ABSTRACT
Many of the issues faced by undergraduate medical students and those planning their curriculum are not new. William Osler, Abraham Flexner and the General Medical Council have in turn made significant contributions to shaping today's UK undergraduate medical curriculum. It is anticipated that the reports from Robert Francis, Don Berwick and the Future Hospitals Commission about patient safety and quality of care will inform future planning. An increasing curriculum challenge is the achievement of an appropriate balance between biomedical and behavioural sciences in the context of progressive advances in basic and clinical science and increasing professional scrutiny. This requires agreement about the clinical knowledge and skills necessary at the time of registration, and true recognition of the continuum of learning from medical school to the time of retirement. The GMC's Tomorrow's Doctors defines outcomes from undergraduate medical training; this paper identifies 10 principles for curriculum planning to link theoretical educational concepts to practical clinical implementation. Such principles recognise the importance of reducing the burden of learning for an undergraduate student while reinforcing the relevance of generic clinical skills for competent and safe practice.
KEYWORDS: : Core curriculum, inter-professionalism, generalism, clinical apprenticeship, continuum of learning
Introduction
This review was begun with the hope that it would bring a fresh perspective to undergraduate medical education. It is intended as a personal perspective of the issues faced by undergraduate medical training in the UK. An evaluation of the history of undergraduate medical education in the UK over three centuries reveals many areas that remain incompletely addressed. In the sections that follow I reflect on the historical perspective, consider more recent issues and events relevant to undergraduate curriculum planning. I conclude by proposing ten principles that might be seen to underpin the early stages of medical education and training.
Historical perspective
In 1863 the General Medical Council (GMC) raised a concern about the tendency to an ‘overloading of the curriculum of education … followed by results injurious to the student’ and a wish was expressed to find a means ‘to give the student a larger amount of time for self-education’.1 A Council minute of 1869, foreseeing the dangers of an excessively burdensome curriculum stated: ‘Whoever will consider the great extent of sciences which lie at the foundation of Medicine and Surgery … will see that some limit must be assigned to the amount of knowledge which can be fitly exacted’.1 Thomas Huxley put it more forcibly in 1876: ‘The burden we place on the medical student is far too heavy, and it takes some doing to keep from breaking his intellectual back. A system of medical education that is actually calculated to obstruct the acquisition of sound knowledge and to heavily favour the crammer and the grinder is a disgrace’.2 Something that may sound familiar to today's students?
William Osler was an astute bedside clinician and a keen observer of clinical practice who dedicated his life to the training of young doctors.3 This is captured in his epitaph, ‘I taught medical students in the wards’. For Osler medicine was an ‘old art that … must be absorbed in the new science’. At the age of 25 years he took up a chair at McGill University in Montreal where he concentrated his teaching around the bedside and at post mortems. In 1889 he was recruited as foundation physician-in-chief and chair of medicine to Johns Hopkins University, Baltimore; at Johns Hopkins he championed a clerkship system that integrated the values of scientific medicine into clinical practice. Osler considered that disease was the student's chief teacher and teaching should be at the bedside rather than in the lecture theatre. Teaching away from the bedside was a ‘bastard substitute’.4
Abraham Flexner was not a doctor but became one of the most influential medical educationalists.5 Flexner, who was born in 1866, began his career as a school teacher. He quickly distinguished himself as a progressive educationalist and, after a psychology degree at Harvard, spent time in Germany studying education. Flexner was hired by Andrew Carnegie to advise his Foundation for the Advancement of Teaching on how standards of medical teaching in the USA and Canada could be improved. The publication of Flexner's report in 1910 attracted wide international attention.6 The key to high quality medical education in his view was science. Medical schools should be research-active university departments linked to teaching hospitals with full-time staff. The study of medicine should have stiff entrance requirements, recruiting graduates who would work towards a doctoral degree. After a ‘pre-clinical’ grounding in scientific disciplines, clinical education was to take place through participation in apprenticeship hospital attachments, supported by bedside teaching. The modern medical curriculum was born at the time when ‘the baffling and terrifying world of illness was becoming intelligible and comprehensible’ through biomedical research, particularly with regard to the major killer, infectious disease.5
