Abstract
Background
Uhl’s anomaly is a rare congenital heart disease characterized by ‘Paper-like thinning of the right ventricular (RV) wall’. Since most patients with Uhl’s anomaly die in infancy or childhood, the adult cases of this disorder have been limitedly reported and there were no past report describing this anomaly with ventricular tachycardia (VT), in which catheter ablation was successfully performed.
Case summary
We report the case of a 43-year-old man with a suggested Uhl’s anomaly and VT. He underwent a catheter ablation of the recurrent VT. An electrophysiological study showed the VT (cycle length = 460 ms) with a right bundle branch block pattern and inferior axis represented QRS alternans. Concealed entrainment by pacing from the anterior right ventricle (RV) suggested the mechanism of this VT was re-entry and the QRS alternans was simultaneously reproduced during the pacing. Furthermore, the intracardiac electrograms exhibiting local conduction blocks were documented on the RV free wall near the apex. The electrograms seen in a 2:1 ratio were coincident with slurs in the initial QRS on the 12-lead electrocardiogram. Since the anterior RV wall was considered to be a part of the VT circuit, a linear ablation in that area was performed resulting in VT termination.
Discussion
The local conduction blocks near the RV apex were related to the mechanism of the QRS alternans during the VT in this case. That might be based on the variations in the myocardium lying in the RV, which is the specific feature of Uhl’s anomaly.
Keywords: Uhl’s anomaly, Right ventricle, Ventricular tachycardia, QRS alternans, Localized intraventricular block, Catheter ablation, Case report
Learning points
Uhl’s anomaly is a rare congenital heart disease which is characterized as a partial or complete absence of the right ventricular (RV) myocardium, so called ‘Paper-like thinning of the RV wall’.
Generally, the possible mechanisms of the QRS alternans during ventricular tachycardia were due to triggered activity, varying degrees of aberrancies or refractoriness of the different regions of the ventricles, or multiple exit sites from the site of origin.
Introduction
Uhl’s anomaly of the right ventricle (RV) is a rare congenital heart disease with no known underlying mechanism,1 and was originally described by Henry Uhl as an isolated disorder of the right ventricular (RV) myocardium in 1952.2 This anomaly is characterized by ‘Paper-like thinning of the RV wall’, and partial or complete absence of myocardium, which is replaced by non-functional fibroelastic tissue. As a result, it becomes an extremely dilated thin-walled RV with absence of trabeculation.3 Since most patients with Uhl’s anomaly die in infancy or childhood,4 the adult cases of this disorder have been limitedly reported. Here, we report a very rare case of adult Uhl’s anomaly complicated with ventricular tachycardia (VT) that had arrhythmic features of interest and was successfully treated with catheter ablation.
Timeline
| Time | Events |
|---|---|
| About 36 years ago | Patient was diagnosed with an Uhl’s anomaly in another hospital at the age of 7 years |
