Abstract
Purpose
Eosinophilic inflammation is a key component of severe asthma (SA). However, there has been no reliable serum biomarker for the eosinophilic inflammation of SA. We hypothesized that serum eosinophil-derived neurotoxin (EDN) could predict the eosinophilic inflammation of SA in adult asthmatics.
Methods
Severe asthmatics (n = 235), nonsevere asthmatics (n = 898), and healthy controls (n = 125) were enrolled from Ajou University Hospital, South Korea. The serum levels of EDN and periostin were measured by enzyme-linked immunosorbent assay and compared between severe and nonsevere asthmatics. Their associations with total eosinophil count (TEC) and clinical parameters were evaluated; clinical validation of the K-EDN kit for the measurement of serum EDN was evaluated.
Results
Severe asthmatics were older and had longer disease duration with significantly lower levels of forced expiratory volume in 1 second and methacholine PC20 than nonsevere asthmatics. Significant differences were found in TEC or sputum eosinophil count (%) between the groups. The serum levels of EDN and periostin were significantly higher in severe asthmatics than in nonsevere asthmatics and in healthy controls (all P < 0.05). Although significant correlations were found between serum EDN levels measured by the 2 kits (ρ = 0.545, P < 0.0001), higher correlation coefficients between serum EDN levels measured by the K-EDN kit and TEC were higher (ρ = 0.358, P < 0.0001) than those between serum EDN levels measured by the MBL kit and TEC (ρ = 0.319, P < 0.0001) or serum periostin level (ρ = 0.222, P < 0.0001). Multivariate regression analysis demonstrated that serum EDN levels measured by the K-EDN kit predicted the phenotype of SA (P = 0.003), while 2 other biomarkers did not.
Conclusions
The serum EDN level may be a useful biomarker for assessing asthma severity in adult asthmatics.
Keywords: Eosinophil-derived neurotoxin, asthma, biomarkers
INTRODUCTION
Asthma is a chronic inflammatory disease of multifactorial etiologies that affects 300 million people worldwide. Initially, asthma was considered typical eosinophilic airway inflammation initiated by allergic sensitization, which results in airway hyperresponsiveness (AHR) and acute bronchoconstriction. Among asthmatic patients, severe asthma (SA) is responsible for more than 50% of the medical expense of asthma, even though it accounts for 5%-10% of entire asthma patients. Severe asthmatics are suffering from frequent exacerbations that contribute to progressive lung function decline and increasing burden of medical cost.1
The eosinophilic phenotype of asthma is related to type 2 cytokines such as interleukin (IL)-4, IL-5, and IL-13. Corticosteroid (CS) is a key anti-inflammatory agent to control eosinophilic inflammation, and biologics targeting type 2 inflammation are effective in SA with high total eosinophil count (TEC).2,3 There have been traditional biomarkers used to monitor eosinophilic inflammation in asthma, including TEC, sputum eosinophil count (%), serum periostin level, and fractional excretion of nitric oxide (FeNO) concentration.4 Not only are sputum eosinophil count and FeNO concentration relatively hard to yield and variable by CS therapy, but also the studies of TEC predicting sputum eosinophil counts in eosinophilic asthma have shown conflicting results.5,6,7,8,9,10 To date, TEC has been suggested to be a biomarker for predicting favorable responses to anti-IL-5 antibody treatment in SA.11,12,13 Since there has been no serum biomarker available that can effectively reflect eosinophilic inflammation in SA, the need to identify an appropriate biomarker is continuously emerging. While periostin has been known to be related to type 2 airway inflammation in asthma, several studies have reported eosinophil-derived neurotoxin (EDN), a degranulation protein released from eosinophils, is deemed to represent eosinophil activation in childhood asthma and atopic dermatitis, and its value as a serum biomarker has not yet been evaluated in adult severe asthmatics.14,15
We hypothesized that serum EDN could predict SA. This study aimed to analyze the association of serum EDN with eosinophil-related clinical parameters, including TEC, and serum periostin level in patients with SA as compared to those with nonsevere asthma (NSA). It also aimed to validate the new enzyme-linked immunosorbent assay (ELISA) kit developed in this country.
MATERIALS AND METHODS
Study populations
A total of 1,133 Korean adult asthmatic patients, including 898 severe and 235 nonsevere asthmatics, were enrolled in the study. The study populations included 125 normal controls (NCs) without known allergic diseases. Allergy specialists diagnosed asthma according to the Global Initiative for Asthma guideline. The subjects were classified into the SA and NSA groups by the International European Respiratory Society/American Thoracic Society guidelines.16 Any patient who had known to have underlying respiratory diseases other than asthma was excluded. All participants provided written informed consent before participating in this study, and Ajou University Institutional Review Board approval was obtained (AJIRB-GEN-SMP-13-108).
The demographic characteristics of the study subjects were collected, including age, sex, smoking history, and the duration of asthma. Atopy was defined as at least 1 positive reaction to a skin prick test of 55 common inhalant allergens (Bencard Co., Brentford, UK), in which a positive reaction was defined as the ratio of the mean diameter of wheal of the allergen to histamine was 1 or higher. Chronic rhinosinusitis and nasal polyps were diagnosed with paranasal sinus radiography, computed tomography, and rhinoscopic findings. Pulmonary function test was completed as previously described.17 Methacholine bronchial challenge test was performed using double doses of Provocholine® (methacholine chloride USP, Methapharm Inc., Brantford, Canada) from 1 to 16 mg/mL. Serum total immunoglobulin E (IgE), serum specific IgE, and serum eosinophil cationic protein (ECP) levels were measured by the UniCAP® system (ThermoFisher Scientific, Waltham, MA, USA). Serum samples were collected at the initial visit and frozen at −70°C; on initial evaluation, they were thawed immediately before use. Sputum eosinophil and neutrophil counts were expressed as the percentage of the cells among nonsquamous cells in the samples.
