Abstract
The transition from adolescence to adulthood is a critical life phase as it is during this period that substance use and disorders typically emerge and escalate. Globally, few studies have examined the prevalence and correlates of alcohol and tobacco use among youth (ages 15 – 24). This study seeks to bridge this gap by assessing the influence of structural and micro-level factors on tobacco and alcohol use among youth in Low- and Middle-income countries (LMICs). Data are drawn from the Multiple Indicator Cluster Surveys (MICS) conducted in 29 countries or regions in Eastern Europe, Latin America, Asia and Africa between 2010 and 2015. Analyses focus on lifetime prevalence and age of onset for tobacco and alcohol use. Descriptive analyses highlight regional variations in the prevalence and age of onset of tobacco and alcohol use: tobacco use is more concentrated among youth in Eastern Europe but alcohol use is generalized across the regions. Using multi-level analyses, we find statistically significant main effects for age, gender, educational attainment, rural residence, marital status and exposure to mass media on tobacco and alcohol use outcomes as well as interaction effects for age, gender and education on tobacco and alcohol use outcomes. These findings highlight the need for structural interventions to control tobacco social marketing, and for gender considerations in tobacco and alcohol use prevention programs and policies.
BACKGROUND
Substance use (including tobacco and alcohol use) contributes to nearly half of the morbidities among young people aged 10 – 24 years (Gore et al., 2011; Patton et al., 2009) and to the epidemic of non-communicable diseases among adults such as obesity, cardiovascular disease and cancer (Beaglehole et al., 2011; Ezzati & Riboli, 2013; Sawyer et al., 2012). Alcohol use can interfere with young people’s ability to successfully negotiate the developmental tasks associated with the transition to adulthood (Charlson, Diminic, Lund, Degenhardt, & Whiteford, 2014; Staff et al., 2010). Tobacco use alone is responsible for about 6.3 million annual deaths worldwide and accounts for 6.3% of the global burden of disease, mostly in low- and middle-income countries (LMICs) (Murray & Lopez, 2013). Tobacco is a gateway drug to other types of substance use including alcohol and illicit drugs (Chen et al., 2002; Torabi, Bailey, & Majd‐Jabbari, 1993). Substance use and misuse can lead to unintentional injuries and increased risk for HIV/AIDS among youth (Mbulaiteye et al., 2000; Zablotska et al., 2006), due to increased risky sexual behavior, sexual coercion and intimate partner violence among youth (Choudhry, Agardh, Stafstrom, & Ostergren, 2014; Mehra, Agardh, Stafstrom, & Ostergren, 2014; Shuper, Joharchi, Irving, & Rehm, 2009; Zablotska et al., 2009). As such, the prevention of substance use and disorders is necessary for the realization of the global sustainable development goals (SDGs) related to reductions in premature mortality from non-communicable diseases, non-intentional deaths and injuries, and global burden of HIV and AIDS (United Nations, 2016).
The transition from adolescence to adulthood is a critical period during which future health and life trajectories are established (Beaglehole et al., 2011; National Research Council, 2015; Sawyer et al., 2012). It is during this phase that substance use and disorders typically emerge and escalate (Brown et al., 2008; Schulenberg & Maggs, 2002; Schulenberg, Sameroff, & Cicchetti, 2004). Numerous studies have examined the risk and protective factors for substance use among young people, but the majority of these studies focus on youth in high-income countries (Patton et al., 2012). The few existing studies outside this context largely focus on younger adolescents (ages 11 – 15) yet substance use typically emerges and escalates in middle to late adolescence, and the factors that influence substance use vary between younger and older adolescents and young adults (Dodge et al., 2009; Staff et al., 2010). The transition from adolescence to adulthood is also characterized with changes in social roles (e.g. marriage, parenthood, employment) and contexts for individual development, which may differently shape young people’s risk for substance use and disorders (Staff et al., 2010). The present study is designed to address this gap by focusing on tobacco and alcohol use in LMICs during late adolescence and early adulthood.
Socio-demographic variations in tobacco and alcohol use have been widely documented. Tobacco and alcohol use generally increase with age, and an early age of onset for alcohol and tobacco use is associated with increased risk for substance abuse and addiction in adulthood (Sawyer et al., 2012). Tobacco and alcohol use, both previously higher among males, have increased among females and are now higher among females than males, especially in LMICs (DiNapoli, 2009; Global Youth Tobacco Survey (GYTS) Collaborating Group, 2003; Schulenberg et al., 2017; WHO, 2010). Prior studies have reported lower levels of tobacco use but higher levels of alcohol use among youth with college or higher education (Karam, Kypri, & Salamoun, 2007; Schulenberg, Maslowsky, Patrick, & Martz, 2016; Slutske et al., 2004; Staff et al., 2010). The relationship between socio-economic status and tobacco/alcohol use has been contradictory. Some studies have reported higher levels of tobacco/alcohol use among youth in more affluent households (Hanson & Chen, 2007; Huckle, You, & Casswell, 2010; Moor et al., 2015; Pförtner et al., 2015; Richter, Leppin, & Gabhainn, 2006; Spijkerman, van den Eijnden, & Huiberts, 2008). Other studies have reported higher levels of use among youth in less affluent households (Dishion, Capaldi, & Yoerger, 1999; Huckle et al., 2010; Moor et al., 2015; Pförtner et al., 2015). Tobacco and alcohol use is also higher among youth in residing in urban areas compared to rural areas (Savell et al., 2015). Alcohol use tends decline with transition into marital roles (Staff et al., 2010). However, prior studies have found that higher levels of tobacco and alcohol use among youth who are married at a younger age (Kuntsche, Knibbe, Engels, & Gmel, 2007; Kuntsche, Knibbe, Gmel, & Engels, 2005; Schulenberg & Maggs, 2002; Staff et al., 2010).
Tobacco and alcohol use has been associated with psychosocial and environmental factors. Early childhood exposures (e.g. childhood behavioral problems, parental alcoholism) (Dishion et al., 1999; Sibley et al., 2014) and psychosocial factors (e.g. low self-esteem and mental health problems) (Dodge et al., 2009; Masten & Cicchetti, 2010) have also been associated with tobacco and alcohol use among young people. Contextual influences on tobacco and alcohol use include family and peer factors e.g. parental or sibling substance use, parental supervision and monitoring, socio-economic status, peer pressure, association with deviant peers, school drug use policies (Hanson & Chen, 2007; Kuipers et al., 2016; Luk, Wang, & Simons-Morton, 2010; Richter et al., 2006; Simons-Morton & Farhat, 2010). Environmental factors such as mass media exposure to tobacco/alcohol advertising (Anderson, De Bruijn, Angus, Gordon, & Hastings, 2009; Grube & Waiters, 2005; Wakefield, Flay, Nichter, & Giovino, 2003), easy availability of tobacco and alcohol and drug use norms (Bendtsen et al., 2014; Snedker, Herting, & Walton, 2009; Thrul, Lipperman-Kreda, Grube, & Friend, 2014; Winstanley et al., 2008) also influence substance use among young people.
Globally, regional variations in the prevalence of tobacco and alcohol use among young adolescents (aged 11– 15) have been documented (Bendtsen et al., 2014; Degenhardt et al., 2008; Moor et al., 2015; Page & Danielson, 2011; WHO, 2010), although differences in study approaches to assessing tobacco and alcohol use limit direct comparisons of estimates. Existing data suggest that alcohol and substance use may be higher among adolescents in Europe and the Americas than among those in Africa and other regions (Degenhardt et al., 2008; Karam et al., 2007; World Health Organization, 2016a, 2016b). For example, the World Health Organization (2014) estimated prevalence of current alcohol use among young people aged 15 – 19 is 29.3% in Africa, 52.7% in the Americas, 69.5% in Europe, and 10% in Eastern Mediterranean region (WHO, 2014). The estimated prevalence of current cigarette use in the Global Youth Tobacco Survey conducted between 1999 and 2008 among students aged 13 – 15 years ranged from 7% among boys and 2% among girls in Eastern Mediterranean region to 21% among boys and 17% among girls in the European Region. The prevalence of cigarette smoking in the African region was 14% among boys and 5% among girls (Centers for Disease Control (CDC), 2016).
Regional variation in alcohol and tobacco use among young people has been attributed to structural factors such as laws and regulations and socio-cultural norms related to alcohol and tobacco use (Anderson, De Bruijn, Angus, Gordon, & Hastings, 2009; Bendtsen et al., 2014; Bendtsen, Damsgaard, Tolstrup, Ersbøll, & Holstein, 2013; Grube & Waiters, 2005). These cross-national variations in substance use have been associated with increasing globalization, industrialization, urbanization and mass media exposure, possibly due to their impact on traditional family and community controls on the transition to adulthood such as reduced parental control, social support and social cohesion, and through rapid dissemination of non-traditional ideas and values (Sawyer et al., 2012).