| About 12 years ago | Ventricular tachycardia (VT) occurred, and the patient was referred to our hospital for management of the VT. Implantation of an implantable cardioverter-defibrillator (ICD) was performed after unsuccessful catheter ablation of the VT |
| For over a decade | Frequency of appropriate ICD therapies for VT had gradually increased |
| 20 days before present ablation admission | Clinical VT was detected with ambulatory electrocardiogram monitor during another hospitalization for VT management |
| Admission for re-ablation for the VT | |
| Day 5: electrophysiological study and ablation | Catheter ablation was performed resulting in termination and non-inducibility of the VT |
| Day 10 | Discharged home |
| 2 years after the ablation | No evidence of further episodes of VT |
Case presentation
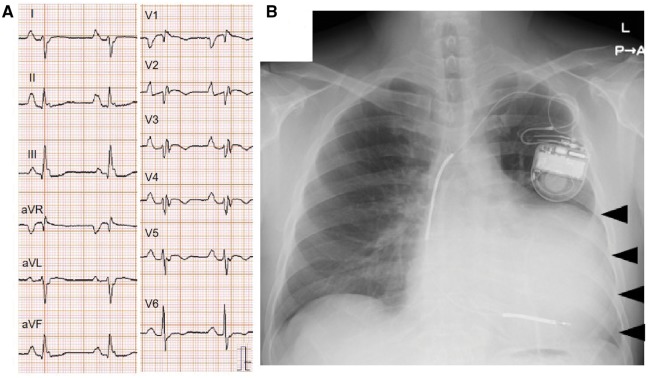
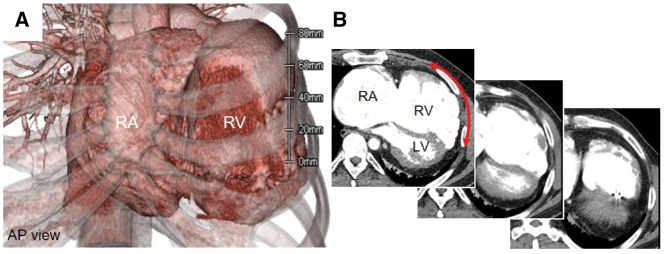
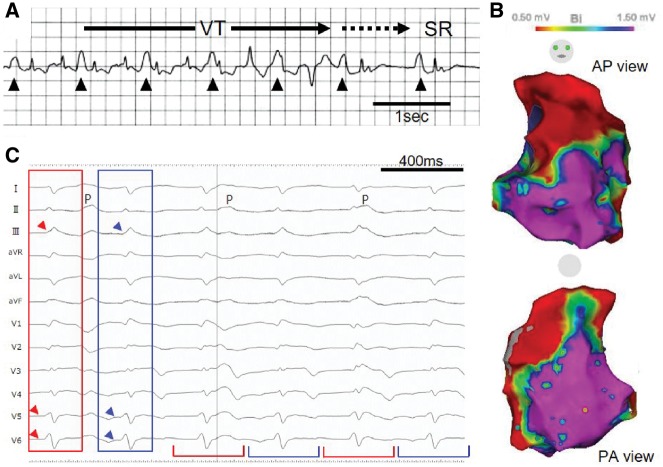
Our patient was a 43-year-old man. At the age of 7 years, he was first documented with cardiomegaly by a chest X-ray and was diagnosed with a suggested Uhl’s anomaly by echocardiography and scintigraphy in another university hospital. He had no family history of sudden cardiac death. His first VT episode was seen when he was 31 years old, and he was referred to our hospital for intensive treatment of the VT including catheter ablation. Soon after an unsuccessful catheter ablation of the VT, an implantable cardioverter-defibrillator (ICD) was implanted along with medical treatment including amiodarone. Since the frequency of appropriate ICD therapies for ventricular tachyarrhythmias had gradually increased in the previous decade, he was referred to undergo a repeat catheter ablation. Although he was haemodynamically stable even during the arrhythmias and felt no palpitation, on admission, his blood pressure was 140/84 mmHg, pulse rate was 68/min, and respiratory rate was 18/min with an O2 saturation of 95% on room air. He showed predominantly right sided heart failure with jugular venous distention and pitting oedema in the lower extremities. Blood test showed no electrolyte abnormalities and a high serum B-type natriuretic peptide level of 336 (<18.4) pg/mL. His baseline electrocardiogram (ECG) exhibited normal sinus rhythm with large P waves, an rsr’ QRS complex in leads V1–4, and right-axis deviation (Figure 1A). A chest X-ray revealed enlargement of the cardiac silhouette with a contour of the large RV without severe pulmonary oedema (Figure 1B). Electrocardiogram-gated multi-detector computed tomography (MDCT) depicted the specific features of Uhl’s anomaly—a remarkable RV and right atrial dilatation, and the localized coexistence of a severely thin RV wall and partial defects of the RV muscular wall (Figure 2). These images indicated that his diagnosis was Uhl’s anomaly rather than arrhythmogenic right ventricular cardiomyopathy in which residual myocardium was replaced by fat and fibrosis.5,6 Transthoracic echocardiography revealed similar morphological findings; severe RV dilatation (RV dimension was 72 mm) resulting in D-shaped left ventricle. Left ventricular ejection fraction was 35%. An ambulatory ECG monitor detected a mildly wide QRS tachycardia with a rate of 140–150 b.p.m. and atrioventricular dissociation, which was considered to be the clinical VT (Figure 3A).
