1. Introduction
The beneficial medical properties of cannabis in treatment of variety of diseases have been widely recognized across many cultures (Zuardi, 2006, Aggarwal et al., 2009, Birdsall et al., 2016). At the end of the 19th century in Europe, cannabis was considered effective for the treatment of chronic pain, asthma, sleep disorders, depression, and loss of appetite (Guy et al., 2004, Manzanares et al., 2006, Sabo et al., 2013). Medical use of cannabis continued until the first half of the 20th century, when legal restrictions were introduced due to the psychoactive constituent - delta-9-tetrahydrocannabinol (THC), which is one of at least 113 cannabinoids identified in cannabis (Ben Amar, 2006, Horvat et al., 2007).
In Serbia, cannabis is classified under narcotic drugs, and the production, sale and possession of cannabis for recreational use or any form of medical marijuana products is illegal (Law on Psychoactive Controlled Substances). Recently, a number of countries in Europe have introduced specific laws and programs to allow patients to use cannabis preparations to effectively relieve the symptoms of chronic pain, muscle cramps and spasticity in patients with multiple sclerosis, to alleviate nausea and vomiting and to improve weight gain and appetite in patients with AIDS (European Monitoring Centre for Drugs and Drug Addiction, 2017). Besides Netherlands, a country with more than 10 years of experience in medical cannabis use, medical cannabis has also been legalized in Italy, Spain, France, Romania and Czech Republic. As for the countries surrounding Serbia, Croatia and Macedonia are the most recent countries which have allowed the use of cannabis in medical purposes (Bifulco and Pisanti, 2015).
As more countries in Europe and worldwide continue to change laws for medical marijuana use, public interest in medical cannabis legalization in Serbia is growing. When medical cannabis is legalized in Serbia, doctors will be the ones who will prescribe the products and answer to patients’ questions about its use, benefits and side effects. It is of immense importance to bear in mind specific harmful effects of cannabis, especially in young people. Cannabis is indicated as a possible risk factor for cardiovascular disease in young adults due to increased reporting of cardiovascular complications related to cannabis and their extreme seriousness (Jouanjus et al., 2014). Furthermore, exposure to cannabis during adolescence has been connected to deviations in the normal neurodevelopment, producing a brain particularly at risk of psychiatric disorders such as schizophrenia (Iannitelli et al., 2017, Quartini et al., 2017).
Yet, prospective doctors may receive minimal education on this issue throughout the curriculum. A paucity of studies exist evaluating future health care professionals’ knowledge and attitude towards medical cannabis (Sabo et al., 2013, Ben Amar, 2006). In Serbia, one study evaluated beliefs about medical cannabis among fourth-year medical students, while another included only the final year students of pharmacy (Vujcic et al., 2017, Stojanović et al., 2017).
The aim of this study was to determine the frequency of recreational cannabis use among medical students and to explore their knowledge about therapeutic use/abuse, side effects and current legislation status of medical cannabis, as well as attitudes toward its legalization.
2. Material and methods
The survey was conducted on sample of students of the third, fifth and sixth year of integrated academic studies of medicine at the Faculty of Medicine in Novi Sad, Serbia, between November 1st, 2017 and December 15th, 2017. The research was approved by the Ethical Committee of the Faculty of Medicine in Novi Sad (approval number 01-39/240/1).
The sample size, which was the total number of registered medical students of selected years, was 350. All students were eligible to participate in the study. Self-administered anonymous questionnaires were distributed to students of each year during lectures. We chose the lectures where attendance was compulsory in order to achieve high percentage of target population. Only those students who were not present on the day of the survey were excluded. Before each questionnaire was filled in, they received information about the survey and then signed the informed consent.
The questionnaire was created by a combination of questions from the surveys performed by (Moeller and Woods, 2015; Vujcic et al., 2017), with the modifications necessary to ensure correct answers to questions and claims and to be more suitable for prospective doctors who will be able to prescribe, recommend, and treat patients with cannabis-based preparations.
