Abstract
In recent years, an increasing research effort has been directed toward remediation of single-sided deafness. Contralateral routing of signal (CROS) is the longest standing rehabilitation solution for individuals with single-sided deafness. The primary goal of CROS technology is to transfer the signal received at the deaf ear to the better hearing ear, thereby reducing the impact of the acoustic head-shadow. This allows for individuals with single-sided deafness to regain access to sounds located at the deaf ear. The hearing deficits associated with single-sided deafness are often debilitating. While surgical management of single-sided deafness is on the rise, CROS hearing aids offer a nonsurgical option to compensate for some of the deficits that occur when a listener is limited to a single ear. Limitations of early CROS devices resulted in poor adoption and acceptance in those with single-sided deafness. Following significant advances in both design and technology, the acceptance of CROS devices has increased in recent years. This paper reviews relevant literature in CROS application for the management of single-sided deafness. Technological advances, benefits, limitations, and clinical considerations are also reviewed in this article.
Keywords: CROS, contralateral routing of signal, single-sided deafness, SSD, unilateral hearing loss, hearing aid
Introduction
Vestibular schwannomas most often arise in the internal auditory canal, making unilateral hearing loss the most common initial pathological feature. 1 2 The associated hearing loss is often progressive in nature as a result of disease or treatment, leading to single-sided deafness (SSD) or severe asymmetrical sensorineural hearing loss in many patients. The concomitant deficits of SSD are a common source of quality of life reduction in patients with vestibular schwannoma. 3 Individuals with SSD experience significant deficits in spatial hearing. When compared with normal hearers, individuals with SSD suffer from reduced sound awareness, difficulty with speech perception in noisy or reverberant environments, inability to localize auditory events in azimuth, and increased effort with listening. 4 5 6 7 These impairments occur due to the loss of auditory cues provided through binaural hearing. The integration of acoustic information from both ears is critical for processing of auditory signals. The auditory input received at each ear is characterized by marginal differences that are analyzed in the brainstem, giving rise to spatial hearing.
In binaural hearing, the ear closest to the sound source receives the signal earlier and at a higher intensity. The differences in these timing and level cues for a sound arriving at two ears are critical for processing of complex auditory signals, such as sound source localization and speech perception in noise. Low frequency signals have long wavelengths allowing them to travel around the head. As such interaural timing differences are greatest for signals below 1,000 Hz, while interaural level differences are more significant for high frequencies. 8 High frequency signals are characterized by shorter wavelengths and, as such, are obstructed by the head. The acoustic head-shadow ( Fig. 1A ) is a physical phenomenon that serves to benefit binaural listeners by adding the ear with the more favorable signal to noise ratio when listening in spatially separated speech and noise. This filtering of the auditory signal based on binaural hearing cues also allows for suppression of unwanted signals, thereby improving the signal to noise ratio. Likewise, depending on the frequency characteristics and the source location, the interaction of the acoustic sound wave with the torso, head, and pinna provides important temporal, spectral, and intensity information. Binaural listeners are able to take advantage of these frequency dependent cues to perform complex auditory tasks, such as the perception of speech in competing noise and localization of acoustic signals.
Fig. 1.
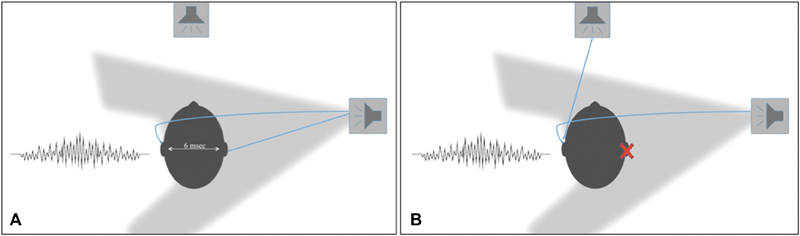
The acoustic head-shadow is demonstrated for binaural ( A ) and monaural ( B ) listeners. The interaural time are represented for signals at 0 degrees azimuth and lateralized 90 degrees to the right of the listener. In ( B ) the negative impact of the acoustic head-shadow is demonstrated for monaural listeners when competing noise is directed at the better hearing ear.
The Monaural Listening Condition
Individuals with SSD become monaural listeners, thereby losing access to the essential interaural auditory cues required for processing of complex acoustic signals. In individuals with SSD, all sounds arrive to the nonimpaired ear at the same time and level regardless of the location of the sound ( Fig. 1B ). This is further complicated by the head-shadow effect where the head acts as an acoustic barrier to sound as it travels from one side of the head to the other. Where the acoustic head-shadow benefits binaural listeners, it often results in significant deficits in speech understanding for monaural listeners. In individuals with SSD, the barrier created by the head for signals located at our about the impaired ear, results in an attenuation of the sound at the better hearing ear. The head-shadowing that occurs is most significant for high frequency signals 8 negatively impacting speech perception. The consequence of this is greater in noise, particularly when the noise is masking the better hearing ear ( Fig. 1B ). In the monaural listening condition, the brain can no longer use the different signal to noise ratios at the two ears as the sound is no longer spatially separated. The result of this is an inability of the SSD listener to separate speech from competing noise, even at low noise levels.