Measurement of serum EDN and serum periostin
The serum levels of EDN were measured using 2 different ELISA kits, following each manufacturer's protocol. The one is a commercial kit that has already been used for the measurement of EDN (MBL International, Woburn, MA, USA), and the other is a newly developed kit named the K-EDN kit (SKIMS-BIO Co., Seoul, Korea). Their measurements were taken as previously described.18 As another biomarker for eosinophilic inflammation, serum periostin levels were measured simultaneously using ELISA (Shino-Test, Kanagawa, Japan) as previously described.19
Statistical analysis
The Mann-Whitney U test and the χ2 test were used to compare the unpaired continuous and dichotomous variables. Spearman rank correlation analysis defined correlations among the continuous variables. Logistic regression analyses identified the contributions of continuous and dichotomous variables to SA. All statistical analyses were performed by using IBM SPSS software version 18.0 (IBM Corp., Armonk, NY, USA). P values of < 0.05 were considered statistically significant.
RESULTS
Demographic and clinical characteristics
Demographic and clinical parameters of the study subjects were compared (Table 1). Severe asthmatics were older (46.01 ± 13.93 vs. 42.69 ± 14.63 years, P = 0.001) and had more frequent smoking history (57.4% vs. 45.9%, P = 0.023) and longer asthma duration (8.04 ± 6.61 vs. 5.72 ± 10.56 years, P < 0.0001) compared to nonsevere asthmatics. They had higher prevalences of upper airway comorbidities such as chronic rhinosinusitis (50.0% vs. 35.0%, P = 0.008) and nasal polyps (41.7% vs. 28.0%, P = 0.007). However, no difference was noted in the proportion of female sex or atopy between severe and nonsevere asthmatics (62.55% vs. 61.87%, P = 0.848; 53.33% vs. 54.48%, P = 0.885, respectively). Severe asthmatics had lower levels of baseline forced expiratory volume in 1 second (FEV1; 71.38% ± 21.81% vs. 89.75% ± 20.29%, P < 0.001) and lower methacholine PC20 levels (7.37 ± 12.15 vs. 10.79 ± 20.09 mg/mL, P = 0.042). While log-transformed serum total IgE level was not significantly different (2.27 ± 0.55 vs. 2.20 ± 0.64, P = 0.248), log-transformed TEC was measured higher in severe asthmatics (2.53 ± 0.44 vs. 2.39 ± 0.47, P = 0.002). Sputum eosinophil count was identified higher in severe asthmatics (26.95% ± 35.59% vs. 22.11% ± 33.15%, P = 0.031), whereas sputum neutrophil count was not different between the groups (56.62% ± 35.29% vs. 58.90% ± 33.84%, P = 0.558). Both serum ECP level (44.52 ± 45.95 µg/L vs. 31.99 ± 38.46 µg/L, P < 0.0001) and serum periostin level (91.56 ± 41.21 ng/mL vs. 77.72 ± 38.56 ng/mL, P = 0.001) were measured higher in severe asthmatics than in nonsevere asthmatics.
Table 1. Comparisons of clinical characteristics and eosinophil biomarkers between severe and nonsevere asthmatics.
| Variables | Severe asthmatics (n = 235) | Non severe asthmatics (n = 898) | P value |
|---|---|---|---|
| Age (yr) | 46.01 ± 13.93 | 42.69 ± 14.63 | 0.001 |
| Sex (female, %) | 62.6 | 61.9 | 0.848 |
| Atopy (%) | 54.4 | 54.9 | 0.885 |
| Smoking history (current and ex-smoker, %) | 57.4 | 45.9 | 0.023 |
| Duration of asthma (yr) | 8.04 ± 6.61 | 5.72 ± 10.56 | < 0.0001 |
| Chronic rhinosinusitis (%) | 50.0 | 35.0 | 0.008 |
| Nasal polyp (%) | 41.7 | 28.0 | 0.007 |
| Log (baseline FEV1) | 1.83 ± 0.15 | 1.94 ± 0.12 | < 0.0001 |
| Log (methacholine PC20) | 0.40 ± 0.67 | 0.53 ± 0.73 | 0.042 |
| Log (total IgE) | 2.27 ± 0.55 | 2.20 ± 0.64 | 0.248 |
| Log (total eosinophil count) | 2.53 ± 0.44 | 2.39 ± 0.47 | 0.002 |
| Sputum eosinophil (%) | 26.95 ± 35.59 | 22.11 ± 33.15 | 0.031 |
| Sputum neutrophil (%) | 56.62 ± 35.29 | 58.90 ± 33.84 | 0.558 |
| Serum ECP (µg/L) | 44.52 ± 45.95 | 31.99 ± 38.46 | < 0.0001 |
| Serum EDN (MBL) (ng/mL) | 69.08 ± 42.40 | 58.46 ± 35.56 | 0.034 |
| Serum EDN (K-EDN) (ng/mL) | 157.75 ± 128.18 | 109.02 ± 104.12 | 0.001 |
| Serum periostin (ng/mL) | 91.56 ± 41.21 | 77.72 ± 38.56 | 0.001 |
Each value is presented as mean ± standard deviation or %.
