Abstract
Eosinophils have long been recognized as a central effector cell in the lungs of asthmatic patients. They contribute to airway inflammation and remodeling through releasing several molecules such as cytokines, granule proteins, lipid mediators and extracellular traps/vesicles. Repeated evidence reveals that intense eosinophil infiltration in upper and lower airway mucosae contributes to the pathogenesis of aspirin-exacerbated respiratory disease (AERD). Persistent eosinophilia is found to be associated with type 2 immune responses, cysteinyl leukotriene overproduction and eosinophil-epithelium interactions. This review highlights recent findings about key mechanisms of eosinophil activation in the airway inflammation of AERD. In addition, current biologics (targeting type 2 immune responses) were suggested to control eosinophilic inflammation for AERD patients.
Keywords: Eosinophils, epithelium, therapy
INTRODUCTION
Aspirin-exacerbated respiratory disease (AERD) is characterized by hypersensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs), asthma and chronic rhinosinusitis (CRS) with nasal polyps (NPs).1 Overproduction of cysteinyl leukotrienes (cysLTs) is a hallmark of AERD in the pathogenic mechanisms. CysLTs induce smooth muscle constriction and potentially enhance eosinophil accumulation in the bronchial mucosa.2 Therefore, eosinophilia is commonly found in peripheral blood and upper and lower airway mucosae of AERD patients.3 In addition, AERD is a type 2 immune-mediated airway disease associated with increased expression of Th2 cytokines such as interleukin (IL)-4, IL-5 and IL-13, resulting in persistent eosinophilic inflammation.4 Although many studies have shown evidence that activated effector cells such as eosinophils, neutrophils, mast cells and platelets are involved in the pathogenesis of AERD,5 this review emphasizes recent insights into how eosinophils work in airway mucosa of AERD patients.
SECTION 1: EOSINOPHILS RELEASE MULTIPLE MEDIATORS
A novel molecule released from activated eosinophils may provide a new perspective, as AERD is not fully explained by type 2 cytokines (via Th2/ILC2 responses) or overproduced cysLTs. Extracellular traps from eosinophils composed of DNA and granule proteins are involved in innate immunity and associated with several allergic diseases.6 Moreover, recent studies have revealed that eosinophils from asthmatic patients secrete higher levels of extracellular vesicles, leading to the development and progression of asthma.7 These findings suggest that activated eosinophils contribute to the pathogenesis of AERD through producing several molecules (Table). However, further investigations are needed to understand the role of innate immune responses to activate eosinophils in AERD.
Table. Mechanisms of activated eosinophils in the pathogenesis of aspirin-exacerbated respiratory disease CysLT, cysteinyl leukotriene; IL, interleukin.
| Key factors | Main sources | Function | |
|---|---|---|---|
| Type 2 immunity | |||
| IL-5 | Th2/ILC2 | Increase eosinophil activation/survival | |
| CysLT overproduction | |||
| LTE4 | Eosinophils | Elevate eosinophil accumulation | |
| Induce smooth muscle constriction | |||
| Eosinophil-epithelium interaction | |||
| Extracellular traps/vesicles | Eosinophils | Enhance airway inflammation | |
CysLTs
CysLTs, a class of inflammatory lipid mediators, contribute to several characteristic features of AERD. These molecules are derived from effector cells through arachidonic acid metabolism (upon ingesting COX-1 inhibitors such as aspirin and NSAIDs) that oxidizes arachidonic acid to form unstable intermediate leukotriene (LTA4).8 In eosinophils, LTA4 is changed into LTC4 by the enzyme LTC4 synthase and sequentially converted into LTD4.9 Urinary LTE4 (a stable end product) levels, a biomarker for systemic leukotriene production, are significantly higher in AERD patients compared to patients with aspirin-tolerant asthma (ATA) at baseline. Furthermore, these levels even increase 100-fold on aspirin challenge.10 These mediators contribute to eosinophil activation, mucus production, vascular leakage, and edema, which enhance airway inflammation and remodeling in AERD patients.11
Eosinophil extracellular traps
Activated eosinophils release extracellular traps in an NADPH oxidase-dependent manner (associated with reactive oxygen species production), which is distinct from apoptosis and necrosis.12 Many reports have demonstrated that eosinophil extracellular traps are often associated with blood and tissue eosinophilia.13,14 Extracellular traps have a function in innate immunity to infectious disease; however, these molecules are cytotoxic enough to induce tissue damage in asthmatic airways.15,16 In addition, the percentage of eosinophils forming extracellular traps was significantly elevated under severe airway inflammation.17 Although the pathophysiological function of extracellular traps has not been completely determined, our current study demonstrates that the percentage of eosinophils producing extracellular traps is negatively correlated with baseline forced expiratory volume in 1 second and positively correlated with the levels of eosinophil-derived neurotoxin in serum.18 These suggest that extracellular traps may play a crucial role in severe eosinophilic inflammation and airway obstruction.