For these reasons, individuals with SSD are subject to significant hearing disability and handicap despite one normally functioning ear. 9 10 11 12 The negative effects of SSD are not simply auditory in nature. The social and emotional consequences have been well demonstrated throughout the literature, 7 13 14 with reports suggesting a handicap that exceeds that which is observed in bilateral hearing loss. 10 Effective processing of auditory signals is fundamental to even the most basic of communication needs. The spatial hearing deficits experienced by the SSD listener undeniably contribute to reduction in quality of life and increased handicap and disability. Individuals with SSD report that difficulties specific to communicating in noise have both social and vocational consequences which may ultimately lead to embarrassment and depression. 7 15 Strategies to combat this may include adapting or positioning to allow for the talker to be located at the better hearing ear; although this is not always achievable, particularly in multitalker situations or meetings. Further, the constant effort applied by the listener to adjust to the listening environment is fatiguing, and ultimately unsustainable for many listeners.
Contralateral Routing of Signal
Reducing the negative effects of the acoustic head-shadow in individuals with SSD may serve to mitigate some of the issues associated with monaural listening. This can be achieved by rerouting the acoustic signal from the impaired (deaf) ear to the normal hearing ear for processing. Contralateral routing of signal (CROS) hearing aids are a nonsurgical management option consisting of a hearing aid worn on the impaired ear containing a microphone and transmitter. This hearing aid transmits the acoustical signal to a receiver in a hearing aid worn on the better hearing ear. In the case of patients who have contralateral hearing loss, the hearing aid on the better hearing ear can also be used to provide amplification in addition to the CROS input. This configuration, termed BiCROS, is typically reserved for those individuals who have mild to moderate aidable hearing loss in the contralateral (better hearing) ear.
Harford and Barry 16 first introduced the CROS hearing aid in 1965. Studies using CROS hearing aids demonstrated that minimizing the acoustic head-shadow could significantly improve listening in noise ability in monaural listeners. 16 Despite this benefit, adoption and acceptance rates of CROS hearing aids were low in the SSD population. Initial CROS systems relied on wired transmission of the signal from the impaired ear to the normal ear, and were coupled to the ear with an ear mold. In addition to the unfavorable aesthetics of the wired CROS systems, the use of an ear mold occluded the ear, thereby causing a significant disruption of ear canal acoustics in the better hearing ear. It has been shown that individuals with SSD become reliant on monaural level and spectral cues, and may even use this information to adapt to improve their ability to localize sound. 17 18 19 In addition to changing the natural acoustics of the ear canal, the ear mold required in initial CROS systems reduced audibility in the better hearing ear. These limitations served as barriers to adoption and acceptance of early CROS devices, as those with SSD are highly dependent on access to sound in the only hearing ear.
Wireless CROS devices were later introduced, which served to improve the cosmetics of CROS hearing aids, but lacked in sound quality. These initial wireless CROS hearing aids relied on radio frequency transmission of the signal which was subject to electromagnetic interferences, distortion, and timing delays. 20 Limited acceptance of CROS hearing aids at this time are largely attributed to complaints of occlusion in the better ear, poor sound quality, and discomfort. 20 Additional limitations included aesthetics, size, and poor battery life. Despite some improvements, the remaining technological limitations failed to increase the acceptance of CROS by individuals with SSD.
In recent years, CROS hearing aid systems have undergone significant advances, addressing many of the early acoustic limitations associated with CROS and BiCROS hearing aids. Improvements in hearing aid technology and design have allowed for seamless between ear signal transmissions. Current wireless streaming between hearing devices allows the signal from the impaired ear to be transmitted to the better hearing ear with no audible delays and virtually no interference. In addition to this, microphone technology and signal-processing advances have allowed for an improved acoustic experience. 21 Environmental recognition is now possible through advanced algorithms, resulting in better noise reduction. 22 Directional microphones are now standard in most hearing aid systems and automatic adaptive directionality allows for real time beam forming to improve the signal to noise ratio for listeners. 23
Improvements in hearing aid design have also played an important role in increasing user comfort and reducing the stigma associated with hearing aids. 24 Reduction in the size of hearing aids has led to a marked improvement in cosmesis. Arguably, one of the most influential advances is the development of open fit hearing aids. 25 Early CROS systems relied on the use of an earmold to not only deliver the sound transmitted from the impaired ear but also to retain the hearing aid in the ear. Current CROS systems use an open fit where a thin tube with a small dome is placed in the ear canal minimizing the obstruction of the natural acoustics of the ear ( Fig. 2 ). For most listeners with normal hearing in the contralateral ear, this will remove the occlusion effect as it allows for sound to enter the normal hearing ear naturally and with minimal obstruction. 26 Kiessling and colleagues 26 measured the occlusion effect in 19 listeners with normal hearing below 1,500 Hz and found a mean reduction of 12 dB in occlusion with use of open fit domes when compared with traditional venting. Not only was this effect significant but mean occlusion in dB was comparable to the natural open ear canal, 23 suggesting an absence of occlusion. The combination of these improvements in hearing aid technology over the past several years have led to an increase in adoption and acceptance of CROS 27 28 and BiCROS 29 devices.
