Abstract
Background
The alarmingly rising prevalence of allergic diseases has led to substantial healthcare and economic burdens worldwide. The integrated use of traditional Chinese medicines (TCM) and Western medicines has been common in treating subjects with allergic diseases in clinical practice in Taiwan. However, limited studies have been conducted to evaluate long-term trends and prescription patterns of TCM use among subjects with allergic diseases. Thus, we conducted a nationwide population-based study to characterize TCM use among subjects with allergic diseases.
Methods
A total of 241,858 subjects with diagnosed atopic dermatitis, asthma or allergic rhinitis in the period of 2003–2012 were identified from the National Health Insurance Research Database (NHIRD) in Taiwan and included in this study. We assessed trends and prescribed patterns related to TCM (both single herbs and herbal formulas) among the study subjects over the 10-year study period.
Results
The overall proportions of TCM use were 30.5%, 29.0% and 45.7% in subjects with atopic dermatitis, asthma and allergic rhinitis, respectively. We found increasing trends of TCM use among subjects having atopic dermatitis and asthma, with annual increase of 0.91% and 0.38%, respectively, over the 10-year study period while the proportion remained steadily high (from 46.6% in 2003 to 46.3% in 2012) among subjects having allergic rhinitis. Moreover, the number of hospitalization due to allergic diseases in TCM users was significantly smaller than that in non TCM users for all three allergic diseases.
Conclusion
A notable proportion (30%–50%) of subjects with allergic diseases in Taiwan has used TCM, with the highest proportion of TCM use found in subjects with allergic rhinitis, whereas increasing trends of TCM use are found among subjects with atopic dermatitis and asthma, respectively. Our results suggest that TCM use may help reduce the severe episodes of allergic diseases necessitating hospitalizations.
Keywords: Prescription patterns, Traditional Chinese medicine, Allergic diseases
Introduction
Allergic diseases such as atopic dermatitis, asthma and allergic rhinitis have increased noticeably in recent decades and are emerging as a major clinical and public health issue not only in Taiwan, but also worldwide.1, 2, 3, 4 It has been documented by the World Allergy Organization (WAO) White Book on Allergy 2013 update5 that approximately 30–40% of the worldwide population is affected by one or more allergic diseases, such as atopic dermatitis, asthma, allergic rhinitis and food allergy etc. The increasing prevalence of allergic diseases during the past decades has also led to considerable economic, medical and social burdens.6
It is long known that Western medicines, e.g., antihistamines, corticosteroids, leukotriene modifiers, beta2-agonists, and anticholinergics etc., have been widely administered to treat subjects with allergic diseases.7 However, available Western-medicine treatment for allergic diseases may only offer symptomatic relief, but is lack of curative efficacy. Thus, managing allergic diseases using conventional Western medicines has remained a major challenge.
On the other hand, there is a general impression among some people in Chinese society including Taiwan that traditional Chinese medicine (TCM) is better in curing the root of a disease and has milder adverse effects when compared to Western medicines.8 In addition, the lack of curative efficacy in Western medicines may explain, at least in part, why a considerable proportion of subjects with allergic diseases seek complementary and alternative treatment, specifically, TCM.9 TCM has been used for thousands of years in Asian countries, including China, Japan, Korea and Taiwan. However, trends and prescription patterns of TCM use in subjects with allergic diseases have been largely unexplored.
The National Health Insurance Program (NHIP) in Taiwan has launched since 1995, covering nearly 99.6% of the total population residing in Taiwan.10 Since 1996, TCM use has been reimbursed by the NHIP. In the present study, using data collected by the NHIP, we investigated 10-year trends and prescription patterns of TCM use in subjects with three common allergic diseases, specifically, atopic dermatitis, asthma and allergic rhinitis, from 2003 to 2012 in Taiwan.
Methods
Data source
In this study, we used registry data derived from the Longitudinal Health Insurance Database 2005 (LHID2005) composed of medical claims data, which are part of the National Health Insurance Research Database (NHIRD) in Taiwan. In brief, the NHIP, a government-run, single-payer program, has provided mandatory medical care to residents in Taiwan since 1995. The NHIRD contains reimbursement claims data collected by the NHIP, including demographic characteristics, outpatient and inpatient claims data and prescription records (both Western medicines and TCM). Previous studies have reported that enrollees representing nearly 99% of the total population in Taiwan.10 The LHID2005, a subset derived from the NHIRD, included 1,000,000 individuals (approximately 5% of the total population of Taiwan) and randomly sampled from the 2005 National Health Insurance Registry for Beneficiaries of the original NHIRD. As described in the following link (http://nhird.nhri.org.tw/en/Data_Subsets.html) – “There was no significant difference in the gender distribution (χ2 = 0.008, df = 1, P-value = 0.931) between the patients in the LHID2005 and the original NHIRD”, the information has provided supportive evidence that the LHID2005 was representative for the entire Taiwan population. The Institutional Review Board of the National Health Research Institutes, Taiwan approved this study protocol (the ethics approval reference number: EC1050302-E).
Study population
In the present study, subjects diagnosed with atopic dermatitis, asthma and allergic rhinitis in the period of 2003–2012 were included. In considering substantial degree of variation in seeking treatment among prevalent subjects, we excluded subjects who were diagnosed as atopic dermatitis, asthma and allergic rhinitis before 2003. We defined subjects with allergic disease(s) based on the International Classification of Diseases [ICD]-9-CM codes during the study period of 2003–2012. Diagnoses of three examined allergic diseases in this study were described as follow: i) atopic dermatitis defined as at least one inpatient or two outpatient medical claims records within a year (ICD-9 code = 691.8)11, 12; ii) asthma defined as at least one inpatient or two outpatient medical claims records within a year (ICD-9 code = 493)13; and iii) allergic rhinitis defined as at least one inpatient or two outpatient medical claims records within a year (ICD-9 = 477).12 The date of the second outpatient medical claims record or the date of one inpatient medical claims record were used for defining time to diagnosis of the three examined allergic diseases.
Assessment of traditional Chinese medicine use
Currently, the NHIP has reimbursed two kinds of Chinese herbal remedies: Chinese single herbs and Chinese herbal formulas. Each Chinese herbal formula is combined with two or more fixed proportions of Chinese single herbs, strictly followed the TCM classics. TCM use for the three allergic diseases evaluated in this study was directly recorded in the LHID2005. Thus, we identified Chinese herbal remedies based on prescription records from the LHID2005, then grouped study subjects as TCM users or non TCM users.
Data analysis
We calculated mean and corresponding standard deviation (SD), or counts and corresponding percentages for the baseline demographic and clinical characteristics of study subjects, including: age, sex, enrollee category as a proxy measure to represent the study subjects' socio-economic status, geographical area and healthcare utilization of outpatient and inpatient visits one year after the index date. Student's t-test was used for continuous variables and chi-square test was used for categorical variables, respectively, to compare demographic and clinical characteristics between subjects with and without TCM use. In addition to the corresponding statistical tests, we compared demographic and clinical characteristics between subjects with and without TCM use using standardized mean differences (SMDs), which were computed as the absolute difference in means or proportions divided by a pooled standard deviation in two groups.14, 15 Previous studies have reported that SMDs are not sensitive to sample size and more suitable in determining meaningful differences than traditional significance tests.14 SMDs less than 0.1 are considered as adequate balance for corresponding variables between groups.16 To investigate time trends for TCM use in each examined allergic disease, we first transformed the calendar year by subtracting 2003 from the year and dividing the results by 9. Thus, the transformed values were 0 for 2003 and 1 for 2012. Next, we performed linear regression analyses for evaluating 10-year time trends of TCM use for three examined allergic diseases (atopic dermatitis, asthma and allergic rhinitis) in this study. All of the analyses were performed using SAS version 8.2 (SAS institute, Cary, NC). P values less than 0.05 were declared to be statistically significant.