FEV1, forced expiratory volume in 1 second; PC20, provocation concentration causing a 20% fall in FEV1; Log (total IgE), log-transformed serum total immunoglobulin E levels; Log (total eosinophil count), log-transformed total eosinophil count; ELISA, enzyme-linked immunosorbent assay; EDN, eosinophil-derived neurotoxin; Serum EDN (MBL), serum EDN levels measured by ELISA kit of MBL; Serum EDN (K-EDN), serum EDN levels measured by ELISA kit of K-EDN.
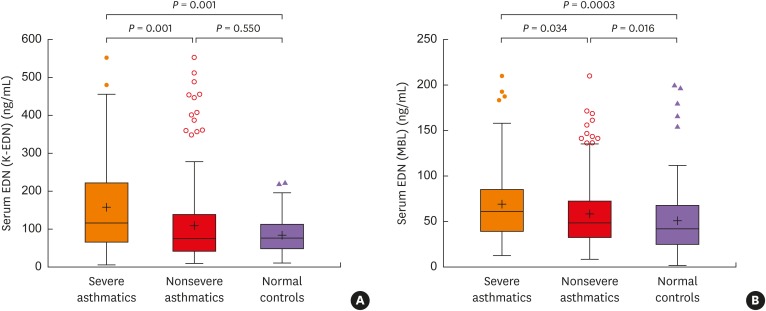
Comparison of serum EDN levels measured by the 2 different ELISA kits
Serum EDN levels measured by both MBL and K-EDN kits were higher in severe asthmatics (69.08 ± 42.40 vs. 58.46 ± 35.56 ng/mL, P = 0.034; 157.75 ± 128.18 vs. 109.02 ± 104.12 ng/mL, P = 0.001, respectively), while no difference was found between nonsevere asthmatics and NCs (P = 0.55) as shown in Fig. 1. Although a significant correlation was found between serum EDN levels measured by the 2 ELISA kits (ρ = 0.545; P < 0.0001), the mean serum EDN level was found to be higher by the K-EDN kit than by the MBL kit in all study subjects. Serum EDN levels measured by the MBL kit showed a significant difference between severe and nonsevere asthmatics, but they were not so significant as serum EDN levels measured by the K-EDN kit (P = 0.034 and P = 0.001, respectively; Fig. 1). The mean age of NCs was 51.1 years, which was older than that of severe or nonsevere asthmatics. Analysis of covariance was performed to identify the contribution of age to the serum EDN levels measured by the K-EDN kit, but no significant impact was observed (P = 0.104).
Fig. 1. (A) Comparison of serum EDN levels measured by the K-EDN kit among severe asthmatics, nonsevere asthmatics, and NCs. (B) Comparison of serum EDN levels measured by the MBL kit between severe asthmatics, nonsevere asthmatics, and NCs.
EDN, eosinophil-derived neurotoxin; NC, normal control.
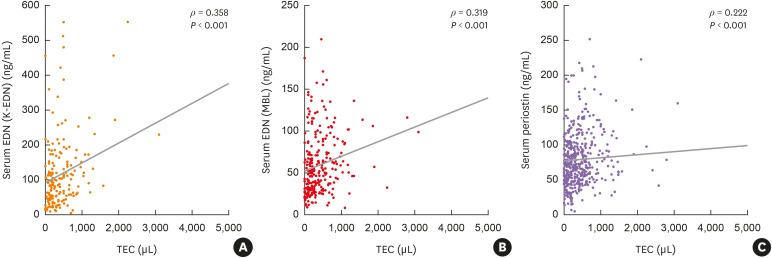
Association of serum EDN with clinical parameters including TEC
When correlations between serum EDN levels measured by the 2 kits and TEC were evaluated, serum EDN levels measured by the K-EDN kit showed a higher correlation coefficient (ρ = 0.358, P < 0.001, Fig. 2A) than that measured by the MBL kit (ρ = 0.319, P < 0.001, Fig. 2B). Serum periostin levels were less correlated to TEC than serum EDN levels measured by the 2 kits (ρ = 0.222, P < 0.0001, Fig. 2C). Significant correlations were found between serum EDN levels measured by the 2 kits and serum periostin levels (ρ = 0.304, P < 0.0001 for serum EDN levels measured by K-EDN kit; ρ = 0.302, P < 0.0001 for serum EDN levels measured by MBL kit), but less correlated to TEC. Serum EDN levels measured by the 2 kits were significantly correlated (ρ = 0.545, P < 0.0001). Serum ECP levels were correlated to TEC (ρ = 0.302, P < 0.0001); they were less correlated to TEC than serum EDN levels were. There was no significant correlation between ECP levels and serum periostin levels (ρ = 0.083 and P = 0.083, respectively). Either serum ECP, EDN levels measured by the 2 kits or periostin levels were not correlated to sputum eosinophil count.
Fig. 2. Correlation between the eosinophilic biomarkers in total asthmatics. (A) TEC and serum EDN levels measured by the K-EDN kit. (B). TEC and serum EDN levels measured by the MBL kit. (C) TEC and serum periostin levels.
EDN, eosinophil-derived neurotoxin; TEC, total eosinophil count.