Fig. 2.
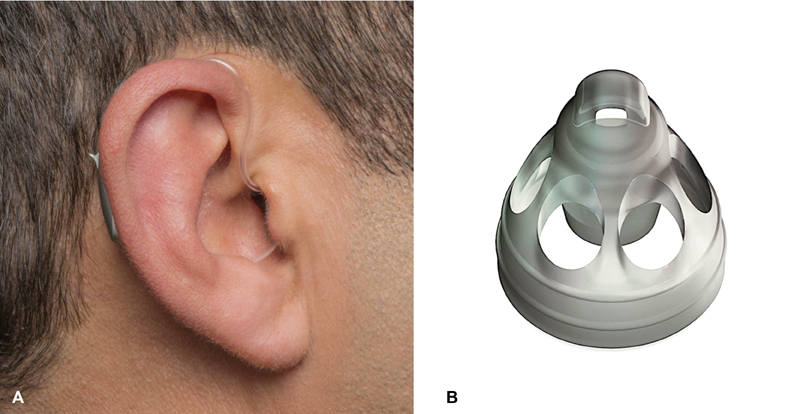
The illustrations show current open fit CROS hearing aid configurations. Here, the hearing aid processor/transmitter is behind the pinna and the signal is delivered via a small thin tube ( A ) with an open dome ( B ) allowing for minimal obstruction of the natural ear canal acoustics (Images courtesy to Phonak, LLC, with permission). CROS, contralateral routing of signal.
Benefits of CROS Amplification
The primary advantage of rerouting of the acoustic signal from the impaired ear to the better hearing ear is the ability to regain access to sound on that side. Sound awareness for deaf ear listening allows for the listener to be engaged regardless of the location of the speaker, a critical component of daily communication. Situational listening, such as holding a conversation while driving or while walking are examples of challenges often faced by individuals with SSD. The location of the speaker combined with competing noise in these situations results in an inability to consistently and effectively access speech at the deaf ear. The ability of CROS devices to reduce the negative effects of the acoustic head-shadow have been well established. 16 27 30 The primary benefit of this is the ability to improve speech perception in noise for speech directed at the poorer hearing ear. 16 27 30 These studies have shown that rerouting is successful in improving the signal-to-noise ratio for sounds directed to the deaf ear in noisy environments. Early studies suggested CROS hearing aids offered limited benefit compared with surgical rerouting solutions, such as osseointegrated bone conduction implants. 31 32 33 34 Recent studies have found no significant differences in objective or subjective outcomes with new wireless CROS technology compared with osseointegrated bone conduction implants. 27 28 35 The adoption and acceptance of current CROS technology has not only increased but seems to be comparable to that of surgical rerouting solutions. 28
Other benefits of CROS hearing aids include the design and ease of use. In 2012, 24 a survey of nearly 4,000 hearing aid candidates found that eliminating the visibility of the hearing aid would increase the likelihood of adopting hearing aids by 29 to 38%. Along these lines, an earlier study by the same group found that 48% of individuals with hearing loss who have not adopted hearing aids attribute this to the stigma associated with hearing aid use. 36 The improvement in aesthetics, particularly small and discreet housing of current wireless CROS and BiCROS hearing aids, has undoubtedly impacted acceptance of this solution. Additionally, because these devices by in large serve primarily to reroute the signal from the deaf ear to the better hearing ear, minimal management is required. In the case of true SSD, where no contralateral hearing loss is present, CROS devices do not require sophisticated programming or fitting strategies. Because the signal is typically being routed to a normal hearing ear with a normally functioning inner ear organ, benefits are immediately measureable. As such, adaptation to CROS hearing aids is rapid, with many users able to report on subjective benefit immediately. This allows for CROS hearing aids to be fit quickly with minimal adjustments. Furthermore, such solutions do not require the long-term management typically associated with surgical solutions. 37 38 39 40 Given their relative low cost and noninvasive nature, CROS hearing aids should be the first option considered in management of SSD.
Limitations of CROS Amplification
While CROS input allows for audibility from both sides of the head, the information is still processed through a monaural auditory system. The biggest limitation of CROS and BiCROS solutions is that binaural hearing is not restored, thereby leaving tasks that require binaural input fundamentally impaired. CROS and BiCROS hearing aids allow for access to sound from the impaired side and offer improved audibility. These devices cannot, however, resolve an individual's impairment for complex auditory tasks heavily reliant on binaural cues provided through binaural hearing, such as binaural summation, binaural squelch, or localization of sounds.