Results
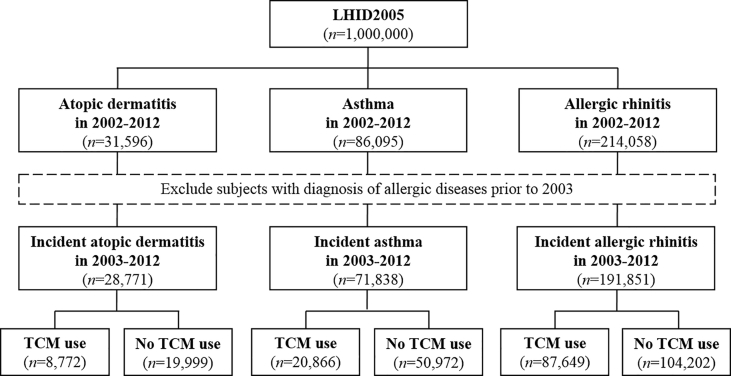
A total of 241,858 subjects diagnosed with one or more allergic diseases including atopic dermatitis, asthma and allergic rhinitis in the period of 2003–2012 were included in this study and examined in the subsequent analyses. Among those, there were 28,771 subjects with atopic dermatitis, 71,838 subjects with asthma, and 191,851 subjects with allergic rhinitis. Fig. 1 shows the detailed flow chart regarding identification for the study subjects. For the percentages of TCM use, we found that 30.5% subjects with atopic dermatitis were TCM users; 29.0% subjects with asthma were TCM users; and 45.7% subjects with allergic rhinitis were TCM users.
Fig. 1.
Flowchart of study subjects identified from the Longitudinal Health Insurance Database 2005 (LHID2005) from 2003 to 2012 in Taiwan.
Table 1 presents the distributions of baseline and clinical characteristics included age, sex, enrollee category, geographical area and healthcare utilization of outpatient and inpatient visits one year after the index date. The distributions of age, sex and enrollee category (except for atopic dermatitis) are different between subjects with and without TCM use in three allergic diseases examined in this study (all SMDs more than or equal to 0.1 for age and sex in three allergic diseases; enrollee category: SMD = 0.08 for atopic dermatitis, SMD = 0.10 for asthma, and SMD = 0.11 for allergic rhinitis). There was no difference in distributions of geographic area in three examined allergic diseases (all SMDs < 0.1). The mean age and corresponding standard deviation at diagnosis of allergic diseases in subjects with TCM use was 32.81 ± 25.48 years, while the group of subjects without TCM use was 32.33 ± 21.37 years. Females were predominant in TCM users for all three allergic diseases. In terms of healthcare utilization one year after the index date, subjects with TCM use had more outpatient visits in three examined allergic diseases (all SMDs > 0.1), and less inpatient visits, compared to the group of subjects without TCM use in asthma and allergic rhinitis, but not atopic dermatitis (number of hospitalization: SMD = 0.06 for atopic dermatitis; SMD = 0.11 for asthma; and SMD = 0.10 for allergic rhinitis) (Table 1).
Table 1.
Demographic characteristics of patients with diagnosed atopic dermatitis, asthma and allergic rhinitis in the period of 2003–2012, grouped by status of TCM use.
| Atopic dermatitis (n = 28,771) |
Asthma (n = 71,838) |
Allergic rhinitis (n = 191,851) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TCM use |
No TCM use |
χ2,b | P | SMDd | TCM use |
No TCM use |
χ2 | P | SMD | TCM use |
No TCM use |
χ2 | P | SMD | |
| (n = 8772) |
(n = 19,999) |
(n = 20,866) |
(n = 50,972) |
(n = 87,649) |
(n = 104,202) |
||||||||||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||||||||||
| Age, years | |||||||||||||||
| Age<10 | 1584 (18.06) | 5637 (28.19) | 488.2 | <10−5 | 0.29 | 5272 (25.27) | 17,877 (35.07) | 943.7 | <10−5 | 0.25 | 15,223 (17.37) | 25,446 (24.42) | 3290.1 | <10−5 | 0.27 |
| 10 ≤ age<30 | 2414 (27.52) | 4639 (23.20) | 3155 (15.12) | 6775 (13.29) | 28,950 (33.03) | 27,532 (26.42) | |||||||||
| 30 ≤ age<50 | 2408 (27.45) | 3877 (19.39) | 4658 (22.32) | 7643 (14.99) | 26,610 (30.36) | 24,987 (23.98) | |||||||||
| Age≥50 | 2366 (26.97) | 5846 (29.23) | 7781 (37.29) | 18,677 (36.64) | 16,866 (19.24) | 26,237 (25.18) | |||||||||
| Sex | |||||||||||||||
| Females | 5343 (60.91) | 10,061 (50.31) | 275.5 | <10−5 | 0.22 | 11,649 (55.83) | 24,163 (47.40) | 420.2 | <10−5 | 0.17 | 49,162 (56.09) | 49,675 (47.67) | 1350.6 | <10−5 | 0.17 |
| Males | 3429 (39.09) | 9938 (49.69) | 9217 (44.17) | 26,809 (52.60) | 38,487 (43.91) | 54,527 (52.33) | |||||||||
| Enrollee category | |||||||||||||||
| I | 647 (7.38) | 1214 (6.07) | 38.6 | <10−5 | 0.08 | 1476 (7.07) | 2962 (5.81) | 138.3 | <10−5 | 0.10 | 7367 (8.41) | 7054 (6.77) | 594.6 | <10−5 | 0.11 |
| II | 2594 (29.57) | 5677 (28.39) | 5723 (27.43) | 13,307 (26.11) | 30,088 (34.33) | 32,947 (31.62) | |||||||||
| III | 2324 (26.49) | 5331 (26.66) | 6291 (30.15) | 14,454 (28.36) | 20,969 (23.92) | 24,837 (23.84) | |||||||||
| IV | 1022 (11.65) | 2737 (13.69) | 2676 (12.82) | 7299 (14.32) | 8798 (10.04) | 12,925 (12.40) | |||||||||
| Other | 2185 (24.91) | 5040 (25.20) | 4700 (22.52) | 12,950 (25.41) | 20,427 (23.31) | 26,439 (25.37) | |||||||||
| Geographical area | |||||||||||||||
| Urban | 2661 (30.34) | 6043 (30.22) | 24.3 | 2.2 × 10−5 | 0.06 | 5902 (28.29) | 14,269 (27.99) | 11.9 | 7.9 × 10−3 | 0.03 | 26,216 (29.91) | 32,364 (31.06) | 81.2 | <10−5 | 0.07 |
| Suburban | 4954 (56.48) | 10,918 (54.59) | 11,885 (56.96) | 28,667 (56.24) | 51,184 (58.40) | 58,779 (56.41) | |||||||||
| Rural | 775 (8.83) | 1937 (9.69) | 1957 (9.38) | 5061 (9.93) | 6098 (6.96) | 7807 (7.49) | |||||||||
| Other |
382 (4.35) |
1101 (5.51) |
1122 (5.38) |
2975 (5.84) |
4151 (4.74) |
5252 (5.04) |
|||||||||
| TCM use |
No TCM use |
tc | P | SMD | TCM use |
No TCM use |
t | P | SMD | TCM use |
No TCM use |
t | P | SMD | |
| Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
Mean ± SD |
||||||||||
| Health utilizationa | |||||||||||||||
| No. of inpatient visits | 0.18 ± 0.75 | 0.23 ± 0.80 | 4.9 | <10−5 | 0.06 | 0.36 ± 0.94 | 0.47 ± 1.14 | 13.4 | <10−5 | 0.11 | 0.13 ± 0.52 | 0.19 ± 0.66 | 22.7 | <10−5 | 0.10 |
| No. of outpatient visits | 31.43 ± 19.75 | 25.07 ± 18.34 | 25.7 | <10−5 | 0.33 | 34.38 ± 20.24 | 26.12 ± 17.95 | 51.3 | <10−5 | 0.43 | 26.85 ± 17.33 | 21.92 ± 15.82 | 64.7 | <10−5 | 0.30 |
Abbreviation: TCM: traditional Chinese medicine; SD: standard deviation; SMD: standardized mean difference.
Health utilization is calculated based on one year after the index date.
Critical values were calculated by chi-squared test.
Critical values were calculated by Student's t-test.
SMD more than or equal to 0.1 between two groups is marked in bold.