Eosinophil extracellular vesicles
Extracellular vesicles are small molecules that contain multiple bioactive proteins, lipids, and nucleic acid, which are important for intercellular communication.19 These membrane-bound carriers are continuously released by several cells and contain different cellular components, depending on their origin.20 Extracellular vesicles have been implicated in the pathogenesis of multiple diseases such as cancer, metabolic disorders, and allergic diseases.21,22,23,24 Because of their abundance and unique composition, these molecules have potential as a biomarker for the diagnosis and prognosis of a wide variety of diseases.25 Recently, it has been demonstrated that eosinophils from asthmatic patients secrete a greater quantity of extracellular vesicles than those from healthy control subjects.26 Moreover, production of extracellular vesicles from eosinophils was enhanced in response to inflammatory stimuli such as eotaxin-1 and tumor necrosis factor-α.27 These findings are important to understand the complicated secretory activities of eosinophils underlying immune responses. It is evident that extracellular vesicles participate in allergic diseases with a significant implication in asthma progression. However, further studies are still needed to clarify a specific role of extracellular vesicles in AERD patients.
SECTION 2: EOSINOPHILS INTERACT WITH AIRWAY EPITHELIAL CELLS
Airway epithelial cells represent the first line of the barrier which constantly maintains the mucosal interface epithelium. These cells are involved in innate immunity by expression of diverse pattern recognition receptors against viruses, microorganisms or environmental pollutants.28 Moreover, infiltration of immune cells into the proximity of epithelium results in the induction of adaptive immunity through interactions with epithelial cells.29 Epithelium-derived cytokines such as IL-33, IL-25 and thymic stromal lymphopoietin (TSLP) are implicated in the pathophysiology of asthma.30 In addition to inflammatory features, airway remodeling (changes in the structure and function of epithelium) found in asthmatic patients results in increased resistance of airflow.31 AERD patients present a remodeling process that affects both the upper and lower airways.32 Several molecules released from airway epithelium have been reported to be associated with airway inflammation and remodeling.
Surfactant protein D (SPD)
SPD is a member of the collectin family of proteins mainly produced by airway epithelial cells.33 This molecule is a component of innate immunity within the airways binding to pathogens and inducing phagocytosis by interacting with phagocytic cells.34 In addition, SPD modulates allergic responses through the regulation of eosinophil activation.35 Emerging evidence has demonstrated that SPD is associated with several pulmonary diseases including asthma.36 The SPD level in BALF is significantly lower in patients with severe asthma than in those with mild asthma or healthy control subjects.37 Recently, our group has revealed that the serum SPD level was reduced in AERD patients compared to ATA patients. Moreover, the increased number of eosinophils (LTE4-mediated) in the lungs enhances airway inflammation and remodeling; however, SPD treatment attenuates the symptoms in mice,38 indicating that SPD may have a protective function against eosinophils in the airway inflammation of AERD.
Folliculin (FLCN)
FLCN is an intracellular protein expressed in several inflammatory cells including airway epithelial cells.39,40 This molecule has been suggested to be associated with activation of epithelial cells and maintenance of the integrity of the epithelium barrier through regulation of cell-cell adhesion and expression of cell-cell junctions.41,42 Impairment of epithelial barrier function (change in junctional complexes) is important in allergic disease including occupational asthma.43,44 In AERD patients with NPs, airway epithelium is disrupted by detachment of epithelial cells and damage of intercellular junctions.45 In addition, our recent study demonstrated a significantly higher level of serum FCLN in the AERD group compared to the ATA group.46 Airway eosinophilia found in AERD could increase FLCN release from airway epithelial cells, which enhances epithelial activation and disruption, suggesting that modulation of FLCN may be a potential therapeutic target for AERD.
