Abstract
Background
Takotsubo cardiomyopathy (TCM) is a reversible acute cardiac disease that mimics acute myocardial infarction (AMI). In patients with a history of an old myocardial infarction who develop TCM, cardiac magnetic resonance imaging (CMRI) is the first-line non-invasive diagnostic tool for clearly discriminating between AMI and TCM.
Case summary
A 65-year-old woman who suffered a myocardial infarction in 2012, was admitted to undergo sigmoid colon tumour surgery in January 2017. Soon after surgery, she developed angina associated with ST-segment elevation, as shown by electrocardiography and increased cardiac enzyme levels. Acute coronary syndrome was diagnosed. She had a good clinical response to treatment with intravenous nitroglycerine, opioids, clopidogrel, aspirin, bisoprolol, and atorvastatin. Transthoracic echocardiography (TTE) showed anteroseptal and apical left ventricular akinesia with balloon-like dilatation, akinesia of the inferior wall and inferior interventricular septum, and global systolic dysfunction. Coronary angiography did not identify coronary artery lesions, and a tentative diagnosis of TCM was made. Cardiac magnetic resonance imaging confirmed the segmental contraction abnormalities seen in the TTE and identified myocardial oedema without delayed hyperenhancement after gadolinium administration, which confirmed the diagnosis of TCM and ruled out acute ischaemic damage. She was discharged when asymptomatic. Cardiac magnetic resonance imaging at 2 months showed disappearance of the anteroseptal and apical contraction abnormality, regression of myocardial oedema and normalization of global left ventricular systolic function.
Discussion
This case confirms that CMRI is a non-invasive diagnostic method for accurately differentiating between AMI and TCM in patients with a prior myocardial infarction. cardiac magnetic resonance imaging should be incorporated as a diagnostic criterion for TCM.
Keywords: Takotsubo cardiomyopathy, Takotsubo syndrome, Cardiac magnetic resonance, Acute myocardial infarction, Case report
Learning points
In post-menopausal women with a history of an old myocardial infarction, the differential diagnosis between Takotsubo cardiomyopathy (TCM) and acute myocardial infarction (AMI) is challenging but is crucial for making the correct diagnosis and providing the best treatment. Patients with suspected TCM may have an apical AMI defined by cardiac magnetic resonance imaging as the final diagnosis.
Cardiac magnetic resonance imaging is a non-invasive diagnostic method that offers an accurate differential diagnosis between AMI and TCM in patients with an old myocardial infarction.
Introduction
Takotsubo cardiomyopathy (TCM) is a reversible acute cardiac disease that, in its initial presentation, mimics acute myocardial infarction (AMI).1,2 Takotsubo cardiomyopathy is characterized by transient akinesia or dyskinesia, primarily affecting the apical region of the left ventricle (LV), electrocardiographic changes such as ST-segment elevation or T wave inversion, and increased levels of cardiac enzymes in the absence of coronary disease.3,4 Takotsubo cardiomyopathy mainly affects post-menopausal women and is usually triggered by an episode of acute emotional or unusual physical stress.5,6Some patients admitted with suspected AMI for whom coronary angiography has ruled out coronary artery disease might have definite AMI or another acute cardiac pathology that mimics it.2 Thus, the differential diagnosis can be challenging but is essential to ensure correct and optimal treatments. In patients with a history of myocardial infarction, the differential diagnosis is even more difficult. In this scenario, cardiac magnetic resonance imaging (CMRI) emerges as a first-line non-invasive diagnostic tool that allows clear discrimination between AMI and TCM.7 A recent study reported that 29% of patients with suspected TCM based on a pattern of left ventricular contraction had an apically localized AMI confirmed by CMRI.8 We present a patient with a history of an old myocardial infarction who developed TCM soon after colon surgery and whose diagnosis was confirmed by CMRI.
