Abstract
Background
Papillary muscle (PM) rupture is a devastating mechanical complication of myocardial infarction that leads to cardiogenic shock and death. In this case, we report a patient with acute mitral regurgitation due to PM rupture that was treated successfully with MitraClip.
Case summary
An 85-year-old female patient with anterior ST-elevation myocardial infarction complicated with PM rupture and acute severe mitral regurgitation was admitted to our hospital. The patient’s surgical risk was considered to be prohibitively high, and was therefore, referred for transcatheter edge-to-edge repair with MitraClip. The procedure was successful, and the patient was discharged home in a stable condition.
Discussion
Acute mitral regurgitation due to PM rupture is a mechanical complication of myocardial infarction that should be treated early because of high mortality rates. This case highlights the role of MitraClip in acute mitral regurgitation and acute heart failure as an alternative to surgery method in high-risk patients.
Keywords: MitraClip, Edge-to-edge repair, Acute mitral regurgitation, Acute heart failure, Papillary muscle rupture, Case report
Learning points
The importance of early revascularization in acute myocardial infarction in order to avoid the development either of heart failure or of any mechanical complication.
The role of MitraClip in treating patients with acute mitral regurgitation due to papillary muscle rupture.
Introduction
Papillary muscle (PM) rupture is a lethal mechanical complication of myocardial infarction that if left untreated can lead to cardiogenic shock and death. Partial rupture of a PM produces acute mitral regurgitation requiring immediate management. If not recognized and treated successfully, it is associated with extremely high mortality rates with more than 90% of the patients dying within the first week.1,2 Fortunately, due to the emphasis on early revascularization with percutaneous coronary interventions, these complications have become rare, representing only 2.3% of patients with acute myocardial infarction.3
The treatment of choice for this complication is surgical repair4 or replacement of the valve. However, many patients are considered to be at high surgical risk and thus not eligible for surgical management; in these acutely ill patients with intractable heart failure, transcatheter edge-to-edge repair may be a solution as a bail-out therapy. In this case, we report on a patient with acute mitral regurgitation due to PM rupture at prohibitive surgical risk and that was managed successfully with edge-to-edge repair with the MitraClip system (Abbott Vascular, Santa Clara, CA, USA).
Timeline
| 24 June 2016 | Admission to a hospital with signs of recent myocardial infarction and percutaneous coronary intervention of a totally occluded intermediate artery |
| 27 June 2016 | Three days later, the patient developed acute pulmonary oedema and cardiogenic shock requiring treatment with inotropes and intra-aortic balloon pump counterpulsation |
| 1 July 2016 | Evaluation with transoesophageal echo recognized papillary muscle rupture and prolapse of the lateral part of the mitral valve producing severe mitral regurgitation |
| 2 July 2016 | Heart team assessment for mitral valve repair or replacement. The patient was considered to be inoperable and was turned down from the cardiac surgeons |
| 3 July 2016 | Admission to our hospital for transcatheter mitral valve repair |
| 4 July 2016 | MitraClip implantation |
| 13 July 2016 | Discharged home |
| Twenty months of follow-up, slightly symptomatic, and New York Heart Association II clinical status | |
| 15 February 2018 |
Case presentation
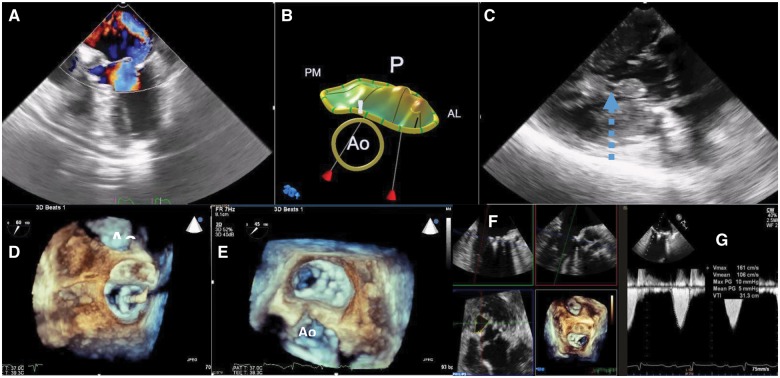