The first part of the questionnaire referred to socio-demographic characteristics of the students such as year of study, gender, place of residence, and data about previous recreational cannabis use. The second part consisted of 13 questions. The first four questions were close-ended and related to the perceived awareness of the students about the possible therapeutic effect of cannabis, as well as its side effects. To be specific, students who stated to be familiar with the possible therapeutic and/or side effects were offered additional two multiple response questions composed of the list of specific indications for which cannabis has been approved and the list of side effects. These questions were followed by three close-ended questions about opinion of the students on the abuse potential of the therapeutic use of cannabis. These questions referred to its potential to cause addiction, open the abuse area, or to be the gateway to hard drugs. The last four questions examined students' knowledge about the current state of legalization of cannabis for therapeutic use in Serbia and other countries, whether they consider that the therapeutic use of cannabis requires the development of defined guidelines, as well as their attitude toward the legalization of cannabis for therapeutic use in Serbia. In addition, students answered if the issuing of the preparations based on cannabis in the pharmacy should require a prescription or not. The last multiple response question identified the main source of the information about cannabis use (the answers offered were media, family, regular curriculum or students’ workshops and conferences).
After data collection, data entry and processing was done in the IBM SPSS version 22. New variables “number of recognized indications” and “number of recognized side effects” were created by counting the number of indications/side effect each student has marked in given list. The differences between male and female students, students who previously used cannabis and those who never used cannabis, as well as differences between students of different years of study were compared. Chi square test was used to compare nominal variables, while t-test for independent samples and Anova with Tuckey post-hoc test were used for numerical variables. Man-Whitney and Kruskal-Wallis were used for numeric data with non-parametric distribution. All p value less than 0.05 were considered significant.
3. Results
Out of 350 questionnaire distributed, the survey was completed by 316 students (response rate 90.3%). Nearly two-thirds (67.7%) of students were female, while approximately a third (33.2%) of students reported using marijuana at least once in their lifetime. Cannabis was significantly more commonly used by male students (p = 0.007), while there was no significant difference in the recreational use of cannabis between students of different years of study (p = 0.830) (Table 1).
Table 1.
Demographic characteristics and previous cannabis use among investigated students.
| Characteristics | All students N (%) |
Marijuana status |
|||
|---|---|---|---|---|---|
| yes N (%) |
no N (%) |
p | |||
| Gender | female | 214 (67.7) | 60 (28) | 154 (72) | 0.007 |
| male | 102 (22.3) | 45 (44.1) | 57 (55.9) | ||
| Year of the study | third | 130 (41.1) | 45 (42.9) | 85 (40.3) | 0.830 |
| fifth | 91 (28.8) | 28 (26.7) | 63 (29.9) | ||
| sixth | 96 (30.3) | 32 (30.5) | 63 (29.9) | ||
| Total | 316 (100) | 105 (33.2) | 211 (66.7) | ||
Table 2 shows the students perceived awareness of the therapeutic and side effects of cannabis, current legislation, as well as their attitudes toward cannabis abuse and legalization. Majority of students stated that they are familiar with the fact that there are approved indications for cannabis (258, 81.6%), while little more than two thirds of the students considered themselves familiar with side effects of cannabis use (205, 64.9%). Students who reported previous cannabis use were more familiar with its therapeutic and side effects (p ≤ 0.001). Also, students who have never used cannabis were more familiar with possible cannabis abuse, such as that use of cannabis for therapeutic purposes can cause addiction (p ≤ 0.001), open the abuse area (p = 0.031) and can be the gateway to hard drugs (p = 0.001). In addition, students who previously used cannabis were more familiar with the current legalization process in Serbia (p = 0.006) and significantly larger number of students who previously used cannabis were of the opinion that the use of cannabis for therapeutic purposes should be legalized in Serbia (p = 0.006). The year of study did not affect the students' awareness of the therapeutic and side effects of cannabis, as well as their attitudes toward abuse and legalisation of medical cannabis (Table 2).
Table 2.