Due to the inability to interpret interaural timing and level cues, SSD listeners demonstrate poor sound source localization in azimuth. 31 32 41 Interestingly, some researchers have demonstrated that monaural listeners can in fact localize in the horizontal plane by relying on spectral cues 17 42 or perceived level differences in the signal, as it moves from the impaired ear to the normal hearing ear. 43 Although the improved localization abilities do not approach that of normal hearing listeners, the results suggest a “remapping” 44 may occur in some monaural listeners, and provide improved functionality. It is important to note that this is not an effect of adding a hearing device, 42 rather it is an ability of some SSD listeners to employ compensatory mechanisms to improve their localization strategies. 43 44 The utilization of ear level devices, however, may serve to disrupt access to monaural spectral cues in this population. 45 The pinnae allows for collection of high-frequency cues which is used to provide information about where a sound is located in elevation. 46 Agterberg and colleagues demonstrated that some monaural listeners are able to utilize these high frequency spectral cues to improve localization abilities, despite the inability to access binaural cues. 17 The degree to which use of said spectral cues improves perceived handicap and provides functional benefit remains unclear. Though, it may point to the continued ambiguity in those who adopt and accept CROS as a management option for their SSD and those who do not. It may be that those who adopt and accept CROS are more handicapped by impairments related to hearing in noise than impaired spatial perception. Equally, it may suggest that those who reject CROS have adapted 44 and become dependent on the subtle spectral cues ablated by CROS hearing aid use. Other research suggests that monaural listeners show a preference to use of level cues for source localization in the horizontal plane. 43 Reweighting, or learning to rely on unchanged monaural cues, has been shown to benefit individuals with SSD in localization. 44 Rerouting of the signal through use of the CROS device eliminates the ability to detect such level cues, thereby disrupting the reweighting strategy that may be employed by monaural listeners. Yet, these strategies are not evident in all individuals with SSD. In fact, the vast majority of studies fail to demonstrate functional horizontal localization abilities in this population. 27 31 32 35 41 Remapping and reweighting of auditory cues is reliant on a variety factors and occurs over time. 44 It is more likely that those who can take advantage of these strategies are younger listeners with good residual access to high frequency hearing 17 who have had time to adapt to the monaural hearing condition.
While CROS and BiCROS hearing devices assist a patient in accessing speech signals arriving to the deaf ear, they cannot distinguish a signal of interest from that which is distracting (i.e., noise). Specifically, when noise is on the CROS transmitter side it is amplified and transferred to the better ear which could interfere with the signal of interest. Studies have demonstrated that in listening situations where the signal of interest is at the better hearing ear and noise is being transferred by way of the CROS microphone from the impaired side, a significant decrease in speech understanding is observed. 31 32 33 35 47 Recent studies have found gains in speech understanding from CROS input to be notably greater than the potential loss that occurs when noise is transferred to the better hearing ear. 35 48 While this may potentially outweigh the negative affect for some users, it follows that those who reject CROS may find even a small decrement in better ear hearing to be too disruptive to their everyday listening needs.
The primary benefit for CROS and BiCROS amplification is realized when the signal is spatially separated from competing signals. 31 32 35 While there is an estimated 6 dB reduction in speech signals associated with the head-shadow effect in monaural listeners, 49 the signal-to-noise ratio will in fact vary depending on the orientation of the signal relative to the good ear. 49 Specifically, this reduction and thereby deficit decreases as signals move more medially toward the front of the listener. Understandably, degree of benefit will vary according to the listening condition. The inability to fully control the listening environment is a challenge for monaural listener's using a rerouting system. Diffuse noise, for example, doesn't allow for successful separation of signal and interferer. This may prove even more problematic in BiCROS users where the signal (in this case, interfering noise) is not only rerouted but also amplified in the better hearing ear. These challenges may serve to limit benefit with CROS use in certain listening situations and ultimately influence adoption and acceptance.
Considerations in CROS Amplification
The primary goal of CROS hearing aids is to successfully deliver the signal that would be obtained in the deaf ear to the better hearing ear. There are some key challenges to achieving this. How and where the sound is collected is an important consideration. The microphone placement of CROS devices is typically placed superiorly at the top of the pinnae. This microphone location does not allow for natural collection of sound with the benefits of the pinnae to collect full spectrum of sound. One of the primary benefits of contemporary wireless CROS amplification is the ability to utilize open fit strategies that minimize disruption of the natural ear canal acoustics. 25 It should not be overlooked that the introduction of anything into the ear canal will disrupt the natural ear canal acoustics, regardless of how small or unobtrusive. This effect can be significant in those with small ear canals. As such, it is important to determine the effectiveness of CROS through the use of real ear measurements.