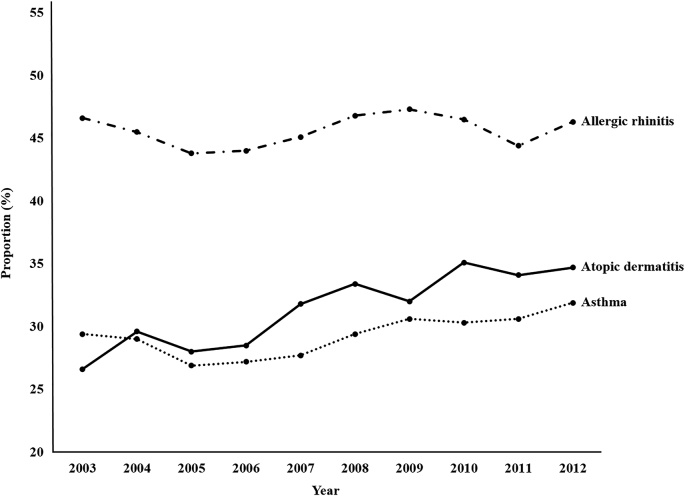
We examined the time trends of TCM use in subjects with atopic dermatitis, asthma and allergic rhinitis, separately, over the study period of 2003–2012. The overall proportions of TCM use were 30.5%, 29.0% and 45.7% in subjects with atopic dermatitis, asthma and allergic rhinitis, respectively. Significantly increasing trends in TCM use were observed among subjects with atopic dermatitis and asthma, individually, from 2003 to 2012 (Fig. 2). Specifically, the proportion of TCM use among subjects with atopic dermatitis increased from 26.6% in 2003 to 34.7% in 2012, with a β of 0.91, indicating that there was a 0.91% annual increase of TCM use. The proportion of TCM use among subjects with asthma increased from 29.4% in 2003 to 31.9% in 2012, with a β of 0.38, indicating that there was a 0.38% annual increase of TCM use. On the other hand, the proportions of TCM use for subjects with allergic rhinitis ranged from 46.6% in 2003 to 46.3% in 2012, without a significant trend change over the 10-year study period (Fig. 2).
Fig. 2.
Time trends of TCM use among subjects with atopic dermatitis, asthma and allergic rhinitis, separately, in the period of 2003–2012.
The top 10 TCM single herbs and herbal formulas for treating atopic dermatitis, asthma and allergic rhinitis, respectively, were shown in Table 2, Table 3, Table 4. Among subjects with atopic dermatitis, three most commonly prescribed single herbs were Huang-qin (1.81%), Gan-cao (1.63%), and Yan-hu-suo (1.63%); and three most commonly prescribed herbal formulas were Xiao-feng-san (2.83%), Jia-wei-xiao-yao-san (2.63%), and Xin-yi-qing-fei-tang (2.49%) (Table 2). Among subjects with asthma, three most commonly prescribed single herbs were Bei-mu (2.49%), Jie-geng (2.32%), and Ku-xing-ren (2.3%); and three most commonly prescribed herbal formulas were Xiao-ching-lung-tang (3.37%), Ma-xing-gan-shi-tang (3.31%), and Xin-yi-qing-fei-tang (2.93%) (Table 3). Among subjects with allergic rhinitis, three most commonly prescribed single herbs were Jie-geng (2.07%), Bai-zhi (1.99%), and Huang-qin (1.94%); and three most commonly prescribed herbal formulas were Xin-yi-qing-fei-tang (4.13%), Xiao-ching-lung-tang (3.50%), and Xin-yi-san (3.15%) (Table 4).
Table 2.
The top 10 commonly prescribed single herbs and herbal formulas for treating patients with atopic dermatitis in 2003–2012.
| Single herbs | |||||
|---|---|---|---|---|---|
| Pin-yin name | Latin name | Botanical plant name | Therapeutic indication | N | % |
| Huang-qin | Radix Scutellariae | Scutellaria baicalensis Georgi | Clear heat and dry dampness, purge fire, relieve toxicity, cool blood and stop bleeding. | 1204 | 1.81 |
| Gan-cao | Radix Glycyrrhizae | Glycyrrhiza uralensis Fisch. | Tonify qi of heart and spleen, dispel phlegm, relieve cough and dyspnea, relieve spasm and pain, clear heat, relieve toxicity, and harmonize property of medicine. | 1085 | 1.63 |
| Yan-hu-suo | Rhizoma Corydalis | Corydalis yanhusuo W. T. Wang | Activate blood, promote flow of qi, and alleviate pain. | 1084 | 1.63 |
| Jie-geng | Radix Platycodonis | Platycodon grandiflorum (Jacq.) A. DC. | Ventilate lung, dispel phlegm, relieve sore throat, and expel pus. | 1044 | 1.57 |
| Chan-tui | Periostracum Cicadae | Cryptotympana pustulata Fabricius | Disperse wind-heat, relieve sore throat and produce sound, relieve itching, promote eruption, improve vision and remove nebula, extinguish wind and relieve spasms. | 1004 | 1.51 |
| Bei-mu | Bulbus Fritillariae Cirrhosae or Bulbus Fritillariae Thunbergii | Fritillaria chrrhosa D. Don or Fritillaria thunbergii Miq. | Clear and resolve heat-phlegm, moisten and resolve dry phlegm, stop cough, dissipate nodulation and resolve swelling and cure abscess | 1000 | 1.50 |
| Lian-qiao | Forsythiae Fructus | Forsythia suspensa (Thunb.) Vahl. | Clear heat and remove toxicity, disperse wind-heat, and clear heart-heat. | 974 | 1.47 |
| Bai-zhi | Radix Angelicae Dahuricae | Angelica dahurica (Hoffm.) Benth. & Hook.f. ex Franch. & Sav. | Expel wind and release exterior, alleviate pain, relieve stuffy nose, dry dampness and stop leucorrhea. | 968 | 1.46 |
| Mu-dan-pi | Cortex Moutan | Paeonia suffruticosa Andr. | Clear heat and cool blood, activate blood and resolve stasis, and reduce deficiency heat. | 862 | 1.30 |
| Ku-xing-ren | Semen Armeniacae Amarae | Prunus armeniaca L. | Relieve cough and dyspnea, moisten intestines for relaxing bowels. | 855 | 1.29 |
| Herbal formulas | |||||
|---|---|---|---|---|---|
| Pin-yin name | English name | Ingredients of herbal formula Pin-yin name (Latin name) |
Therapeutic indication | N | % |
| Xiao-feng-san | Wind Dispersing Powder | Dang-gui (Radix Angelicae Sinensis), Sheng-di (Radix Rehmanniae), Fang-feng (Radix Ledebouriellae), Chan-tui (Periostracum Cicadae), Zhi-mu (Rhizoma Anemarrhenae), Ku-shen (Radix Sophorae Flavescentis), Hu-ma-ren (Semen Sesamum), Jing-jie (Herba Schizonepetae), Cang-zhu (Rhizoma Atractylodis), Niu-bang-zi (Fructus Arctii), Shi-gao (Gypsum Fibrosum), Gan-cao (Radix Glycyrrhizae), Mu-tong (Caulis Akebiae) | Dispel wind pathogen, nourish blood, and remove dampness and heat. | 1583 | 2.83 |
| Jia-wei-xiao-yao-san | Supplemented Free Wanderer Powder | Dang-gui (Radix Angelicaesinensis), Fu-ling (Poria), Zhi-zi (Fructus Gardeniae), Bo-he (Herba Menthae), Bai-shao-yao (Radix Paeornate), Chai-hu (Radix Bupleuri), Gan-cao (Radix Glycyrrhizae), Bai-zhu (Rhizoma Macrocephalae), Mu-dan-pi (Cortex Moutan), Gan-jiang (Rhizoma Zingiberis) | Tonify blood, clear liver fire and strengthen the spleen. | 1473 | 2.63 |
| Xin-yi-qing-fei-tang | Magnolia and Gypsum Combination | Shi-gao (Gypsum Fibrosum), Huang-qin (Radix Scutellariae), Zhi-zi (Fructus Gardeniae), Mai-men-dong (Radix Ophiopogonis), Bai-he (Bulbus Lilii), Zhi-mu (Rhizoma Anemarrhenae), Pi-pa-ye (Folium Eriobotryae), Xin-yi (Flos Magnoliae), Gan-cao (Radix Glycyrrhizae), Sheng-ma (Rhizoma Cimicifugae) | Dispel the heat of lung, disseminatelung-qi, and unblock the orifices, especially the nose. | 1395 | 2.49 |
| Ge-gen-tang | Puerariae Decoction | Ge-gen (Radix Puerariae), Ma-huang (Herba Ephedrae), Gui-zhi (Ramulus Cinnamomi), Bai-shao (Radix Paeoniae), Zhi-gan-cao (Radix Glycyrrhizae), Sheng-jiang (Zingiberis Rhizoma Recens), Da-zao (Zizyphi Fructus) | Relieve exterior syndrome by means of diaphoresis, remove toxicity, relax the tendons, and temper the stomach and spleen. | 1203 | 2.15 |