Figure 1.
(A) Twelve-lead electrocardiogram on admission. Large P wave, an rsr’ QRS complex in leads V1–4 with right axis deviation are seen. (B) Chest X-ray. Cardiomegaly with a protrusion of an enlarged right ventricular silhouette (arrowhead) are found.
Figure 2.
Electrocardiogram-gated multi-detector computed tomography. (A) Three-dimensional imaging. Severely dilated right atrium and right ventricle are seen. (B) Of note, the localized coexistence of the residual muscular wall, severely thin right ventricle wall, and partial defects of the right ventricle muscular wall were also seen (red arrow). AP, anterior-posterior; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
Figure 3.
(A) Ambulatory electrocardiogram monitor at the time of the spontaneous termination of the ventricular tachycardia. A relatively mildly wide QRS tachycardia at 140–150 b.p.m. is followed by the spontaneous restoration to sinus rhythm. This tachycardia was diagnosed as ventricular tachycardia because of the dissociation between the large P waves (arrowhead) and R waves. (B) Electroanatomic voltage map of the right ventricle during sinus rhythm. The voltage amplitude greater than or equal to 1.50 mV is seen in a part of the anterior free wall and interventricular septum. (C) Twelve-lead electrocardiogram of the induced ventricular tachycardia during the electrophysiological study. Alternate changes in the QRS complex morphology, so called QRS alternans, is seen (red and blue brackets), which is especially obvious in leads V5 and V6 as slurs just before the QRS complex (red and blue arrowheads). P means P wave during the ventricular tachycardia. SR, sinus rhythm; VT, ventricular tachycardia.
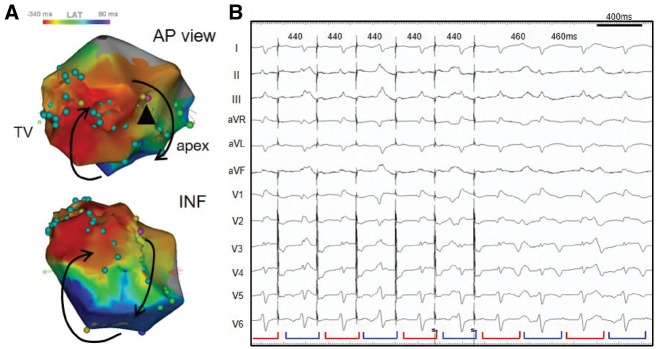
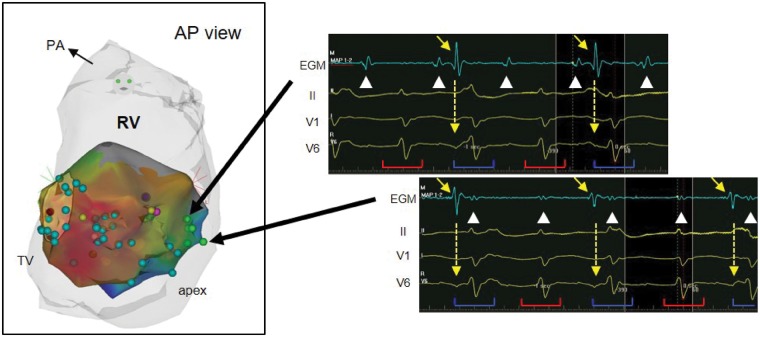
The patient underwent an electrophysiological study (EPS) and catheter ablation under guidance with the Carto 3 electroanatomical mapping system (Biosense Webster, South Diamond Bar, CA, USA). Voltage mapping of the RV endocardium during sinus rhythm showed a broad electrical scar area, whereas a preserved voltage amplitude was seen on the anterior wall and interventricular septum (Figure 3B). A VT (cycle length = 460 ms) with a right bundle branch block pattern and inferior axis was induced with programmed RV extrastimulation (Figure 3C). During the VT, QRS alternans was seen, which was especially obvious in leads V5 and V6. Since his haemodynamic state was stable during the VT, we could perform activation mapping (Figure 4A). Concealed entrainment by pacing from the low-voltage zone of the anterior RV with a post-pacing interval of 475 ms suggested that the mechanism of this VT was re-entry. Interestingly, the QRS alternans was simultaneously reproduced during the entrainment pacing (Figure 4B). Furthermore, the intracardiac electrograms exhibiting 2:1 conduction were documented on the RV free wall near the apex (Figure 5). There were two components, one was coincident with the VT cycle length, but the other was seen in a 2:1 ratio. At the timing of the appearance of a latter electrogram, slurs in the initial QRS on the 12-lead ECG occurred, which was related to the mechanism of the QRS alternans during the VT.
