Background
Acute leukemia is the most common childhood cancer worldwide. Over the last few decades, survival rates have improved dramatically, with current 5-year overall survival rates for acute lymphoblastic leukemia (ALL) in high-income countries estimated at >90%.1 This improvement in survival is mainly the result of using risk-adapted therapy and providing better supportive care.
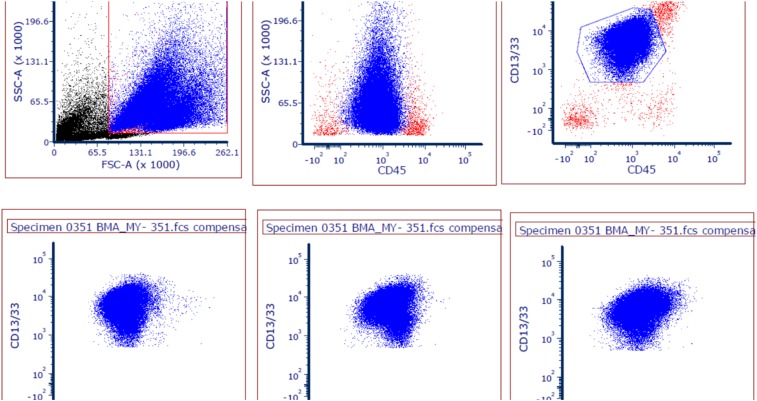
Figure 1.
APML flow cytometry plot from the Uganda cohort.
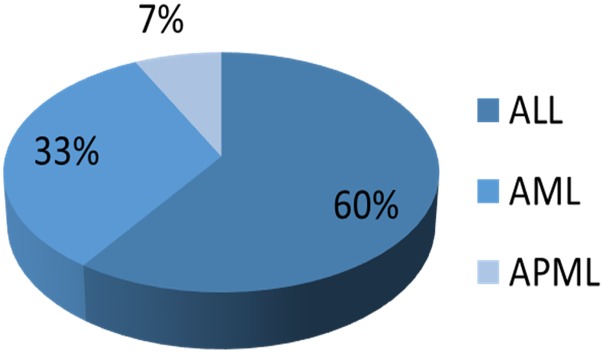
Figure 2.
Percentages of ALL, acute myeloid leukemia (AML), and acute promyelocytic leukemia (APML) diagnosed by flow cytometry in the Uganda cohort.
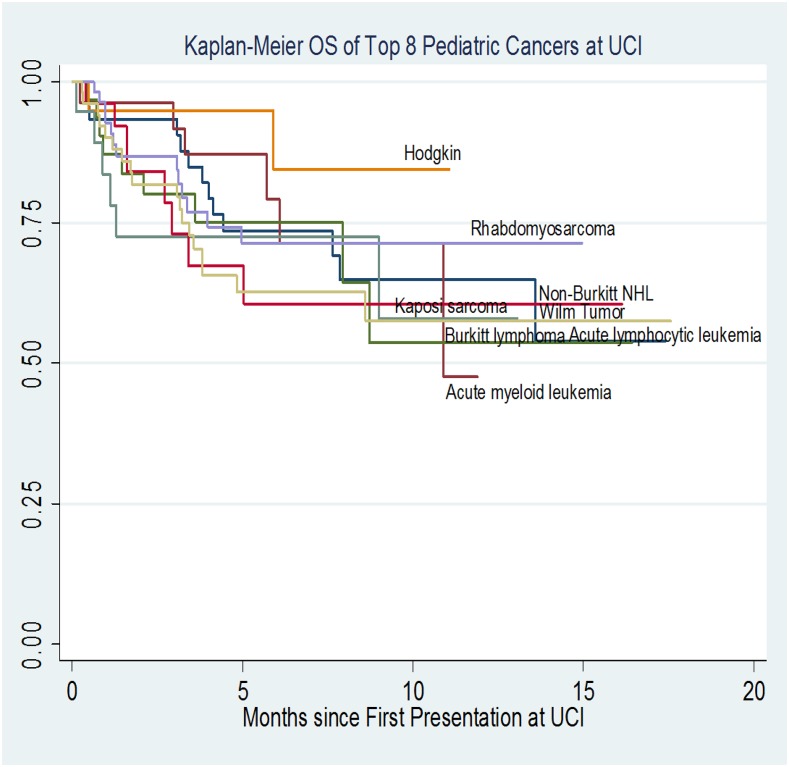
Figure 3.