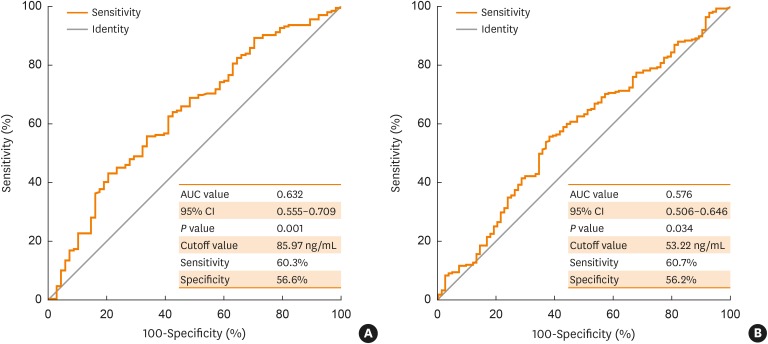
Serum EDN level as a biomarker of SA
The receiver operating characteristic curves of serum EDN levels measured by the 2 kits were obtained to predict the phenotype of SA. Serum EDN levels measured by the K-EDN kit showed a higher area under the curve (AUC) value with statistical significance (AUC value: 0.632, P = 0.002 at the cutoff value of 85.97 ng/mL with 60.3% of sensitivity and 56.6% of specificity, Fig. 3A) than those measured by the MBL kit (AUC value: 0.576, P = 0.034 at the cutoff value of 53.22 ng/mL with 60.7% of sensitivity and 56.2% of specificity, Fig. 3B). In addition, the predictability of each clinical parameter for SA was analyzed using univariate and multivariate logistic regression analyses (Table 2). Serum EDN levels measured by both K-EDN and MBL kits as well as serum ECP and periostin levels were identified to be significant parameters associated with SA in the univariate analysis (all P < 0.05). However, multivariate analysis showed that serum EDN levels measured by the K-EDN kit remained a significant parameter (P = 0.003) for predicting the phenotype of SA.
Fig. 3. (A) ROC curves for the serum EDN levels measured by the K-EDN kit in the prediction of severe asthma in the total asthmatics. (B) ROC curves for the serum EDN levels measured by the MBL kit in the prediction of severe asthma in the total asthmatics.
ROC, receiver operating characteristic; EDN, eosinophil-derived neurotoxin; AUC, area under the curve; CI, confidence interval.
Table 2. Predictability for severe asthma by univariate and multivariate logistic regression analyses.
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Duration of asthma | 1.016 (0.995–1.038) | 0.131 | - | - |
| Total IgE (IU/L) | 1.000 (1.000–1.000) | 0.694 | - | - |
| Total eosinophil count (/uL) | 1.000 (1.000–1.000) | 0.116 | - | - |
| Sputum eosinophil count (%) | 1.004 (0.998–1.011) | 0.207 | - | - |
| Sputum neutrophil count (%) | 0.998 (0.991–1.005) | 0.586 | - | - |
| Serum ECP (µg/L) | 1.007 (1.002–1.011) | 0.002 | - | - |
| Serum periostin (ng/mL) | 1.008 (1.003–1.013) | 0.001 | - | - |
| Serum EDN (MBL) (ng/mL) | 1.007 (1.001–1.013) | 0.025 | - | - |
| Serum EDN (K-EDN) (ng/mL) | 1.003 (1.001–1.006) | 0.003 | 1.004 (1.002–1.007) | 0.003 |
CI, confidence interval; IgE, immunoglobulin E; ECP, eosinophil cationic protein; EDN, eosinophil-derived neurotoxin; ELISA, enzyme-linked immunosorbent assay; Serum EDN (MBL), serum EDN levels measured by ELISA kit of MBL; Serum EDN (K-EDN), serum EDN levels measured by ELISA kit of K-EDN; OR, odds ratio.
The total study subjects were divided into 2 groups (high responders and low responders) according to each cutoff value of 85.97 ng/mL for the K-EDN kit and 54.22 ng/mL for the MBL kit; their demographic and clinical characteristics were compared (data not shown). The high-responders of the K-EDN showed a higher prevalence of SA (31.5% vs. 18.9%, P = 0.016) as well as a lower log-transformed baseline FEV1 level (1.92 ± 0.11 vs. 1.95 ± 1.00, P = 0.019) compared to low-responders of the K-EDN. They also had higher log-transformed TEC and sputum eosinophil count (2.58 ± 0.46 vs. 2.35 ± 0.41, P < 0.0001; 28.59% ± 37.37% vs. 18.14% ± 31.79%, P = 0.044, respectively), and lower serum ECP (52.83 ± 46.30 µg/L vs. 31.65 ± 32.62 µg/L, P < 0.0001) and periostin (95.88 ± 44.74 ng/mL vs. 73.63 ± 36.16 ng/mL, P < 0.0001) levels; methacholine PC20 levels and sputum neutrophil counts had no differences (P = 0.813 and P = 0.960, respectively). The high-responder group of the MBL kit had similar results of higher SA prevalence (29.8% vs. 17.6%, P = 0.007), lower log-transformed baseline FEV1 level (1.92 ± 0.12 vs. 1.96 ± 0.09, P = 0.003), higher log-transformed TEC and sputum eosinophil count (2.58 ± 0.44 vs. 2.32 ± 0.45, P < 0.0001; 28.75% ± 37.49% vs. 17.64% ± 30.83%, P = 0.025, respectively), as well as higher serum ECP and periostin level (47.97 ± 44.33 µg/L vs. 33.19 ± 37.38 µg/L, P < 0.0001; 92.83 ± 40.59 ng/mL vs. 74.66 ± 39.49 ng/mL, P < 0.0001, respectively). Additionally, they had a higher female proportion and a lower log-transformed methacholine PC20 level compared to low responders of MBL kit (55.6% vs. 68.4%, P = 0.012; 0.57 ± 0.63 vs. 0.77 ± 0.58, P = 0.009, respectively).