Periostin
Periostin (a secreted matricellular protein) is produced by airway epithelial cells, leading to eosinophilic inflammation in asthmatic patients.47 It has been demonstrated that periostin is a key player for inducing airway hyperresponsiveness in mice.48 In addition, expression of periostin in airway epithelial cells is up-regulated in the presence of IL-13 (a pleiotropic Th2-cytokine) in vitro.49 IL-13 is released by several immune cells such as eosinophils, mast cells, basophils, and activated T cells.50 Previously, we have shown that the serum periostin level was significantly higher in patients with AERD (severe asthma/eosinophilic asthma) than in those with ATA. In addition, the serum periostin level is positively correlated with blood and sputum eosinophil counts.51 Furthermore, our recent evidence reveals that production of periostin is markedly elevated under the eosinophilic condition and positively associated with the transforming growth factor-β1 level.52 Therefore, periostin may play a crucial role in eosinophilic inflammation and remodeling in the airway of AERD patients.
SECTION 3: THERAPEUTIC APPROACH
For the management of AERD patients, anti-inflammatory medications including inhaled/systemic corticosteroid with or without long-acting beta2-agonist have been prescribed to achieve symptom controls with absolute avoidance from aspirin/NSAIDs.53 Regarding aspects of cysLTs overproduction, several drugs such as leukotriene receptor antagonists and 5-lipooxygenase inhibitors have been applied to suppress the leukotriene production pathways. In addition, a monoclonal antibody targeting the high-affinity receptor binding site on human immunoglobulin E (IgE) was suggested for AERD treatment.54 Furthermore, some ongoing studies on several biologics (targeting type 2 immune responses) have been under clinical trials to control eosinophilic inflammation in AERD patients.
Anti-IL-5 antibody
Previous studies have shown an abundant cytokine and chemokine milieu consistent with type 2 immunity in AERD.4 Some investigations confirmed that there were significant correlations between levels of IL-5 and cysLTs/ECP in NPs and nasal lavage fluid in AERD patients. IL-5 is also elevated in CRS with NPs in AERD patients compared to healthy controls or those with sinusitis without polyps, suggesting that IL-5 plays an important role in eosinophilic inflammation in upper and lower airway mucosae of AERD.55 There are monoclonal anti-IL-5 or anti-IL-5 receptor antibodies such as mepolizumab, reslizumab, and benralizumab, which are suggested effective for severe eosinophilic asthma.56 In the same context, they could also be applicable to control eosinophilic inflammation in upper and lower airway mucosae of AERD.57 Mepolizumab was evaluated in a small, randomized trial of patients with severe NPs, which proposed that it was beneficial for eosinophilic NPs, a key feature of AERD.58 Therefore, inhibition of type 2 response has a potential benefit in managing both conditions, CRS/NPs and AERD.
Antibodies to IL-33 and TSLP
Although eosinophilic inflammation reflects the effect of Th2 cells and allergen-specific IgE, there is a complementary pathway mediated by the innate immune system promoting the similar inflammatory process, especially as an amplifier of Th2 response. Eosinophilic inflammation is initiated by cytokines such as IL-33 and TSLP which are substantially derived from epithelial and other barrier cells damaged by microbes or toxins.59,60 IL-33 is an alarmin-like cytokine that activates both myeloid and lymphoid innate effector cells, thereby facilitating production of cytokines like IL-5, IL-13 and IL-9.61,62,63 A recent study demonstrated that IL-33 might be another cytokine playing an important role in the pathogenesis of AERD. The same study revealed that IL-33 was up-regulated in the airway epithelial layer and depended on cysLTs expression in mouse models, suggesting that IL-33 is a component of cysLT-driven innate immune response that promotes activation of mast cells and is attributed to AERD pathogenesis.64 Moreover, IL-33 is a potent stimulus for eosinophil activation that exacerbates airway inflammation.65 TSLP is an IL-7-like cytokine thought to be important in bronchial asthma, atopic dermatitis, and NPs, and induces type 2 cytokine production; therefore, it can activate eosinophils and basophils.66,67 A previous study investigated the effect of human monoclonal anti-TSLP IgG2λ in allergic asthmatic patients, suggesting a beneficial effect in reducing bronchoconstriction and airway inflammation against allergen challenge.59 Another report demonstrated that TSLP promoted mast cell-derived PGD2 production and dysregulation of this kind of innate immune system substantially contributes to the pathogenesis of AERD.68 Although these antibodies against IL-33 and TSLP are under clinical trial, they will be future treatment targets for AERD.