Structural indicators of national economic development and income inequity have also emerged as important predictors of substance use among young people (Elgar, Roberts, Parry-Langdon, & Boyce, 2005; Pampel, 2007; Pfoertner, Rathmann, Moor, Kunst, & Richter, 2016; Rehm et al., 2009). In low-income countries, there is a strong relation between economic wealth and alcohol consumption: the higher the gross domestic product (GDP), the higher the overall volume of consumption and the lower the proportions of abstainers (Rehm et al., 2009). Income inequity (measured using the GINI) has also been associated with alcohol use. A study of school aged children (aged 11 – 15) in 31 European countries, Canada, the United States and Europe found that younger adolescents (aged 11 – 13) living in countries with high income inequities consumed more alcohol than their counterparts living in countries of low income inequity (Elgar et al., 2005).
The unregulated marketing of unhealthy behaviors and lifestyles by multi-national tobacco and alcohol corporations in LMICs has also emerged as a potent threat to health of young people in these countries (Grube & Waiters, 2005; Stacy, Zogg, Unger, & Dent, 2004; Wakefield, Flay, Nichter, & Giovino, 2003). There is evidence of targeted marketing of these products to young people (Maziak, 2011; Warren, Jones, Eriksen, Asma, & group, 2006) and women (WHO, 2010) in LMICs. Moreover, the increased access to digital media (i.e. internet and social network sites such as Facebook) in LMICs has transformed the very notion of an adolescent’s peer group influences (O’Keeffe & Clarke-Pearson, 2011) and provided a medium for the rapid dissemination of information, attitudes and risky behaviors (Grube & Waiters, 2005; Sawyer et al., 2012; Wakefield et al., 2003).
OBJECTIVES
Developing contextually and developmentally relevant interventions to mitigate the consequences of substance use among youth in LMICs requires understanding of the contextually relevant micro-structural factors that shape youth’s substance use. This paper seeks to contribute to this goal by examining the prevalence and correlates (both micro and structural) of tobacco and alcohol use among youth in LMICs. Using a cross-sectional sample of 27 countries or regions representing LMICs, we examine cross-national and multi-level effects of micro- and structural- level risk factors for lifetime use of tobacco and alcohol, age of onset for tobacco and alcohol, and current (30-day) use of tobacco and alcohol. We also assessed within country effects of micro-level factors on tobacco and alcohol use, and gender by age and education interactions on tobacco and alcohol use. We hypothesized that tobacco and alcohol use would be higher in Europe compared to Africa and the Middle East, and that these regional variations in alcohol and tobacco use would be driven by structural- level factors such as national economic development and income inequity. We also hypothesized that alcohol/tobacco use would be higher among male than female youth. Lastly, we also hypothesized positive association between alcohol use and education attainment and a negative association between tobacco use and education attainment.
METHODS
Data
This study utilizes Multiple Indicator Cluster Survey (MICS) data. Datasets are available for download upon request from http://mics.unicef.org/. MICS is a cross-sectional household survey conducted by UNICEF and governments in over 100 low- and middle- income countries, to assist with monitoring the health of women and children in those countries. UNICEF provides training, materials, and support for standard methods of data collection across participating countries. The uniformity in measures, sample size determination, sampling and post-stratification adjustments enables comparability of data across countries. However, in some countries, data were collected at both national and regional level (e.g. Macedonia and Macedonia Roma settlements) and in other countries, data were collected at the regional level only (e.g. Kenya Turkana, Bungoma and Kakamega settlements). In the present analyses, these regional datasets were analyzed separately because the regions do not adequately represent a given country. Additionally, only 11 of the 27 countries (or regions) included in these analyses had data on both male and female respondents.
These analyses focused on youth ages 15 to 24. Data are drawn from two rounds of surveys (i.e. MICS4 and MICS5) conducted between 2010 and 2015. For each country (or region), the most recent data were utilized. Only countries with data on alcohol and tobacco use among youth were included in these analyses. The 27 countries and regions are located in Eastern Europe (i.e. Belarus, Bosnia, Bosnia Roma settlements, Kosovo, Kosovo Roma settlements, Macedonia, Macedonia Roma settlements, Moldova, Montenegro, Montenegro Roma settlements, and Ukraine), the Caribbean (i.e. Barbados, Panama, Jamaica, Dominican Republic), Africa (Kenya Bungoma, Kenya Kakamega and Kenya Turkana regions, Madagascar, Sao Tome and Principe, and Tunisia), and Asia (Nepal, Nepal West, Pakistan Punjab, Mongoliaand Mongolia Khuv settlements).
Measures
The primary outcome measures were tobacco and alcohol use variables. Three sets of outcome variables were examined in these analyses: (1) lifetime use of tobacco and alcohol – binary variables coded as yes or no; (2) current (past 30-day) use of tobacco and alcohol – binary variables coded as yes or no; and (3) age of onset for tobacco and alcohol use – age when respondent first used alcohol or tobacco.
Micro-level factors included: age (years); sex (male or female); marital status (currently married and previously/never married); type of place of residence (urban or rural); level of education (primary school, secondary school, and higher education); household income quintiles (poorest, poor, middle, rich and richest); and frequency of exposure to mass media (i.e. mean frequency of listening to radio, watching TV, reading newspapers or magazines in the past month). This mass media index demonstrated adequate psychometric properties in these analyses: α = 0.72.
Structural level factors included four national development indicators: Gross Domestic Product per capita (GDPpc), Gross National Income per Capita (GNIpc), Human Development Index (HDI) and GINI index- an indicator of income inequity. These data were abstracted from the World Bank database (http://data.worldbank.org/indicator/). Additionally, an aggregated mass media exposure score was computed for each country.
Data analysis
Data analyses were conducted using SPSS IBM version 24. Descriptive analyses were utilized to examine the distribution of the tobacco and alcohol indicators: age of onset for tobacco and alcohol were found to be normally distributed. Bivariate analyses were also conducted to examine the associations between the micro- and structural- level factors affecting tobacco and alcohol outcomes. To examine the cross-national and multi-level effects of micro- and structural- level risk factors on tobacco and alcohol use (both lifetime and current) and age of onset, a series of multi-level logistic and linear regressions was conducted. Logistic regression models were used to analyze the binary outcomes related to both lifetime use and current use of tobacco and alcohol, while linear regression models were used for the continuous outcomes related to age of onset for tobacco and alcohol use.
For each outcome variable, the cross-national multi-level analyses started with a random intercept model without any micro-level or structural factors, followed by a random intercept model with structural factors only and then with both structural and micro-level factors. In all the analyses, a country indicator was used as a cluster variable. Due to potential for collinearity, each structural factor was analyzed with a unique model. Akaike’s information criteria (AIC) and a percent of correct model classification were used to determine model fit.
To assess the within-country predictors of tobacco and alcohol use, a series of multivariate logistic regression and linear regression models were conducted. Micro-level factors were added simultaneously to each model as predictor variables. Due to the small sample size relative to the number of independent predictors and the lower proportion of respondents who had ever tried smoking, within-country variation in tobacco and alcohol use could not be examined in the Kenya Turkana, Bungoma and Turkana regions. Montenegro Roma settlements were also dropped from these analyses due to a low sample size, while Tunisia was dropped from the analyses on alcohol use due to the low proportion (0.6%) of respondents who reported alcohol use.
Lastly, gender by age and education interactions were assessed using a series of multivariate logistic regression and linear regression models. Each interaction was assessed independently. Only statistically significant interactions are included in this report.
RESULTS
Table 1 presents a descriptive summary of lifetime use and age of onset for tobacco and alcohol use among youth. The prevalence of lifetime tobacco use ranged from less than one percent in Kenya (i.e. Bungoma and Kakamega) and Pakistan Punjab regions to over 60% in Belarus (60.3%). Eastern European countries had the highest prevalence of lifetime tobacco use (> 40%). Water pipe (85.4%) and cigarette (7.4%) were the most frequently utilized type of smoked tobacco products, while snuff (29.6%) and dip (29.8%) were the most frequently utilized smokeless tobacco products. The prevalence of lifetime alcohol use ranged from less than one percent in Lebanon and Tunisia to over 80% in the Dominican Republic (83.3%), Ukraine (84.5%), Belarus (88%) and Moldova (89%).
Table 1.