Students awareness of the therapeutic and side effects of cannabis and their attitudes toward cannabis abuse and legalisation
| Questions and statements | Recreational marijuana use |
Year of the study |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| yes N (%) |
no N (%) |
p | third N (%) |
fifth N (%) |
sixth N (%) |
p | |||
| Knowledge | I am familiar with the possible therapeutic effect of cannabis | yes | 99 (94.3) | 159 (75.4) | <0.001 | 99 (76.2) | 81 (89.0) | 78 (82.1) | 0.052 |
| no | 6 (5.7) | 52 (24.6) | 31 (23.8) | 10 (11.0) | 17 (17.9) | ||||
| I am familiar with the side effects of cannabis | yes | 87 (82.9) | 118 (55.9) | <0.001 | 83 (63.8) | 67 (73.6) | 55 (57.9) | 0.079 | |
| no | 18 (17.1) | 93 (44.1) | 47 (36.2) | 24 (26.4) | 40 (42.1) | ||||
| Abuse | The use of cannabis for therapeutic purposes can cause addiction | yes | 48 (45.7) | 148 (70.1) | <0.001 | 83 (63.8) | 56 (61.5) | 57 (60.0) | 0.836 |
| no | 57 (54.3) | 63 (29.9) | 47 (36.2) | 35 (39.5) | 38 (40.0) | ||||
| The use of cannabis for therapeutic purposes would cause drug abuse | yes | 88 (83.8) | 195 (92.4) | 0.031 | 117 (90.0) | 83 (91.2) | 83 (87.4) | 0.677 | |
| no | 17 (16.2) | 16 (7.6) | 13 (10.0) | 8 (8.8) | 12 (12.6) | ||||
| The use of cannabis for therapeutic purposes may be the gateway to hard drugs use | yes | 45 (42.9) | 134 (63.5) | 0.001 | 76 (58.5) | 58 (63.7) | 45 (47.4) | 0.068 | |
| no | 60 (57.1) | 77 (36.5) | 54 (41.5) | 33 (26.3) | 50 (52.6) | ||||
| Legislation | The use of cannabis requires the development of clear guidelines | yes | 98 (93.3) | 202 (95.7) | 0.519 | 121 (93.1) | 89 (97.8) | 90 (28.5) | 0.287 |
| no | 7 (6.7) | 9 (4.3) | 9 (7.9) | 2 (2.2) | 5 (1.6) | ||||
| I am aware that in some countries therapeutic use of cannabis has been approved | yes | 103 (98.1) | 195 (92.4) | 0.073 | 122 (93.8) | 87 (95.6) | 89 (93.7) | 0.817 | |
| no | 2 (1.9) | 16 (7.6) | 8 (6.2) | 4 (4.4) | 6 (6.3) | ||||
| I am familiar with the current legalization process of cannabis in Serbia | yes | 57 (54.3) | 79 (37.4) | 0.006 | 52 (40.0) | 46 (50.5) | 38 (40.0) | 0.230 | |
| no | 48 (45.7) | 132 (62.6) | 78 (60.0) | 45 (49.5) | 57 (60.0) | ||||
| The use of cannabis for therapeutic purposes should be legalized in Serbia | yes | 90 (85.7) | 150 (71.1) | 0.006 | 94 (72.3) | 67 (73.6) | 79 (83.2) | 0.14 | |
| no | 15 (14.3) | 61 (28.9) | 36 (27.7) | 24 (26.4) | 16 (16.8) | ||||
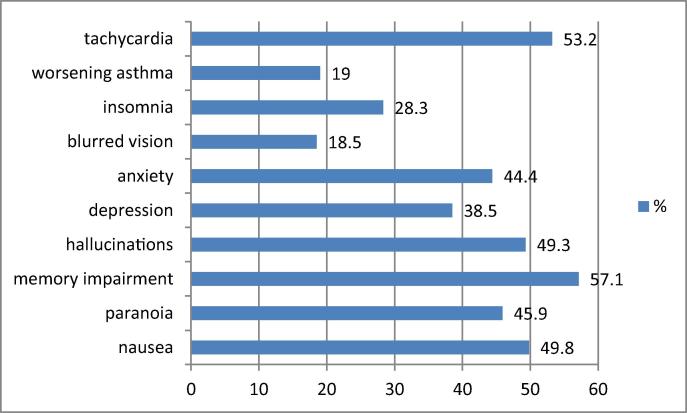
For students stated in the previous part of the questionnaire that they were familiar with the possible therapeutic effects, the most commonly recognized therapeutic indications for cannabis use were: chronic pain (194, 75.2%), cancer (190, 73.6%) and muscle spasm (94, 36.4%) (Fig. 1), while for the students who previously stated that they were familiar with possible side effects the most common adverse effects were memory impairment (117, 57.1%), tachycardia (109, 53.2%), nausea (102, 49.8%) and hallucinations (101, 49.3%) (Fig. 2). On average, students marked as recognized 3 indications (M = 3, IQR = 2–4) and 4 side effects (M = 4, IQR = 3–5). There was statistically significant difference in the number of recognized indications between students of different study year (p = 0.049), final year students recognized larger number of indications than 3rd year students (p = 0.018). The same was observed for the number of recognized side effects (p = 0.033). Students who reported previous cannabis use identified larger number of indications (p < 0.001) than those who did not, but there was no difference in number of recognized side effects among cannabis users and non-users.