CONCLUSION
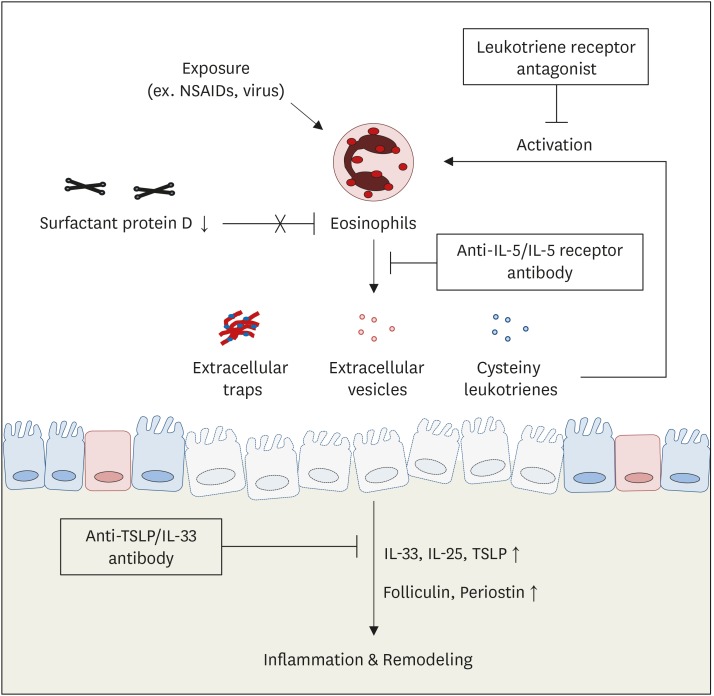
The clinical feature of AERD is moderate to severe asthma comorbid with CRS and NPs, which is associated with eosinophilic inflammation and cysLT overproduction in upper and lower airways. The pathophysiology of AERD is complicated; however, activation of immune cells (especially eosinophils), dysregulation of the arachidonic acid metabolism and alteration of genetic/epigenetic factors are important mechanisms in AERD patients. In addition, a novel molecule released by eosinophils (extracellular traps and extracellular vesicles) may provide an explanation of more severe airway inflammation and remodeling in AERD. A lower level of SPD (protective function) with higher levels of FLCN and periostin (pathogenic functions) further suggest playing critical roles of eosinophils interacting with airway epithelium, contributing to the pathogenesis of AERD. Therefore, biologics targeting eosinophilic inflammation may have potential benefits to manage AERD patients (Figure).
Figure. Therapeutic approach to the management of AERD patients. A leukotriene receptor antagonist attenuates asthma exacerbation caused by cysteinyl leukotriene production. An anti-IL-5/IL-5 receptor antibody inhibits eosinophil activation to release several mediators. An anti-TSLP or IL-33 antibody may potentially reduce type 2 immune responses associated with eosinophilic inflammation.
AERD, aspirin-exacerbated respiratory disease; IL, interleukin; NSAID, nonsteroidal anti-inflammatory drug; TSLP, thymic stromal lymphopoietin; SPD, surfactant protein D; CysLT, cysteinyl leukotriene.
ACKNOWLEDGMENTS
This study was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI16C0992).
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
References
- 1.Lee JH, Jung CG, Park HS. An update on the management of aspirin-exacerbated respiratory disease. Expert Rev Respir Med. 2018;12:137–143. doi: 10.1080/17476348.2018.1417843. [DOI] [PubMed] [Google Scholar]
- 2.Gauvreau GM, Parameswaran KN, Watson RM, O'Byrne PM. Inhaled leukotriene E(4), but not leukotriene D(4), increased airway inflammatory cells in subjects with atopic asthma. Am J Respir Crit Care Med. 2001;164:1495–1500. doi: 10.1164/ajrccm.164.8.2102033. [DOI] [PubMed] [Google Scholar]
- 3.Okano M, Kariya S, Ohta N, Imoto Y, Fujieda S, Nishizaki K. Association and management of eosinophilic inflammation in upper and lower airways. Allergol Int. 2015;64:131–138. doi: 10.1016/j.alit.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Conley DB, Tripathi A, Seiberling KA, Schleimer RP, Suh LA, Harris K, et al. Superantigens and chronic rhinosinusitis: skewing of T-cell receptor V beta-distributions in polyp-derived CD4+ and CD8+ T cells. Am J Rhinol. 2006;20:534–539. doi: 10.2500/ajr.2006.20.2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laidlaw TM, Boyce JA. Aspirin-exacerbated respiratory disease--new prime suspects. N Engl J Med. 2016;374:484–488. doi: 10.1056/NEJMcibr1514013. [DOI] [PubMed] [Google Scholar]
- 6.Simon D, Simon HU, Yousefi S. Extracellular DNA traps in allergic, infectious, and autoimmune diseases. Allergy. 2013;68:409–416. doi: 10.1111/all.12111. [DOI] [PubMed] [Google Scholar]
- 7.Mazzeo C, Cañas JA, Zafra MP, Rojas Marco A, Fernández-Nieto M, Sanz V, et al. Exosome secretion by eosinophils: a possible role in asthma pathogenesis. J Allergy Clin Immunol. 2015;135:1603–1613. doi: 10.1016/j.jaci.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 8.Reid GK, Kargman S, Vickers PJ, Mancini JA, Léveillé C, Ethier D, et al. Correlation between expression of 5-lipoxygenase-activating protein, 5-lipoxygenase, and cellular leukotriene synthesis. J Biol Chem. 1990;265:19818–19823. [PubMed] [Google Scholar]