| Ma-xing-gan-shi-tang | Mahuang and Apricot Seed Combination | Ma-huang (Herba Ephedrae), Xing-ren (Semen Armeniacae), Zhi-gan-cao (Radix Glycyrrhizae), Shi-gao (Gypsum Fibrosum) | Disperse superficial pathogens, and remove heat from the lung to relieve asthma. | 1159 | 2.07 |
| Yin-qiao-san | Honeysuckle and Forsythia Powder | Jin-yin-hua (Flos Lonicerae), Lian-qiao (Forsythiae Fructus), Jie-geng (Radix Platycodi), Niu-bang-zi (Fructus Arctii), Bo-he (Herba Menthae), Dan-dou-chi (Semen Sojae Praeparata), Jing-jie (Herba Schizonepetae), Dan-zhu-ye (Herba Lophatheri), Xian-lu-gen (Rhizoma Phragmitis), Gan-cao (Radix Glycyrrhizae) | Dispel pathogenic factors in the superficies, and clear away heat and toxic material. | 1115 | 1.99 |
| Xiao-ching-lung-tang | Minor Blue Dragon Combination | Ma-huang (Herba Ephedrae), Shao-yao (Radix Paeoniae Alba), Gan-jiang (Rhizoma Zingiberis), Wu-wei-zi (Fructus Schisandrae), Gui-zhi (Ramulus Cinnamomi), Ban-xia (Rhizoma Pinelliae), Xi-xin (Herba Asari), Zhi-gan-cao (Radix Glycyrrhizae) | Induce diaphoresis to reduce watery phlegm, and relieve cough and asthma. | 1040 | 1.86 |
| Jing-fang-bai-du-san | Schizonepeta and Siler Formula | Jing-jie (Herba Schizonepetae), Fang-feng (Radix Saposhnikoviae), Qiang-huo (Rhizoma et Radix Notopterygii), Du-huo (Radix Angelicae Pubescentis), Chai-hu (Radix Bupleuri), Qian-hu (Radix Peucedani), Chuan-xiong (Rhizoma Chuanxiong), Jie-geng (Radix Platycodi), Fu-ling (Poria), Sheng-jiang (Zingiberis Rhizoma Recens), Bo-he (Herba Menthae), Zhi-ke (Fructus Aurantii), Gan-cao (Radix Glycyrrhizae) | Dispel wind-cold, relieve exterior syndrome, and eliminate dampness. | 1006 | 1.80 |
| Shu-jing-huo-xue-tang | Channel-Coursing Blood-Quickening Decoction | Dang-gui (Radix Angelicae Sinensis), Shao-yao (Radix Paeoniae Alba), Sheng-di (Radix Rehmanniae), Cang-zhu (Rhizoma Atractylodis), Huai-niu-xi (Radix Achyranthis Bidentatae), Chen-pi (Pericarpium Citri Reticulatae), Tao-ren (Semen Persicae), Wei-ling-xian (Radix Clematidis), Qiang-huo (Rhizoma et Radix Notopterygii), Fang-feng (Radix Saposhnikoviae), Long-dan-cao (Radix Gentianae), Chuan-xiong (Rhizoma Chuanxiong), Bai-zhi (Radix Angelicae Dahuricae), Fu-ling (Poria), Gan-cao (Radix Glycyrrhizae) | Unblock and relax the channels, invigorate the blood, break up blood stasis, dispel wind-dampness, and strengthen the tendons. | 932 | 1.67 |
| Long-dan-xie-gan-tang | Gentian Liver-Purging Decoction | Long-dan-cao (Radix Gentianae), Chai-hu (Radix Bupleuri), Huang-qin (Radix Scutellariae), Zhi-zi (Fructus Gardeniae), Ze-xie (Rhizoma Alismatis), Che-qian-zi (Semen Plantaginis), Mu-tong (Caulis Akebiae), Dang-gui (Radix Angelicae Sinensis), Sheng-di (Radix Rehmanniae), Gan-cao (Radix Glycyrrhizae) | Purge excessive pathogenic fire in the liver and gallbladder, and clear away damp-heat in the lower-jiao. | 929 | 1.66 |
Table 3.
The top 10 commonly prescribed single herbs and herbal formulas for treating patients with asthma in 2003–2012.
| Single herbs | |||||
|---|---|---|---|---|---|
| Pin-yin name | Latin name | Botanical plant name | Therapeutic indication | N | % |
| Bei-mu | Bulbus Fritillariae Cirrhosae or Bulbus Fritillariae Thunbergii | Fritillaria chrrhosa D. Don or Fritillaria thunbergii Miq. | Clear and resolve heat-phlegm, moisten and resolve dry-phlegm, stop cough, dissipate nodulation and resolve swelling, and cure abscess | 3974 | 2.49 |
| Jie-geng | Radix Platycodonis | Platycodon grandiflorum (Jacq.) A. DC. | Ventilate lung, dispel phlegm, relieve sore throat, and expel pus. | 3704 | 2.32 |
| Ku-xing-ren | Semen Armeniacae Amarae | Prunus armeniaca L. | Relieve cough and dyspnea, and moisten intestines for relaxing bowels. | 3675 | 2.30 |
| Huang-qin | Radix Scutellariae | Scutellaria baicalensis Georgi | Clear heat and dry dampness, purge fire, relieve toxicity, cool blood and stop bleeding. | 2940 | 1.84 |
| Gan-cao | Radix Glycyrrhizae | Glycyrrhiza uralensis Fisch. | Tonify qi of heart and spleen, dispel phlegm, relieve cough and dyspnea, relieve spasm and pain, clear heat, relieve toxicity, and harmonize property of medicine. | 2655 | 1.66 |
| Yu-xing-cao | Houttuyniae Herba | Houttuynia cordata Thunb. | Clear heat and remove toxicity, cure abscess and discharge pus, clear lung heat, clear heat and remove dampness. | 2324 | 1.45 |
| Yan-hu-suo | Rhizoma Corydalis | Corydalis yanhusuo W. T. Wang | Activate blood, promote flow of qi, and alleviate pain. | 2317 | 1.45 |
| Bai-zhi | Radix Angelicae Dahuricae | Angelica dahurica (Hoffm.) Benth. & Hook.f. ex Franch. & Sav. | Expel wind and release exterior, alleviate pain, relieve stuffy nose, dry dampness and stop leucorrhea. | 2255 | 1.41 |
| Mai-men-dong | Radix Ophiopogonis | Ophiopogon japonicus (L.f.) Ker-Gawl. | Nourish yin of stomach, lung and heart, clear heat of stomach, lung and heart, calm heart and induce tranquilization. | 2121 | 1.33 |
| Hou-po | Magnoliae Officinalis Cortex | Magnolia officinalis Rehd. et Wils. | Dry dampness, move qi, and relieve dyspnea. | 2004 | 1.25 |
| Herbal formulas | |||||
|---|---|---|---|---|---|
| Pin-yin name | English name | Ingredients of herbal formula Pin-yin name (Latin name) |
Therapeutic indication | N | % |
| Xiao-ching-lung-tang | Minor Blue Dragon Combination | Ma-huang (Herba Ephedrae), Shao-yao (Radix Paeoniae Alba), Gan-jiang (Rhizoma Zingiberis), Wu-wei-zi (Fructus Schisandrae), Gui-zhi (Ramulus Cinnamomi), Ban-xia (Rhizoma Pinelliae), Xi-xin (Herba Asari), Zhi-gan-cao (Radix Glycyrrhizae) | Induce diaphoresis to reduce watery phlegm, and relieve cough and asthma. | 4640 | 3.37 |
| Ma-xing-gan-shi-tang | Mahuang and Apricot Seed Combination | Ma-huang (Herba Ephedrae), Xing-ren (Semen Armeniacae), Zhi-gan-cao (Radix Glycyrrhizae), Shi-gao (Gypsum Fibrosum) | Disperse superficial pathogens, and remove heat from the lung to relieve asthma. | 4555 | 3.31 |