In the UK medical education was developed largely on the basis of the apprenticeship system. When the need for a foundation in the basic sciences relevant to medicine became recognised, courses in anatomy, physiology, biochemistry and pharmacology were introduced as a preliminary to clinical studies. Thus was born the pre-clinical/clinical divide which was perpetuated through most of the twentieth century, with each part of the course proliferating without the moderating influence of the other, and without a coordinated examination of the overall aims of the course. Until the introduction of provisional registration in 1953, newly qualified doctors were legally entitled to undertake any form of medical practice without supervision, and without any requirement for further training.1
Concerns about patient safety led the Goodenough Committee in 1946 to advocate the introduction of what was to become known as the pre-registration year.7 The Committee argued that it was no longer appropriate to let newly qualified doctors enter independent practice without further training. Goodenough recommended (as an extension of undergraduate training) a period of service providing general experience under supervision prior to the acquisition of full GMC registration. The notion of a pre-registration year as part of the continuum of basic medical education was endorsed by the Royal Commission on Medical Education in 1965–68 – ‘the undergraduate medical course does not provide sufficient training for the immediate practice of medicine’.8
The Committee of Inquiry into the Regulation of the Medical Profession was highly critical of the organisational structure that had developed around the pre-registration year: ‘all too often the graduate is regarded as a much needed extra pair hands rather than a probationer doctor still requiring supervision and training in a significant point in his career’.9 The Merrison Report made a number of recommendations that relaxed the prescriptiveness of the requirements of the undergraduate course as assessed at the qualifying examination. It required the GMC Education Committee to ‘determine the extent of the knowledge and skill which is to be required from candidates at qualifying examinations’. The perception of what the newly qualified doctor should know and be capable of doing in the eyes of their teachers and those for whom they worked as pre-registration house officers did not alter significantly despite all of these changes. There remained a persisting drive towards an unrealistic degree of completeness in the curriculum reinforced by the reluctance of disciplines and specialties to surrender what they saw as their entitlement to teaching time and by an excessive enthusiasm of some teachers for their own subject.
Tomorrow's doctors
In 1993 the GMC published a ‘blueprint’ for undergraduate medical training.1 Tomorrow's Doctors represented a step change in medical training by taking the start of the pre-registration year as the reference point to which the ‘professional’ component of the undergraduate course is directed. In 1993 the curriculum was framed in terms of objectives; since 2003, these objectives have been defined as educational outcomes.10 The curriculum was no longer intended to be all-embracing but to contain a core which was more rigorously defined than previously. This ‘core curriculum’ detailed the requirements that must be satisfied before a newly qualified doctor can assume the responsibilities of a pre-registration house officer. The GMC foresaw the greater educational opportunity afforded by what they termed ‘special study modules’ (SSMs) that encouraged students to study in depth areas of particular interest to them. Well-designed SSMs provide insights into scientific method and the discipline of research, and engender an approach to medicine that is constantly questioning and self-critical.
Tomorrow's Doctors requires subject disciplines to integrate their contributions into a thematic, largely systems-based course with students having ‘real life’ experiences in the earliest parts of the curriculum while continuing to learn foundation disciplines in the later years. The foundation disciplines included behavioural and social sciences and humanities, as well as biomedical science. There is much greater emphasis on people and populations, on communication (including listening) skills, and on medical ethics and relevant law. The curriculum was intended to familiarise students with ever-changing health care systems, multi-professionalism and healthcare in the community. Perhaps the most striking of all the GMC recommendations was the vertical and horizontal integration of what were formerly called pre-clinical subjects and clinical disciplines – a reversal of Flexner principles.
Francis and Berwick Reports
The exposure of poor care and higher mortality rates at a hospital trust in England, Mid Staffordshire NHS Foundation Trust, has recently highlighted for all health professionals the critical importance of a focus on patient care and safety at the earliest stages of undergraduate curricula. A recommendation of Robert Francis's public inquiry into the Mid-Staffordshire Foundation Trust drew strong attention to the importance of education and training and the immediate need to integrate essential shared values of quality of patient care in the culture of the NHS.11 Don Berwick's review of patient safety in the NHS in England recommends that a ‘mastery of patient safety sciences and practices’ should be part of the initial preparation and lifelong education of all health care professionals.12 He proposed that these recommendations be embedded in all future training programmes.