- 9.Narayanankutty A, Reséndiz-Hernández JM, Falfán-Valencia R, Teran LM. Biochemical pathogenesis of aspirin exacerbated respiratory disease (AERD) Clin Biochem. 2013;46:566–578. doi: 10.1016/j.clinbiochem.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Christie PE, Tagari P, Ford-Hutchinson AW, Charlesson S, Chee P, Arm JP, et al. Urinary leukotriene E4 concentrations increase after aspirin challenge in aspirin-sensitive asthmatic subjects. Am Rev Respir Dis. 1991;143:1025–1029. doi: 10.1164/ajrccm/143.5_Pt_1.1025. [DOI] [PubMed] [Google Scholar]
- 11.Peters-Golden M, Gleason MM, Togias A. Cysteinyl leukotrienes: multi-functional mediators in allergic rhinitis. Clin Exp Allergy. 2006;36:689–703. doi: 10.1111/j.1365-2222.2006.02498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ueki S, Melo RC, Ghiran I, Spencer LA, Dvorak AM, Weller PF. Eosinophil extracellular DNA trap cell death mediates lytic release of free secretion-competent eosinophil granules in humans. Blood. 2013;121:2074–2083. doi: 10.1182/blood-2012-05-432088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dworski R, Simon HU, Hoskins A, Yousefi S. Eosinophil and neutrophil extracellular DNA traps in human allergic asthmatic airways. J Allergy Clin Immunol. 2011;127:1260–1266. doi: 10.1016/j.jaci.2010.12.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon D, Hoesli S, Roth N, Staedler S, Yousefi S, Simon HU. Eosinophil extracellular DNA traps in skin diseases. J Allergy Clin Immunol. 2011;127:194–199. doi: 10.1016/j.jaci.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Yousefi S, Simon D, Simon HU. Eosinophil extracellular DNA traps: molecular mechanisms and potential roles in disease. Curr Opin Immunol. 2012;24:736–739. doi: 10.1016/j.coi.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Ueki S, Konno Y, Takeda M, Moritoki Y, Hirokawa M, Matsuwaki Y, et al. Eosinophil extracellular trap cell death-derived DNA traps: their presence in secretions and functional attributes. J Allergy Clin Immunol. 2016;137:258–267. doi: 10.1016/j.jaci.2015.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gevaert E, Zhang N, Krysko O, Lan F, Holtappels G, De Ruyck N, et al. Extracellular eosinophilic traps in association with Staphylococcus aureus at the site of epithelial barrier defects in patients with severe airway inflammation. J Allergy Clin Immunol. 2017;139:1849–1860.e6. doi: 10.1016/j.jaci.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 18.Choi Y, Le Pham D, Lee DH, Lee SH, Kim SH, Park HS. Biological function of eosinophil extracellular traps in patients with severe eosinophilic asthma. Exp Mol Med. 2018;50:104. doi: 10.1038/s12276-018-0136-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simons M, Raposo G. Exosomes--vesicular carriers for intercellular communication. Curr Opin Cell Biol. 2009;21:575–581. doi: 10.1016/j.ceb.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Maas SL, Breakefield XO, Weaver AM. Extracellular vesicles: unique intercellular delivery vehicles. Trends Cell Biol. 2017;27:172–188. doi: 10.1016/j.tcb.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becker A, Thakur BK, Weiss JM, Kim HS, Peinado H, Lyden D. Extracellular vesicles in cancer: cell-to-cell mediators of metastasis. Cancer Cell. 2016;30:836–848. doi: 10.1016/j.ccell.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi Y, Kwon Y, Kim DK, Jeon J, Jang SC, Wang T, et al. Gut microbe-derived extracellular vesicles induce insulin resistance, thereby impairing glucose metabolism in skeletal muscle. Sci Rep. 2015;5:15878. doi: 10.1038/srep15878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chelakkot C, Choi Y, Kim DK, Park HT, Ghim J, Kwon Y, et al. Akkermansia muciniphila-derived extracellular vesicles influence gut permeability through the regulation of tight junctions. Exp Mol Med. 2018;50:e450. doi: 10.1038/emm.2017.