| Xin-yi-Qing-fei-tang | Magnolia and Gypsum Combination | Shi-gao (Gypsum Fibrosum), Huang-qin (Radix Scutellariae), Zhi-zi (Fructus Gardeniae), Mai-men-dong (Radix Ophiopogonis), Bai-he (Bulbus Lilii), Zhi-mu (Rhizoma Anemarrhenae), Pi-pa-ye (Folium Eriobotryae), Xin-yi (Flos Magnoliae), Gan-cao (Radix Glycyrrhizae), Sheng-ma (Rhizoma Cimicifugae) | Dispel the heat of lung, and disseminate lung-qi, and unblock the orifices, especially the nose. | 4029 | 2.93 |
| Ding-chuan-tang | Arrest Wheezing Decoction | Bai-guo (Semen Ginkgo), Ma-huang (Herba Ephedrae), Su-zi (Fructus Perillae), Gan-cao (Radix Glycyrrhizae), Kuan-dong-hua (Flos Farfarae), Xing-ren (Semen Armeniacae), Huang-qin (Radix Scutellariae), Ban-xia (Rhizoma Pinelliae), Sang-bai-pi (Cortex Mori) | Facilitate the flow of the lung-qi to descend upward flow, eliminate phlegm and relieve asthma. | 3267 | 2.37 |
| Ge-gen-tang | Puerariae Decoction | Ge-gen (Radix Puerariae), Ma-huang (Herba Ephedrae), Gui-zhi (Ramulus Cinnamomi), Bai-shao (Radix Paeoniae), Zhi-gan-cao (Radix Glycyrrhizae), Sheng-jiang (Zingiberis Rhizoma Recens), Da-zao (Zizyphi Fructus) | Relieve exterior syndrome by means of diaphoresis, remove toxicity, relax the tendons and temper the stomach and spleen. | 3037 | 2.21 |
| Yin-qiao-san | Honeysuckle and Forsythia Powder | Jin-yin-hua (Flos Lonicerae), Lian-qiao (Forsythiae Fructus), Jie-geng (Radix Platycodi), Niu-bang-zi (Fructus Arctii), Bo-he (Herba Menthae), Dan-dou-chi (Semen Sojae Praeparata), Jing-jie (Herba Schizonepetae), Dan-zhu-ye (Herba Lophatheri), Xian-lu-gen (Rhizoma Phragmitis), Gan-cao (Radix Glycyrrhizae) | Dispel pathogenic factors in the superficies, and clear away heat and toxic material. | 2720 | 1.98 |
| Xin-yi-san | Magnolia Flower Powder | Xin-yi (Flos Magnoliae), Chuan-xiong (Rhizoma Chuanxiong), Mu-tong (Caulis Akebiae), Fang-feng (Radix Saposhnikoviae), Qiang-huo (Rhizoma et Radix Notopterygii), Gao-ben (Radices Ligustici Sinensis), Sheng-ma (Rhizoma Cimicifugae), Bai-zhi (Radix Angelicae Dahuricae), Zhi-gan-cao (Radix Glycyrrhizae) | Expel wind-cold, and unblock the nasal passages. | 2688 | 1.95 |
| Cang-er-san | Xanthium Powder | Cang-er-zi (Fructus Xanthii), Xin-yi (Flos Magnoliae), Bai-zhi (Radix Angelicae Dahuricae), Bo-he (Herba Menthae) | Disperse wind, alleviates pain, and unblock the nose. | 2678 | 1.94 |
| Zhi-sou-san | Stop Coughing Powder | Zi-wan (Radix Asteris), Bai-bu (Radix Stemonae), Bai-qian (Rhizoma Cynanchi Stauntonii), Jing-jie (Herba Schizonepetae), Jie-geng (Radix Platycodi), Chen-pi (Pericarpium Citri Reticulatae), Gan-cao (Radix Glycyrrhizae) | Stop coughing, transform phlegm, release the exterior, and ventilate the lungs. | 2588 | 1.88 |
| Jia-wei-xiao-yao-san | Supplemented Free Wanderer Powder | Dang-gui (Radix Angelicaesinensis), Fu-ling (Poria), Zhi-zi (Fructus Gardeniae), Bo-he (Herba Menthae), Bai-shao-yao (Radix Paeornate), Chai-hu (Radix Bupleuri), Gan-cao (Radix Glycyrrhizae), Bai-zhu (Rhizoma Macrocephalae), Mu-dan-pi (Cortex Moutan), Gan-jiang (Rhizoma Zingiberis) | Tonify blood, clear liver fire, and strengthen the spleen. | 2316 | 1.68 |
Table 4.
The top 10 commonly prescribed single herbs and herbal formulas for treating patients with allergic rhinitis in 2003–2012.
| Single herbs | |||||
|---|---|---|---|---|---|
| Pin-yin name | Latin name | Botanical plant name | Therapeutic indication | N | % |
| Jie-geng | Radix Platycodonis | Platycodon grandiflorum (Jacq.) A. DC. | Ventilate lung, dispel phlegm, relieve sore throat, and expel pus. | 16,279 | 2.07 |
| Bai-zhi | Radix Angelicae Dahuricae | Angelica dahurica (Hoffm.) Benth. & Hook.f. ex Franch. & Sav. | Expel wind and release exterior, alleviate pain, relieve stuffy nose, dry dampness and stop leucorrhea. | 15,642 | 1.99 |
| Huang-qin | Radix Scutellariae | Scutellaria baicalensis Georgi | Clear heat and dry dampness, purge fire and relieve toxicity, cool blood and stop bleeding. | 15,263 | 1.94 |
| Bei-mu | Bulbus Fritillariae Cirrhosae or Bulbus Fritillariae Thunbergii | Fritillaria chrrhosa D. Don or Fritillaria thunbergii Miq. | Clear and resolve heat-phlegm, moisten and resolve dry-phlegm, stop cough, dissipate nodulation and resolve swelling and cure abscess | 14,443 | 1.84 |
| Cang-er-zi | Fructus Xanthii | Xanthium sibiricum Patr. | Disperse wind-cold, relieve nasal obstruction and stop pain. | 13,146 | 1.67 |
| Ku-xing-ren | Semen Armeniacae Amarae | Prunus armeniaca L. | Relieve cough and dyspnea, and moisten intestines for relaxing bowels. | 12,857 | 1.64 |
| Gan-cao | Radix Glycyrrhizae | Glycyrrhiza uralensis Fisch. | Tonify qi of heart and spleen, dispel phlegm, relieve cough and dyspnea, relieve spasm and pain, clear heat and relieve toxicity, and harmonize property of medicine. | 12,413 | 1.58 |
| Yu-xing-cao | Houttuyniae Herba | Houttuynia cordata Thunb. | Clear heat and remove toxicity, cure abscess and discharge pus, clear lung heat, clear heat and remove dampness. | 11,725 | 1.49 |
| Chan-tui | Periostracum Cicadae | Cryptotympana pustulata Fabricius | Disperse wind-heat, relieve sore throat and produce sound, relieve itching and promote eruption, improve vision and remove nebula, and extinguish wind and relieve spasms. | 11,543 | 1.47 |
| Yan-hu-suo | Rhizoma Corydalis | Corydalis yanhusuo W. T. Wang | Activate blood, promote flow of qi, and alleviate pain. | 10,987 | 1.40 |
| Herbal formulas | |||||
|---|---|---|---|---|---|
| Pin-yin name | English name | Ingredients of herbal formula Pin-yin name (Latin name) | Therapeutic indication | N | % |
| Xin-yi-qing-fei-tang | Magnolia and Gypsum Combination | Shi-gao (Gypsum Fibrosum), Huang-qin (Radix Scutellariae), Zhi-zi (Fructus Gardeniae), Mai-men-dong (Radix Ophiopogonis), Bai-he (Bulbus Lilii), Zhi-mu (Rhizoma Anemarrhenae), Pi-pa-ye (Folium Eriobotryae), Xin-yi (Flos Magnoliae), Gan-cao (Radix Glycyrrhizae), Sheng-ma (Rhizoma Cimicifugae) | Dispel the heat of lung, disseminate lung-Qi, and unblock the orifices, especially the nose. | 27,222 | 4.13 |
| Xiao-ching-lung-tang | Minor Blue Dragon Combination | Ma-huang (Herba Ephedrae), Shao-yao (Radix Paeoniae Alba), Gan-jiang (Rhizoma Zingiberis), Wu-wei-zi (Fructus Schisandrae), Gui-zhi (Ramulus Cinnamomi), Ban-xia (Rhizoma Pinelliae), Xi-xin (Herba Asari), Zhi-gan-cao (Radix Glycyrrhizae) | Induce diaphoresis to reduce watery phlegm, and relieve cough and asthma. | 23,080 | 3.50 |
