Dear Editor,
CLL is the most common adult leukemia in western countries accounting for 25–30% cases with a median age of diagnosis of 70 years [1]. Most patients are asymptomatic at diagnosis and come to clinical attention due to incidentally detected lymphocytosis. Cutaneous lesions can be seen in 25% of CLL cases but usually represent non-specific etiology like infection, autoimmune phenomenon or even more common in relapse/refractory cases [2]. True leukemic involvement is seen in less than 5% cases and may portend a better prognosis. Here, we describe a case of CLL with skin involvement at initial presentation.
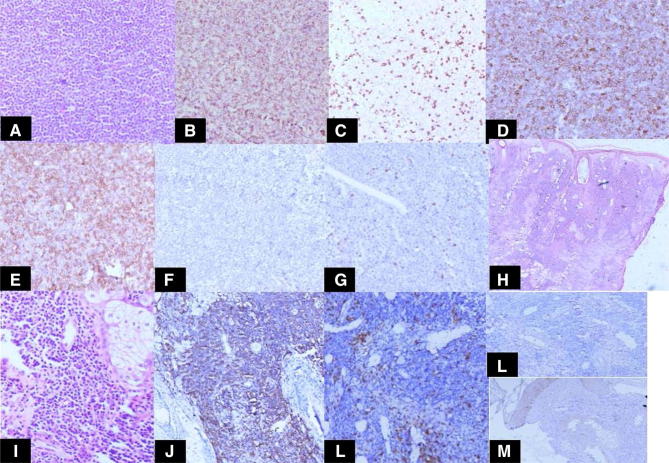
A 45-year-old lady, with no prior co-morbidities was referred to our center with complaints of swelling over the left earlobe and the bridge of nose for 6 months. On examination, she had generalized lymphadenopathy with multiple palpable cervical, axillary and inguinal lymph nodes. Her baseline compete blood count showed a total leucocyte count of 125,000 with 90% abnormal lymphocytes without anaemia or thrombocytopenia. Flow cytometry of peripheral blood showed 90% abnormal lymphocytes which were CD5, CD19 (dim), CD20 (dim), CD23 and negative for CD10, CD30, CD103, CD138, BCL-1, BCL-6 suggestive of CLL. A biopsy was done from the nasal nodule which showed a normal epidermis, but dermis being infiltrated with lymphocytes and few histiocytes with sparing of dermal appendages and extending into subcutis. Immunohistochemistry (IHC) was positive for CD19, CD20, CD5 and CD 23 and negative for cyclin D1 (Fig. 1a–g). A lymph node biopsy was done from retroauricular node which showed effacement of lymph node architecture with replacement by abnormal lymphocytes with similar IHC markers as in skin biopsy (Fig. 1h–m). CECT chest abdomen pelvis at baseline showed multiple enlarged abdominal lymph nodes with axillary lymphadenopathy without any hepatosplenomegaly. A final diagnosis of CLL Rai stage II was made. The patient is under observation currently as she doesn’t meet IWGCLL criteria for treatment.
Fig. 1.
a Microphotograph shows effacement of lymph nodal architecture by small size lymphoid cell. [H&E ×100] Immunohistochemistry shows the cell are immunopositive for b CD20, d CD5, e CD23 while negative for c CD3, f CD10 and g Cyclin D1. The skin biopsy diffuse infiltration of dermis by small lymphoid cells [h H&E ×100, i H&E ×200]. The cells are immunopositive for CD20 (j) while negative for CD3 (k), CD10 (l) and Cyclin D1 (m)
Presentation of CLL with skin involvement is rare with only a handful of cases reported in literature. The reported lesions include papules, plaques, nodules and ulcerations with predilection for head and neck areas [2]. Majority of skin lesions in CLL are a manifestation of autoimmune phenomenon which are common in CLL rather than direct infiltration [2]. Evident skin involvement at baseline is more common in Richter syndrome or T-CLL [3]. Typically, skin manifestations happen late in the natural history of the disease, often after multiple treatment and recurrence. This early presentation is far less common.
Leukemia cutis, in CLL, is usually seen as infiltration of small lymphoid cells with round nuclear contours in the dermis. The largest case series of cutaneous manifestations in CLL comes from Cerroni et al. [4] in which they described three main architectural patterns, however the impact of such patterns on prognosis is not clear. Since upfront skin involvement is rare in patients with B-CLL, there is no prospective data to guide whether therapy should be determined by the presence of skin involvement. In the study by Cerroni et al. [4], the 5-year survival of these patients was 66.6%, suggesting that they had a good, if not a more favorable, prognosis compared to those without skin involvement. Other studies have shown similar results indicating that although skin involvement in Richter syndrome or T-CLL portends a poor prognosis, that may not be the case in B-CLL [5]. However firm conclusions are difficult to draw because of the rarity of the condition and retrospective nature of the data. We have kept our patient under follow-up as he was asymptomatic and did not meet standard criteria for CLL treatment.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Robak E, Robak T. Skin lesions in chronic lymphocytic leukemia. Leuk Lymphoma. 2007;485:855–865. doi: 10.1080/10428190601137336. [DOI] [PubMed] [Google Scholar]
- 3.Giles FJ, O’Brien SM, Keating MJ. Chronic lymphocytic leukemia in (Richter’s) transformation. Semin Oncol. 1998;25:117–125. [PubMed] [Google Scholar]
- 4.Cerroni L, Zenahlik P, Hofler G. Specific cutaneous infiltrates of B-cell chronic lymphocytic leukemia: a clinicopathologic and prognostic study of 42 patients. Am J Surg Pathol. 1996;20:1000–1010. doi: 10.1097/00000478-199608000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Colburn DE, Welch MA, Giles FJ. Skin infiltration with chronic lymphocytic leukemia is consistent with a good prognosis. Hematology. 2002;7:187–188. doi: 10.1080/1024533021000008164. [DOI] [PubMed] [Google Scholar]