DISCUSSION
Eosinophils are key cells in the airway inflammation of SA and associated with persistent elevation of type 2 inflammatory markers. Since increased expression of periostin in serum/tissue has been suggested to be a biomarker for type 2 inflammation in adult asthmatic patients,20 our previous study demonstrated that adult asthmatics with SA had significantly higher serum periostin levels, indicating that serum periostin is a biomarker for type 2 inflammation in adult asthmatics.4 However, the present study showed that the serum periostin level was not correlated with TEC, whereas TEC is a marker for determining anti-IL-5 antibody treatment for SA patients. It is necessary to establish a useful serum biomarker for assessing the degree of type-2 airway inflammation in the management of SA.21,22 There have been a few studies suggesting the serum EDN level to be a biomarker for asthma severity in childhood.23 This is the first study to suggest that the serum EDN level is a useful serum biomarker for assessing the severity of SA in adult asthmatics. The serum EDN level was significantly higher in patients with SA than in those with NSA; the significant correlation coefficient was noted between TEC and serum EDN measured by the K-EDN kit compared to those by the MBL kit, and between TEC and serum periostin/ECP levels. In addition, multivariate analysis showed that serum EDN levels measured by the K-EDN kit remained a single significant parameter for predicting SA.
Recent large-scale studies have led to a better understanding of the characteristics of SA. They proved distinct demographic/clinical characteristics consistently relevant to SA; older age, possible associations with female sex and smoking, frequent exacerbations, low baseline lung function, atopy rate, need for high doses of inhaled or systemic CS, and higher prevalence of upper and lower respiratory comorbidities.24,25,26 We confirmed that the characteristics of severe asthmatics in this study were consistent with these findings. However, no differences were noted in the female sex and atopy. It also showed that lower lung function and increased AHR are key features of SA. Moreover, it was noted that eosinophilic inflammation was another key feature of SA in this study. Serum EDN levels measured by the K-EDN and MBL kits as well as TEC, sputum eosinophil count, serum periostin, and serum ECP levels were significantly higher in severe asthmatics than in nonsevere asthmatics. These findings confirmed that eosinophilia in blood/airway secretion is the key feature of SA in adult asthmatics. TEC and sputum eosinophilia (>3%) have been used to define eosinophilic asthma.27,28,29 A previous study demonstrated that adult asthmatics with more than 300/µL of TEC had the highest tendency of asthma exacerbation among cutoff values of 200 to 400/µL.30 Still, another study demonstrated that TEC was rarely correlated with eosinophilia in bronchoalveolar lavage (BAL) fluid or endobronchial biopsies in patients with SA.31 It is not practical to differentiate phenotypes using these parameters, since the phenotypes vary widely among patients and depend on clinical severity and medications used.26,32,33 Due to these clinical characteristics of SA, clinically applicable serum biomarkers that reflect eosinophilic inflammation are necessary to keep severe asthmatics from exacerbation and lung function decline.
It is essential to distinguish phenotypes between eosinophilic and noneosinophilic asthmatics because the more severe eosinophilic inflammation, the higher risk of asthma exacerbation which develops SA. Effective control of eosinophilic inflammation has proved beneficial to reduce asthma exacerbation.34,35,36,37 As the phenotype of eosinophilic asthma has been determined by sputum eosinophil counts, sputum induction carries a risk of asthma exacerbation, especially in severe asthmatics, and it is not always successful because of its variability.38 In addition, lab facilities and expertise are required to analyze sputum samples. For this reason, a serum biomarker, which is stable and reproducible to represent type 2 inflammation, is considered useful as it is relatively safe and easy-to-access in real clinical practice. Among eosinophil-derived molecules, EDN is known to be relatively cheap and stable to measure. Elevated EDN levels were found in serum, urine, and other body fluids in patients with eosinophil-associated diseases.39 The serum EDN level was the only marker for differentiating childhood asthmatics with acute exacerbation from those in stable status, showing a greater correlation with the severity of asthma when compared to serum ECP levels or TEC.23 In addition, it was correlated with the degree of persistent airflow limitation in allergic asthmatics.40 Our previous study investigated that peripheral blood eosinophils and serum EDN levels were elevated in SA, which was attributed to increased eosinophil extracellular traps that promoted the degranulation of eosinophils. A significnat correlation was found between extracellular trap-contating eosinophils and EDN levels.41 We found that the serum EDN level was significantly higher in severe asthmatics than in nonsevere asthmatics; especially, serum EDN level measured by the K-EDN kit are more significantly elevated in severe asthmatics than those measured by the MBL kit. We also observed that serum EDN levels measured by the K-EDN kit was significantly elevated in severe asthmatics compared to NCs, while no difference was found between nonsevere asthmatics and NCs or between total asthmatics and NCs. Additionally, serum EDN levels measured by the K-EDN kit showed a better correlation to TEC than those measured by the MBL kit or serum periostin levels. Moreover, serum EDN levels measured by the K-EDN kit could predict SA best among other clinical parameters. Periostin is known as a type 2 inflammation marker, but it is mainly released from airway epithelial cells affected by IL-13 and various stimuli, but not from eosinophils. In the present study, a relatively weak correlation was found between the serum periostin and TEC levels. In patients with SA, furthermore, periostin is more valuable in evaluating eosinophil activation status than in evaluating peripheral eosinophil count. When eosinophils are activated, they release several mediators including MBP, ECP, and EDN. To date, we cannot measure serum MBP levels using a kit. Several studies showed confounding results of serum ECP level as a biomarker for asthma and other allergic diseases.15,42,43 Serum ECP level can be measured using commercially available kits, although their cost is expensive. In the present study, a significantly higher serum ECP level was noted in severe asthmatics than in nonsevere asthmatics; however, a lower correlation was found with TEC. ECP is also a highly charged protein with sticky quality; therefore, it is likely to adhere to the wall of a sample tube or other substances. Therefore, its level is variable from each measurement. These findings suggest that the serum EDN level can be applied as a stable serum biomarker for better assessing the severity of eosinophilic inflammation, especially in SA.