| Xin-yi-san | Magnolia Flower Powder | Xin-yi (Flos Magnoliae), Chuan-xiong (Rhizoma Chuanxiong), Mu-tong (Caulis Akebiae), Fang-feng (Radix Saposhnikoviae), Qiang-huo (Rhizoma et Radix Notopterygii), Gao-ben (Radices Ligustici Sinensis), Sheng-ma (Rhizoma Cimicifugae), Bai-zhi (Radix Angelicae Dahuricae), Zhi-gan-cao (Radix Glycyrrhizae) | Expel wind-cold, and unblock the nasal passages. | 20,780 | 3.15 |
| Cang-er-san | Xanthium Powder | Cang-er-zi (Fructus Xanthii), Xin-yi (Flos Magnoliae), Bai-zhi (Radix Angelicae Dahuricae), Bo-he (Herba Menthae) | Disperse wind, alleviates pain, and unblock the nose. | 19,686 | 2.98 |
| Ge-gen-tang | Puerariae Decoction | Ge-gen (Radix Puerariae), Ma-huang (Herba Ephedrae), Gui-zhi (Ramulus Cinnamomi), Bai-shao (Radix Paeoniae), Zhi-gan-cao (Radix Glycyrrhizae), Sheng-jiang (Zingiberis Rhizoma Recens), Da-zao (Zizyphi Fructus) | Relieve exterior syndrome by means of diaphoresis, remove toxicity, relax the tendons, and temper the stomach and spleen. | 18,857 | 2.86 |
| Ma-xing-gan-shi-tang | Mahuang and Apricot Seed Combination | Ma-huang (Herba Ephedrae), Xing-ren (Semen Armeniacae), Zhi-gan-cao (Radix Glycyrrhizae), Shi-gao (Gypsum Fibrosum) | Disperse superficial pathogens, and remove heat from the lung to relieve asthma. | 15,382 | 2.33 |
| Jia-wei-xiao-yao-san | Supplemented Free Wanderer Powder | Dang-gui (Radix Angelicaesinensis), Fu-ling (Poria), Zhi-zi (Fructus Gardeniae), Bo-he (Herba Menthae), Bai-shao-yao (Radix Paeornate), Chai-hu (Radix Bupleuri), Gan-cao (Radix Glycyrrhizae), Bai-zhu (Rhizoma Macrocephalae), Mu-dan-pi (Cortex Moutan), Gan-jiang (Rhizoma Zingiberis) | Tonify blood, clear liver fire, and strengthen the spleen. | 14,737 | 2.23 |
| Yin-qiao-san | Honeysuckle and Forsythia Powder | Jin-yin-hua (Flos Lonicerae), Lian-qiao (Forsythiae Fructus), Jie-geng (Radix Platycodi), Niu-bang-zi (Fructus Arctii), Bo-he (Herba Menthae), Dan-dou-chi (Semen Sojae Praeparata), Jing-jie (Herba Schizonepetae), Dan-zhu-ye (Herba Lophatheri), Xian-lu-gen (Rhizoma Phragmitis), Gan-cao (Radix Glycyrrhizae) | Dispel pathogenic factors in the superficies, and clear away heat and toxic material. | 14,264 | 2.16 |
| Chuan-xiong-cha-tiao-san | Ligusticum Chuanxiong Powder to Be Taken with Green Tea | Bo-he (Herba Menthae), Chuan-xiong (Rhizoma Chuanxiong), Qiang-huo (Rhizoma et Radix Notopterygii), Bai-zhi (Radix Angelicae Dahuricae) Jing-jie (Herba Schizonepetae), Fang-feng (Radix Saposhnikoviae), Xi-xin (Herba Asari), Gan-cao (Radix Glycyrrhizae) |
Dispel wind pathogen, and relieve pain. | 12,212 | 1.85 |
| Bu-zhong-yi-qi-tang | Tonify the Middle and Augment the Qi Decoction | Huang-qi (Radix Astragali), Gan-cao (Radix Glycyrrhizae), Ren-shen (Radix Ginseng), Dang-gui (Radix Angelicae Sinensis), Chen-pi (Pericarpium Citri Reticulatae), Sheng-ma (Rhizoma Cimicifugae), Chai-hu (Radix Bupleuri), Bai-zhu (Rhizoma Atractylodis Macrocephalae) | Reinforce the middle-jiao and invigorate qi, and elevate yang-qi to treat prolapse. | 11,027 | 1.67 |
Discussion
This study identified 10-year trends and prescription patterns of TCM use among subjects with allergic diseases over the study period of 2003–2012 in Taiwan. To the best of our knowledge, this is the first study simultaneously evaluating 10-year trends and prescription patterns of TCM use in subjects with three common allergic diseases, specifically, atopic dermatitis, asthma and allergic rhinitis. Our study demonstrated that considerable proportions of patients with allergic diseases (30.5% for atopic dermatitis, 29% for asthma, and 45.7% for allergic rhinitis, respectively) in Taiwan had used TCM. The results showed increasing trends of TCM use over the 10-year study period among subjects with atopic dermatitis and asthma, respectively. When we assessed the proportions of TCM use among three examined allergic diseases, the highest proportion of TCM use was observed in subjects with allergic rhinitis, but the trend remained steady over the 10-year study period. Taken together, a notable proportion (30–50%) of subjects with allergic diseases in Taiwan had used TCM. Moreover, our results indicated that the number of inpatient visits in subjects with TCM use was significantly smaller than that in subjects without TCM use for all three examined allergic diseases.
To date, the trends and prescription patterns of TCM use in subjects with allergic diseases remain largely unclear. Our study demonstrated that considerable proportions of subjects with allergic diseases (30.5% for atopic dermatitis, 29% for asthma, and 45.7% for allergic rhinitis, respectively) had used TCM. Of note, we found increasing trends of TCM use among subjects with atopic dermatitis and asthma, respectively. Particularly, we observed a 0.91% annual increase for subjects with atopic dermatitis and a 0.38% annual increase for subjects with asthma, respectively. On the other hand, the proportions of TMC use for subjects with allergic rhinitis remained steadily high (from 46.6% in 2003 to 46.3% in 2012) over the 10-year study period. The reasons for the observed increasing trends of TCM use in three examined allergic diseases in Taiwan remain unclear but it may reflect common beliefs that TCM use may potentially “cure the root of allergic diseases” or “cut the tail of allergic diseases”. Besides, there is a general impression among some people in Chinese society including Taiwan that TCM use tends to have milder adverse effects, though with slower clinical effects than Western medicines.8
Previous studies have reported the therapeutic effects of TCM on allergic diseases.17, 18 For example, Chen et al examined whether TCM use affected combined use of corticosteroid among children with atopic dermatitis and found that TCM use reduced the number of corticosteroid prescriptions (both topical and systemic) among children with atopic dermatitis within one-year follow-up.17 The results from the Hung et al study have suggested that asthmatic children receiving adjuvant treatment with integrated TCM decreased frequency of emergency room visits and hospital admissions.18 However, the concern related to low certainty for efficacy of TCM use has been reported by previous studies.19, 20, 21 Thus, further investigation in making conclusive evidence for efficacy of TCM on allergic diseases would be warranted.