Fig. 1.
Identified indications for therapeutic use of cannabis.
Fig. 2.
Identified side effects of cannabis therapeutic use.
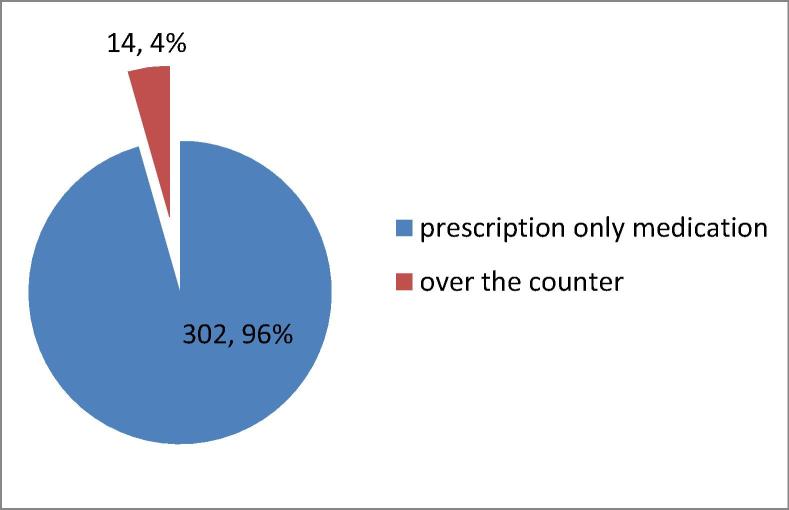
Almost all of the examined students believed that approved products based on cannabis should be issued as prescription only medications (302, 96%) (Fig.3).
Fig. 3.
Students' opinion regarding cannabis issuing (if legalized for therapeutic use).
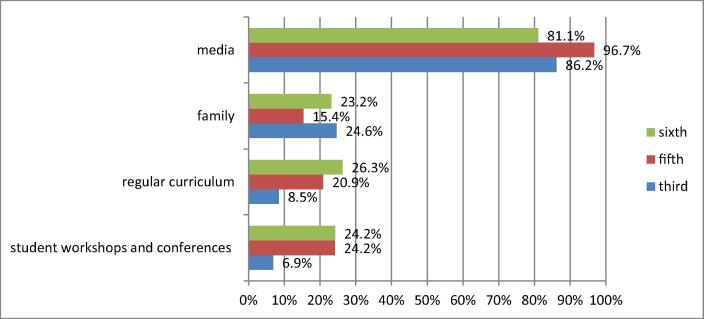
Students of all study years were mostly informed about cannabis therapeutic use through the media (96.7% fifth year, 86.2% third year and 81.1% sixth year). However, students of the fifth and sixth year were notably more informed through courses, at student workshops and conferences compared to students of the third year of study (Fig. 4).
Fig. 4.
Sources of medical information regarding cannabis use.
4. Discussion
This study aimed to reflect the medical students’ knowledge regarding medical cannabis use and its possible abuse in relation to their previous use of marijuana and education. To the best of our knowledge, this is the first detailed study of this type conducted in Serbia.
The lifetime use of cannabis was reported by 32% of the medical students in our study, which is in agreement with the earlier study conducted in Belgrade among medical students, as well as with the study which included not-only medical students at the University of Belgrade. Although the majority of students were female, the frequency of previous cannabis use was significantly higher among male students. This finding is not compatible with those obtained in similar studies performed in Serbia, Greece and Kansas, where no gender differences was noticed regarding previous cannabis consumption among medical and pharmacy students (Moeller and Woods, 2015, Papazisis et al., 2015, Vujcic et al., 2017). On the other hand, our result is in line with the Serbian national survey regarding cannabis use, according to which the lifetime use of cannabis was higher among male respondents (10.4%) aged 18–64 years than among females as well as among medical students in Brazil (Petroianu et al., 2010). However, sensitive nature of asking respondents about previous use of illegal cannabis could be a reason for misreporting on this topic among as general population (Tourangeau and Yan, 2007).