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi Y, Park H, Park HS, Kim YK. Extracellular vesicles, a key mediator to link environmental microbiota to airway immunity. Allergy Asthma Immunol Res. 2017;9:101–106. doi: 10.4168/aair.2017.9.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vlassov AV, Magdaleno S, Setterquist R, Conrad R. Exosomes: current knowledge of their composition, biological functions, and diagnostic and therapeutic potentials. Biochim Biophys Acta. 2012;1820:940–948. doi: 10.1016/j.bbagen.2012.03.017. [DOI] [PubMed] [Google Scholar]
- 26.Cañas JA, Sastre B, Mazzeo C, Fernández-Nieto M, Rodrigo-Muñoz JM, González-Guerra A, et al. Exosomes from eosinophils autoregulate and promote eosinophil functions. J Leukoc Biol. 2017;101:1191–1199. doi: 10.1189/jlb.3AB0516-233RR. [DOI] [PubMed] [Google Scholar]
- 27.Akuthota P, Carmo LA, Bonjour K, Murphy RO, Silva TP, Gamalier JP, et al. Extracellular microvesicle production by human eosinophils activated by “Inflammatory” stimuli. Front Cell Dev Biol. 2016;4:117. doi: 10.3389/fcell.2016.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hiemstra PS, McCray PB, Jr, Bals R. The innate immune function of airway epithelial cells in inflammatory lung disease. Eur Respir J. 2015;45:1150–1162. doi: 10.1183/09031936.00141514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schleimer RP, Kato A, Kern R, Kuperman D, Avila PC. Epithelium: at the interface of innate and adaptive immune responses. J Allergy Clin Immunol. 2007;120:1279–1284. doi: 10.1016/j.jaci.2007.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitchell PD, O’Byrne PM. Epithelial-derived cytokines in asthma. Chest. 2017;151:1338–1344. doi: 10.1016/j.chest.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 31.Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma. From bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000;161:1720–1745. doi: 10.1164/ajrccm.161.5.9903102. [DOI] [PubMed] [Google Scholar]
- 32.Mascia K, Borish L, Patrie J, Hunt J, Phillips CD, Steinke JW. Chronic hyperplastic eosinophilic sinusitis as a predictor of aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2005;94:652–657. doi: 10.1016/S1081-1206(10)61323-3. [DOI] [PubMed] [Google Scholar]
- 33.Wright JR. Immunoregulatory functions of surfactant proteins. Nat Rev Immunol. 2005;5:58–68. doi: 10.1038/nri1528. [DOI] [PubMed] [Google Scholar]
- 34.Reid KB. Interactions of surfactant protein D with pathogens, allergens and phagocytes. Biochim Biophys Acta. 1998;1408:290–295. doi: 10.1016/s0925-4439(98)00074-x. [DOI] [PubMed] [Google Scholar]
- 35.von Bredow C, Hartl D, Schmid K, Schabaz F, Brack E, Reinhardt D, et al. Surfactant protein D regulates chemotaxis and degranulation of human eosinophils. Clin Exp Allergy. 2006;36:1566–1574. doi: 10.1111/j.1365-2222.2006.02598.x. [DOI] [PubMed] [Google Scholar]
- 36.Hartl D, Griese M. Surfactant protein D in human lung diseases. Eur J Clin Invest. 2006;36:423–435. doi: 10.1111/j.1365-2362.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- 37.Mackay RM, Grainge CL, Lau LC, Barber C, Clark HW, Howarth PH. Airway surfactant protein D deficiency in adults with severe asthma. Chest. 2016;149:1165–1172. doi: 10.1016/j.chest.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choi Y, Lee DH, Trinh HK, Ban GY, Park HK, Shin YS, et al. Surfactant protein D alleviates eosinophil-mediated airway inflammation and remodeling in patients with aspirin-exacerbated respiratory disease. Allergy. 2018 doi: 10.1111/all.13458. [DOI] [PubMed] [Google Scholar]