Real ear measures utilize a small microphone placed in the ear canal to record the frequency and intensity characteristics of the signal at the tympanic membrane. This objective tool allows the clinician to determine the real ear unaided response, or the sound pressure level across frequencies measured in an open/unaided ear canal. In true CROS fittings, it is important to ensure that the presence of the hearing aid in the ear canal does not occlude the ear, and thereby reduce or distort the natural acoustic signal in the normal hearing ear. This measure can be repeated with the open fit hearing device in the ear canal to check for occlusion. If there the device is occluding, a reduction in the response will be observed at some or all of the frequencies. An ideal CROS fitting should produce a response that mimics the real ear unaided response with little to no reduction in sound pressure level at the tympanic membrane. It is also essential to ensure that the CROS microphone placed on the deaf ear is successfully transmitting the signal to the better hearing ear. For this measure, the signal should be presented to the deaf ear with the CROS hearing aid on and in place at 45 to 90 degrees azimuth to simulate the acoustic head-shadow ( Fig. 3 ). The measurement is taken in the better hearing ear and compared with the real ear unaided response. The goal of this measure is to ensure that the full spectrum of the responses matches unaided response of the better hearing ear, indicating the CROS system is overcoming the head-shadow effect. Some CROS users will report that soft sounds are too loud, or dissatisfaction with the sound quality. Current CROS hearing devices do provide some mild gain in the high frequencies. Real ear measures also will help to determine if too much gain is being applied and allow the clinician to make adjustments to improve the sound quality for the listener. BiCROS fittings real ear measures are used not only to verify the signal from the deaf ear but also that the amplification applied is meeting the specified targets to appropriately aid the hearing loss in the better hearing ear. The reader is recommended to reference Dillon for further details on verification of CROS and BiCROS hearing aids. 50
Fig. 3.
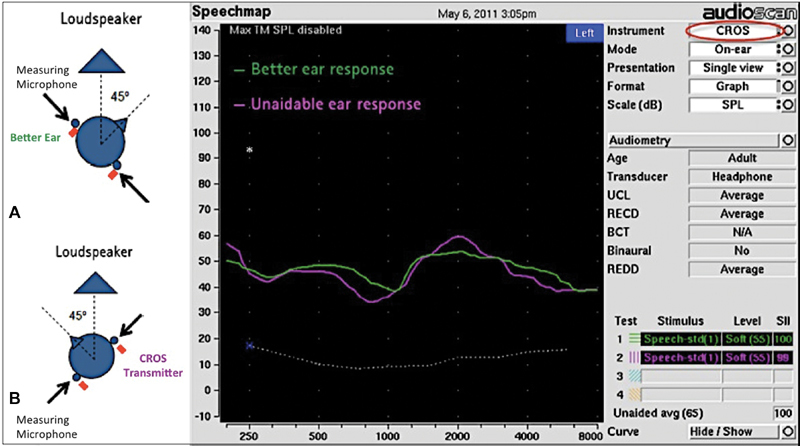
Real ear probe microphone set up for CROS hearing aid verification. ( A ) and ( B ) demonstrate the test setup with the loud speaker positioned first at the better hearing ear ( A ) and then at the side of the CROS transmitter ( B ). Green represents the real ear unaided response. Pink represents the response measured in the better ear delivered contralaterally from the CROS microphone (Images courtesy to Phonak, LLC, with permission). CROS, contralateral routing of signal.
It should be noted that speech perception in noise performance and that benefit with implantable and nonimplantable devices may vary within the same subject. 35 While the efficacy of rerouting solutions has been well established in the SSD population, others report limited to no benefit with rerouting in the SSD population. 51 52 These things considered, to ensure successful management of SSD, it is imperative that appropriate evaluation methods are applied to determine potential benefit. 53 Needs assessments that accurately characterize the listening deficits of the SSD listener are an important component in the evaluation and management of this population. Likewise, utilizing speech in noise measures to assess for reduction of the head-shadow can offer important insight into the potential benefit gained through rerouting. Although rerouting solutions do not provide binaural input, including localization or other measures that demonstrate binaural benefit may assist clinicians in better determining appropriate treatment options. Comprehensive pretreatment measures may assist with triaging patients more effectively and may provide insight into the perceived benefit with device use. 54
Summary
Current CROS technology solutions provide a noninvasive, aesthetically appealing, low-cost option for individuals with SSD. CROS solutions do not provide restoration of binaural hearing and cannot improve tasks requiring binaural input, such as localization. The primary benefits realized from CROS hearing devices are improved sound awareness from the impaired side and better hearing in noise when speech is located at impaired side. As such, appropriate pretreatment measures should be utilized when determining candidacy for rerouting. Likewise fitting of devices should be optimized to ensure CROS performance and absence of occlusion in the better hearing ear. An increase in acceptance of CROS technology, along with recent reports of objective and subjective benefit, suggest that some individuals with SSD may be adequately remediated with rerouting. CROS devices are nonsurgical, and should be considered prior to offering a surgical solution. In those individuals with SSD who do not benefit from CROS technology, referral for evaluation and consideration of alternative options, such as bone conduction or cochlear implants may be considered. *
Footnotes
Bone conduction implants and cochlear implants are not universally approved to treat single-sided deafness or asymmetric sensorineural hearing loss. Use of these products for the SSD indication may not be approved or may be subject to restrictions in the region and/or country in which you practice.