Overview of variables included in the analysis
| Variable | Description | Values / Measures |
|---|---|---|
| Outcome variables | ||
| Tobacco use | Ever tried tobacco | 1 – ever, 2 – never |
| Tobacco age of onset | Age when the first whole cigarette was smoked | Number of years |
| Alcohol use | Ever drunk alcohol | 1 – ever, 2 – never |
| Alcohol age of onset | Age when alcohol was used for the first time | Number of years |
| Individual level predictor variables | ||
| Gender | Sex of respondent | 0 – male, 1 – female |
| Age | Years categorized as 15 – 19 years and 20 – 24 years | 1 – 15-19 years, 2 – 20-24 years |
| Education | Education of the respondent | 0 – preschool, 1 - primary, 2 – secondary, 3 - higher |
| Marital Status | Marital status of the respondent | 0 – formerly married/in union, 1 – currently married/in union, 2 – never married/in union |
| Household income | Household income quintile | 1 – Poorest, 2 – Second, 3 – Middle, 4 - Fourth 5 - Richest |
| Residence | Type of residence | 0 – rural, 1 - urban |
| Exposure to Mass media | Mean exposure to mass media | Measured as mean frequency of: reading newspaper or magazine, listening to the radio, watching TV and Internet usage in the past month |
| Country level predictor variables | ||
| GDPpc | Gross Domestic Product per capita | |
| GNI | Gross National Income | |
| HDI | Human Development Index | |
| GINI | GINI coefficient of inequality | |
The median age at onset for tobacco use was 16.2 years, ranging from 14.4 years in Nepal to 20 years among the youth in Kenya Turkana region. Notably, Roma settlements had a high prevalence (>40%) and a low age of onset (< 16 years) for tobacco use. The median age of first alcohol use was 16.2 years, ranging from 12.8 years in Nepal West to 18.6 years in Tunisia. In three countries (or regions), the mean age of onset for alcohol use was less than 14 years: Kenya Bungoma region (13.9 years), Nepal (13.8 years) and Nepal West (12.8 years). Only Mongolia and Tunisia had a mean age of onset for alcohol use that was over 18 years.
Cross-national variation in tobacco and alcohol use
The intercepts for all the tobacco related outcomes (i.e., lifetime use, age of onset, and current use) were statistically significant thus indicating that these outcomes varied across countries (results not presented). Among the alcohol outcomes, only age of onset of alcohol use had a significant intercept, thus suggesting cross-national variation in age of onset for alcohol use differed across the country but lifetime use and current use of alcohol.
With the exception of the aggregated country level mass media exposure score, none of the structural level factors (i.e. GDPpc, GNI, HDI and GINI) was significantly associated with lifetime use, current use or age of onset of tobacco and alcohol use (results not presented). Therefore, none of the structural factors was included in the subsequent analyses. The country level aggregated mass media score was significantly associated with greater odds for lifetime tobacco use (AOR = 1.64; p < .001) and alcohol use (AOR = 1.464; p < .001). The addition of the micro-level factors to the model greatly improved model fit and percent of correct classification, but the models with the aggregated mass media score did not differ from the models with micro-level factors only. Therefore, the subsequent findings focus on models with micro-level factors only.
Tables 2 presents the results of the multi-variable logistic and regression analyses conducted to assess the influence of micro-level factors on lifetime use, current use and age of onset for tobacco and alcohol use.
Table 2.
Descriptive statistics for prevalence (of ever use), age of onset and frequency of using alcohol and tobacco among youth aged 15 – 24 years
| Country |
Tobacco use |
Alcohol use |
|||
|---|---|---|---|---|---|
| Sample size |
Ever use Percent |
Age of onset Median (SD) |
Ever use Percent |
Age of onset Median (SD) |
|
| Barbados | 388 | 22.2 | 16.6 (2.8) | 77.4 | 15.9 (2.8) |
| Belarus | 1,673 | 60.3 | 15.9 (2.0) | 88.0 | 16.2 (1.7) |
| Bosnia | 1,952 | 39.7 | 16.2 (2.3) | 53.8 | 16.3 (2.0) |
| Bosnia Roma | 1,095 | 49.6 | 14.9 (2.5) | 51.0 | 15.3 (2.3) |
| Dominican Republic | 10,904 | 10 | 17.0 (3.4) | 83.3 | 15.2 (2.4) |
| Kenya Bungoma | 480 | 0.7 | 17.6 (2.1) | 15.8 | 13.9 (5.3) |
| Kenya Kakamega | 380 | 0.9 | 15.4 (7.5) | 13.0 | 17.0 (3.3) |
| Kenya Turkana | 418 | 1.6 | 20.0 (0.0) | 15.9 | 15.1 (4.7) |
| Kosovo | 2,674 | 54.3 | 15.5 (3.3) | 40.8 | 16.5 (2.7) |
| Kosovo Roma | 816 | 43.0 | 14.0 (3.6) | 27.2 | 16.2 (2.8) |
| Lebanon** | 2,047 | 4.1 | 17.1 (3.3) | ||
| Macedonia | 1,081 | 40.1 | 16.3 (2.3) | 44.4 | 16.3 (1.7) |
| Macedonia Roma | 371 | 40.9 | 14.1 (3.0) | 39.1 | 16.3 (2.8) |
| Madagascar | 1,278 | 13.4 | 15.6 (3.1) | 47.9 | 15.7 (3.2) |
| Moldova | 2,290 | 44.8 | 16.1 (3.0) | 89.4 | 15.9 (2.4) |
| Mongolia | 3,486 | 35.9 | 16.8 (2.9) | 63.1 | 18.1 (2.0) |
| Mongolia Khuv | 962 | 33.8 | 16.4 (3.0) | 55.2 | 18.1 (2.0) |
| Montenegro | 1,542 | 34.3 | 16.5 (2.4) | 58.6 | 16.5 (2.1) |
| Montenegro Roma | 699 | 26.6 | 14.5 (2.4) | 38.2 | 15.0 (2.2) |
| Nepal | 5,227 | 3.3 | 14.4 (4.3) | 14.2 | 13.8 (4.8) |
| Nepal West | 2,831 | 3.4 | 14.4 (3.5) | 9.2 | 12.8 (3.8) |
| Pakistan Punjab | 21,195 | 0.9 | 16.9 (4.2) | n/a | |
| Sao Tome | 2,089 | 9.4 | 17.9 (3.3) | 70.0 | 16.5 (2.6) |
| Tunisia | 3,322 | 5.1 | 17.5 (2.2) | 0.6 | 18.6 (1.6) |
| Ukraine | 2,513 | 48.1 | 16.2 (1.5) | 84.5 | 16.2 (1.5) |
n/a – no data available
For Lebanon the questions about alcohol consumption were asked, but none of the respondents reported any alcohol use.
Lifetime use of tobacco and alcohol:
In the multivariable models, accounting for all other risk factors, the odds of ever using tobacco and alcohol increased with age: 19% for tobacco use and 21.5% for alcohol use. Male youth were three times more likely than female youth to have used tobacco (OR = 3.206; 95% CI: 2.98, 3.45; p < 0.001), and almost twice as likely as female youth to have used alcohol (OR = 1.913; 95% CI: 1.78, 2.06; p < 0.001).
There were statistically significant differences in tobacco use between youth with primary education and youth with college or university education but all other education level comparisons were statistically insignificant. Youth with primary education were more likely to report tobacco use than youth with college or university education (OR = 1.268; 95% CI: 1.12, 1.44; p < 0.001). For alcohol, youth with primary or lower education (OR = 0.641; 95% CI: 0.57, 0.72; p < 0.001) and secondary school education (OR = 0.671; 95% CI: 0.62, 0.73; p < 0.001) were significantly less likely to have used alcohol compared to youth with higher education.
Married youth were significantly more likely to have used tobacco (OR = 1.124; 95% CI: 1.05, 1.21; p < 0.05) and alcohol (OR = 1.388; 95% CI: 1.28, 1.50; p < 0.001) than unmarried youth. Youth residing in rural areas were significantly less likely to have used tobacco (OR = 0.787; 95% CI: 0.73, 0.84; p < 0.001) and alcohol (OR = 0.907; 95% CI: 0.85, 0.97; p < 0.001) than youth in residing in urban areas. Socio-economic differences in tobacco and alcohol use also emerged: the odds of ever using tobacco and alcohol generally increased with wealth. A higher frequency of mass media exposure was positively associated with tobacco use (OR = 1.023; 95% CI: 1.01, 1.04; p < 0.001) and alcohol use (OR = 1.058; 95% CI: 1.04, 1.07; p < 0.001).
Age of onset for tobacco and alcohol use:
Controlling for all other risk factors in the multivariable analyses, we found that age of onset for both tobacco (β = −1.187; p < 0.001) and alcohol (β = −0.757; p < 0.001) was significantly higher for female than male youth. Age of onset for tobacco and alcohol use was lower among youth with primary or secondary education, in comparison to youth with a higher educational attainment. A similar pattern was observed for educational differences with regard to alcohol use. The age of onset for both tobacco use (β = 0.440; p < 0.05) and alcohol use (β = 0.624; p < 0.001) was higher among married youth than unmarried youth, and was not associated with household wealth. With regard to place of residence, the age of onset alcohol use was higher among rural than urban residents (β = 0.907; p < 0.05) but was not significantly different for tobacco use. Age of onset was not associated with frequency of mass media exposure.
Current use of tobacco and alcohol use
The pattern of the findings for current use of tobacco and alcohol use (not presented) mirrored findings on lifetime use of tobacco and alcohol. Age and increased educational attainment were associated with increased odds for current tobacco use, while male gender and rural residence were associated with lower odds for current tobacco use. For alcohol use, age, primary school attainment, and mass media exposure were associated with increased odds for current alcohol use, while secondary school attainment, being married, and poor household wealth were associated with lower odds for current alcohol use.