Figure 4.
(A) Electroanatomic activation map during the ventricular tachycardia. Counterclockwise activation on the inferolateral aspect of the right ventricle can be seen. (B) QRS alternans on the 12-lead electrocardiogram during entrainment pacing. Concealed entrainment was obtained by pacing from a low-voltage area in the anterior right ventricle (pink tag: arrowhead). The same QRS alternans as the ventricular tachycardia was reproduced by the pacing (red and blue brackets). AP, anterior-posterior; INF, inferior; LAT, local activation time; TV, tricuspid valve.
Figure 5.
Local ventricular electrograms on the right ventricle free wall near the apex during the ventricular tachycardia (green tags). The electrograms reveal that two components, one coincident with the ventricular tachycardia cycle length (white arrowhead), but the other seen in a 2:1 ratio (yellow arrow) are seen. At the same timing as the appearance of the larger electrogram, there were slurs of the QRS on the 12-lead electrocardiogram (dotted arrow). AP, anterior-posterior; PA, pulmonary artery; RV, right ventricle; TV, tricuspid valve.
Although a critical narrow isthmus of the VT re-entrant circuit was not definitely detected by the EPS, the anterior RV wall was a part of the VT circuit. Thus, a horizontal linear ablation with a target of the diastolic potentials in that area was performed resulting in VT termination. No VT was induced after catheter ablation. He has been free from appropriate ICD therapy in more than 2 years of follow-up.
Discussion
The main prognostic factors of Uhl’s anomaly are ventricular arrhythmias and right-sided heart failure.4,7–9 To date, only a few cases in living adult patients with Uhl’s anomaly have been reported.7–10 This case, to the best of our knowledge, is the first case of a suggested Uhl’s anomaly complicated with VT, in which catheter ablation was successfully performed. Interestingly, QRS alternans during the VT was observed in our case. Furthermore, this QRS alternans was reproduced by entrainment pacing from the circuit of the VT. Generally, possible electrical mechanisms of QRS alternans are due to triggered activity, varying degrees of aberrancy, refractoriness of different regions of the ventricles, or multiple exit sites from the site of origin.11,12
In our case, two types of local electrograms on the RV free wall near the apex were documented. Those components could be considered as near-field and far-field electrograms, which suggested the existence of local 2-to-1 conduction block between the two regions. The distal region was considered to be the bystander area from the fact that the post pacing interval of 70 ms was longer than the VT cycle length. As the QRS alternans and 2 to 1 conduction on the RV free wall near the apex occurred simultaneously, the electrical heterogeneity of the excitation in this bystander area generated the QRS alternans during the VT.