Timeline
| Time | Events |
|---|---|
| 5 years ago | Acute myocardial infarction of the inferior wall treated with primary angioplasty for a critical proximal right coronary lesion with two overlapping drug-eluting stents |
| Over last 5 years | Asymptomatic under cardioprotective treatment |
| December 2016 | Sigmoid colon tumour diagnosed incidentally |
| 26 January 2017 | 13:30: Sigmoid colon tumour surgery performed uneventfully 14:51: Chest pain in the post-operative recovery room with electrocardiogram suggesting ST-elevation myocardial infarction accompanied by increased levels of cardiac enzymes. Treated with intravenous nitroglycerine, aspirin, clopidogrel, atorvastatin, and bisoprolol with good clinical response |
| 27 January 2017 | Transferred to a tertiary hospital for coronary angiography and specialized management. Transthoracic echocardiography showed akinesia of the mid-apical segments of the left ventricle with balloon-like dilatation and akinesia of the inferoseptal and inferior walls of the left ventricle and ejection fraction of 40% |
| 28 January 2017 | Coronary angiography did not identify any coronary artery lesions. A tentative diagnosis of Takotsubo cardiomyopathy (TCM) was suggested |
| 30 January 2017 | Cardiac magnetic resonance imaging (CMRI) confirmed the segmental contraction abnormalities seen in echocardiography with intense myocardial oedema on T2-weighted images without late hyperenhancement after intravenous gadolinium administration, confirming the diagnosis of TCM and ruling out acute ischaemic damage |
| 6 February 2017 | Patient left hospital free of symptoms |
| 3 April 2017 | CMRI follow-up revealed disappearance of the mid-apical contraction abnormality of the left ventricle, regression of the myocardial oedema, and normalization of global left ventricular systolic function |
Case presentation
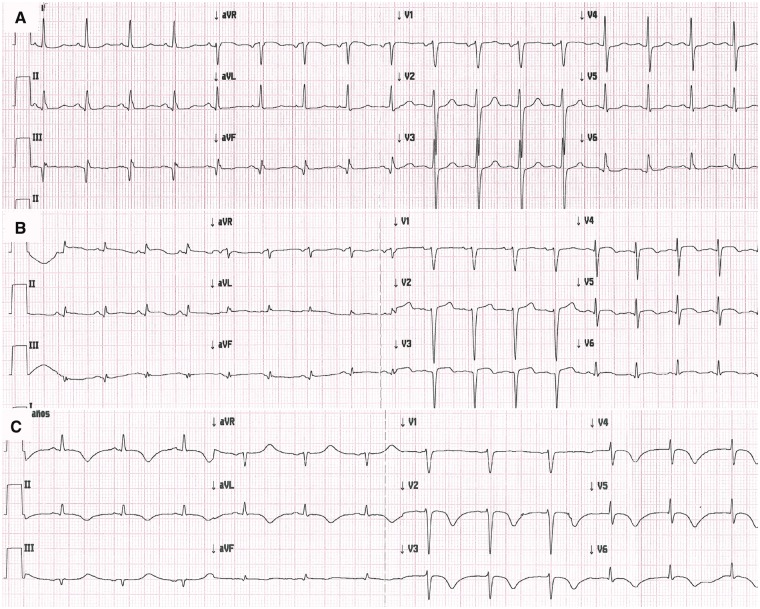
In January 2017, a 65-year-old woman with a history of essential hypertension and an old myocardial infarction was admitted to a local hospital for sigmoid colon tumour surgery. In 2012, she had suffered an inferior AMI, which was successfully treated with primary angioplasty for a critical proximal right coronary lesion with two overlapping drug-eluting stents. She remained asymptomatic under cardioprotective treatment. Soon after colon surgery, she developed angina that was accompanied by ST-segment elevation as shown by electrocardiography (Figure1B). She had blood pressure of 112/63 mmHg, heart rate of 108 b.p.m. and oxygen saturation of 98% on room air. On physical examination, she had regular cardiac rhythm with normal S1 and S2, with no murmurs appreciated and clear lungs. The operative wound was unremarkable. Cardiac enzymes were increased with a maximum troponin-I concentration of 657 ng/mL (upper normal limit <14 ng/mL), maximum total creatine phosphokinase (CPK) concentration of 450 U/L (upper normal limit <192 U/L), and maximum CKP mass concentration of 20.45 ng/mL (upper normal limit <3.61 ng/mL U/L). Post-operative haemoglobin was 12.3 g/dL. Based on a diagnosis of acute coronary syndrome, 500 mg of aspirin, 600 mg of clopidogrel, 80 mg of atorvastatin, 2.5 mg of bisoprolol, opioids and intravenous nitroglycerine were administered, and the patient had a good clinical response with disappearance of the chest pain and regression of the ST-segment elevation.