Interactive effects
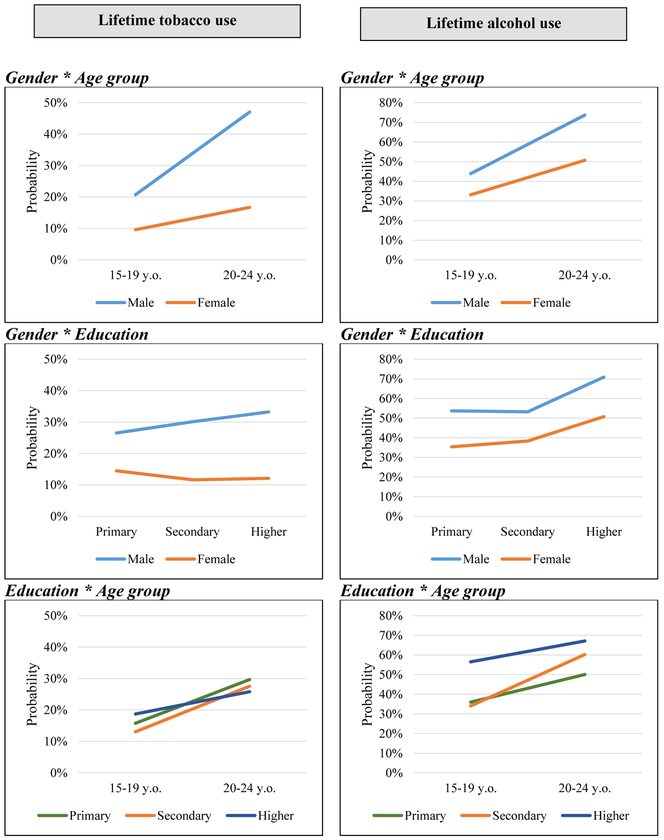
To address our third research question regarding potential age, gender and education interactive effects on tobacco and alcohol use outcomes, graphical plots of statistically significant findings are presented in Figures 1 and 2.
Figure 1.
Estimated probabilities for gender, age, and education interaction effects on lifetime tobacco and alcohol use
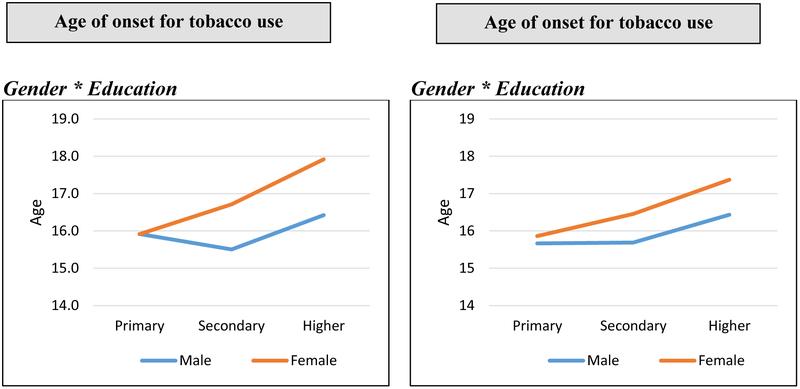
Figure 2.
Estimated marginal effects for gender and education interaction effects on age of onset for tobacco and alcohol use.
Lifetime tobacco and alcohol use:
For lifetime tobacco use, we found statistically significant interactive effects between age and gender, age and education, gender and education. For lifetime alcohol use, we found statistically significant gender and age effects, education and age effects as well as gender and education effects.
For both males and females, the predictive odds of lifetime tobacco and alcohol use increased with age although the gender gap was wider for tobacco use than alcohol use. The odds of lifetime tobacco use increased with educational attainment among males but declined with education among females. On the contrary, the odds of lifetime alcohol use increased with education for both males and females. Among 15 – 19 year olds, the odds of lifetime alcohol and tobacco were highest among youth with higher educational attainment and lowest among youth with secondary school education. However, this pattern was inverted among 20 – 24 year olds with the lowest odds of lifetime tobacco use observed among youth with higher education and the highest odds observed among youth with only primary education. The probabilities of lifetime alcohol use remained high among youth with higher education and low among youth with primary or lower education.
Age of onset for tobacco and alcohol use:
For age of onset for tobacco and alcohol use, we found marginally significant interaction effects for gender and education. Irrespective of the level of educational attainment, the age of onset for both tobacco and alcohol use remained higher among females compared to males. The age of onset for tobacco use was slightly lower among youth with secondary education than youth with primary or higher educational attainments. The age of onset for alcohol use was comparable for youth with primary and secondary school educational attainments.
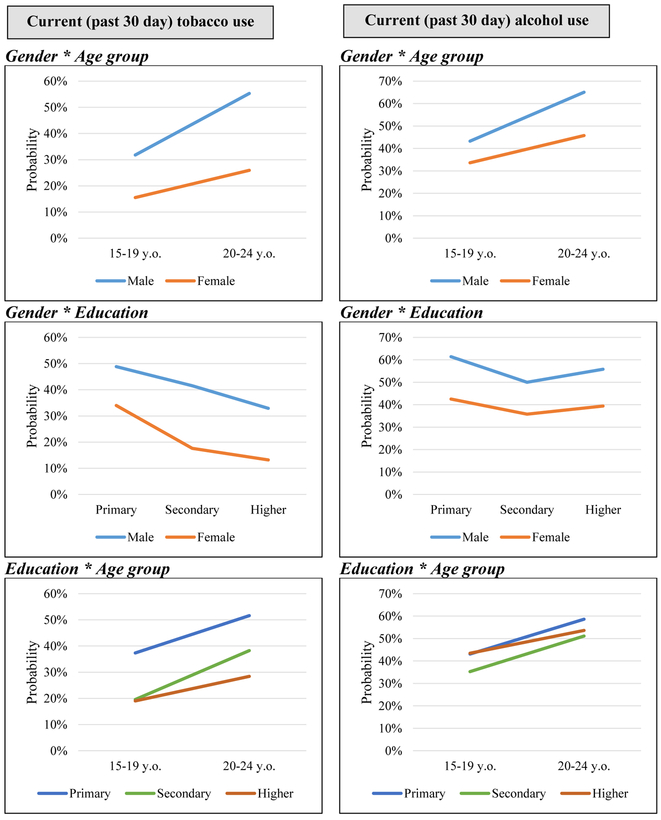
Current tobacco and alcohol use:
For current tobacco use, we found statistically significant interaction effects for gender and age. For current alcohol use, we found statistically significant age and gender effects, marginally significant gender and education effects, and statistically significant age and education effects.
The probability of current tobacco and alcohol use was higher among males than females, irrespective of age. For both males and females, the probability of current tobacco use declined with increased educational attainment. However, for alcohol, the probability of current alcohol use was lower among youth with secondary education, compared to youth with primary and higher educational attainment. Irrespective of age, the probability of current tobacco use was highest among youth with primary or less education and lowest among youth with higher education. Youth with secondary school education (irrespective of age) had the lowest probability for current alcohol use. Among 15 – 19 year olds, the probabilities for alcohol use among youth with primary or less education and youth with higher education were comparable. However, within the 20 – 24 age group, youth with primary education or less had the highest probability of current alcohol use.
Within country effects of micro-level factors on tobacco and alcohol use
Results from the multi-level logistic and linear regressions examining within-country effects of micro-level factors (Tables S1 – S4) were largely consistent with the pattern of findings from analyses on country level variations, with a few notable exceptions. In Macedonia, youth with primary or lower education had lower odds for lifetime tobacco use than youth with tertiary education, but in the Dominican Republic, Pakistan Punjab and Lebanon, youth with primary or lower education had higher odds for lifetime tobacco use than youth with tertiary education (Table S1). In Belarus, Bosnia and the Dominican Republic, youth with secondary education had higher odds for lifetime tobacco use than youth with tertiary education but the reverse was true for youth in Kosovo and Mongolia (Table S1). In the Dominican Republic, the odds for lifetime alcohol use were higher among youth with secondary education than youth with tertiary education (Table S2). Mass media exposure was associated with a higher age of onset for tobacco use in Kosovo and Ukraine but associated with a lower age of onset in the Dominican Republic (Table S3).