Challenges to UK medical undergraduate education
Medical schools in the UK have a dual role: to extend biomedical and scientific understanding, and to create curricula that prepare future doctors to practise within the NHS. The more recent history of medical education is a reminder that a generic medical curriculum does not inevitably result from a perfect understanding of how to train future doctors but rather from social, political and scientific influences over the time it was created. Richard Horton puts it succinctly as ‘a backward looking appeal that fails to deal seriously with contemporary issues and to provide a foundation for re-interpreting medicine in a new era of science’.13 Tomorrow's Doctors correctly identifies the shift in balance between hospital-based services and those provided in general practice and the community, the significance of an ageing, multi-racial population, the growth in the public's understanding of disease and disability, the importance of a doctor's ability to communicate effectively, and unforeseen moral and ethical issues arising from scientific advances. However, it has yet to fully recognise the challenge to curriculum development from progressive advances in genomic and cell biology or to find an appropriate balance between the basic and behavioural sciences during the time when ‘personalised medicine’ is gaining momentum.
Future medical training
The objective of the recent Shape of Training Review of postgraduate medicine (SOT)14 was to ‘make sure that over the next 30 years, the UK continues to train doctors who are fit to practise, are able to meet patient and service needs, and provide safe and high quality care’ – an ambitious agenda given the large number of reports and changes to the structure of postgraduate medical training that pre-date SOT.15–17 Two of the key messages from SOT that resonate with undergraduate training will require detailed consideration as part of undergraduate curriculum planning:
> ‘Patients and the public need more doctors who are capable of providing general care in broad specialties across a range of different settings. This is being driven by a growing number of people with multiple co-morbidities, an ageing population, health inequalities and increasing patient expectations.’
> ‘Full registration should move to the point of graduation from medical school, provided there are measures in place to demonstrate graduates are fit to practise at the end of medical school. Patients’ interests must be considered first and foremost as part of this change.’
The latter recommendation diverges from previous recommendations from Goodenough, Merrison and Todd, who supported pre-registration a year post-graduation.
Future Hospital Commission
In 2012, the Royal College of Physicians appointed a Future Hospital Commission (FHC) to address how hospital services needed to change in the future to address patient needs. The FHC's report Future hospital: caring for medical patients18 highlights the importance of the re-introduction of generalism into medical training: ‘Medical education and training will develop doctors with the knowledge and skills to manage the current and future demographic of patients. This includes the expertise to manage older patients with frailty and dementia, and lead and coordinate the ‘whole care’ of patients in hospital and into the community’. The report comments about future undergraduate medical training:
The curriculum of undergraduate training (at medical school) must emphasise the importance of acute and (general) internal medicine. Community placements for medical students and trainees will be required. Such a broad-based training programme might include acute and/or (general) internal medicine, community care, psychiatry and general practice. Consideration should be given to when community care rotations, supervised by specialists, are most useful for trainees and patients. This may be later in training. Most training for any doctor should occur in the setting in which they will eventually be primarily working. This may mean partly community and secondary care environments for physicians, rather than tertiary care centres. At the undergraduate level, extended clinical placements under the umbrella of generalism, possibly in the third year of 5 years and second year of graduate entry programmes, which includes both hospital and community practice (including primary care), would be highly desirable.
The significance of the FHC's recommendations to undergraduate curriculum planning is twofold: the importance of the ‘join up’ with postgraduate training, and the implications of continuing change to health service delivery that must inform clinical placements and career choices of future doctors. Although FHC focuses on the hospital setting, it emphasises the crucial importance of out-of-hospital care and the pivotal role of multi-professional teamwork and social care.