Figure 1.
(A) Twelve-lead preoperative electrocardiogram; (B) post-operative electrocardiogram during angina after colon surgery showing ST-segment elevation on inferior and anterolateral leads; (C) electrocardiogram tracing 2 days later shows prominent symmetric negative T waves and regression of the ST-segment elevation.
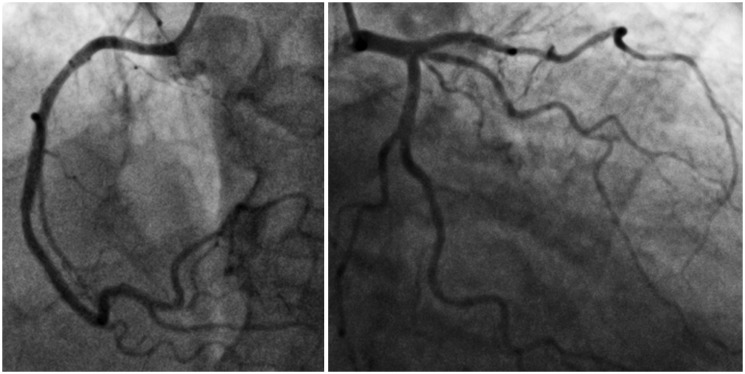
The following day, the patient was transferred to Clinica Reñaca, a tertiary hospital in Viña del Mar, Chile, for coronary angiography and specialized management. On admission to the intensive care unit, she was asymptomatic without signs of heart failure. Her brain natriuretic peptide concentration was elevated to a maximum of 1285 pg/mL (upper normal limit <286 pg/mL). Electrocardiography showed prominent symmetric negative T waves (Figure1C). Transthoracic echocardiography showed akinesis of the mid-apical segments of the LV with balloon-like dilatation and akinesis of the inferoseptal and inferior walls with impaired left ventricular systolic function, as shown by an ejection fraction of 40%. Coronary angiography did not identify any coronary artery lesions (Figure2), and a tentative diagnosis of TCM was suggested.
Figure 2.
Right coronary artery in the left cranial view (left) and left coronary artery in the caudal right oblique view (right), showing absence of coronary artery lesions.
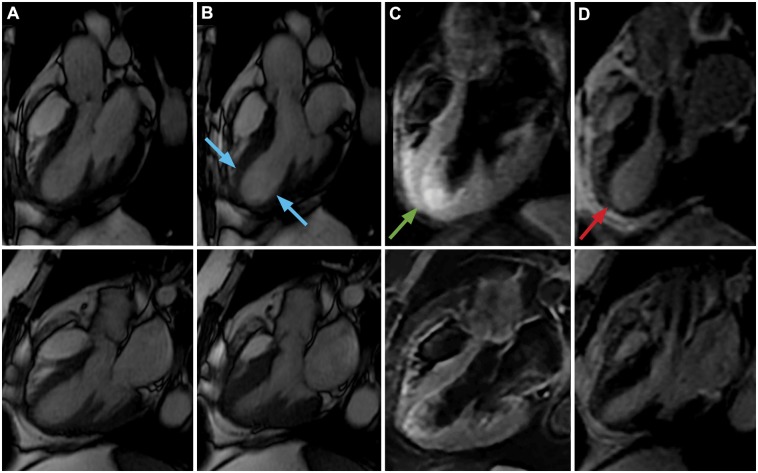
Cardiac magnetic resonance imaging on Day 3 confirmed the segmental contraction abnormalities seen by echocardiography (Figure3A and B, upper; Supplementary material online, Videos S1–S4). On T2-weighted short-time inversion recovery images, high signal intensity was present in middle and apical segments of the LV, which suggested the presence of myocardial oedema (Figure 3C, upper, Figure4, upper left and upper right, and Figure5, upper) without late hyperenhancement after intravenous gadolinium administration (Figure6, upper). However, late gadolinium enhancement was present in the inferoseptal and inferior walls of the LV, reflecting old myocardial scarring (Figure6, upper, red arrows; Supplementary material online, Video S4). These findings confirmed the diagnosis of TCM and ruled out acute ischaemic damage. Clopidogrel was stopped and enalapril 5 mg was started twice daily along with bisoprolol and aspirin 100 mg daily, and the patient was discharged when asymptomatic.