In parallel, pharmacological effects of single herbs and herbal formulas on three examined allergic diseases have been reported by several studies. First, three major pharmacological effects for TCM in treating subjects with atopic dermatitis have been documented, including anti-inflammation, reduction of histamine release, and anti-oxidation, respectively.17, 22 For example, Cheng et al investigated treatment effect of Xiao-feng-san, the top one prescribed herbal formula for treating subjects with atopic dermatitis in this study. Their results suggested that Xiao-feng-san might be an alternative therapeutic choice for subjects with severe and extensive atopic dermatitis.22 Second, both observational and animal studies have indicated that anti-asthmatic activity of TCM was through inhibiting bronchoconstriction and the migration of eosinophils to airway, and reducing airway hyper-responsiveness via regulating the Th2 cells.23, 24, 25, 26, 27 For instance, Wang et al demonstrated that Xiao-ching-lung-tang, the top one prescribed herbal formula for treating subjects with asthma in this study, has anti-inflammatory, anti-airway remodeling, and immune regulatory effects in their chronic asthmatic murine model.28 Previous studies have further indicated that pharmacological effects of TCM for treating allergic diseases were not only immune-modulatory effects, but also anti-inflammatory effect.29, 30 A randomized double blind study has reported that Xin-yi-san, one of the top 10 commonly prescribed herbal formulas in treating subjects with allergic rhinitis in the present study, has pharmacological effects on attenuating clinical symptoms of patients with perennial allergic rhinitis and exerting diverse immunomodulatory effects, such as suppression of serum immunoglobulin E levels and enhanced production of interleukin (IL)-10, IL-8, and soluble intercellular adhesion molecule (sICAM).31 Yang et al evaluated potential mechanisms regarding treatment effect of Bu-zhong-yi-qi-tang, also one of the top 10 commonly prescribed herbal formulas in treating subjects with allergic rhinitis in the present study, in patients with perennial allergic rhinitis. Their results suggested that Bu-zhong-yi-qi-tang played an anti-inflammation role through suppressing prostaglandin E2 (PGE2) and leukotriene C4 (LTC4).29
Of note, we have found notably extent of the top 10 commonly prescribed TCM (both single herbs and herbal formulas) among these three allergic diseases are the same. For example, Huang-qin is the top one single herbs prescribed in subjects with atopic dermatitis, the top four single herbs prescribed in subjects with asthma, and the top three single herbs prescribed in subjects with allergic rhinitis; whereas Xin-yi-qing-fei-tang is the top three herbal formula prescribed in subjects with atopic dermatitis, the top three herbal formula prescribed in subjects with asthma, and the top one herbal formula prescribed in subjects with allergic rhinitis. The observed results may be partly supported by the following explanations. According to the visceral manifestation theory in TCM, all these three allergic diseases are related to the same visceral, “lung”. It is known that “lung” is a pair of organs locating in the thoracic cavity above the diaphragm. It controls respiration, dominates “qi” (the circulating life force whose existence and properties are the basis of traditional Chinese medicine and philosophy), governs diffusion and depurative down-bearing and regulates the waterways, therefore, is closely related to the function of the nose and skin surface.32 It is different from the view of Western medicines that both allergic rhinitis and asthma are belonged to respiratory system whereas atopic dermatitis is belonged to dermatological field. In addition, epidemiological data documents that coexistence of atopic dermatitis, asthma and allergic rhinitis is commonly occurred in the same subject, suggesting these allergic diseases share common causal mechanisms.33 Furthermore, previous studies have reported that Scutellariae radix (Latin name of Huang-qin) attenuates immunological responses in a mouse model of atopic dermatitis, mainly through decreasing IL-5 levels; modulates ovalbumin (OVA)-induced airway inflammation through suppressing IL-4/Stat6 signaling in a murine model of asthma; and baicalin, another component extracted from Scutellariae radix, effectively reduce allergic response in an OVA-induced allergic rhinitis animal model.34, 35, 36 Findings from previous studies have lent further support for the observed overlapping prescriptions of TCM in three allergic diseases investigated in this study.
Some caveats in this study should be noted. First, detailed information on clinical symptoms and laboratory reports are not available in the NHRID. But this issue should be undifferentiated between subjects with and without TCM use. Second, the NHIP in Taiwan only reimburses granular or powder forms of TCM herbs and formulas recording in the “Taiwan Herbal Pharmacopeia” that is published by Taiwan's Ministry of Health and Welfare (https://www.mohw.gov.tw/dl-10568-0efff195-8aff-4f6a-b19f-c18fbbf8dfb0.html). On the other hand, TCM in herbal form and herbal folk medicine are not reimbursed by the NHIP and are not included in this study. Therefore, it is likely that the prevalence of TCM use in three examined allergic diseases may be underestimated. Third, our results may or may not be generalizable, as the common prescription knowledge base among licensed TCM physicians might vary across countries. As such, caution should be taken when interpreting the results in this study. Fourth, the big standard deviations of age at diagnosis of allergic diseases in subjects with or without TCM use were noticed. Since we did not exclude study subjects based on their age, both children and adults were included in this study. It was likely a result of the observed big standard deviations.
Conclusion
In conclusion, a notable proportion (30–50%) of subjects with allergic diseases in Taiwan has used TCM, with the highest proportion of TCM use in subjects with allergic rhinitis, whereas increasing trends of TCM use are found among subjects with atopic dermatitis and asthma, respectively. Moreover, our results suggest that TCM use may help reduce severe episodes of these three allergic diseases that necessitate hospitalizations. Further investigation would be merited to better understand the efficacy and safety of TCM, particularly, potential interactions with Western medicines.
Declarations
Ethics approval and consent to participate
The Institutional Review Board of the National Health Research Institutes, Taiwan, approved this study protocol.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Funding
HJT and TCY are supported in part by grants from the Ministry of Science and Technology, National Health Research Institutes, and Chang Gung Memorial Hospital (PI: HJT, MOST 103-2314-B-400-004-MY3, MOST 107-2314-B-400-031-MY3, PH-105-SP-05, PH-105-SP-04, and PH-106-PP-08; PI: TCY, MOST 103-2314-B-182-030, MOST 104-2314-B-182-046-MY2, MOST 106-2314-B-182-051-MY3, CORPG3H0101, CORPG3F0361, CMRPG3F1711, CORPG3F0081 and CMRPG3E1201).
Conflict of interest
The authors declare no conflict of interest.
Authors' contributions
Tsung-Chieh Yao and Hui-Ju Tsai conceptualized, designed and supervised the study; raised funding for the study and staff working on the project, assisted in data analysis, interpreted the results and drafted the manuscript. Ya-Wen Huang performed data analysis, assisted in data collection, interpreted the results, and drafted the manuscript. Pei-Ying Lin, Chun-Hui Chu and Fang-Yu Chang provided intellectual inputs and assisted in data analysis and results interpretation. All authors contributed to the interpretation and discussion of the results; read and approved the final article.
Acknowledgements
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by the National Health Research Institutes (Registered numbers: 99081, 99136, 99287, 101014, NHRID-101-548). The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health or National Health Research Institutes.
Contributor Information
Hui-Ju Tsai, Email: tsaihj@nhri.org.tw.
Tsung-Chieh Yao, Email: yao@adm.cgmh.org.tw.