An issue not considered by the Future Hospitals Commission is the increasing provision of NHS health care by the independent sector, and the consequences this may have for the delivery of education and training. Private providers presently are not required to contribute to the training agenda and most are reluctant to consider this because of service implications. This is already beginning to impact on postgraduate training; for health professions other than medicine it has already impacted on undergraduate training.
What type of training do doctors need?
The dilemmas and issues of modern health care must be central to the education and training of doctors and other health care professionals. Revisions to Tomorrow's Doctors in 2015 will need to anticipate future health service requirements rather than reflect the past. Undoubtedly Francis, Berwick, Shape of Training and the FHC will influence these considerations. David Weatherall provides a practical starting point: ‘Good doctoring requires an ability to cut through many of the unexplained manifestations of disease, to appreciate what is important and what can be disregarded and when to get to the core of the problem knowing when scientific explanations have failed and simple kindness and empiricism must takeover’.19
The Educating Future Physicians for Ontario (EFPO) project identified seven roles of a doctor that were later defined by CanMEDS as essential competencies: medical expert; communicator; collaborator; manager; health advocate; scholar; and professional.20
Such competencies need to be identified as outcomes in curriculum planning; they will require a scheme of continuous assessment across a spectrum of life-long learning centred on student/doctor. The undergraduate programme is only the preliminary step in this continuum of medical education that lays down the foundation for future professional life; its coordination with later stages of training is essential. What is disappointing, despite all good intentions, is a fragmented rather than seamless approach to learning from the start at medical school through to retirement – an explicit continuum of learning and training does not exist.
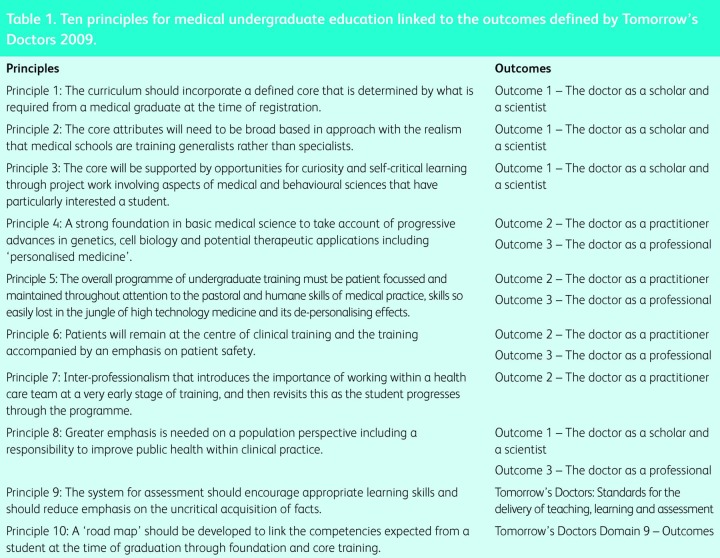
It is timely, in this context, to present a number of principles as UK undergraduate medical curricula are reviewed and revised. Such principles, which represent a personal perspective, are not new but they do require restating. Table 1 cross links these 10 principles to the outcomes defined by the GMC in Tomorrow's Doctors.10
Table 1.
Ten principles for medical undergraduate education linked to the outcomes defined by Tomorrow's Doctors 2009.
Principle 1
The curriculum should incorporate a defined core that is determined by what is required from a medical graduate at the time of registration. This will be all the more important if registration occurs at the time of graduation.
Principle 2
The core attributes will need to be broad-based in approach, given the realism that medical schools are training generalists rather than specialists. The challenge will lie firstly in achieving an agreement about what is core and secondly in delivering a generalist viewpoint. The increasing dearth of generalists has resulted in medical sciences increasingly being presented according to a specialist-based compartmentalised approach that is at odds with modern-day integrative biology.
An important element of medical training is to equip future doctors with sufficient knowledge of the complexity and evidence base of day-to-day clinical issues to enable them to counsel and guide their patients through ‘a morass of uncertainty’. Those who teach must be informed by the latest research findings.
The core curriculum will permit standardisation of course content across medical schools and reflect an appropriate balance between basic medical and the behavioural sciences.