Figure 3.
Upper: Cine cardiac magnetic resonance imaging three-chamber view images at (A) end-diastole and (B) end-systole, showing akinesia in the mid-apical segments of the left ventricle (blue arrows), typical of apical ballooning Takotsubo cardiomyopathy (see also Supplementary material online, Video S1); (C) T2-weighted short-time inversion recovery three-chamber view showing transmural signal hyperintensity (myocardial oedema) in the mid-apical segments of the left ventricle (green arrow); (D) Late gadolinium enhancement excluded myocardial scarring (red arrow). Lower: At the 2-month follow-up, cine cardiac magnetic resonance imaging three-chamber view images at (A) end-diastole and (B) end-systole, showing disappearance of the anteroseptal and apical contraction abnormality and normalization of global left ventricular systolic function (see also Supplementary material online, Video S2); (C) T2-weighted short-time inversion recovery three-chamber view showing regression of the myocardial oedema; (D) Late gadolinium enhancement showing no changes.
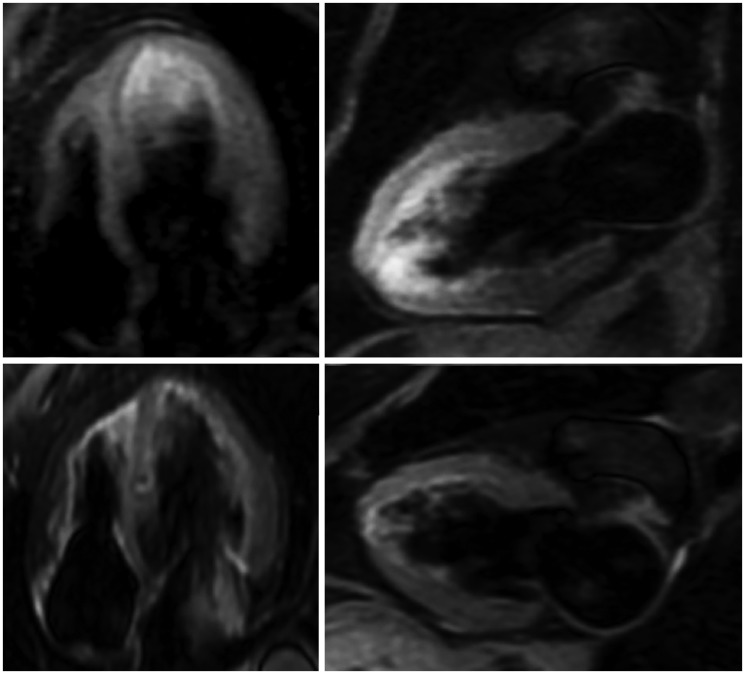
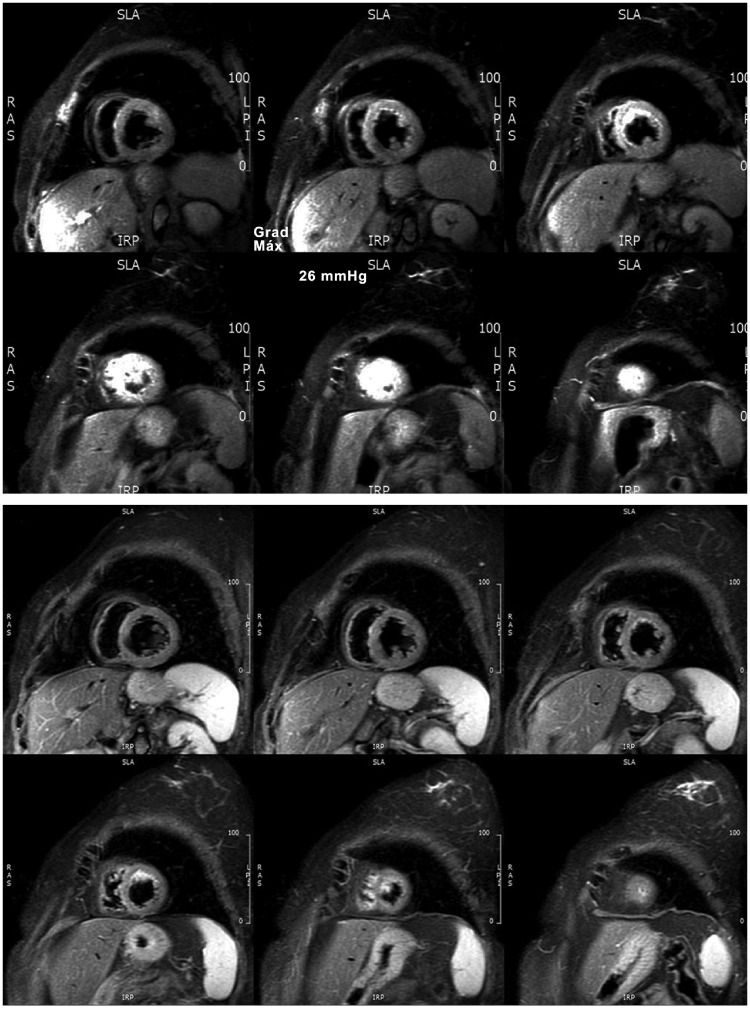
Figure 4.
Cardiac magnetic resonance imaging T2-weighted short-time inversion recovery four-chamber view images (Upper left) and two-chamber view images (Upper right) showing transmural signal hyperintensity (myocardial oedema) in the mid-apical segments of the left ventricle; short-time inversion recovery images at the 2-month follow-up show regression of myocardial oedema.
Figure 5.
Upper: Cardiac magnetic resonance imaging T2-weighted short-time inversion recovery short-axis-view images showing transmural signal hyperintensity (myocardial oedema) in the mid-apical segments of the left ventricle; Lower: short-time inversion recovery images at the 2-month follow-up show regression of myocardial oedema.
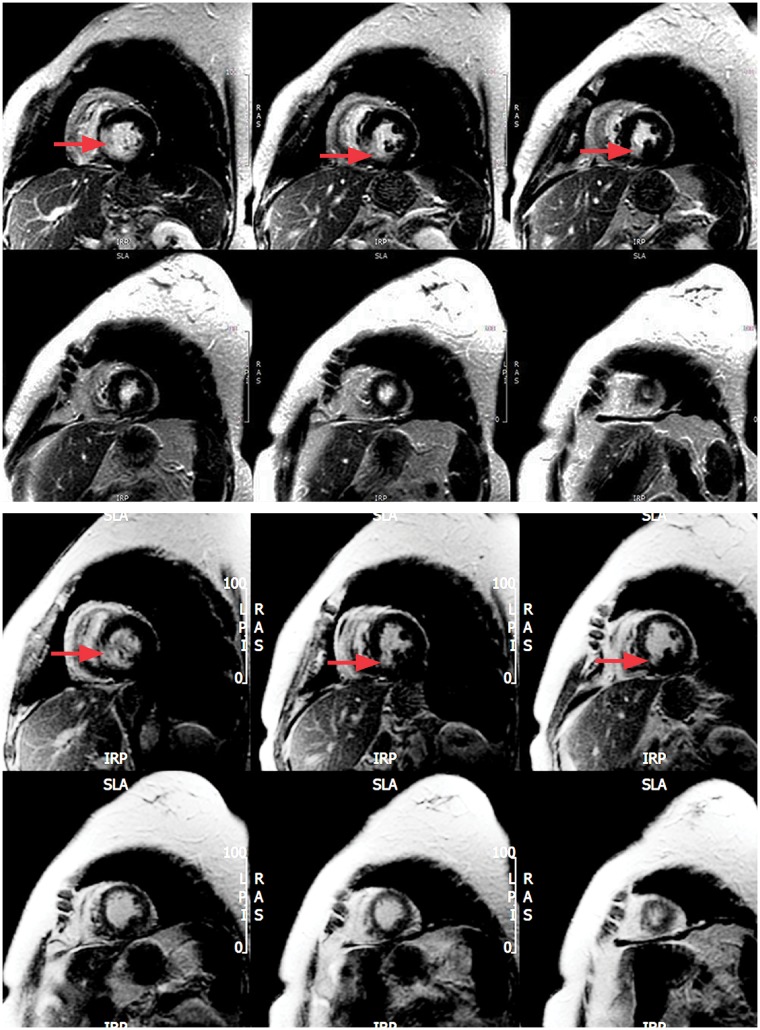
Figure 6.
Upper: Late gadolinium enhancement shows higher signal intensity in the inferoseptal and inferior walls of the left ventricle, which reflects old myocardial scarring (red arrows), but no hyperenhancement in the mid-apical segments; Lower: At the 2-month follow-up, no significant changes are seen (red arrows).