An 85-year-old female patient with prior history of hypertension, was urgently admitted to an outside institution with symptoms of progressive dyspnoea and malaise of ∼1 week duration. The patient later revealed all symptoms being preceded by an episode of persistent substernal chest discomfort that she managed at home without contacting her primary physician. In the emergency department, she was found with electrocardiographic evidence of a recent acute myocardial infarction (Q in precordial leads V1–V4 with ST elevations and T-wave inversions). She was diagnosed with an anterior ST-elevation myocardial infarction, pretreated with aspirin 325 mg, and clopidogrel 600 mg and urgently underwent coronary intervention with a drug-eluting stent to an occluded intermediate artery. The rest of the coronary arteries were without stenoses. Echocardiography 24-h later showed akinetic anterior and lateral wall with an estimated ejection fraction of 40%. After initial clinical improvement, the patient abruptly deteriorated on the third day with onset of acute pulmonary oedema and cardiogenic shock. At this time, the electrocardiogram did not show any dynamic changes of the ST-T segments or any arrhythmias. Repeat coronary angiography was without any further stenosis and re-evaluation with echocardiography revealed new severe mitral regurgitation and no other abnormalities that could lead to shock, such as pericardial effusion—tamponade or ventricular septal defect (VSD). Clinical examination at the time revealed an elderly female in moderate distress, requiring supplemental oxygen (60% FiO2) for maintenance of a saturation of 92–93%, with orthopnoea, jugular venous distension, and bilateral inspiratory crackles on lung auscultation. There was a two out of six systolic apical murmur, without evident gallop rhythm and mild peripheral oedema. The patient was transferred to our institution for further management and possible surgery. Upon transfer, she was in New York Heart Association (NYHA) Class IV with persistent pulmonary oedema despite high doses of intravenous furosemide (180 mg/24 h), on high dose supplemental oxygen (60% venturi mask), and on dobutamine infusion at 3 μg/kg/min. A transoesophageal echo exam (TOE) revealed partial rupture of the anterolateral PM with flail anterior (A1 and A2 scallops) and posterior leaflet (P1 scallop) (Figure 1A–C, Supplementary material online, Videos S1 and S2). This PM rupture and flail mitral valve produced severe acute mitral regurgitation, pulmonary oedema, and cardiogenic shock. The patient was evaluated by the heart team and was considered at prohibitive surgical risk [log EuroSCORE 43% (85-years-old female, critical preoperative state/cardiogenic shock, EF 30–50%, recent myocardial infarction) and STS score 13%]. Indeed, she was in intractable heart failure, despite maximal intravenous diuretics, with dyspnoea at rest, radiographic appearance of bilateral pulmonary oedema, and in need of intra-aortic balloon counterpulsation for stabilization. She was thus referred for emergency transcatheter mitral valve edge-to-edge repair with MitraClip (Abbott Vascular, Santa Clara, CA, USA), (Figure 1D, Supplementary material online, Video S3). Two clips were implanted at the central and lateral part of the valve. The first clip was implanted at the A2–P2 scallop towards the lateral aspect of the valve. Due to the significant remaining regurgitation coming from the flail anterolateral commissure (Supplementary material online, Video S4), a second clip was implanted lateral to the first within the commissure. The final result after implantation of these two clips was with an effective reduction of mitral regurgitation from torrential to mild-moderate, while creating a single orifice valve (‘zipping’ of the lateral commissure) with an estimated (with use of three-dimensional echocardiographic multiplanar reconstruction) residual valve area of 2.1 cm2 and a mean transmitral gradient of 6 mmHg (Figure 1E–G, Supplementary material online, Video S5). Subsequent to the MitraClip procedure, the patient was weaned off both intra-aortic balloon counterpulsation and inotropic support (dobutamine and dopamine infusions). The patient was also switched to oral diuretics and had reduced supplemental oxygen demands. The post-procedural course was uneventful. She was discharged home a week later on standard heart failure therapy including metoprolol, ramipril, furosemide, spironolactone, and ivabradine. At the 20-month follow-up, she remains in stable clinical condition in NYHA class II, and no further interventions were required on the mitral valve. Echocardiography revealed moderate mitral regurgitation and a mean transmitral gradient of 6 mmHg.