References
- 1.Yao T.C., Ou L.S., Yeh K.W. Associations of age, gender, and BMI with prevalence of allergic diseases in children: PATCH study. J Asthma. 2011;48:503–510. doi: 10.3109/02770903.2011.576743. [DOI] [PubMed] [Google Scholar]
- 2.Gupta R., Sheikh A., Strachan D.P., Anderson H.R. Burden of allergic disease in the UK: secondary analyses of national databases. Clin Exp Allergy. 2004;34:520–526. doi: 10.1111/j.1365-2222.2004.1935.x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta R., Sheikh A., Strachan D.P., Anderson H.R. Time trends in allergic disorders in the UK. Thorax. 2007;62:91–96. doi: 10.1136/thx.2004.038844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Punekar Y.S., Sheikh A. Establishing the incidence and prevalence of clinician-diagnosed allergic conditions in children and adolescents using routinely collected data from general practices. Clin Exp Allergy. 2009;39:1209–1216. doi: 10.1111/j.1365-2222.2009.03248.x. [DOI] [PubMed] [Google Scholar]
- 5.WAO white book on allergy. http://www.worldallergy.org/definingthespecialty/white_book.php Available from:
- 6.Kabir Z., Manning P.J., Holohan J., Goodman P.G., Clancy L. Prevalence of symptoms of severe asthma and allergies in Irish school children: an ISAAC protocol study, 1995–2007. Int J Environ Res Publ Health. 2011;8:3192–3201. doi: 10.3390/ijerph8083192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vignola A.M. Effects of inhaled corticosteroids, leukotriene receptor antagonists, or both, plus long-acting beta2-agonists on asthma pathophysiology: a review of the evidence. Drugs. 2003;63(Suppl 2):35–51. doi: 10.2165/00003495-200363002-00004. [DOI] [PubMed] [Google Scholar]
- 8.Lam T.P. Strengths and weaknesses of traditional Chinese medicine and Western medicine in the eyes of some Hong Kong Chinese. J Epidemiol Community Health. 2001;55:762–765. doi: 10.1136/jech.55.10.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hassed C. An integrative approach to asthma. Aust Fam Physician. 2005;34:573–576. [PubMed] [Google Scholar]
- 10.Cheng S.H., Chiang T.L. The effect of universal health insurance on health care utilization in Taiwan. Results from a natural experiment. J Am Med Assoc. 1997;278:89–93. doi: 10.1001/jama.278.2.89. [DOI] [PubMed] [Google Scholar]
- 11.Suh D.C., Sung J., Gause D., Raut M., Huang J., Choi I.S. Economic burden of atopic manifestations in patients with atopic dermatitis – analysis of administrative claims. J Manag Care Pharm. 2007;13:778–789. doi: 10.18553/jmcp.2007.13.9.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hankin C.S., Cox L., Lang D. Allergy immunotherapy among Medicaid-enrolled children with allergic rhinitis: patterns of care, resource use, and costs. J Allergy Clin Immunol. 2008;121:227–232. doi: 10.1016/j.jaci.2007.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Marra F., Marra C.A., Richardson K. Antibiotic use in children is associated with increased risk of asthma. Pediatrics. 2009;123:1003–1010. doi: 10.1542/peds.2008-1146. [DOI] [PubMed] [Google Scholar]
- 14.Mamdani M., Sykora K., Li P. Reader's guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ. 2005;330:960–962. doi: 10.1136/bmj.330.7497.960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Austin P.C., Mamdani M.M. A comparison of propensity score methods: a case-study estimating the effectiveness of post-AMI statin use. Stat Med. 2006;25:2084–2106. doi: 10.1002/sim.2328. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez A.F., Mi X., Hammill B.G. Associations between aldosterone antagonist therapy and risks of mortality and readmission among patients with heart failure and reduced ejection fraction. J Am Med Assoc. 2012;308:2097–2107. doi: 10.1001/jama.2012.14795. [DOI] [PubMed] [Google Scholar]
- 17.Chen H.Y., Lin Y.H., Wu J.C. Use of traditional Chinese medicine reduces exposure to corticosteroid among atopic dermatitis children: a 1-year follow-up cohort study. J Ethnopharmacol. 2015;159:189–196. doi: 10.1016/j.jep.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Hung Y.C., Hung I.L., Sun M.F. Integrated traditional Chinese medicine for childhood asthma in Taiwan: a Nationwide cohort study. BMC Complement Altern Med. 2014;14:389. doi: 10.1186/1472-6882-14-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu S., Yang A.W., Xue C.C. Chinese herbal medicine for atopic eczema. Cochrane Database Syst Rev. 2013:CD008642. doi: 10.1002/14651858.CD008642.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tan H.Y., Zhang A.L., Chen D., Xue C.C., Lenon G.B. Chinese herbal medicine for atopic dermatitis: a systematic review. J Am Acad Dermatol. 2013;69:295–304. doi: 10.1016/j.jaad.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 21.Shi Z.F., Song T.B., Xie J., Yan Y.Q., Du Y.P. The traditional Chinese medicine and relevant treatment for the efficacy and safety of atopic dermatitis: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Altern Med. 2017;2017:6026434. doi: 10.1155/2017/6026434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng H.M., Chiang L.C., Jan Y.M., Chen G.W., Li T.C. The efficacy and safety of a Chinese herbal product (Xiao-Feng-San) for the treatment of refractory atopic dermatitis: a randomized, double-blind, placebo-controlled trial. Int Arch Allergy Immunol. 2011;155:141–148. doi: 10.1159/000318861. [DOI] [PubMed] [Google Scholar]
- 23.Yang S.H., Kao T.I., Chiang B.L., Chen H.Y., Chen K.H., Chen J.L. Immune-modulatory effects of bu-zhong-yi-qi-tang in ovalbumin-induced murine model of allergic asthma. PLoS One. 2015;10 doi: 10.1371/journal.pone.0127636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang T.P., Liu P.H., Lien A.S., Yang S.L., Chang H.H., Yen H.R. Characteristics of traditional Chinese medicine use in children with asthma: a nationwide population-based study. Allergy. 2013;68:1610–1613. doi: 10.1111/all.12273. [DOI] [PubMed] [Google Scholar]
- 25.Jayaprakasam B., Doddaga S., Wang R., Holmes D., Goldfarb J., Li X.M. Licorice flavonoids inhibit eotaxin-1 secretion by human fetal lung fibroblasts in vitro. J Agric Food Chem. 2009;57:820–825. doi: 10.1021/jf802601j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li G.Z., Chai O.H., Lee M.S., Han E.H., Kim H.T., Song C.H. Inhibitory effects of Houttuynia cordata water extracts on anaphylactic reaction and mast cell activation. Biol Pharm Bull. 2005;28:1864–1868. doi: 10.1248/bpb.28.1864. [DOI] [PubMed] [Google Scholar]
- 27.Choi J.H., Hwang Y.P., Lee H.S., Jeong H.G. Inhibitory effect of Platycodi Radix on ovalbumin-induced airway inflammation in a murine model of asthma. Food Chem Toxicol. 2009;47:1272–1279. doi: 10.1016/j.fct.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 28.Wang S.D., Lin L.J., Chen C.L. Xiao-Qing-Long-Tang attenuates allergic airway inflammation and remodeling in repetitive Dermatogoides pteronyssinus challenged chronic asthmatic mice model. J Ethnopharmacol. 2012;142:531–538. doi: 10.1016/j.jep.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 29.Yang S.H., Yu C.L. Antiinflammatory effects of Bu-zhong-yi-qi-tang in patients with perennial allergic rhinitis. J Ethnopharmacol. 2008;115:104–109. doi: 10.1016/j.jep.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 30.Furuya Y., Akashi T., Fuse H. Effect of Bu-zhong-yi-qi-tang on seminal plasma cytokine levels in patients with idiopathic male infertility. Arch Androl. 2004;50:11–14. doi: 10.1080/01485010490250515. [DOI] [PubMed] [Google Scholar]
- 31.Yang S.H., Yu C.L., Chen Y.L., Chiao S.L., Chen M.L. Traditional Chinese medicine, Xin-yi-san, reduces nasal symptoms of patients with perennial allergic rhinitis by its diverse immunomodulatory effects. Int Immunopharmacol. 2010;10:951–958. doi: 10.1016/j.intimp.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 32.Ma Z., Jia C., Guo J., Gu H., Miao Y. Features analysis of five-element theory and its basal effects on construction of visceral manifestation theory. J Tradit Chin Med. 2014;34:115–121. doi: 10.1016/s0254-6272(14)60064-9. [DOI] [PubMed] [Google Scholar]
- 33.Pinart M., Benet M., Annesi-Maesano I. Comorbidity of eczema, rhinitis, and asthma in IgE-sensitised and non-IgE-sensitised children in MeDALL: a population-based cohort study. Lancet Respir Med. 2014;2:131–140. doi: 10.1016/S2213-2600(13)70277-7. [DOI] [PubMed] [Google Scholar]
- 34.Kim J., Lee I., Park S., Choue R. Effects of Scutellariae radix and aloe vera gel extracts on immunoglobulin E and cytokine levels in atopic dermatitis NC/Nga mice. J Ethnopharmacol. 2010;132:529–532. doi: 10.1016/j.jep.2010.08.049. [DOI] [PubMed] [Google Scholar]
- 35.Ryu E.K., Kim T.H., Jang E.J. Wogonin, a plant flavone from Scutellariae radix, attenuated ovalbumin-induced airway inflammation in mouse model of asthma via the suppression of IL-4/STAT6 signaling. J Clin Biochem Nutr. 2015;57:105–112. doi: 10.3164/jcbn.15-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou Y.J., Wang H., Sui H.H., Li L., Zhou C.L., Huang J.J. Inhibitory effect of baicalin on allergic response in ovalbumin-induced allergic rhinitis guinea pigs and lipopolysaccharide-stimulated human mast cells. Inflamm Res. 2016;65:603–612. doi: 10.1007/s00011-016-0943-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.