There are several limitations in this study. First, it is a cross-sectional study in a single tertiary center. Although the number of subjects was not small, replicated experiments in other subjects' samples are needed to enhance and consolidate the hypothesis. Secondly, it was difficult to control the medications such as inhaled/systemic CS that could affect eosinophilic inflammation status in the study subjects. Thirdly, further investigations are required to explore the exact function of EDN (difference from periostin) and other inflammatory mechanisms than eosinophilic inflammation in the pathogenesis of SA. Airway neutrophilia was documented in patients with severe exacerbations, but its role in SA remains to be elucidated.44 A few studies demonstrated increased IL-17 levels in samples (induced sputum, BAL samples, and bronchial biopsies) of severe asthmatics.45,46,47 In another study, IL-17-producing cells and IL-17-related gene expression signature were increased and orthogonal to eosinophilic inflammation in SA.48 Some patients with SA have mixed cellular profiles (both sputum eosinophilia and neutrophilia). Our previous report demonstrated increased expression of neutrophil extracellular traps (NETs) in severe asthmatics compared to nonsevere asthmatics. NETs were found to induce eosinophil activation, suggesting a close interaction between these 2 inflammatory cells.49 Follow-up studies are essential to evaluate the clinical significance of serum EDN, treatment response to anti-inflammatory medications, and long-term outcomes in SA.
The results of this study suggest that the serum EDN level can help identify SA in adult asthmatics. Considering that SA has heterogeneous phenotypes, further studies are needed to identify useful biomarkers for assessing subtypes and long-term clinical outcome of SA.
ACKNOWLEDGMENTS
This study was supported by a grant (HI16C0992 and HI14C2628) from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Korea. We appreciate to SKIMS-BIO Co. (Seoul, Korea) to provide the K-EDN kit to measure serum EDN levels in this study.
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
References
- 1.Yoo KH, Ahn HR, Park JK, Kim JW, Nam GH, Hong SK, et al. Burden of respiratory disease in Korea: an observational study on allergic rhinitis, asthma, COPD, and rhinosinusitis. Allergy Asthma Immunol Res. 2016;8:527–534. doi: 10.4168/aair.2016.8.6.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3:355–366. doi: 10.1016/S2213-2600(15)00042-9. [DOI] [PubMed] [Google Scholar]
- 3.Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–659. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 4.Kim MA, Izuhara K, Ohta S, Ono J, Yoon MK, Ban GY, et al. Association of serum periostin with aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2014;113:314–320. doi: 10.1016/j.anai.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Pin I, Freitag AP, O'Byrne PM, Girgis-Gabardo A, Watson RM, Dolovich J, et al. Changes in the cellular profile of induced sputum after allergen-induced asthmatic responses. Am Rev Respir Dis. 1992;145:1265–1269. doi: 10.1164/ajrccm/145.6.1265. [DOI] [PubMed] [Google Scholar]
- 6.Pizzichini MM, Pizzichini E, Clelland L, Efthimiadis A, Mahony J, Dolovich J, et al. Sputum in severe exacerbations of asthma: kinetics of inflammatory indices after prednisone treatment. Am J Respir Crit Care Med. 1997;155:1501–1508. doi: 10.1164/ajrccm.155.5.9154849. [DOI] [PubMed] [Google Scholar]
- 7.Silkoff PE, McClean P, Spino M, Erlich L, Slutsky AS, Zamel N. Dose-response relationship and reproducibility of the fall in exhaled nitric oxide after inhaled beclomethasone dipropionate therapy in asthma patients. Chest. 2001;119:1322–1328. doi: 10.1378/chest.119.5.1322. [DOI] [PubMed] [Google Scholar]
- 8.Wagener AH, de Nijs SB, Lutter R, Sousa AR, Weersink EJ, Bel EH, et al. External validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthma. Thorax. 2015;70:115–120. doi: 10.1136/thoraxjnl-2014-205634. [DOI] [PubMed] [Google Scholar]
- 9.Hastie AT, Moore WC, Li H, Rector BM, Ortega VE, Pascual RM, et al. Biomarker surrogates do not accurately predict sputum eosinophil and neutrophil percentages in asthmatic subjects. J Allergy Clin Immunol. 2013;132:72–80. doi: 10.1016/j.jaci.2013.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schleich FN, Manise M, Sele J, Henket M, Seidel L, Louis R. Distribution of sputum cellular phenotype in a large asthma cohort: predicting factors for eosinophilic vs neutrophilic inflammation. BMC Pulm Med. 2013;13:11. doi: 10.1186/1471-2466-13-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldman M, Hirsch I, Zangrilli JG, Newbold P, Xu X. The association between blood eosinophil count and benralizumab efficacy for patients with severe, uncontrolled asthma: subanalyses of the Phase III SIROCCO and CALIMA studies. Curr Med Res Opin. 2017;33:1605–1613. doi: 10.1080/03007995.2017.1347091. [DOI] [PubMed] [Google Scholar]