Figure 1.
(A) Mid-oesophageal view at 0® with colour flow depicting severe mitral regurgitation due to flail anterior leaflet, eccentric wall hugging jet with large flow convergence zone. (B) Schematic representation of the mitral valve highlighting prolapse/flail of the anterior (A1 and A2 scallops) and posterior (P1 scallop) leaflets. (C) Transgastric long-axis view of the left ventricle. Arrow points to the partial rupture of the anterolateral papillary muscle head. (D) Positioning of the MitraClip over the mid segment of the mitral valve, evaluation for perpendicularity. (E) Final result with ‘zipping’ of the lateral commissure to the mid segment of the valve. (E) Multiplanar reconstruction and evaluation of the residual orifice area, measured at 2.1 cm2. (G) Continuous wave Doppler, mean gradient 5 mmHg. AL, anterolateral; Ao, aortic valve; PM, posteromedial.
Discussion
Papillary muscle rupture is a rare but lethal mechanical complication of myocardial infarction. The reported incidence of this condition is 1–3% and if left untreated the prognosis is poor with 50% mortality within the first 24 h and 80% within the first week.4,5 The posteromedial PM is affected more often because of its blood supply from the right coronary artery. On the contrary, the anterolateral PM receives blood from both the diagonal branch of the left anterior descending artery and the left circumflex artery. This double blood supply explains why the anterolateral PM is affected only in large anterior infarcts and the relative incidence of rupture compared to the posteromedial PM rupture is just 1/4–1/9.6 Early revascularization is well known to reduce the incidence of this complication, however, as in the case presented, patients may still present late, and despite a technically successful revascularization will still be at risk for PM rupture. In our experience, PM rupture and more so of the anterior PM has been an extremely rare event.
Imaging with transthoracic and transoesophageal echo (TOE) is essential in diagnosis of PM rupture and evaluation of the severity of the mitral regurgitation. Three-dimensional TOE further enables identification of the prolapsing segments of the mitral valve and enhances our understanding of underlying pathology. This is critical in deciding anatomic eligibility for surgical or transcatheter repair.
The treatment of choice in patients with myocardial infarction complicated with PM rupture is surgical replacement or repair when possible.4 If the rupture is complete, repair might be difficult because of the friable infarcted tissue. An acute mitral regurgitation due to partial PM rupture is often amenable to a successful repair. However, there are many patients that are considered to be inoperable, or at high risk and cannot be managed surgically. These patients could have the option of transcatheter management,7–9 and the only clinically available method is the edge-to-edge repair with the MitraClip device (Abbott Vascular, Santa Clara, CA, USA). Based on the EVEREST I and II trials,10 the MitraClip device (Abbott Vascular, Santa Clara, CA, USA) can be applied to patients with degenerative aetiology meeting specific anatomic criteria (‘EVEREST’ criteria); the procedure is included in the recent guidelines ACC/AHA and ESC for high risk or inoperable patients.11,12 In clinical practice and in difficult clinical situations, anatomic eligibility for MitraClip (Abbott Vascular, Santa Clara, CA, USA) depends on three factors: ability to approximate the leaflets, size of the mitral valve orifice (to avoid iatrogenic stenosis), and adequate transoesophageal imaging to guide the procedure.
The case reported highlights several important and novel aspects of MitraClip (Abbott Vascular, Santa Clara, CA, USA) for mechanical PM rupture. First the patient was in extremis, with intractable acute heart failure despite maximal support and intra-aortic balloon counterpulsation. Treatment options were limited to extremely high-risk surgery or palliative therapy; transcatheter repair emerged as a possibility given the safety profile and the high potential benefit to risk ratio. The anatomy was challenging given the large flail width and flail gap with involvement of the lateral commissure. The procedure was successful in decreasing the degree of regurgitation, while creating a single orifice mitral valve with an acceptable area of 2.1 cm2 and a mean gradient of about 6 mmHg. The patient was discharged home a few days later and at a follow-up of 22 months the patient required no further interventions to the mitral valve and no further hospitalizations for heart failure.