- 39.Baba M, Hong SB, Sharma N, Warren MB, Nickerson ML, Iwamatsu A, et al. Folliculin encoded by the BHD gene interacts with a binding protein, FNIP1, and AMPK, and is involved in AMPK and mTOR signaling. Proc Natl Acad Sci U S A. 2006;103:15552–15557. doi: 10.1073/pnas.0603781103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fröhlich BA, Zeitz C, Mátyás G, Alkadhi H, Tuor C, Berger W, et al. Novel mutations in the folliculin gene associated with spontaneous pneumothorax. Eur Respir J. 2008;32:1316–1320. doi: 10.1183/09031936.00132707. [DOI] [PubMed] [Google Scholar]
- 41.Goncharova EA, Goncharov DA, James ML, Atochina-Vasserman EN, Stepanova V, Hong SB, et al. Folliculin controls lung alveolar enlargement and epithelial cell survival through E-cadherin, LKB1, and AMPK. Cell Reports. 2014;7:412–423. doi: 10.1016/j.celrep.2014.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khabibullin D, Medvetz DA, Pinilla M, Hariharan V, Li C, Hergrueter A, et al. Folliculin regulates cell-cell adhesion, AMPK, and mTORC1 in a cell-type-specific manner in lung-derived cells. Physiol Rep. 2014;2:2. doi: 10.14814/phy2.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Georas SN, Rezaee F. Epithelial barrier function: at the front line of asthma immunology and allergic airway inflammation. J Allergy Clin Immunol. 2014;134:509–520. doi: 10.1016/j.jaci.2014.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pham DL, Trinh TH, Ban GY, Kim SH, Park HS. Epithelial folliculin is involved in airway inflammation in workers exposed to toluene diisocyanate. Exp Mol Med. 2017;49:e395. doi: 10.1038/emm.2017.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Takahashi T, Kato A, Berdnikovs S, Stevens WW, Suh LA, Norton JE, et al. Microparticles in nasal lavage fluids in chronic rhinosinusitis: potential biomarkers for diagnosis of aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2017;140:720–729. doi: 10.1016/j.jaci.2017.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trinh HK, Pham DL, Choi Y, Kim HM, Kim SH, Park HS. Epithelial folliculin enhances airway inflammation in aspirin-exacerbated respiratory disease. Clin Exp Allergy. 2018;48:1464–1473. doi: 10.1111/cea.13253. [DOI] [PubMed] [Google Scholar]
- 47.Jia G, Erickson RW, Choy DF, Mosesova S, Wu LC, Solberg OD, et al. Periostin is a systemic biomarker of eosinophilic airway inflammation in asthmatic patients. J Allergy Clin Immunol. 2012;130:647–654.e10. doi: 10.1016/j.jaci.2012.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bentley JK, Chen Q, Hong JY, Popova AP, Lei J, Moore BB, et al. Periostin is required for maximal airways inflammation and hyperresponsiveness in mice. J Allergy Clin Immunol. 2014;134:1433–1442. doi: 10.1016/j.jaci.2014.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ito Y, Al Mubarak R, Roberts N, Correll K, Janssen W, Finigan J, et al. IL-13 induces periostin and eotaxin expression in human primary alveolar epithelial cells: Comparison with paired airway epithelial cells. PLoS One. 2018;13:e0196256. doi: 10.1371/journal.pone.0196256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hershey GK. IL-13 receptors and signaling pathways: an evolving web. J Allergy Clin Immunol. 2003;111:677–690. doi: 10.1067/mai.2003.1333. [DOI] [PubMed] [Google Scholar]
- 51.Kim MA, Izuhara K, Ohta S, Ono J, Yoon MK, Ban GY, et al. Association of serum periostin with aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2014;113:314–320. doi: 10.1016/j.anai.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 52.Choi Y, Lee DH, Lee JH, Shin YS, Kim SH, Park HS. Immunomodulatory function of surfactant protein D in eosinophilic asthma. Allergy. 2018 doi: 10.1111/all.13588. [DOI] [PubMed] [Google Scholar]