DISCUSSION
In LMICs, the burden of disease among young people attributable to substance use, especially tobacco and alcohol use is projected to increase (Charlson et al., 2014), but few studies have examined the prevalence and correlates of substance use among youth in LMICs. Understanding of the drivers of youth’s substance use behavior is necessary for developing effective prevention programs and policies. This paper makes a needed and unique contribution to our understanding of the structural and micro-level factors that influence alcohol and tobacco use among youth aged 15 – 24 years in LMICs. Similar with prior studies among younger adolescents (Bendtsen et al., 2014; Degenhardt et al., 2008; Moor et al., 2015; Page & Danielson, 2011), we found evidence of cross-national variation in tobacco and alcohol use: tobacco use was higher among youth in Europe compared to the Middle East and African regions but alcohol use is more generalized across the regions. The higher prevalence of tobacco use in European countries is well documented (CDC, 2016; Degenhardt et al., 2008; Karam et al., 2007). It has been attributed to contextual factors such as laws and regulations and socio-cultural norms related to alcohol and tobacco use (Anderson et al., 2009; Bendtsen et al., 2014; Bendtsen et al., 2013; Grube & Waiters, 2005).
The ubiquity of alcohol use across countries suggests that alcohol use is part of the normative adolescent experience in many countries, while the low prevalence of alcohol use in the Mediterranean region reflects the very restrictive socio-religious norms and country policies regarding alcohol use and access. Tobacco regulation policies vary globally (WHO, 2013). Restrictive regulations governing the advertising and sales of tobacco and alcohol to minors as well as financial disincentives such as tobacco excise taxes and price increases have been effective in reducing tobacco and alcohol consumption among adolescents in HICs (Chaloupka, Straif, & Leon, 2010; Ranson, Jha, Chaloupka, & Nguyen, 2002; WHO, 2015). In contrast to prior studies, we did not find support for the role of national wealth, income or income inequity on tobacco and alcohol use (Elgar et al., 2005; Pampel, 2007; Pfoertner et al., 2016; Rehm et al., 2009). This indicates that in LMICs, variation in these broad national assessments of wealth are unrelated to variation in tobacco and alcohol use among youth. This finding also suggests that in LMICs, mechanisms of teen tobacco and alcohol use pertain more to community and individual spheres. As such, interventions to address youth substance use should utilize a multi-prong approach, with structural, community and micro-level interventions.
In this study, frequency of mass media exposure was positively associated with lifetime and current alcohol and tobacco use (both lifetime and current use) but did not appear to influence the age of onset of tobacco and alcohol use. This finding is consistent with previous reports that mass media exposure, particularly exposure to tobacco/alcohol use marketing increases the risk of alcohol and tobacco use among young people (Anderson et al., 2009; Grube & Waiters, 2005; Wakefield et al., 2003). Today, young people live in media-rich contexts where they receive direct and indirect persuasive messages about substance use norms and outcome expectancies including subtle suggestions about the pros and cons of substance use. Despite the existing restrictions on marketing and sell of tobacco and alcohol to minors, there is an increase tobacco marketing to young people in LMICs (African Tobacco Control Alliance, 2016; Savell et al., 2015; WHO, 2013). For example, a recent multi-country report found that the number of tobacco outlets were almost three times higher in LMICs compared to HICs, and the number of tobacco advertisements was 81 times higher in LMICs compared to HICs (Savell et al., 2015). Efforts of intensified marketing of alcohol to young people in LMICs have also been documented (Babor, Robaina, & Jernigan, 2015; Jernigan & Babor, 2015; WHO, 2014).
The tobacco industry has deployed a multi-channel approach to promote tobacco use among young people in LMICs, especially to young girls and women (Savell et al., 2015; WHO, 2010, 2013). Such efforts include tobacco sales outlets around schools, posters and billboards, advertisements on structures or buildings, umbrellas, windows and doors of stores and their sidewalks, sales of single cigarettes, and display of non-tobacco products such as sweets and snacks together with cigarettes (African Tobacco Control Alliance, 2016). Taken together, these findings underscore the need for concerted efforts to increase surveillance and control the marketing of alcohol and tobacco to young people in LMICs. Additionally, there is a need to equip young people with media deconstruction skills, to desist persuasive messaging on tobacco and alcohol use.
Our findings on the effects of age and gender are consistent with the literature on substance use among young people (Johnston, O’malley, Miech, Bachman, & Schulenberg, 2017; Kessler et al., 2005). The greater prevalence of substance use among males has been attributed to gender role norms: men tend to have greater social power than women do and this is often expressed in form of restrictions on women’s behavior including prohibitions against women’s drinking and smoking (Brady & Randall, 1999; Huselid & Cooper, 1992; Wilsnack, Vogeltanz, Wilsnack, & Harris, 2000). However, there are sex differences in alcohol metabolism (i.e. women become intoxicated on smaller quantities of alcohol) which may increase women’s risk for alcohol use disorder (Becker & Hu, 2008; Brady & Randall, 1999). Women may have greater difficulties to quit smoking (Perkins, 2001; Wetter et al., 1999) and are at increased risk for smoking related diseases among women (Huxley & Woodward, 2011; Perkins, 2001; Peters, Huxley, & Woodward, 2013). Recent study reports have highlighted that diminishing gap between young girls and boys with regarding to smoking and use of non-cigarette tobacco products (Degenhardt et al., 2008; GYTS Collaborating Group, 2003; WHO, 2010), which has several implications for the expanding burden of chronic diseases and reproductive cancers in LMICs. Therefore, there is an increased need for gender considerations in alcohol and tobacco prevention and treatment programming (Amos, Greaves, Nichter, & Bloch, 2011).
Similar to prior studies, we found educational differences in alcohol and tobacco use: tobacco use was higher among high-school dropouts while alcohol use was higher among college students (Karam et al., 2007; Schulenberg et al., 2016; Slutske et al., 2004). Previous studies have reported higher levels of tobacco use among young people with lower levels of education attainment (Berg et al., 2011; Jamal et al., 2015; Staff et al., 2010). This has been attributed to the work stress and uncertainty associated with low occupational status, part-time and temporary work arrangements (Staff et al., 2010). Alcohol misuse among college students is a multi-dimensional, culturally embedded experience that could be attributed to: (1) exploratory behavior associated with new contexts and the search for novel experiences; (2) a conduit to new friendships, romantic and sexual relationships as well as social bonding; and (3) a coping strategy for the stress of experiencing multiple developmental transitions over a relatively short time period or difficulties negotiating new role transitions (Schulenberg & Maggs, 2002). On the other hand, youth with lower levels of educational attainment also have already joined the workforce and may limit their alcohol consumption to avoid interferences with their adult role responsibilities such as work and family (Staff et al., 2010).
The findings on the relationship between marital status and alcohol/tobacco use are not consistent with the current evidence on the role of the social role transitions on alcohol use among youth. In the United States, family role transitions such as marriage and parenthood have been associated with lower substance use among youth because they tend to reduce leisure time or to crowd out recreational activities that encourage substance use, provide norms and expectations against substance use and increase conformity to conventional adult social roles (Staff et al., 2010). Additionally, married youth may also be low on sensation seeking and high on religiosity, which further reduces their engagement in risk behaviors (Staff et al., 2010). However, our finding of higher alcohol and tobacco use among married youth is more consistent with the perspective that youth who married at a younger age may have self-selected into adult-like roles that are more compatible with alcohol use (Schulenberg & Maggs, 2002; Staff et al., 2010), or the alcohol and tobacco use could may serve a stress-relieving function of fulfilling these responsibilities (Kuntsche et al., 2007; Kuntsche et al., 2005).
The relationship between socio-economic status and alcohol/tobacco use among youth varies considerably in the literature: prior studies have reported both positive (Hanson & Chen, 2007; Huckle et al., 2010; Moor et al., 2015; Pförtner et al., 2015; Richter et al., 2006; Spijkerman et al., 2008) and negative associations (Dishion et al., 1999; Huckle et al., 2010; Moor et al., 2015; Pförtner et al., 2015). In our analyses, we did not find any association between socio-economic status and age of onset for alcohol and tobacco use among youth. Consistent with prior studies (Hanson & Chen, 2007; Huckle et al., 2010; Moor et al., 2015; Pförtner et al., 2015; Richter et al., 2006; Spijkerman et al., 2008), we found that youth living in more affluent households were more likely to report alcohol and tobacco use than their peers in less affluent households. The higher prevalence of substance use among youth living in more affluent households has been largely attributed to greater access to expendable income (Bellis et al., 2007; Hanson & Chen, 2007; Martin et al., 2009; Spijkerman et al., 2008), reduced parental supervision and enforcement of house rules regarding substance use, or youth that may feel safer experimenting with alcohol or tobacco (Bellis et al., 2007; Hanson & Chen, 2007; Martin et al., 2009; Spijkerman et al., 2008). Prior studies reporting lower rates of alcohol/tobacco use among youth from affluent households have highlighted the potential role of parental education and parenting styles: more affluent (and therefore more educated) parents may influence their children’s substance use risk by transmitting values and norms that discourage alcohol and tobacco use (Richter et al., 2006). On the other hand, the higher rates of alcohol and tobacco use among youth from low socio-economic backgrounds have been associated with depressive symptomatology, suggesting that tobacco and alcohol may be used to self-medicate (Luthar & Becker, 2002). Low socio-economic youth may also be more vulnerable to substance use because they experience greater pressure to smoke, perceive stronger social norms towards smoking from significant others (e.g. parents, peers), live in environments with greater exposure to alcohol and tobacco use and have less stringent enforcement of alcohol and tobacco use within their homes (De Vries, 1995). Taken together, these findings suggest that the nature of the relationship between socio-economic status and youth’s alcohol/tobacco use varies across contexts. However, parent-child communication on alcohol and tobacco use may play a pivotal role in preventing alcohol and tobacco use among young people, and should be promoted as a public health strategy.
