on the global AIDS epidemic 2013. In: Joint United Nations Programme on HIV/AIDS (UNAIDS);2013. [Google Scholar]
- 7.World Health Organization. Clinical guidance across the continuum of care: managing common coinfections and comorbidities. In. Edited by Organization WH;2013. [Google Scholar]
- 8.Suhrcke M, Boluarte TA, Niessen L. A systematic review of economic evaluations of interventions to tackle cardiovascular disease in low- and middle-income countries. BMC Public Health 2012;12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strand KB, Chisholm D, Fekadu A, Johansson KA. Scaling-up essential neuropsychiatric services in Ethiopia: a cost-effectiveness analysis. Health Policy Plan 2016;31:504–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sikander S, Lazarus A, Bangash O, Fuhr DC, Weobong B, Krishna RN, et al. The effectiveness and cost-effectiveness of the peer-delivered Thinking Healthy Programme for perinatal depression in Pakistan and India: the SHARE study protocol for randomised controlled trials. Trials 2015;16:534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scanlon PH, Aldington SJ, Leal J, Luengo-Fernandez R, Oke J, Sivaprasad S, et al. Development of a cost-effectiveness model for optimisation of the screening interval in diabetic retinopathy screening. Health Technol Assess 2015;19:1–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubinstein AL, Irazola VE, Poggio R, Gulayin P, Nejamis A, Beratarrechea A. Challenges and opportunities for implementation of interventions to prevent and control CVD in low-resource settings: a report from CESCAS in Argentina. Glob Heart 2015;10:21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaziano T, Abrahams-Gessel S, Surka S, Sy S, Pandya A, Denman CA, et al. Cardiovascular disease screening by community health workers can be cost-effective in low-resource countries. Health Aff 2015;34:1538–1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Durao S, Ajumobi O, Kredo T, Naude C, Levitt NS, Steyn K, et al. Evidence insufficient to confirm the value of population screening for diabetes and hypertension in low- and-middle- income settings. S Afr Med J 2015;105:98–102. [DOI] [PubMed] [Google Scholar]
- 15.Denny L, Prendiville W. Cancer of the cervix: early detection and cost-effective solutions. Int J Gynaecol Obstet 2015;131 (Suppl 1):S28–S32. [DOI] [PubMed] [Google Scholar]
- 16.Campos NG, Castle PE, Wright TC Jr, Kim JJ. Cervical cancer screening in low-resource settings: a cost-effectiveness framework for valuing tradeoffs between test performance and program coverage. Int J Cancer 2015;137:2208–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91–108. [DOI] [PubMed] [Google Scholar]
- 18.El-Sadr WM, Goosby E. Building on the HIV platform: tackling the challenge of noncommunicable diseases among persons living with HIV. AIDS 2018;32 (Suppl. 1):S1–S3. [DOI] [PubMed] [Google Scholar]
- 19.WHO. STEPwise approach to surveillance (STEPS). WHO; 2017. [Google Scholar]
- 20.Patel P, Rose CE, Collins PY, Nuche-Berenguer B, Sahasrabuddhe VV, Peprah E, et al. , for the NIH HIV/NCD Project Disease Condition Technical Operating Group. Noncommunicable diseases among HIV-infected persons in low-income and middle-income countries: a systematic review and metaanalysis. AIDS 2018;32 (Suppl. 1):S5–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishtar S The NCDs cooperative: a call to action. Lancet 2017; 390:1820–1821. [DOI] [PubMed] [Google Scholar]
- 22.Rabkin M, de Pinho H, Michaels-StrasserS, Naitore D, Rawat A, Topp SM. Strengthening the health workforce to support integration of HIV and noncommunicable disease services in sub-Saharan Africa. AIDS 2018;32 (Suppl. 1):S47–S54. [DOI] [PubMed] [Google Scholar]
- 23.Pastakia SD, Tran DN, Manji I, Wells C, Kinderknecht K, Ferris R. Building reliable supply chains for noncommunicable disease commodities: lessons learned from HIV and evidence needs. AIDS 2018;32 (Suppl. 1):S55–S61. [DOI] [PubMed] [Google Scholar]
- 24.Juma K, Reid M, Roy M, Vorkoper S, Temu TM, Levitt NS, et al. From HIV prevention to non-communicable disease health promotion efforts in sub-Saharan Africa: A Narrative Review. AIDS 2018;32 (Suppl. 1):S63–S73. [DOI] [PubMed] [Google Scholar]
- 25.Njuguna B, Vorkoper S, Patel P, Reid MJA, Vedanthan R, Pfaff C, et al. Models of integration of HIV and noncommunicable disease care in sub-Saharan Africa: lessons learned and evidence gaps. AIDS 2018;32 (Suppl. 1):S33–S42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nugent R, Barnabas RV, Golovaty I, Osetinsky B, Roberts DA, Bisson C, et al. Costs and cost-effectiveness of HIV/noncom- municable disease integration in Africa: from theory to practice. AIDS 2018;32 (Suppl. 1):S83–S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mwagomba BLM, Ameh S, Bongomin P, Juma PA, Kyobutungi C, MacKenzie RK, et al. Opportunities and challenges for evidence-informed HIV-noncommunicable disease integrated care policies and programs: lessons from Malawi, South Africa, Swaziland and Kenya. AIDS 2018;32 (Suppl. 1):S21–S32. [DOI] [PubMed] [Google Scholar]
- 28.Johnson M, Wilkinson J, Gardner A, Kupfer LE, Kimaiyo S, Von Zinkernagel D. Global partnerships to support noncommunicable disease care in low and middle-income countries: lessons from HIV/AIDS. AIDS 2018;32 (Suppl. 1):S75–S82. [DOI] [PubMed] [Google Scholar]
- 29.Kemp CG, Weiner BJ, Sherr KH, Kupfer LE, Cherutich PK, Wilson D, et al. Implementation science for integration of HIV and non-communicable disease services in sub-Saharan Africa: a systematic review. AIDS 2018;32 (Suppl. 1):S93–S105. [DOI] [PubMed] [Google Scholar]
- 30.National Cancer Institute. RFA-CA-15–007: planning for regional centers of research excellence in noncommunicable diseases in low and middle income countries (P20). Bethesda, MD: National Institutes of Health;2016. [Google Scholar]
- 31.Fogarty International Center. RFA-TW-16–002: international research training grants: fogarty global health training program (D43). Bethesda, MD: National Institutes of Health;2016. [Google Scholar]
- 32.National Heart Lung and Blood Institute. NOT-HL-17–520: notice of intent to publish a funding opportunity announcement for heart, lung, and blood co-morbidities implementation models in people living with HIV (HLB SIMPLe) (U01). Bethesda, MD: National Institutes of Health;2017. [Google Scholar]