Cardiac magnetic resonance imaging at the 2-month follow-up revealed persistence of the left ventricular inferoseptal and inferior wall late gadolinium hyperenhancement (Figure6, lower, red arrows; Supplementary material online, Video S8), which reflected myocardial scarring caused by the AMI in 2012. Cardiac magnetic resonance imaging also revealed disappearance of the mid-apical contraction abnormality of the LV (Figure3A and B, lower, and Supplementary material online, Videos S5–S8), regression of the myocardial oedema (Figure3C, lower, Figure4, lower left, Figure4, lower right and Figure5, lower) and normalization of global left ventricular systolic function (Supplementary material online, Videos S5–S8).
Discussion
In patients with known coronary heart disease, making a differential diagnosis between TCM and AMI is essential because of the therapeutic implications and prognosis. In hospitalized patients with a suspected AMI, the finding of a normal coronary tree does not exclude an acute coronary event. In these patients, AMI can result from coronary vasospasm8,9 or a coronary embolism with spontaneous lysis of the clot.7,10 In patients with AMI, CMRI is a powerful diagnostic tool that enables the detection of oedema, necrosis, intramyocardial haemorrhage and microvascular obstruction,9,11 and the differentiation of AMI from other acute cardiomyopathies of non-ischaemic origin, such as myocarditis and TCM.2,12 In AMI, late enhancement has a subendocardial or transmural location, reflecting the vascular distribution of the affected myocardial territory,13 whereas in non-ischaemic pathology, its usual location is subepicardial or intramural,12–14 as in cases of acute myocarditis. The cause of this condition is unknown, but direct catecholamine-mediated myocardial stunning is the most likely hypothesis. Whereas coronary vasospasm might play a role, it is not observed in the majority of patients, and when present, it is not clear whether it represents a causal factor or is an epiphenomenon caused by elevated catecholamines.15