CONCLUSIONS
This paper capitalizes on existing multi-national data to bridge the knowledge gap on the national- and individuallevel determinants of tobacco and alcohol use among youth in LMICs. The comparability in study design and data collection methods allows for comparison of substance use outcomes and correlates across countries. Our findings make a unique contribution on social determinants of alcohol and tobacco use among youth in LMICs; the findings highlight the role of educational attainment, mass media exposure and marital status.
However, this paper is not without limitations: (1) we utilize cross-sectional data so we cannot establish direct causation between the social factors and alcohol/tobacco use; (2) not all countries collected data on both males and females, and this variation limits generalization of gender findings across countries; (3) we rely on self-reported data that is vulnerable to measurement bias from social desirability: substance use among females is socially stigmatized so participants could have been less truthful in their responses, which could result in underestimation of the prevalence of alcohol and tobacco use especially among females thereby influencing the pattern of findings on gender differences in alcohol and tobacco use; and (4) our analyses include a limited set of potential drivers of tobacco and alcohol use; in particular, there is potential value in understanding the potential impact attitudinal and environmental factors on alcohol and tobacco use among youth in LMICs. As such, our findings should be interpreted within these constraints.
Nonetheless, the findings provide preliminary data on prevalence and national/individual factors associated with alcohol and tobacco use among youth; these findings could be of use for tobacco and alcohol prevention programming. Findings from a recent systematic review of substance use prevention and treatment interventions for young people indicate that the following structural interventions are effective at reducing substance use among young people: (1) bans on mass media advertising of substance use to reduce acceptability and normalization of substance use; (2) increased minimum age of purchase for alcohol and tobacco; (3) taxation and minimum pricing to reduce demand and use; and (4) restrictions on number and types of tobacco/alcohol sales outlets (Stockings et al., 2016). The evidence from this review also indicates that skills trainings rather than information provision is more effective at preventing substance use among young people (Stockings et al., 2016). Therefore, young people will greatly benefit from skills trainings that impact refusal skills to desist peer pressure and media deconstruction skills (Scull, Kupersmidt, & Erausquin, 2014; Stockings et al., 2016). While our findings indicate the males remain a higher risk for tobacco and alcohol use, the diminishing gender gap in tobacco and alcohol use among young people, coupled with reports of targeted marketing of tobacco to girls and women in LMICs (CDC, 2016; WHO, 2010), underscore the importance of incorporating gender consideration in alcohol and tobacco use prevention programs and policies. At a research level, there is a need to strengthen data collection across a range of contexts to allow better estimation of the prevalence and future burden of substance use among youth. These data collection efforts should also prioritize consistency and comparability of key design elements and variables to facilitate comparisons and understanding of key risk and protective factors of substance use across different contexts. Lastly, there is a need for longitudinal studies with internationally representative samples of youth to inform our understanding of life course variations in substance use in LMICs, particularly within the rapidly evolving the socio-ecological contexts.
Supplementary Material
Figure 3.
Estimated marginal means for current tobacco and alcohol use.
Table 3:
Multi-level models on country level predictors of tobacco and alcohol use among youth
| Tobacco use | Alcohol use | |||
|---|---|---|---|---|
| Ever use AORa |
Age of onset β coef (95% CI). |
Ever use AORa |
Age of onset β coef. |
|
| Intercept | 0.005 (0.002, 0.01)*** | 17.386 (16.7, 18.1) *** | 0.014 (0.004, 0.05)*** | 17.014 (16.43, 17.59)*** |
| Age | 1.190 (1.18, 1.20)*** | 1.215 (1.20, 1.23)*** | ||
| Maleb | 3.206 (2.98, 3.45)*** | −1.187 (−1.76, −0.61)*** | 1.913 (1.78, 2.06)*** | −0.757 (−1.08, −0.44)*** |
| Primary educationc | 1.268 (1.12, 1.44)*** | −1.496 (−2.06, −0.93)*** | 0.641 (0.57, 0.72)*** | −1.390 (−1.87, −0.92)*** |
| Secondary educationc | 1.047 (0.98, 1.12) | −1.117 (−1.40, −0.83)*** | 0.672 (0.62, 0.73)*** | −0.894 (−1.07, −0.72)*** |
| Currently marriedd | 1.124 (1.05, 1.21)** | 0.440 (0.15, 0.73) ** | 1.388 (1.28, 1.50*** | 0.624 (0.29, 0.95)*** |
| Rurale | 0.787 (0.73, 0.84)*** | −0.090 (−0.30, 0.12) | 0.907 (0.85, 0.97)** | −0.009 (−0.13, 0.11) |
| Household income poorestf | 0.824 (0.74, 0.92)*** | 0.154 (−0.04, 0.35) | 0.767 (0.69, 0.85)*** | 0.256 (0.03, 0.48)* |
| Household income poorerf | 0.819 (0.75, 0.89)*** | 0.158 (−0.09, 0.42) | 0.795 (0.72, 0.87)*** | 0.153 (−0.09, 0.40) |
| Household income middlef | 0.792 (0.73, 0.86)*** | 0.375 (0.07, 0.68)* | 0.822 (0.75, 0.89)*** | 0.243 (0.09, 0.40)** |
| Household income richerf | 0.844 (0.78, 0.92)*** | −0.020 (−0.12, 0.08) | 0.846 (0.78, 0.92)*** | 0.013 (−0.12, 0.14) |
| Frequency of exposure to mass media | 1.023 (1.01, 1.04)*** | 0.014 (−0.03, 0.06) | 1.058 (1.04, 1.07)*** | −0.013 (−0.04, 0.01) |
p < 0.05,
p < 0.01,
p<0.001
‘Never used’ is a reference category;
Reference group is females;
Reference group is no formal education;
Reference group is not currently married;
Reference group is urban;
Reference group richest
AOR – Adjusted Odds Ratios. β coef – Beta coefficients
Acknowledgements
Development of this manuscript was supported in part by research grants R01DA001411 (to R. Miech and L. Johnston) and R01DA016575 (to J. Schulenberg and L. Johnston) from the National Institute on Drug Abuse. The study sponsors had no role in the study design, collection, analysis or interpretation of the data, writing of the manuscript, or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the study sponsors.
Footnotes
Declaration of interest
The authors do not have any conflicts of interest to report.
Contributor Information
Massy Mutumba, Health Behavior and Biological Sciences, University of Michigan School of Nursing, Ann Arbor, Michigan 48109 USA, Tel: +1734-647-0323, Fax: +1734-936-5525, mmutumba@umich.edu.
John Schulenberg, Institute for Social Research and, Department of Psychology, Ann Arbor, MI 48106-1248, schulenberg@umich.edu.