- 12.Corren J, Weinstein S, Janka L, Zangrilli J, Garin M. Phase 3 study of reslizumab in patients with poorly controlled asthma: effects across a broad range of eosinophil counts. Chest. 2016;150:799–810. doi: 10.1016/j.chest.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 13.Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med. 2016;4:549–556. doi: 10.1016/S2213-2600(16)30031-5. [DOI] [PubMed] [Google Scholar]
- 14.Kim CK. Eosinophil-derived neurotoxin: a novel biomarker for diagnosis and monitoring of asthma. Korean J Pediatr. 2013;56:8–12. doi: 10.3345/kjp.2013.56.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taniuchi S, Chihara J, Kojima T, Yamamoto A, Sasai M, Kobayashi Y. Serum eosinophil derived neurotoxin may reflect more strongly disease severity in childhood atopic dermatitis than eosinophil cationic protein. J Dermatol Sci. 2001;26:79–82. doi: 10.1016/s0923-1811(00)00151-1. [DOI] [PubMed] [Google Scholar]
- 16.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–373. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 17.Kim SH, Yang EM, Lee HN, Choi GS, Ye YM, Park HS. Association of the CCR3 gene polymorphism with aspirin exacerbated respiratory disease. Respir Med. 2010;104:626–632. doi: 10.1016/j.rmed.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 18.Kim CK, Callaway Z, Park JS, Kwon E. Utility of serum eosinophil-derived neurotoxin (EDN) measurement by ELISA in young children with asthma. Allergol Int. 2017;66:70–74. doi: 10.1016/j.alit.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Masuoka M, Shiraishi H, Ohta S, Suzuki S, Arima K, Aoki S, et al. Periostin promotes chronic allergic inflammation in response to Th2 cytokines. J Clin Invest. 2012;122:2590–2600. doi: 10.1172/JCI58978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parulekar AD, Atik MA, Hanania NA. Periostin, a novel biomarker of TH2-driven asthma. Curr Opin Pulm Med. 2014;20:60–65. doi: 10.1097/MCP.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 21.Corren J, Lemanske RF, Jr, Hanania NA, Korenblat PE, Parsey MV, Arron JR, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365:1088–1098. doi: 10.1056/NEJMoa1106469. [DOI] [PubMed] [Google Scholar]
- 22.Fajt ML, Gelhaus SL, Freeman B, Uvalle CE, Trudeau JB, Holguin F, et al. Prostaglandin D2 pathway upregulation: relation to asthma severity, control, and TH2 inflammation. J Allergy Clin Immunol. 2013;131:1504–1512. doi: 10.1016/j.jaci.2013.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim CK, Callaway Z, Fletcher R, Koh YY. Eosinophil-derived neurotoxin in childhood asthma: correlation with disease severity. J Asthma. 2010;47:568–573. doi: 10.3109/02770901003792833. [DOI] [PubMed] [Google Scholar]
- 24.European Network for Understanding Mechanisms of Severe Asthma. The ENFUMOSA cross-sectional European multicentre study of the clinical phenotype of chronic severe asthma. Eur Respir J. 2003;22:470–477. doi: 10.1183/09031936.03.00261903. [DOI] [PubMed] [Google Scholar]
- 25.Dolan CM, Fraher KE, Bleecker ER, Borish L, Chipps B, Hayden ML, et al. Design and baseline characteristics of the epidemiology and natural history of asthma: Outcomes and Treatment Regimens (TENOR) study: a large cohort of patients with severe or difficult-to-treat asthma. Ann Allergy Asthma Immunol. 2004;92:32–39. doi: 10.1016/S1081-1206(10)61707-3. [DOI] [PubMed] [Google Scholar]
- 26.Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol. 2007;119:405–413. doi: 10.1016/j.jaci.2006.11.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belda J, Leigh R, Parameswaran K, O'Byrne PM, Sears MR, Hargreave FE. Induced sputum cell counts in healthy adults. Am J Respir Crit Care Med. 2000;161:475–478. doi: 10.1164/ajrccm.161.2.9903097. [DOI] [PubMed] [Google Scholar]
- 28.Spanevello A, Confalonieri M, Sulotto F, Romano F, Balzano G, Migliori GB, et al. Induced sputum cellularity. Reference values and distribution in normal volunteers. Am J Respir Crit Care Med. 2000;162:1172–1174. doi: 10.1164/ajrccm.162.3.9908057. [DOI] [PubMed] [Google Scholar]
- 29.Thomas RA, Green RH, Brightling CE, Birring SS, Parker D, Wardlaw AJ, et al. The influence of age on induced sputum differential cell counts in normal subjects. Chest. 2004;126:1811–1814. doi: 10.1378/chest.126.6.1811. [DOI] [PubMed] [Google Scholar]
- 30.Tran TN, Khatry DB, Ke X, Ward CK, Gossage D. High blood eosinophil count is associated with more frequent asthma attacks in asthma patients. Ann Allergy Asthma Immunol. 2014;113:19–24. doi: 10.1016/j.anai.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 31.Ullmann N, Bossley CJ, Fleming L, Silvestri M, Bush A, Saglani S. Blood eosinophil counts rarely reflect airway eosinophilia in children with severe asthma. Allergy. 2013;68:402–406. doi: 10.1111/all.12101. [DOI] [PubMed] [Google Scholar]