The diagnosis of TCM is based mainly on the diagnostic criteria proposed by the Mayo Clinic4 and recently by the European Society of Cardiology,16 which do not incorporate CMRI as an additional diagnostic criterion. However, about one-third of patients with suspected TCM can have an apical AMI, as defined using CMRI for the final diagnosis.8 The results of CMRI for differential diagnosis between these pathologies are relevant, especially in patients with a previous AMI, as in this case. In this scenario, CMRI can confirm the diagnosis of TCM and can identify the distribution of the regional wall motion abnormality, the presence of oedema, which reflects reversible myocardial damage, and the absence of fibrosis representing irreversible myocardial damage.9
Conclusion
This case study has confirmed that CMRI, a non-invasive diagnostic method, offers an accurate differential diagnosis between AMI and TCM in patients with an old myocardial infarction. CMRI should be incorporated as a diagnostic criterion for TCM.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1. Tsuchihashi K, Ueshima K, Uchida T, Oh-Mura N, Kimura K, Owa M, Yoshiyama M, Miyazaki S, Haze K, Ogawa H, Honda T, Hase M, Kai R, Morii I.. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J Am Coll Cardiol 2001;38:11–18. [DOI] [PubMed] [Google Scholar]
- 2. Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, Rihal CS.. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 2004;141:858–865. [DOI] [PubMed] [Google Scholar]
- 3. Dote K, Sato H, Tateishi H, Uchida T, Ishihara M.. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol 1991;21:2013–2014. [PubMed] [Google Scholar]
- 4. Prasad A, Lerman A, Rihal CS.. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J 2008;155:408–417. [DOI] [PubMed] [Google Scholar]
- 5. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E.. Apical ballooning syndrome or Takotsubo cardiomyoptahy: a systematic review. Eur Heart J 2006;27:1523–1529. [DOI] [PubMed] [Google Scholar]
- 6. Agarwal S, Bean MG, Hata JS, Castresana MR.. Perioperative takotsubo cardiomyopathy: a systematic review of published cases. Semin Cardiothorac Vasc Anesth 2017;21:277–290. [DOI] [PubMed] [Google Scholar]