Conclusion
Papillary muscle rupture is a lethal complication of a myocardial infarction that has become rare in the era of early revascularization. The method of choice for treating these patients who present with acute and often intractable heart failure remains the surgical approach but new transcatheter techniques like the edge-to-edge repair can be a safe alternative option for patients at high surgical risk. Consideration should be given for a formal endorsement of edge-to-edge repair as an option for severe mitral regurgitation following PM rupture.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: K.S. and M.C. have proctoring activities for Abbot Vascular. All other authors have no conflict of interest.
Supplementary Material
References
- 1. Jain SKA, Larsen TR, Darda S, Saba S, David S.. A forgotten devil; rupture of mitral valve papillary muscle. Am J Case Rep 2013;14:38–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nishimura RA, Gersh BJ, Schaff HV.. The case for an aggressive surgical approach to papillary muscle rupture following myocardial infarction: “From paradise lost to paradise regained”. Heart 2000;83:611–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi-Min Yuan HJ, Lavee J.. The mechanical complications of acute myocardial infarction: echocardiographic visualizations. Turkish J Thoracic Cardiovasc Surg 2011;19:36–42. [Google Scholar]
- 4. Bouma W, Wijdh-den Hamer IJ, Klinkenberg TJ, Kuijpers M, Bijleveld A, van der Horst ICC, Erasmus ME, Gorman JH, Gorman RC, Mariani MA.. Mitral valve repair for post-myocardial infarction papillary muscle rupture. Eur J Cardiothorac Surg 2013;44:1063–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nishimura RA, Schaff HV, Shub C, Gersh BJ, Edwards WD, Tajik AJ.. Papillary muscle rupture complicating acute myocardial infarction: analysis of 17 patients. Am J Cardiol 1983;51:373–377. [DOI] [PubMed] [Google Scholar]
- 6. Doi T, Nagura S, Fukahara K, Yoshimura N.. Surgical treatment of complete anterolateral papillary muscle rupture following acute myocardial infarction. Ann Thorac Cardiovasc Surg 2014;20:926–928. [DOI] [PubMed] [Google Scholar]
- 7. Bahlmann E, Frerker C, Kreidel F, Thielsen T, Ghanem A, van der Schalk H, Grahn H, Kuck K-H.. MitraClip implantation after acute ischemic papillary muscle rupture in a patient with prolonged cardiogenic shock. Ann Thorac Surg 2015;99:e41–e42. [DOI] [PubMed] [Google Scholar]
- 8. Bilge M, Alemdar R, Yasar AS.. Successful percutaneous mitral valve repair with the MitraClip system of acute mitral regurgitation due to papillary muscle rupture as complication of acute myocardial infarction. Catheter Cardiovasc Interv 2014;83:E137–E140. [DOI] [PubMed] [Google Scholar]
- 9. Wolff R, Cohen G, Peterson C, Wong S, Hockman E, Lo J, Strauss BH, Cohen EA.. MitraClip for papillary muscle rupture in patient with cardiogenic shock. Can J Cardiol 2014;30:1461.e13–1461.e14. [DOI] [PubMed] [Google Scholar]
- 10. Feldman T, Foster E, Glower DD, Glower DG, Kar S, Rinaldi MJ, Fail PS, Smalling RW, Siegel R, Rose GA, Engeron E, Loghin C, Trento A, Skipper ER, Fudge T, Letsou GV, Massaro JM, Mauri L.. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395–1406. [DOI] [PubMed] [Google Scholar]
- 11. Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, Iung B, Lancellotti P, Lansac E, Rodriguez Muñoz D, Rosenhek R, Sjögren J, Tornos Mas P, Vahanian A, Walther T, Wendler O, Windecker S, Zamorano JL; ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017;38:2739–2791. [DOI] [PubMed] [Google Scholar]
- 12. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, Jneid H, Mack MJ, McLeod CJ, O’Gara PT, Rigolin VH, Sundt TM, Thompson A. 2017 AHA/ACC focused update of the 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol 2017;70:252–289. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.