Survival rates for the most common pediatric cancers at the UCI. Accurate diagnosis is essential for choosing and using optimal therapy and for understanding disease-specific risks.
Table 1.
ALL subtypes and MRD outcomes at 1 month
| No. | % | |
|---|---|---|
| ALL subtype | ||
| Pre-B | 49 | 80.3 |
| T-cell | 12 | 19.7 |
| MRD at the end of induction | ||
| MRD negative, <0.01% | 30 | 35.3 |
| MRD positive, >0.01 | 16 | 18.8 |
| MRD not performed | 39 | 45.9 |
In contrast, in low-income countries, outcomes of acute leukemia remain poor because of lack of or inaccurate diagnosis, treatment-related mortality, treatment abandonment, and suboptimal treatment protocols.2,3 Optimal outcomes require the ability to obtain rapid and accurate diagnosis and having biological data available so that modern risk-adapted protocols can be chosen. Historically, in Uganda, pediatric leukemia diagnoses were based on slides stained with hematoxylin and eosin, and the diagnosis was dependent on the availability of a hematopathologist.
Objective
Here we present the steps taken to improve the diagnostic process, promote the use of risk-adapted therapy, and collaborate on outcomes for children with acute leukemia in Uganda.
Initiatives to improve leukemia diagnosis and treatment.
Establishment of a pediatric hematology-oncology fellowship program, which is a collaboration between Uganda Cancer Institute (UCI), Makerere University, Mulago Hospital, the Global Hematology Oncology Pediatric program (founded by Texas Children’s Cancer and Hematology Centers), and Baylor College of Medicine.
Recruitment of hematologists and oncologists trained in the United States and the United Kingdom to work on site.
Establishment of a multiparametric flow cytometry laboratory to provide immunophenotypes for suspected leukemia diagnoses and evaluate patients for minimal residual disease (MRD).
Implementation of risk-adapted treatment protocols for acute leukemia.
Training of laboratory scientists to carry out analyses.
Discussion of flow cytometry and morphology results in multidisciplinary tumor boards.
Outcomes
Since June 2017, we have analyzed 307 bone marrow samples and blood specimens from 143 patients by using flow cytometry to establish diagnosis and measure MRD. An example of a flow plot is shown in Figure 1.
One hundred nineteen cases of acute leukemia were diagnosed by immunophenotyping, with an unexpectedly high percentage of patients with acute promyelocytic leukemia. The findings are summarized in Figure 2 and Table 1.
Using subtype-specific risk-adapted therapy to treat children with ALL improved 1-year overall survival from 30% to 70%. A Kaplan-Meier curve is shown in Figure 3.
Conclusions
International collaborations have had a significant impact on leukemia outcomes at the UCI.
Local capacity was developed to conduct flow cytometry.
Relationships with leading experts from various Western institutions were established.
Our efforts led to improved and accurate leukemia diagnosis.
Accurate diagnosis, disease-appropriate therapy, and risk-adapted treatment protocols are essential for improving survival rates.
Way forward
Initiatives are underway to continue to improve outcomes
Incorporate cytogenetic characteristics into risk stratification.
Study unique biological characteristics and behavior of acute leukemia in children in sub-Saharan Africa.
Treatment protocols and supportive care have not yet been standardized, but need to be standardized as a way forward across Global HOPE sites (Uganda, Malawi, and Botswana).
Acknowledgments
This work was supported by St. Baldrick’s Foundation (for the flow cytometry service) and Grant No. PA-16-086 from the National Institutes of Health, National Cancer Institute.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ruth Namazzi, College of Health Sciences, Makerere University, Kampala, Uganda; e-mail: namazzi101@gmail.com or ruth.namazzi@bcm.edu.
References
- 1.Ries LAG, Eisner MP, Kosary CL, et al. (eds). SEER Cancer Statistics Review, 1973-1999. National Cancer Institute. Bethesda, MD, 2002 http://seer.cancer.gov/csr/1973_1999/ [Google Scholar]
- 2.Nandakumar A, Anantha N, Venugopal T, et al. . Descriptive epidemiology of lymphoid and haemopoietic malignancies in Bangalore, India. Int J Cancer. 1995;63(1):37-42. [DOI] [PubMed] [Google Scholar]
- 3.Howard SC, Pedrosa M, Lins M, et al. . Establishment of a pediatric oncology program and outcomes of childhood acute lymphoblastic leukemia in a resource-poor area. JAMA. 2004;291(20):2471-2475. [DOI] [PubMed] [Google Scholar]