REFERENCES
- African Tobacco Control Alliance. (2016). Big Tobacco, Tiny targets: Tobacco industry targets schools in Africa. Retrieved from Lomé, Togo: http://atca-africa.org/images/Regional-repport/ATCA-TIA-Regional-report.pdf
- Amos A, Greaves L, Nichter M, & Bloch M (2011). Women and tobacco: a call for including gender in tobacco control research, policy and practice. Tobacco Control, tobaccocontrol-2011–050280. [DOI] [PubMed] [Google Scholar]
- Anderson P, De Bruijn A, Angus K, Gordon R, & Hastings G (2009). Impact of alcohol advertising and media exposure on adolescent alcohol use: a systematic review of longitudinal studies. Alcohol and alcoholism, 44(3), 229–243. [DOI] [PubMed] [Google Scholar]
- Babor TF, Robaina K, & Jernigan D (2015). The influence of industry actions on the availability of alcoholic beverages in the African region. Addiction, 110(4), 561–571. [DOI] [PubMed] [Google Scholar]
- Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, Lincoln P, . . . Nishtar S. (2011). UN high-level meeting on non-communicable diseases: addressing four questions. The Lancet, 378(9789), 449–455. [DOI] [PubMed] [Google Scholar]
- Becker JB, & Hu M (2008). Sex differences in drug abuse. Frontiers in neuroendocrinology, 29(1), 36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis MA, Hughes K, Morleo M, Tocque K, Hughes S, Allen T, . . . Fe-Rodriguez E. (2007). Predictors of risky alcohol consumption in schoolchildren and their implications for preventing alcohol-related harm. Substance abuse treatment, prevention, and policy, 2(1), 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendtsen P, Damsgaard MT, Huckle T, Casswell S, Kuntsche E, Arnold P, . . . Simons‐Morton B. (2014). Adolescent alcohol use: a reflection of national drinking patterns and policy? Addiction, 109(11), 1857–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendtsen P, Damsgaard MT, Tolstrup JS, Ersbøll AK, & Holstein BE (2013). Adolescent alcohol use reflects community-level alcohol consumption irrespective of parental drinking. Journal of Adolescent Health, 53(3), 368–373. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Ling PM, Hayes RB, Berg E, Nollen N, Nehl E, . . . Ahluwalia JS. (2011). Smoking frequency among current college student smokers: distinguishing characteristics and factors related to readiness to quit smoking. Health education research, 27(1), 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, & Randall CL (1999). Gender differences in substance use disorders. Psychiatric Clinics of North America, 22(2), 241–252. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, Schulenberg JE, Hingson R, Swartzwelder S, . . . Sher K. (2008). A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics, 121(Supplement 4), S290–S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control: CDC. (2016). Global Youth Tobacco Survey: Part III. Centers for Disease Control; (Ed.). Atlanta, USA: Retrieved from https://www.cdc.gov/tobacco/global/gtss/tobacco_atlas/pdfs/part3.pdf [Google Scholar]
- Chaloupka FJ, Straif K, & Leon ME (2010). Effectiveness of tax and price policies in tobacco control. Tobacco Control, 2010.039982. [DOI] [PubMed] [Google Scholar]
- Charlson FJ, Diminic S, Lund C, Degenhardt L, & Whiteford HA (2014). Mental and substance use disorders in sub-Saharan Africa: predictions of epidemiological changes and mental health workforce requirements for the next 40 years. PLoS One, 9(10), e110208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Unger JB, Palmer P, Weiner MD, Johnson CA, Wong MM, & Austin G (2002). Prior cigarette smoking initiation predicting current alcohol use: Evidence for a gateway drug effect among California adolescents from eleven ethnic groups. Addictive behaviors, 27(5), 799–817. [DOI] [PubMed] [Google Scholar]
- Choudhry V, Agardh A, Stafstrom M, & Ostergren PO (2014). Patterns of alcohol consumption and risky sexual behavior: a cross-sectional study among Ugandan university students. BMC Public Health, 14, 128. doi: 10.1186/1471-2458-14-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vries H (1995). Socio-economic differences in smoking: Dutch adolescents’ beliefs and behaviour. Social science & medicine, 41(3), 419–424. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Chiu W-T, Sampson N, Kessler RC, Anthony JC, Angermeyer M, . . . Huang Y. (2008). Toward a global view of alcohol, tobacco, cannabis, and cocaine use: findings from the WHO World Mental Health Surveys. PLoS Med, 5(7), e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNapoli PP (2009). Early initiation of tobacco use in adolescent girls: key sociostructural influences. Applied Nursing Research, 22(2), 126–132. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Capaldi DM, & Yoerger K (1999). Middle childhood antecedents to progressions in male adolescent substance use: An ecological analysis of risk and protection. Journal of Adolescent Research, 14(2), 175–205. [Google Scholar]
- Dodge K, Malone P, Lansford J, Miller S, Pettit G, & Bates J (2009). A dynamic cascade model of the development of substance-use onset. Monogr Soc Res Child Dev, 74(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar FJ, Roberts C, Parry-Langdon N, & Boyce W (2005). Income inequality and alcohol use: a multilevel analysis of drinking and drunkenness in adolescents in 34 countries. The European Journal of Public Health, 15(3), 245–250. [DOI] [PubMed] [Google Scholar]
- Ezzati M, & Riboli E (2013). Behavioral and dietary risk factors for noncommunicable diseases. New England Journal of Medicine, 369(10), 954–964. [DOI] [PubMed] [Google Scholar]
- Global Youth Tobacco Survey Collaborating Group. (2003). Differences in worldwide tobacco use by gender: findings from the Global Youth Tobacco Survey. The Journal of school health, 73(6), 207. [DOI] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, . . . Mathers CD. (2011). Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet, 377(9783), 2093–2102. [DOI] [PubMed] [Google Scholar]
- Grube JW, & Waiters E (2005). Alcohol in the media: content and effects on drinking beliefs and behaviors among youth. Adolescent medicine clinics, 16(2), 327. [DOI] [PubMed] [Google Scholar]
- Hanson MD, & Chen E (2007). Socioeconomic status and substance use behaviors in adolescents: The role of family resources versus family social status. Journal of health Psychology, 12(1), 32–35. [DOI] [PubMed] [Google Scholar]
- Huckle T, You RQ, & Casswell S (2010). Socio‐economic status predicts drinking patterns but not alcohol‐related consequences independently. Addiction, 105(7), 1192–1202. [DOI] [PubMed] [Google Scholar]
- Huselid RF, & Cooper ML (1992). Gender roles as mediators of sex differences in adolescent alcohol use and abuse. Journal of Health and Social Behavior, 348–362. [PubMed] [Google Scholar]
- Huxley RR, & Woodward M (2011). Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. The Lancet, 378(9799), 1297–1305. [DOI] [PubMed] [Google Scholar]
- Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, . . . King BA. (2015). Current cigarette smoking among adults - United States, 2005–2014. MMWR Morb Mortal Wkly Rep, 64(44), 1233–1240. doi: 10.15585/mmwr.mm6444a2 [DOI] [PubMed] [Google Scholar]
- Jernigan DH, & Babor TF (2015). The concentration of the global alcohol industry and its penetration in the African region. Addiction, 110(4), 551–560. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’malley PM, Miech R, Bachman JG, & Schulenberg JE (2017). Monitoring the Future national survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use. . Institute for Social Research. [Google Scholar]
- Karam E, Kypri K, & Salamoun M (2007). Alcohol use among college students: an international perspective. Current opinion in psychiatry, 20(3), 213–221. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry, 62(6), 593–602. [DOI] [PubMed] [Google Scholar]
- Kuipers MA, de Korte R, Soto VE, Richter M, Moor I, Rimpelä AH, . . . Lorant V. (2016). School smoking policies and educational inequalities in smoking behaviour of adolescents aged 14–17 years in Europe. Journal of epidemiology and community health, 70(2), 132–139. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, & Gmel G (2007). Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. Journal of Studies on Alcohol and Drugs, 68(1), 76–85. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical psychology review, 25(7), 841–861. [DOI] [PubMed] [Google Scholar]
- Luk JW, Wang J, & Simons-Morton BG (2010). Bullying victimization and substance use among US adolescents: Mediation by depression. Prevention Science, 11(4), 355–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, & Becker BE (2002). Privileged but pressured? A study of affluent youth. Child development, 73(5), 1593–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin BA, McCoy TP, Champion H, Parries MT, DuRant RH, Mitra A, & Rhodes SD (2009). The role of monthly spending money in college student drinking behaviors and their consequences. Journal of American College Health, 57(6), 587–596. [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and psychopathology, 22(3), 491. [DOI] [PubMed] [Google Scholar]
- Maziak W (2011). The global epidemic of waterpipe smoking. Addictive behaviors, 36(1), 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mbulaiteye SM, Ruberantwari A, Nakiyingi JS, Carpenter LM, Kamali A, & Whitworth JA (2000). Alcohol and HIV: a study among sexually active adults in rural southwest Uganda. Int J Epidemiol, 29(5), 911–915. [DOI] [PubMed] [Google Scholar]
- Mehra D, Agardh A, Stafstrom M, & Ostergren PO (2014). Is drinking alcohol associated with sexual coercion among Ugandan university students?: a cross-sectional study. Reprod Health, 11(1), 7. doi: 10.1186/1742-4755-11-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor I, Rathmann K, Lenzi M, Pförtner T-K, Nagelhout GE, de Looze M, . . . Kunst AE. (2015). Socioeconomic inequalities in adolescent smoking across 35 countries: a multilevel analysis of the role of family, school and peers. The European Journal of Public Health, cku244. [DOI] [PubMed] [Google Scholar]