References
- 1.Tos M, Stangerup S E, Cayé-Thomasen P, Tos T, Thomsen J. What is the real incidence of vestibular schwannoma? Arch Otolaryngol Head Neck Surg. 2004;130(02):216–220. doi: 10.1001/archotol.130.2.216. [DOI] [PubMed] [Google Scholar]
- 2.Nicoucar K, Momjian S, Vader J P, De Tribolet N. Surgery for large vestibular schwannomas: how patients and surgeons perceive quality of life. J Neurosurg. 2006;105(02):205–212. doi: 10.3171/jns.2006.105.2.205. [DOI] [PubMed] [Google Scholar]
- 3.Rigby P L, Shah S B, Jackler R K, Chung J H, Cooke D D. Acoustic neuroma surgery: outcome analysis of patient-perceived disability. Am J Otol. 1997;18(04):427–435. [PubMed] [Google Scholar]
- 4.Giolas T G, Wark D J. Communication problems associated with unilateral hearing loss. J Speech Hear Disord. 1967;32(04):336–343. doi: 10.1044/jshd.3204.336. [DOI] [PubMed] [Google Scholar]
- 5.Sargent E W, Herrmann B, Hollenbeak C S et al. The minimum speech test battery in profound unilateral hearing loss. Otol Neurotol. 2001;22(04):480–486. doi: 10.1097/00129492-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Douglas S A, Yeung P, Daudia A, Gatehouse S, O'Donoghue G M. Spatial hearing disability after acoustic neuroma removal. Laryngoscope. 2007;117(09):1648–1651. doi: 10.1097/MLG.0b013e3180caa162. [DOI] [PubMed] [Google Scholar]
- 7.Gatehouse S, Noble W. The speech, spatial and qualities of hearing scale (SSQ) Int J Audiol. 2004;43(02):85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Middlebrooks J C, Green D M. Sound localization by human listeners. Annu Rev Psychol. 1991;42:135–159. doi: 10.1146/annurev.ps.42.020191.001031. [DOI] [PubMed] [Google Scholar]
- 9.Araújo P G, Mondelli M F, Lauris J R, Richiéri-Costa A, Feniman M R. Assessment of the auditory handicap in adults with unilateral hearing loss. Rev Bras Otorrinolaringol (Engl Ed) 2010;76(03):378–383. doi: 10.1590/S1808-86942010000300018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sano H, Okamoto M, Ohhashi K, Iwasaki S, Ogawa K. Quality of life reported by patients with idiopathic sudden sensorineural hearing loss. Otol Neurotol. 2013;34(01):36–40. doi: 10.1097/MAO.0b013e318278540e. [DOI] [PubMed] [Google Scholar]
- 11.Silverman C A, Silman S, Emmer M B, Schoepflin J R, Lutolf J J. Auditory deprivation in adults with asymmetric, sensorineural hearing impairment. J Am Acad Audiol. 2006;17(10):747–762. doi: 10.3766/jaaa.17.10.6. [DOI] [PubMed] [Google Scholar]
- 12.Augustine A M, Chrysolyte S B, Thenmozhi K, Rupa V. Assessment of auditory and psychosocial handicap associated with unilateral hearing loss among Indian patients. Indian J Otolaryngol Head Neck Surg. 2013;65(02):120–125. doi: 10.1007/s12070-012-0586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schrøder S A, Ravn T, Bonding P. BAHA in single-sided deafness: patient compliance and subjective benefit. Otol Neurotol. 2010;31(03):404–408. doi: 10.1097/MAO.0b013e3181d27cc0. [DOI] [PubMed] [Google Scholar]
- 14.Desmet J, Bouzegta R, Hofkens A et al. Clinical need for a BAHA trial in patients with single-sided sensorineural deafness. Analysis of a Baha database of 196 patients. Eur Arch Otorhinolaryngol. 2012;269(03):799–805. doi: 10.1007/s00405-011-1733-5. [DOI] [PubMed] [Google Scholar]
- 15.Sano H, Kamijo T, Ino T, Okamoto M. Edaravone, a free radical scavenger, in the treatment of idiopathic sudden sensorineural hearing loss with profound hearing loss. Auris Nasus Larynx. 2010;37(01):42–46. doi: 10.1016/j.anl.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Harford E, Barry J. a rehabilitative approach to the problem of unilateral hearing impairment: the contralateral routing of signals cros. J Speech Hear Disord. 1965;30:121–138. doi: 10.1044/jshd.3002.121. [DOI] [PubMed] [Google Scholar]
- 17.Agterberg M J, Hol M K, Van Wanrooij M M, Van Opstal A J, Snik A F. Single-sided deafness and directional hearing: contribution of spectral cues and high-frequency hearing loss in the hearing ear. Front Neurosci. 2014;8:188. doi: 10.3389/fnins.2014.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothpletz A M, Wightman F L, Kistler D J. Informational masking and spatial hearing in listeners with and without unilateral hearing loss. J Speech Lang Hear Res. 2012;55(02):511–531. doi: 10.1044/1092-4388(2011/10-0205). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumpik D P, Kacelnik O, King A J. Adaptive reweighting of auditory localization cues in response to chronic unilateral earplugging in humans. J Neurosci. 2010;30(14):4883–4894. doi: 10.1523/JNEUROSCI.5488-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill S L, III, Marcus A, Digges E N, Gillman N, Silverstein H.Assessment of patient satisfaction with various configurations of digital CROS and BiCROS hearing aids Ear Nose Throat J 20068507427–430., 442 [PubMed] [Google Scholar]