One possible mechanism of this heterogeneity is a reduction of intercellular electrical coupling due to an impaired ventricular myocardium.13 Another possible explanation is a delayed activation by current-to-load mismatch14 based on the structural discontinuities of the RV myocardium, which can occur in the case of Uhl’s anomaly because of its specific myocardial features. Vigmond et al.15 reported that local unipolar electrograms with a monophasic-like morphology could be recorded at the site of current-to-load mismatch in human epicardial RV outflow tract. Although we did not observe this type of electrogram in the present case, MDCT showed discontinuities and heterogeneities of the RV wall (Figure 2B), which might support the relationship between current-to-load mismatch and the electrical mechanisms the QRS alternans in this case.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. van der Palen RL, van der Wal AC, Robles de Medina PG, Blom NA, Clur SA.. Uhl's anomaly: clinical spectrum and pathophysiology. Int J Cardiol 2016;209:118–121. [DOI] [PubMed] [Google Scholar]
- 2. Uhl HS. A previously undescribed congenital malformation of the heart: almost total absence of the myocardium of the right ventricle. Bull Johns Hopkins Hosp 1952;91:197–209. [PubMed] [Google Scholar]
- 3. James TN, Nichols MM, Sapire DW, DiPatre PL, Lopez SM.. Complete heart block and fatal right ventricular failure in an infant. Circulation 1996;93:1588–1600. [DOI] [PubMed] [Google Scholar]
- 4. Song BG. A rare case of partial absence of the right ventricular musculature in asymptomatic adult man: partial Uhl's anomaly. Heart Lung 2013;42:215–217. [DOI] [PubMed] [Google Scholar]
- 5. Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MGPJ, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DMY, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, Zareba W.. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation 2010;121:1533–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kimura Y, Noda T, Otsuka Y, Wada M, Nakajima I, Ishibashi K, Miyamoto K, Okamura H, Aiba T, Kamakura S, Noguchi T, Anzai T, Satomi K, Ogawa H, Yasuda S, Kusano KF.. Potentially lethal ventricular arrhythmias and heart failure in arrhythmogenic right ventricular cardiomyopathy: what are the differences between men and women? JACC Clin Electrophysiol 2016;2:546–555. [DOI] [PubMed] [Google Scholar]
- 7. Greer ML, MacDonald C, Adatia I.. MRI of Uhl's anomaly. Circulation 2000;101:E230–E232. [DOI] [PubMed] [Google Scholar]
- 8. Otmani A, Leborgne L, Renard C, Bakkour H, Quenum S, Tribouilloy C, Rey JL. Images in cardiovascular medicine. Electrocardiogram, echocardiography, and magnetic resonance imaging characteristics in Uhl's disease. Circulation 2007;115:e11–e12. [DOI] [PubMed] [Google Scholar]
- 9. Cheng JF, Mohammed TL, Griffith BP, White CS.. CT of Uhl's anomaly in an adult. Int J Cardiovasc Imaging 2005;21:663–666. [DOI] [PubMed] [Google Scholar]
- 10. Hébert JL, Duthoit G, Hidden-Lucet F, Cortès-Morichetti M, Bouchachi AA, Azarine A, Fressart V, Simon F, Le Guludec D, Lacotte J, Frank R, Lecarpentier Y. Images in cardiovascular medicine. Fortuitous discovery of partial Uhl anomaly in a male adult. Circulation 2010;121:e426–e429. [DOI] [PubMed] [Google Scholar]
- 11. Yamada T, McElderry HT, Doppalapudi H, Kay GN.. QRS alternans during idiopathic ventricular tachycardia originating from the right coronary cusp of the aorta. Europace 2010;12:133–135. [DOI] [PubMed] [Google Scholar]
- 12. Kalbfleisch S, Hart D, Weiss R.. Two ventricular tachycardias with cycle length and QRS alternans: insights into the mechanism from mapping and ablation of the tachycardias. Pacing Clin Electrophysiol 2009;32:e31–e35. [DOI] [PubMed] [Google Scholar]
- 13. Cooklin M, Wallis WR, Sheridan DJ, Fry CH.. Changes in cell-to-cell electrical coupling associated with left ventricular hypertrophy. Circ Res 1997;80:765–771. [DOI] [PubMed] [Google Scholar]
- 14. Hoogendijk MG, Potse M, Linnenbank AC, Verkerk AO, den Ruijter HM, van Amersfoorth SCM, Klaver EC, Beekman L, Bezzina CR, Postema PG, Tan HL, Reimer AG, van der Wal AC, ten Harkel ADJ, Dalinghaus M, Vinet A, Wilde AAM, de Bakker JMT, Coronel R.. Mechanism of right precordial ST-segment elevation in structural heart disease: excitation failure by current-to-load mismatch. Heart Rhythm 2010;7:238–248. [DOI] [PubMed] [Google Scholar]
- 15. Vigmond EJ, Efimov IR, Rentschler SL, Coronel R, Boukens BJ.. Fractionated electrograms with ST-segment elevation recorded from the human right ventricular outflow tract. HeartRhythm Case Rep 2017;3:546–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.