In our survey, larger share of students who had previously used marijuana more frequently stated that they were familiar with possible therapeutic effects of medical cannabis and its side effects. These findings have already been demonstrated in earlier studies conducted in Serbia and USA (Moeller and Woods, 2015, Vujcic et al., 2017). Likewise, there was no difference between the year of the study with respect to the perceived awareness about therapeutic and adverse effects, which implies that clinical teaching and hospital training during the fifth and sixth years of the study had no influence on students’ knowledge with respect to medical cannabis. Association between the year of the study in relation to therapeutic and adverse effects of medical cannabis was lacked in similar study conducted in Kansas (Moeller and Woods, 2015). However, when the number of identified indications and side-effects was compared among different year students, there were differences between 3rd and final year students. Therefore, it seems that education does to some extent influence the knowledge about cannabis, but the number of identified indications and side-effects was generally low. Furthermore, the only two approved indications identified correctly by more than 50% of medical students were use of cannabis in the treatment of cancer and chronic pain. Besides superficiality in knowledge regarding indications for medical cannabis, the lack of accurate knowledge on adverse reactions was also observed in our study. Not more than two adverse effects (tachycardia and memory impairment) were recognized correctly by more than 50% of all the students included in this investigation. Similar lack of knowledge about the indications and adverse effects of medical cannabis was noted in the previous study conducted in Serbia and in study performed in Kansas (Moeller and Woods, 2015, Vujcic et al., 2017).
Our results has shown that students who have never used marijuana were more familiar with possible cannabis abuse and were more of the opinion that use of cannabis for therapeutic purposes can cause addiction or can be the gateway to hard drugs use. This is in good correlation with previous study about attitudes among Serbian medical students where students who reported previous marijuana users more often believed that medical cannabis is safe in comparison to those who never consumed marijuana (Vujcic et al., 2017). Likewise, Chan et al. has proved that greater belief in medical benefits and lower belief in medical risks were strongly associated with history of cannabis use (Chan et al., 2017; 19).
In our study, the majority of the students were aware that in some countries therapeutic use of cannabis has been approved, while students who previously used cannabis were more addressed in the current legalization process in Serbia. In the earlier study conducted in Serbia among pharmacy students, approximately one third was familiar with the current legalization process (Stojanovićet al., 2017). However, this study did not explore the differences between previous marijuana users and non-users and was conducted among pharmacy students, thus it is not completely comparable with our study. Furthermore, significantly greater number of previous users believed that the use of cannabis for therapeutic purposes should be legalized in Serbia, which is in agreement with other similar studies (Moeller and Woods, 2015, Vujcic et al., 2017). The common belief is that the legalization of medical cannabis might cause in the ‘leakage’ of the cannabis into the illegal market and consequently in the use of medical cannabis for non-medical purposes (Pinkaset al., 2016). This was confirmed by Salomonsen-Sautel et al. who showed that 74% of teenagers in the United States have used someone else’s medical cannabis (Salomonsen-Sautelet al., 2012). The positive attitude toward medical cannabis was also noticed among urban adult population in Belgrade was also confirmed in the similar study performed 2017 by Gazibara et al. These results contrast considerably from students' attitudes explored by Burke and Marx, however this study was performed more than four decades ago (Burke and Marx, 1971). Undoubtedly, changes in legalization, cultural acceptance, social media exposure and decreased perception of risks shift opinions over the past forty years. However, our research has showed that the majority of both previous users and students that never used marijuana were of the opinion that the development of clear guidelines is necessary for cannabis use, which is in accordance with practice regarding cannabis medical use in countries where it is already approved. For example, in Croatia, the prescription should contain the amount of THC in a single dose, the number of individual doses, pharmaceutical formulation, and dosage and application method (Balkan Insight, 2015).
In addition, almost all of the examined students believed that approved products based on cannabis should be issued as prescription only medications, which is also comparable with the previous research conducted among pharmacy students (Stojanovićet al., 2017). In the neighboring country Croatia, where medical cannabis is legal, situation is in line with our students' opinions. Actually, products based on cannabinoids, can be prescribed by physicians working in general and family practice, however only with the recommendation of certain neurology, infectious disease or cancer specialists (Balkan Insight, 2015). In Czech Republic, only 16 specialists are permitted to prescribe medical cannabis, while only 26 pharmacies are authorized to dispense it. Overall, there is no country that allows the possession of medical cannabis without prescription, nor the cultivation of cannabis that is used in medical purposes without government supervision (Guyet al., 2004).