Principle 3
The core will be supported by opportunities for curiosity and self-critical learning through project work involving aspects of medical and behavioural sciences that have particularly interested a student. Such special study modules/components will build on the considerable experience developed in medical schools since the publication of Tomorrow's Doctors in 1993.
Principle 4
The undergraduate medical programme must continue to be informed by research. A strong foundation in basic medical science will take account of progressive advances in genetics, cell biology and potential therapeutic applications including ‘personalised medicine’. It is likely that advances in these areas will revolutionise medical practice within the careers of the students. Nevertheless, the reality is that it will take several years to unravel complex issues of transcriptional and translational gene modifications, the influences of regulatory and modifying genes and the important interactions of the genome with the environment.
The challenge for an evolving curriculum will be to accommodate an expanding science base pertinent to medical undergraduate training and balancie this with a level of appropriate behavioural sciences while avoiding curriculum overload. In the past curriculum planning has been blighted by a desire to include rather than to exclude; good planning requires tight and continuous policing. This will mean sacrifices of the more traditional elements of medical education that include conventions about anatomical and biochemical knowledge. Modern-day technology enables the visualisation of body tissues and viscera that are invisible within even the best preserved cadaver; students will need to be able to interpret such medical images at an early stage in training.
Principle 5
The overall programme of undergraduate training must be patient-focussed and attention must be given throughout to the pastoral and humane skills of medical practice, skills so easily lost in the jungle of high technology medicine and its de-personalising effects. Communication and listening skills are essential requirements of good doctoring, combined with a practical knowledge of medical ethics and law. These underpin the importance of professionalism – I quote from Louis Lasagna's modernised version of the Hippocratic Oath: ‘If I do not violate this oath, may I enjoy life and art, respected while I live and remembered with affection thereafter. May I always act so as to preserve the finest traditions of my calling and may I long experience the joy of supporting those who seek my help’.21
The GMC has published useful guidance for medical students and medical schools about professional values and fitness to practice. The guidance sets out professional standards that are required of students, as well as doctors, in aspects of competence, care and general behaviour.22
Principle 6
Patients will remain at the centre of clinical training, with an emphasis on patient safety. Medicine is best learned within the clinical setting, whether it be by the bedside, in a general practice surgery or during a community placement. Technology should support rather than be a substitute to the patient consultation. There should be greater emphasis on the skills of history taking, clinical examination and the appropriate selection of diagnostic tools. Simulation of a clinical setting has a role but it should not detract from real patient encounters.
All of this will require better integration across health boundaries from community into hospital and the reverse. It may better be facilitated through one organisation having responsibility for the delivery of care both in the community and in hospital; this is underlined by the recent change to local funding to encourage closer working between health and social care services (the Better Care Fund).23
The apprenticeship model should once again be applied to clinical training to highlight the importance of students learning through observation and participation in clinical practice. This requires students to be involved in service as much as regulation permits; it recognises the importance of learning from experience and the importance of the role model provided by the clinical practitioner. Successful clinical placements demonstrate quality leadership and a supportive learning environment. For the future, clinical placements should be offered by all providers of NHS care irrespective of whether they are publically or privately funded.
Several medical schools in the USA and Australia have introduced longitudinal integrated clerkships. For one year, students work continuously with doctors in core specialties (internal medicine, neurology, obstetrics and gynaecology, paediatrics, surgery, radiology and psychiatry) while simultaneously following a panel of patients representing a wide spectrum of medical conditions. Students reported that they felt better prepared for practice, including professional aspects of involving patients in decision making and understanding the impact of social context on patients.24
Principle 7
Inter-professionalism and the importance of working within a healthcare team should be introduced at a very early stage of training and then be revisited this as the student progresses through the programme. Working in healthcare teams will additionally require a student to understand clinical leadership and the potential roles of a doctor. Inter-professionalism should not play ‘lip service’ to the multi-professional nature of health care but simulate clinical settings that newly qualified graduates will encounter. The introduction of inter-professionalism recognises the real difficulties of timetabling for all of the professional groups. There are opportunities towards the end of the medical programme where it is feasible to bring nurses, physiotherapists, pharmacists and other professionals of comparable experience together to work through clinical scenarios. It will need all professions to plan together – in this regard, no one discipline can be considered exceptional.