- 32.Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu W, Bleecker E, Moore W, Busse WW, Castro M, Chung KF, et al. Unsupervised phenotyping of Severe Asthma Research Program participants using expanded lung data. J Allergy Clin Immunol. 2014;133:1280–1288. doi: 10.1016/j.jaci.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. 2008;178:218–224. doi: 10.1164/rccm.200711-1754OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Bradding P, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet. 2002;360:1715–1721. doi: 10.1016/S0140-6736(02)11679-5. [DOI] [PubMed] [Google Scholar]
- 36.Jayaram L, Pizzichini MM, Cook RJ, Boulet LP, Lemière C, Pizzichini E, et al. Determining asthma treatment by monitoring sputum cell counts: effect on exacerbations. Eur Respir J. 2006;27:483–494. doi: 10.1183/09031936.06.00137704. [DOI] [PubMed] [Google Scholar]
- 37.Chlumský J, Striz I, Terl M, Vondracek J. Strategy aimed at reduction of sputum eosinophils decreases exacerbation rate in patients with asthma. J Int Med Res. 2006;34:129–139. doi: 10.1177/147323000603400202. [DOI] [PubMed] [Google Scholar]
- 38.Simpson JL, Scott R, Boyle MJ, Gibson PG. Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology. 2006;11:54–61. doi: 10.1111/j.1440-1843.2006.00784.x. [DOI] [PubMed] [Google Scholar]
- 39.Furuta GT, Kagalwalla AF, Lee JJ, Alumkal P, Maybruck BT, Fillon S, et al. The oesophageal string test: a novel, minimally invasive method measures mucosal inflammation in eosinophilic oesophagitis. Gut. 2013;62:1395–1405. doi: 10.1136/gutjnl-2012-303171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gon Y, Ito R, Hattori T, Hiranuma H, Kumasawa F, Kozu Y, et al. Serum eosinophil-derived neurotoxin: correlation with persistent airflow limitation in adults with house-dust mite allergic asthma. Allergy Asthma Proc. 2015;36:e113–20. doi: 10.2500/aap.2015.36.3884. [DOI] [PubMed] [Google Scholar]
- 41.Choi Y, Le Pham D, Lee DH, Lee SH, Kim SH, Park HS. Biological function of eosinophil extracellular traps in patients with severe eosinophilic asthma. Exp Mol Med. 2018;50:104. doi: 10.1038/s12276-018-0136-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim KW, Lee KE, Kim ES, Song TW, Sohn MH, Kim KE. Serum eosinophil-derived neurotoxin (EDN) in diagnosis and evaluation of severity and bronchial hyperresponsiveness in childhood asthma. Lung. 2007;185:97–103. doi: 10.1007/s00408-006-0054-8. [DOI] [PubMed] [Google Scholar]
- 43.Wojnarowski C, Roithner B, Koller DY, Halmerbauer G, Gartner C, Tauber E, et al. Lack of relationship between eosinophil cationic protein and eosinophil protein X in nasal lavage and urine and the severity of childhood asthma in a 6-month follow-up study. Clin Exp Allergy. 1999;29:926–932. doi: 10.1046/j.1365-2222.1999.00586.x. [DOI] [PubMed] [Google Scholar]
- 44.Ordoñez CL, Shaughnessy TE, Matthay MA, Fahy JV. Increased neutrophil numbers and IL-8 levels in airway secretions in acute severe asthma: clinical and biologic significance. Am J Respir Crit Care Med. 2000;161:1185–1190. doi: 10.1164/ajrccm.161.4.9812061. [DOI] [PubMed] [Google Scholar]
- 45.Nanzer AM, Chambers ES, Ryanna K, Richards DF, Black C, Timms PM, et al. Enhanced production of IL-17A in patients with severe asthma is inhibited by 1α,25-dihydroxyvitamin D3 in a glucocorticoid-independent fashion. J Allergy Clin Immunol. 2013;132:297–304.e3. doi: 10.1016/j.jaci.2013.03.037. [DOI] [PubMed] [Google Scholar]
- 46.Irvin C, Zafar I, Good J, Rollins D, Christianson C, Gorska MM, et al. Increased frequency of dual-positive TH2/TH17 cells in bronchoalveolar lavage fluid characterizes a population of patients with severe asthma. J Allergy Clin Immunol. 2014;134:1175–1186.e7. doi: 10.1016/j.jaci.2014.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bullens DM, Truyen E, Coteur L, Dilissen E, Hellings PW, Dupont LJ, et al. IL-17 mRNA in sputum of asthmatic patients: linking T cell driven inflammation and granulocytic influx? Respir Res. 2006;7:135. doi: 10.1186/1465-9921-7-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choy DF, Hart KM, Borthwick LA, Shikotra A, Nagarkar DR, Siddiqui S, et al. TH2 and TH17 inflammatory pathways are reciprocally regulated in asthma. Sci Transl Med. 2015;7:301ra129. doi: 10.1126/scitranslmed.aab3142. [DOI] [PubMed] [Google Scholar]
- 49.Pham DL, Ban GY, Kim SH, Shin YS, Ye YM, Chwae YJ, et al. Neutrophil autophagy and extracellular DNA traps contribute to airway inflammation in severe asthma. Clin Exp Allergy. 2017;47:57–70. doi: 10.1111/cea.12859. [DOI] [PubMed] [Google Scholar]