- 7. Eitel I, Behrendt F, Schindler K, Kivelitz D, Gutberlet M, Schuler G, Thiele H.. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J 2008;29:2651–2659. [DOI] [PubMed] [Google Scholar]
- 8. Gandhi H, Rodriguez JE, Reynolds H.. Takotsubo Cardiomyopathy versus Apical Infarction in patients with Myocardial infarction and non-obstructive coronary artery disease (MINOCA). JACC 2017;69:270. [Google Scholar]
- 9. Perazzolo MM, Lima JA, Iliceto S.. MRI in acute myocardial infarction. Eur Heart J 2011;32:284–293. [DOI] [PubMed] [Google Scholar]
- 10. Niccoli G, Scalone G, Crea F.. Acute myocardial infarction with no obstructive coronary atherosclerosis: mechanisms and management. Eur Heart J 2015;36:475–481. [DOI] [PubMed] [Google Scholar]
- 11. Kidambi A, Plein S.. Risk stratification in acute myocardial infarction with multiparametric cardiac magnetic resonance imaging: getting to the core of the matter. Eur Heart J 2016;37:1060–1062. [DOI] [PubMed] [Google Scholar]
- 12. Monney PA, Sekhri N, Burchell T, Knight C, Davies C, Deaner A, Sheaf M, Baithun S, Petersen S, Wragg A, Jain A, Westwood M, Mills P, Mathur A, Mohiddin SA.. Acute myocarditis presenting as acute coronary syndrome: role of early cardiac magnetic resonance in its diagnosis. Heart 2011;97:1312–1318. [DOI] [PubMed] [Google Scholar]
- 13. Franco A, Javidi S, Ruehm SG.. Delayed myocardial enhancement in cardiac magnetic resonance imaging. J Radiol Case Rep 2015;9:6–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ.. Cardiovascular magnetic resonance assessment of non-ischemic cardiomyopathies. Eur Heart J 2005;26:1461–1474. [DOI] [PubMed] [Google Scholar]
- 15. Kato K, Lyon AR, Ghadri JR, Templin C.. Takotsubo syndrome: aetiology, presentation and treatment. Heart 2017;103:1461–1469. [DOI] [PubMed] [Google Scholar]
- 16. Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, Sheppard MN, Figtree GA, Parodi G, Akashi YJ, Ruschitzka F, Filippatos G, Mebazaa A, Omerovic E.. Current state of knowledge on Takotsubo syndrome: a position statement from the taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 2016;18:8–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.