Principle 8
Greater emphasis should be given to the population perspective, including an appreciation of the responsibility of doctors to improve public health within clinical practice and an understanding of the fundamentals of health economics. This should include an understanding of the evidence base, with an objective of promoting not simply a ‘cure’ but a ‘curb’ of ill health. Students need to better understand how health services work and how they are funded in the UK and more globally.25 The increasing challenges to health in their professional lives will come from the ageing population, climate change, food security and infection. These should all be encompassed within global health. Special study modules and/or elective periods should provide opportunities for students to extend such interest.
Principle 9
The system for assessment should encourage appropriate learning skills and reduce emphasis on the uncritical acquisition of facts. The scheme should be one of progressive assessment that monitors the acquisition and utilisation of core knowledge, the professional nature of clinical practice and the achievement of competence in skills at appropriate time within the course. The assessment process should be less onerous than at present and more applicable to the stage of training. Every assessment should be accompanied by constructive feedback to enable students to gauge their progress. Looking forward, a national qualifying examination seems increasingly likely and medical schools should learn from the experiences (both good and bad) from North America and postgraduate Royal Medical Colleges’ examinations.
Principle 10
Finally, and importantly, a ‘road map’ should be developed to link the competencies expected from a student at the time of graduation through foundation and core training. In the United States the Accreditation Council for Graduate Medical Education (AGCME) has identified milestones for the AGCME competences that describe levels for achievement by specialty residents.26 The proposed ‘map’ will be informed by the US experience; however, its objective is primarily to present generic skills that represent the continuum of education and training to student/trainee, and to trainers. It will underline the competences expected at the time of graduation, how these are consolidated through foundation and then developed further within core training. Such a ‘map’ will additionally identify how basic and more advanced skills continue to be revisited in training and provide greater clarity about the nature and timings of assessment. It will also provide an opportunity to review aspects of inter-professional experiences and enable more structure to team learning later in training.
Conclusions
There has been considerable progress in the development of medical undergraduate education and training during the last three decades. This has been accompanied by an acknowledgement of the importance of better integration between biomedical and behavioural sciences from the outset of training. Nevertheless, the challenge is to achieve an agreed appropriate balance. This is particularly challenging given the rapid advances in scientific knowledge and the need for healthcare provision to be financially affordable. The role of the doctor working as a professional within a healthcare team remains central to the highest quality of care and safe practice provided to every patient.
Theoretical educational concepts of learning have sometimes disappointed because they are impractical to deliver in the clinical environment. The critical challenge for future curriculum planning in a world increasingly driven by sophisticated technology and patient expectation is to maintain patients at the centre of everything that is taught and learned. This will require continuous updating and ‘policing’ of the core knowledge that defines the agreed skills expected from a doctor at the time of registration. Such an agreement will realise the continuum of learning from undergraduate training through to the day of retirement.
Future plans for the medical undergraduate curriculum should be informed by history through learning from the past; the priority for the future will be to ensure that curriculum content is adaptable to changing needs, not over burdensome to students and can realistically be delivered in a general clinical setting to the benefit of patients, students and clinicians.