- 53.Buchheit KM, Laidlaw TM. Update on the management of aspirin-exacerbated respiratory disease. Allergy Asthma Immunol Res. 2016;8:298–304. doi: 10.4168/aair.2016.8.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bergmann KC, Zuberbier T, Church MK. Omalizumab in the treatment of aspirin-exacerbated respiratory disease. J Allergy Clin Immunol Pract. 2015;3:459–460. doi: 10.1016/j.jaip.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 55.Pérez-Novo CA, Watelet JB, Claeys C, Van Cauwenberge P, Bachert C. Prostaglandin, leukotriene, and lipoxin balance in chronic rhinosinusitis with and without nasal polyposis. J Allergy Clin Immunol. 2005;115:1189–1196. doi: 10.1016/j.jaci.2005.02.029. [DOI] [PubMed] [Google Scholar]
- 56.Fajt ML, Wenzel SE. Development of new therapies for severe asthma. Allergy Asthma Immunol Res. 2017;9:3–14. doi: 10.4168/aair.2017.9.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Simon RA, Dazy KM, Waldram JD. Aspirin-exacerbated respiratory disease: characteristics and management strategies. Expert Rev Clin Immunol. 2015;11:805–817. doi: 10.1586/1744666X.2015.1039940. [DOI] [PubMed] [Google Scholar]
- 58.Gevaert P, Van Bruaene N, Cattaert T, Van Steen K, Van Zele T, Acke F, et al. Mepolizumab, a humanized anti-IL-5 mAb, as a treatment option for severe nasal polyposis. J Allergy Clin Immunol. 2011;128:989–95.e1. doi: 10.1016/j.jaci.2011.07.056. [DOI] [PubMed] [Google Scholar]
- 59.Gauvreau GM, O’Byrne PM, Boulet LP, Wang Y, Cockcroft D, Bigler J, et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. N Engl J Med. 2014;370:2102–2110. doi: 10.1056/NEJMoa1402895. [DOI] [PubMed] [Google Scholar]
- 60.Guo Z, Wu J, Zhao J, Liu F, Chen Y, Bi L, et al. IL-33 promotes airway remodeling and is a marker of asthma disease severity. J Asthma. 2014;51:863–869. doi: 10.3109/02770903.2014.921196. [DOI] [PubMed] [Google Scholar]
- 61.Bartemes KR, Iijima K, Kobayashi T, Kephart GM, McKenzie AN, Kita H. IL-33-responsive lineage- CD25+ CD44(hi) lymphoid cells mediate innate type 2 immunity and allergic inflammation in the lungs. J Immunol. 2012;188:1503–1513. doi: 10.4049/jimmunol.1102832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim HY, Chang YJ, Subramanian S, Lee HH, Albacker LA, Matangkasombut P, et al. Innate lymphoid cells responding to IL-33 mediate airway hyperreactivity independently of adaptive immunity. J Allergy Clin Immunol. 2012;129:216–27.e1. doi: 10.1016/j.jaci.2011.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oliphant CJ, Barlow JL, McKenzie AN. Insights into the initiation of type 2 immune responses. Immunology. 2011;134:378–385. doi: 10.1111/j.1365-2567.2011.03499.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu T, Kanaoka Y, Barrett NA, Feng C, Garofalo D, Lai J, et al. Aspirin-exacerbated respiratory disease involves a cysteinyl leukotriene-driven IL-33-mediated mast cell activation pathway. J Immunol. 2015;195:3537–3545. doi: 10.4049/jimmunol.1500905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stolarski B, Kurowska-Stolarska M, Kewin P, Xu D, Liew FY. IL-33 exacerbates eosinophil-mediated airway inflammation. J Immunol. 2010;185:3472–3480. doi: 10.4049/jimmunol.1000730. [DOI] [PubMed] [Google Scholar]
- 66.Cook EB, Stahl JL, Schwantes EA, Fox KE, Mathur SK. IL-3 and TNFα increase Thymic Stromal Lymphopoietin Receptor (TSLPR) expression on eosinophils and enhance TSLP-stimulated degranulation. Clin Mol Allergy. 2012;10:8. doi: 10.1186/1476-7961-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Noti M, Wojno ED, Kim BS, Siracusa MC, Giacomin PR, Nair MG, et al. Thymic stromal lymphopoietin-elicited basophil responses promote eosinophilic esophagitis. Nat Med. 2013;19:1005–1013. doi: 10.1038/nm.3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Buchheit KM, Cahill KN, Katz HR, Murphy KC, Feng C, Lee-Sarwar K, et al. Thymic stromal lymphopoietin controls prostaglandin D2 generation in patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2016;137:1566–1576.e5. doi: 10.1016/j.jaci.2015.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]