- Murray CJ, & Lopez AD (2013). Measuring the global burden of disease. New England Journal of Medicine, 369(5), 448–457. [DOI] [PubMed] [Google Scholar]
- National Research Council. (2015). Investing in the health and well-being of young adults: National Academies Press. [PubMed] [Google Scholar]
- O’Keeffe GS, & Clarke-Pearson K (2011). The impact of social media on children, adolescents, and families. Pediatrics, 127(4), 800–804. [DOI] [PubMed] [Google Scholar]
- Page RM, & Danielson M (2011). Multi-country, cross-national comparison of youth tobacco use: findings from global school-based health surveys. Addictive behaviors, 36(5), 470–478. [DOI] [PubMed] [Google Scholar]
- Pampel F (2007). National income, inequality and global patterns of cigarette use. Social Forces, 86(2), 445–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Cappa C, Currie D, Riley L, Gore F, . . . Sangowawa AO. (2012). Health of the world’s adolescents: a synthesis of internationally comparable data. The Lancet, 379(9826), 1665–1675. [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, . . . Mathers CD. (2009). Global patterns of mortality in young people: a systematic analysis of population health data. The Lancet, 374(9693), 881–892. [DOI] [PubMed] [Google Scholar]
- Perkins KA (2001). Smoking cessation in women. CNS drugs, 15(5), 391–411. [DOI] [PubMed] [Google Scholar]
- Peters SA, Huxley RR, & Woodward M (2013). Smoking as a risk factor for stroke in women compared with men. Stroke, 44(10), 2821–2828. [DOI] [PubMed] [Google Scholar]
- Pfoertner T-K, Rathmann K, Moor I, Kunst AE, & Richter M (2016). Social inequalities in adolescent smoking: A cross-national perspective of the role of individual and macro-structural factors. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz, 59(2), 206–216. [DOI] [PubMed] [Google Scholar]
- Pförtner TK, Moor I, Rathmann K, Hublet A, Molcho M, Kunst AE, & Richter M (2015). The association between family affluence and smoking among 15‐year‐old adolescents in 33 European countries, Israel and Canada: the role of national wealth. Addiction, 110(1), 162–173. [DOI] [PubMed] [Google Scholar]
- Ranson MK, Jha P, Chaloupka FJ, & Nguyen SN (2002). Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine & Tobacco Research, 4(3), 311–319. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, & Patra J (2009). Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet, 373(9682), 2223–2233. [DOI] [PubMed] [Google Scholar]
- Richter M, Leppin A, & Gabhainn SN (2006). The relationship between parental socio-economic status and episodes of drunkenness among adolescents: findings from a cross-national survey. BMC Public Health, 6(1), 289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savell E, Gilmore AB, Sims M, Mony PK, Koon T, Yusoff K, . . . Calik K. (2015). The environmental profile of a community’s health: a cross-sectional study on tobacco marketing in 16 countries. Bulletin of the World Health Organization, 93, 851–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore S-J, Dick B, Ezeh AC, & Patton GC (2012). Adolescence: a foundation for future health. The Lancet, 379(9826), 1630–1640. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, & Patrick ME (2017). Monitoring the Future national survey results on drug use, 1975–2016: Volume II, college students and adults ages 19–55. [Google Scholar]
- Schulenberg JE, & Maggs JL (2002). A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol, Supplement(14), 54–70. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Maslowsky J, Patrick ME, & Martz ME (2016). Substance use in the context of adolescent development In Brown SA & Zucker RA (Eds.), The Oxford Handbook of Adolescent Substance Abuse. New York: Oxford University Press. [Google Scholar]
- Schulenberg JE, Sameroff AJ, & Cicchetti D (2004). The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and psychopathology, 16(04), 799–806. [DOI] [PubMed] [Google Scholar]
- Scull TM, Kupersmidt JB, & Erausquin JT (2014). The impact of media-related cognitions on children’s substance use outcomes in the context of parental and peer substance use. Journal of youth and adolescence, 43(5), 717–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuper PA, Joharchi N, Irving H, & Rehm J (2009). Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav, 13(6), 1021–1036. doi: 10.1007/s10461-009-9589-z [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE Jr, Molina BS, Coxe S, Kipp H, Gnagy EM, . . . Lahey BB (2014). The role of early childhood ADHD and subsequent CD in the initiation and escalation of adolescent cigarette, alcohol, and marijuana use. Journal of abnormal psychology, 123(2), 362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons-Morton BG, & Farhat T (2010). Recent findings on peer group influences on adolescent smoking. The journal of primary prevention, 31(4), 191–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS, Hunt-Carter EE, Nabors-Oberg RE, Sher KJ, Bucholz KK, Madden PA, . . . Heath AC (2004). Do college students drink more than their non-college-attending peers? Evidence from a population-based longitudinal female twin study. Journal of abnormal psychology, 113(4), 530. [DOI] [PubMed] [Google Scholar]
- Snedker KA, Herting JR, & Walton E (2009). Contextual effects and adolescent substance use: Exploring the role of neighborhoods. Social Science Quarterly, 90(5), 1272–1297. [Google Scholar]
- Spijkerman R, van den Eijnden RJ, & Huiberts A (2008). Socioeconomic differences in alcohol-specific parenting practices and adolescents’ drinking patterns. European addiction research, 14(1), 26–37. [DOI] [PubMed] [Google Scholar]
- Stacy AW, Zogg JB, Unger JB, & Dent CW (2004). Exposure to televised alcohol ads and subsequent adolescent alcohol use. American journal of health behavior, 28(6), 498–509. [DOI] [PubMed] [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL, & Johnston LD (2010). Substance use changes and social role transitions: Proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Development and psychopathology, 22(04), 917–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockings E, Hall WD, Lynskey M, Morley KI, Reavley N, Strang J, . . . Degenhardt L (2016). Prevention, early intervention, harm reduction, and treatment of substance use in young people. The Lancet Psychiatry, 3(3), 280–296. [DOI] [PubMed] [Google Scholar]
- Thrul J, Lipperman-Kreda S, Grube JW, & Friend KB (2014). Community-level adult daily smoking prevalence moderates the association between adolescents’ cigarette smoking and perceived smoking by friends. Journal of youth and adolescence, 43(9), 1527–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torabi MR, Bailey WJ, & Majd‐Jabbari M (1993). Cigarette smoking as a predictor of alcohol and other drug use by children and adolescents: evidence of the “gateway drug effect”. Journal of school health, 63(7), 302–306. [DOI] [PubMed] [Google Scholar]
- United Nations. (2016). Sustainable Development Goals: 17 goals to transform our world. Retrieved from http://www.un.org/sustainabledevelopment/
- Wakefield M, Flay B, Nichter M, & Giovino G (2003). Role of the media in influencing trajectories of youth smoking. Addiction, 98(s1), 79–103. [DOI] [PubMed] [Google Scholar]
- Warren CW, Jones NR, Eriksen MP, Asma S, & group, G. T. S. S. c. (2006). Patterns of global tobacco use in young people and implications for future chronic disease burden in adults. The Lancet, 367(9512), 749–753. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, & Baker TB (1999). Gender differences in smoking cessation. Journal of Consulting and Clinical Psychology, 67(4), 555. [DOI] [PubMed] [Google Scholar]
- Wilsnack RW, Vogeltanz ND, Wilsnack SC, & Harris TR (2000). Gender differences in alcohol consumption and adverse drinking consequences: cross‐cultural patterns. Addiction, 95(2), 251–265. [DOI] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, & Olsen Y (2008). The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug and alcohol dependence, 92(1), 173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, WHO. (2010). Gender, women, and the tobacco epidemic: World Health Organization. Retrieved from http://www.who.int/tobacco/publications/gender/women_tob_epidemic/en/
- World Health Organization, WHO. (2013). WHO report on the global tobacco epidemic, 2013: enforcing bans on tobacco advertising, promotion and sponsorship: World Health Organization, Geneva: Retrieved from http://www.who.int/tobacco/global_report/2013/en/ [Google Scholar]
- World Health Organization. (2014). Global status report on alcohol and health, 2014. World Health Organization, Geneva: Retrived from http://www.who.int/substance_abuse/publications/global_alcohol_report/en/ [Google Scholar]
- World Health Organization. (2015). WHO report on the global tobacco epidemic, 2015: Raising taxes on tobacco. Retrieved from http://apps.who.int/iris/bitstream/handle/10665/178574/9789240694606_eng.pdf?sequence=1
- World Health Organization. (2016a). Psychoactive substance use among adolescents in the WHO African region: prevalence of current drinking. Retrieved from Geneva: http://www.who.int/chp/gshs/A_PrevalenceCurrentDrinking_AFRO.pdf?ua=1
- World Health Organization. (2016b). Psychoactive substance use among adolescents in the WHO region of the Americas: prevalence of current drinking. Retrieved from Geneva: http://www.who.int/chp/gshs/A_PrevalenceCurrentDrinking_AMRO.pdf?ua=1
- World Health Organization Office for Africa. (2014). Monitoring Alcohol Marketing in Africa: Findings from Kenya, Malawi, Namibia and Zambia. Retrieved from Brazaville, Congo: http://eucam.info/wp-content/uploads/2017/02/MAMPA-2012-final.pdf
- Zablotska IB, Gray RH, Koenig MA, Serwadda D, Nalugoda F, Kigozi G, . . . Wawer M. (2009). Alcohol use, intimate partner violence, sexual coercion and HIV among women aged 15–24 in Rakai, Uganda. AIDS Behav, 13(2), 225–233. doi: 10.1007/s10461-007-9333-5 [DOI] [PubMed] [Google Scholar]
- Zablotska IB, Gray RH, Serwadda D, Nalugoda F, Kigozi G, Sewankambo N, . . . Wawer M. (2006). Alcohol use before sex and HIV acquisition: a longitudinal study in Rakai, Uganda. AIDS, 20(8), 1191–1196. doi: 10.1097/01.aids.0000226960.25589.72 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.