References
- 1.General Medical Council Tomorrow's Doctors – recommendations on undergraduate medical education. London: GMC, 1993. Available online at www.gmc-uk.org/Tomorrows_Doctors_1993.pdf_25397206.pdf. [Accessed 20 March 2014.] [Google Scholar]
- 2.Huxley TH. Lecture delivered at the opening of Johns Hopkins University, Baltimore, 1876. [Google Scholar]
- 3.Bliss M. William Osler: A life in medicine. New York: Oxford University Press, 1999. [Google Scholar]
- 4.Cushing H. Life of Sir William Osler. Vol 1. New York: Oxford University Press, 1956. [Google Scholar]
- 5.Bonner TM. Iconoclast: Abraham Flexner and a life in learning. Baltimore: Johns Hopkins University Press, 2002. [Google Scholar]
- 6.Flexner A. Medical Education in the United States and Canada. A report to the Carnegie Foundation for the Advancement of Teaching. Boston: Updike, 1910. [Google Scholar]
- 7.Goodenough W., Chair Report of the Inter-departmental Committee on Medical Schools. London: HMSO, 1944. [Google Scholar]
- 8. Report of the Royal Commission on Medical Education, 1965–68. London: HMSO, 1968. [Google Scholar]
- 9. Inquiry into the Regulation of the Medical Profession. London: HMSO, 1975. [Google Scholar]
- 10.General Medical Council Tomorrow's Doctors 2009. London: GMC, 2009. Available online at www.gmc-uk.org/education/undergraduate/tomorrows_doctors_2009.asp. [Accessed 20 March 2014.] [Google Scholar]
- 11.Francis R., Chair Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Available online at www.midstaffspublicinquiry.com/news/2013/02/publication-inquiry-final-report. [Accessed 20 March 2014.] [Google Scholar]
- 12. Berwick Review into patient safety. London: Department of Health, 2013. Available online at www.gov.uk/government/publications/berwick-review-into-patient-safety. [Accessed 20 March 2014.] [Google Scholar]
- 13.Horton R. Second Opinion: Doctors, diseases and decisions in modern medicine. London: Granta Books, 2003. [Google Scholar]
- 14.Greenaway D., Chair Securing the future of excellent patient care: Final report of the independent review. London: GMC, 2013. Available online at www.shapeoftraining.co.uk/reviewsofar/1788.asp. [Accessed 20 March 2014.] [Google Scholar]
- 15.Department of Health Hospital doctors: training for the future. The report of the working group on specialist medical training. London: DoH, 1993. [Google Scholar]
- 16.Department of Health Modernising medical careers; the response of the four UK health ministers to the consultation on unfinished business: proposals for reform of the senior house officer grade. London: DoH, 2003. [Google Scholar]
- 17.Tooke J., Chair Aspiring to Excellence. Findings and final recommendations of the independent inquiry into Modernising Medical Careers. London: MMC Inquiry, 2008. Available online at www.mmcinquiry.org.uk. [Accessed 20 March 2014.] [Google Scholar]
- 18.Future Hospital Commission Future hospital: caring for medical patients. A report from the Future Hospital Commission to the Royal College of Physicians. London: Royal College of Physicians, 2013. www.rcplondon.ac.uk/sites/default/files/future-hospital-commission-report.pdf [Google Scholar]
- 19.Weatherall D. Science and Medical education: is it time to revisit Flexner? Med Educ 2011;45:44–50. 10.1111/j.1365-2923.2010.03761.x [DOI] [PubMed] [Google Scholar]
- 20.Frank JR. (ed). The CanMEDs 2005 Physician Competency Framework Better standards. Better Physician. Better Care. Ottawa, ON: Royal College of Physicians & Surgeons of Canada, 2005. [Google Scholar]
- 21.Lasagna L. Would Hippocrates rewrite his oath? New York Times Magazine 1964;11:40–3. [Google Scholar]
- 22.General Medical Council Medical students: professional values and fitness to practise. London: GMC, 2009. Available online at www.gmc-uk.org/education/undergraduate/professional_behaviour.asp. [Accessed 20 March 2014.] [Google Scholar]
- 23.Better Care Fund Planning www.england.nhs.uk/ourwork/part-rel/transformation-fund/bcf-plan/ [Accessed 20 March 2014.] [Google Scholar]
- 24.Walters L, Greenhill J, Richards J, et al. Outcomes of longitudinal integrated clinical placements for students, clinicians and society. Med Educ 2012;46:1028–41. 10.1111/j.1365-2923.2012.04331.x [DOI] [PubMed] [Google Scholar]
- 25.Wanless D. Securing our future health: taking a long term view. Final Report. London: HM Treasury, 2002. Available online at www.hm-treasury.gov.uk/wanless. [Accessed 20 March 2014.] [Google Scholar]
- 26.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system – rational and benefits. N Engl J Med 2012;367:1051–55. 10.1056/NEJMsr1200117 [DOI] [PubMed] [Google Scholar]