Students of all study years mostly learned about cannabis therapeutic use through the media, which is partially in line with former researches performed in Serbia where more than a half of pharmacy students learned about medical cannabis from sources other than school (Vujcic et al., 2017, Stojanović et al., 2017). Similarly, students in the study performed in Kansas indicated that they have received little to no education regarding the use of medical cannabis in the pharmacy curriculum (Moeller and Woods, 2015). Despite the fact that our results showed that students of the fifth and sixth year were notably more informed through courses, at student workshops or conferences compared to students of the third year of study, there is a still a lack of formal education regarding cannabis therapeutic use and that education opportunities regarding medical cannabis should be developed in the near future.
Some weaknesses of the study need to me mentioned. Firstly, data on previous cannabis use was self-reported, and considering the sensitive nature of asking such questions, information bias cannot be excluded. Secondly, the survey was performed at the only one institution and should be expanded to include prospective doctors from other Universities in the country. What is more, due to ethical issues, we did not ask students in detail about their demographic characteristics such as religion, income level, monthly allowance and living arrangements which may have lead to certain confounding factors being omitted.
5. Conclusion
Students' knowledge was in correlation with previous marijuana consumption, as previous marijuana users were more knowledgeable about therapeutic and side effects, while students who never consumed marijuana were more aware of possible abuse. Although the majority of students had positive attitude toward cannabis legalization, previous marijuana consumers were more supportive of this issue. Year of the study had not significantly influence both on the knowledge about medical cannabis and attitude toward its legalization. However, superficiality in students' knowledge and lack of formal education speaks in favor of the necessity for introducing lectures about medical cannabis for prospective doctors.
Conflicts of interest
The authors of this manuscript have no conflicts of interest to declare.
Funding
This work was supported by the Ministry of Science and Technological Development, Republic of Serbia (project No. 41012) and by the Provincial Secretariat for Science and Technological Development, Autonomous Province of Vojvodina (project No. 114-451-2178/2016-03).
Acknowledgements
We would like to thank all the students involved in this research for giving up their time to take part in the study.
Footnotes
Peer review under responsibility of King Saud University.
References
- Aggarwal S.K., Carter G.T., Sullivan M.D., ZumBrunnen C., Morrill R., Mayer J.D. Medical use of cannabis in the United States: historical perspectives, current trends, and future directions. J. Opioid. Manage. 2009;5(3):153–168. doi: 10.5055/jom.2009.0016. [DOI] [PubMed] [Google Scholar]
- Balkan Insight, 2015. Croatia legalizes marijuana for medical use <htpp://www.balkaninsight.com/en/article/Croatia-firstbalkan-country-to-legalize-medical-marijuana> (accessed January 15, 2017).
- Ben Amar M. Cannabinoids in medicine: a review of their therapeutic effects. J. Ethnopharmacol. 2006;105(1–2):1–25. doi: 10.1016/j.jep.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Bifulco M., Pisanti S. Medical use of cannabis in Europe. EMBO Rep. 2015;16(2):130–132. doi: 10.15252/embr.201439742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birdsall S.M., Birdsall T.C., Tims L.A. The use of medical marijuana in cancer. Curr. Oncol. Rep. 2016;18(7):40. doi: 10.1007/s11912-016-0530-0. [DOI] [PubMed] [Google Scholar]
- Burke W.M., Marx M.B. Attitudes of professional students toward legal control of psychoactive substances HSMHA. Health. Rep. 1971;86(8):725–732. [PMC free article] [PubMed] [Google Scholar]
- Chan M.H., Knoepke C.E., Cole M.L., McKinnon J., Matlock D.D. Colorado medical students' attitudes and beliefsabout marijuana. J. Gen. Intern. Med. 2017;32:463–485. doi: 10.1007/s11606-016-3957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction, 2017, Cannabis legislation in Europe: an overview. Publications Office of the European Union, Luxembourg.