- 21.Picou E M, Aspell E, Ricketts T A. Potential benefits and limitations of three types of directional processing in hearing aids. Ear Hear. 2014;35(03):339–352. doi: 10.1097/AUD.0000000000000004. [DOI] [PubMed] [Google Scholar]
- 22.Kim G, Lu Y, Hu Y, Loizou P C. An algorithm that improves speech intelligibility in noise for normal-hearing listeners. J Acoust Soc Am. 2009;126(03):1486–1494. doi: 10.1121/1.3184603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCreery R W, Venediktov R A, Coleman J J, Leech H M. An evidence-based systematic review of directional microphones and digital noise reduction hearing aids in school-age children with hearing loss. Am J Audiol. 2012;21(02):295–312. doi: 10.1044/1059-0889(2012/12-0014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kochkin S. MarkeTrak VIII: The key influencing factors in hearing aid purchase intent. Hear Rev. 2012;19(03):12–25. [Google Scholar]
- 25.Stone M A, Moore B C, Meisenbacher K, Derleth R P. Tolerable hearing aid delays. V. Estimation of limits for open canal fittings. Ear Hear. 2008;29(04):601–617. doi: 10.1097/AUD.0b013e3181734ef2. [DOI] [PubMed] [Google Scholar]
- 26.Kiessling J, Brenner B, Jespersen C T, Groth J, Jensen O D. Occlusion effect of earmolds with different venting systems. J Am Acad Audiol. 2005;16(04):237–249. doi: 10.3766/jaaa.16.4.5. [DOI] [PubMed] [Google Scholar]
- 27.Snapp H A, Holt F D, Liu X, Rajguru S M. Comparison of speech-in-noise and localization benefits in unilateral hearing loss subjects using contralateral routing of signal hearing aids or bone-anchored implants. Otol Neurotol. 2017;38(01):11–18. doi: 10.1097/MAO.0000000000001269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finbow J, Bance M, Aiken S, Gulliver M, Verge J, Caissie R. A comparison between wireless cros and bone-anchored hearing devices for single-sided deafness: a pilot study. Otol Neurotol. 2015;36(05):819–825. doi: 10.1097/MAO.0000000000000762. [DOI] [PubMed] [Google Scholar]
- 29.Williams V A, McArdle R A, Chisolm T H. Subjective and objective outcomes from new BiCROS technology in a veteran sample. J Am Acad Audiol. 2012;23(10):789–806. doi: 10.3766/jaaa.23.10.5. [DOI] [PubMed] [Google Scholar]
- 30.Gelfand S A. Usage of CROS hearing aids by unilaterally deaf patients. Arch Otolaryngol. 1979;105(06):328–332. doi: 10.1001/archotol.1979.00790180026005. [DOI] [PubMed] [Google Scholar]
- 31.LinL M, Bowditch S, Anderson M J, May B, Cox K M, Niparko J K. Amplification in the rehabilitation of unilateral deafness: speech in noise and directional hearing effects with bone-anchored hearing and contralateral routing of signal amplification. Otol Neurotol. 2006;27(02):172–182. doi: 10.1097/01.mao.0000196421.30275.73. [DOI] [PubMed] [Google Scholar]
- 32.Niparko J K, Cox K M, Lustig L R. Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otol Neurotol. 2003;24(01):73–78. doi: 10.1097/00129492-200301000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Bosman A J, Hol M K, Snik A F, Mylanus E A, Cremers C W. Bone-anchored hearing aids in unilateral inner ear deafness. Acta Otolaryngol. 2003;123(02):258–260. doi: 10.1080/000164580310001105. [DOI] [PubMed] [Google Scholar]
- 34.Hol M K, Kunst S J, Snik A F, Bosman A J, Mylanus E A, Cremers C W. Bone-anchored hearing aids in patients with acquired and congenital unilateral inner ear deafness (BAHA CROS): clinical evaluation of 56 cases. Ann Otol Rhinol Laryngol. 2010;119(07):447–454. doi: 10.1177/000348941011900704. [DOI] [PubMed] [Google Scholar]
- 35.Snapp H A, Hoffer M E, Liu X, Rajguru S M. Effectiveness in rehabilitation of current wireless CROS technology in experienced bone-anchored implant users. Otol Neurotol. 2017;38(10):1397–1404. doi: 10.1097/MAO.0000000000001614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kochkin S. MarkeTrak VII: obstacles to adult non-user adoption of hearing aids. Hear J. 2007;60(04):24–50. [Google Scholar]
- 37.Gallant S, Lee J, Jethanamest D. Skin necrosis in a magnet-based bone-conduction implant. Ear Nose Throat J. 2017;96(12):454–455. [PubMed] [Google Scholar]
- 38.Van der Gucht K, Vanderveken O, Hamans E, Claes J, Van Rompaey V, Van de Heyning P. Adverse skin reactions following percutaneous bone conduction implant surgery using the linear incision technique with and without subcutaneous tissue reduction. Acta Otolaryngol. 2017;137(02):149–153. doi: 10.1080/00016489.2016.1222548. [DOI] [PubMed] [Google Scholar]
- 39.Dun C A, Faber H T, de Wolf M J, Mylanus E A, Cremers C W, Hol M K. Assessment of more than 1,000 implanted percutaneous bone conduction devices: skin reactions and implant survival. Otol Neurotol. 2012;33(02):192–198. doi: 10.1097/MAO.0b013e318241c0bf. [DOI] [PubMed] [Google Scholar]
- 40.Zeitler D M, Herman B S, Snapp H A, Telischi F F, Angeli S I. Ethnic disparity in skin complications following bone-anchored hearing aid implantation. Ann Otol Rhinol Laryngol. 2012;121(08):549–554. doi: 10.1177/000348941212100809. [DOI] [PubMed] [Google Scholar]
- 41.Wazen J J, Spitzer J B, Ghossaini S N et al. Transcranial contralateral cochlear stimulation in unilateral deafness. Otol Head Neck Surg. 2003;129(03):248–254. doi: 10.1016/S0194-5998(03)00527-8. [DOI] [PubMed] [Google Scholar]
- 42.Agterberg M JH, Snik A FM, Van de Goor R MG, Hol M KS, Van Opstal A J.Sound-localization performance of patients with single-sided deafness is not improved when listening with a bone-conduction deviceHear Res2018; (e-pub ahead of print) Doi: 10.1016/j.heares.2018.04.007 [DOI] [PMC free article] [PubMed]
- 43.Van Wanrooij M M, Van Opstal A J. Contribution of head shadow and pinna cues to chronic monaural sound localization. J Neurosci. 2004;24(17):4163–4171. doi: 10.1523/JNEUROSCI.0048-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keating P, Rosenior-Patten O, Dahmen J C, Bell O, King A J. Behavioral training promotes multiple adaptive processes following acute hearing loss. eLife. 2016;5:e12264. doi: 10.7554/eLife.12264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pedley A J, Kitterick P T. Contralateral routing of signals disrupts monaural level and spectral cues to sound localisation on the horizontal plane. Hear Res. 2017;353:104–111. doi: 10.1016/j.heares.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blauert J. London, England: The MIT Press; 1997. Spatial Hearing: The Psychophysics of Human Sound Localization. [Google Scholar]
- 47.Wazen J J, Ghossaini S N, Spitzer J B, Kuller M. Localization by unilateral BAHA users. Otolaryngol Head Neck Surg. 2005;132(06):928–932. doi: 10.1016/j.otohns.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 48.Taal C H, van Barneveld D C, Soede W, Briaire J J, Frijns J H. Benefit of contralateral routing of signals for unilateral cochlear implant users. J Acoust Soc Am. 2016;140(01):393. doi: 10.1121/1.4955307. [DOI] [PubMed] [Google Scholar]
- 49.Tillman T W, Carhart R, Nicholls S. Release from multiple maskers in elderly persons. J Speech Hear Res. 1973;16(01):152–160. doi: 10.1044/jshr.1601.152. [DOI] [PubMed] [Google Scholar]
- 50.Dillon H. New York: Thieme; 2001. Hearing Aids. In; pp. 434–450. [Google Scholar]
- 51.Arndt S, Laszig R, Aschendorff A et al. [Unilateral deafness and cochlear implantation: audiological diagnostic evaluation and outcomes] HNO. 2011;59(05):437–446. doi: 10.1007/s00106-011-2318-8. [DOI] [PubMed] [Google Scholar]
- 52.Buss E, Dillon M T, Rooth M A et al. Effects of cochlear implantation on binaural hearing in adults with unilateral hearing loss. Trends Hear. 2018;22:2.331216518771173E15. doi: 10.1177/2331216518771173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Snapp H A, Fabry D A, Telischi F F, Arheart K L, Angeli S I. A clinical protocol for predicting outcomes with an implantable prosthetic device (Baha) in patients with single-sided deafness. J Am Acad Audiol. 2010;21(10):654–6625. doi: 10.3766/jaaa.21.10.5. [DOI] [PubMed] [Google Scholar]
- 54.Snapp H, Angeli S, Telischi F F, Fabry D. Postoperative validation of bone-anchored implants in the single-sided deafness population. Otol Neurotol. 2012;33(03):291–296. doi: 10.1097/MAO.0b013e3182429512. [DOI] [PubMed] [Google Scholar]