- Gazibara T., Prpic M., Maric G., Pekmezovic T., Kisic-Tepavcevic D. Medical cannabis in Serbia: the survey of knowledge and attitude in an urban adult population. J. Psychoactive. Drugs. 2017;49(3):217–224. doi: 10.1080/02791072.2017.1292434. [DOI] [PubMed] [Google Scholar]
- Guy G., Whittle B.A., Robson P.J. Pharmaceutical Press; London: 2004. Medical Uses of Cannabis and Cannabinoids. [Google Scholar]
- Horvat O., Raskovic A., Jakovljevic V., Sabo J., Berenji J. Interaction of alcoholic extracts of hops with cocaine and paracetamol in mice. Eur. J. Drug. Metab. Pharmacokinet. 2007;32(1):39–44. doi: 10.1007/BF03190988. [DOI] [PubMed] [Google Scholar]
- Iannitelli A., Quartini A., Tirassa P., Bersani G. Schizophrenia and neurogenesis: a stem cell approach. Neurosci. Biobehav. Rev. 2017;80:414–442. doi: 10.1016/j.neubiorev.2017.06.010. [DOI] [PubMed] [Google Scholar]
- Jouanjus E., Lapeyre-Mestre M., Micallef J. Cannabis use: signal of increasing risk of serious cardiovascular disorders. Am Heart J. 2014;3(2):e000638. doi: 10.1161/JAHA.113.000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law on Psychoactive Controlled Substances. Official Gazette of the Republic of Serbia, No 99/2010 and 57/2018.
- Manzanares J., Julian M., Carrascosa A. Role of the cannabinoid system in pain control and therapeutic implications for the management of acute and chronic pain episodes. Curr. Neuropharmacol. 2006;4(3):239–257. doi: 10.2174/157015906778019527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller K.E., Woods B. Pharmacy students’ knowledge and attitudes regarding medical marijuana. Am. J. Pharm. Educ. 2015;79(6):85. doi: 10.5688/ajpe79685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papazisis G., Sarrigiannidis A., Pourzitaki C., Apostolidou E., Garyfallos G., Kouvelas D. Substance useamong medical students in Greece. Clin. Ther. 2015;37:e95. [Google Scholar]
- Petroianu A., Reis D.C., Cunha B.D., Souza D.M. Prevalence of alcohol, tobacco and psychotropic drug use among medical students at the Universidade Federal de Minas Gerais. Rev. Assoc. Med. Bras. 2010;56(5):568–571. doi: 10.1590/s0104-42302010000500019. (1992) [DOI] [PubMed] [Google Scholar]
- Pinkas J., Jablonski P., Kidawa M., Wierzba W. Use of marijuana for medical purposes. Ann. Agric. Environ. Med. 2016;23(3):525–528. doi: 10.5604/12321966.1219200. [DOI] [PubMed] [Google Scholar]
- Quartini A., Pacitti F., Bersani G., Iannitelli A. From Adolescent neurogenesis to schizophrenia: opportunities challenges and promising interventions. Biomed Rev. 2017;28:66–73. [Google Scholar]
- Sabo A., Horvat O., Stilinovic N., Berenji J., Vukmirovic S. Industrial hemp decreases intestinal motility stronger than Indian hemp in mice. Eur. Rev. Med. Pharmacol. Sci. 2013;17(4):486–490. [PubMed] [Google Scholar]
- Salomonsen-Sautel S., Sakai J.T., Hopfer C. Medical marijuana use among adolescents in substance abuse treatment. J. Am. Acad. Child. Adoles. Psychiatry. 2012;51(7):694–702. doi: 10.1016/j.jaac.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stojanović M., Tomas A., Paut Kusturica M., Rašković A., Ubavić M., Tomić Z., Sabo A., Horvat O. Pharmacy students’ knowledge and attitudes regarding cannabis for medical purposes. Hospital. Pharmacol. 2017;4(3):559–567. [Google Scholar]
- Tourangeau R., Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133(5):859–883. doi: 10.1037/0033-2909.133.5.859. [DOI] [PubMed] [Google Scholar]
- Vujcic I., Pavlovic A., Dubljanin E., Maksimovic J., Nikolic A., Sipetic-Grujicic S. Attitudes toward medical cannabis legalization among serbian medical students. Subst. Use. Misuse. 2017;52(9):1225–1231. doi: 10.1080/10826084.2017.1302959. [DOI] [PubMed] [Google Scholar]
- Zuardi A.W. History of cannabis as a medicine: a review. Rev. Bras. Psiquiatr. 2006;28(2):153–157. doi: 10.1590/s1516-44462006000200015. [DOI] [PubMed] [Google Scholar]