Abstract
This cohort study explores the association between index hospitalization length of stay and hospital readmissions among children.
Hospital readmission rates are widely used as a quality measure for hospitalized patients. Hospital readmission gained attention largely from concerns about the quality of discharge care, including those patients discharged before they were adequately prepared to leave the hospital.1 In adult patients, shorter index hospitalization length of stay (LOS) is associated with a higher risk of hospital readmission for some conditions.2 This association has not been shown in children,3 and it remains unknown whether specific pediatric conditions might benefit from increasing LOS. Therefore, this study explored the association between index hospitalization LOS and pediatric readmissions by capitalizing on the natural variation in LOS across patients and hospitals.
Methods
This was a retrospective cohort study of hospitalized children (aged 0-18 years) using data from 2015 to 2016 from the Pediatric Health Information System database (Children’s Hospital Association), which includes clinical and billing data from 49 children’s hospitals, representing approximately 20% of all US discharges for children. This study was considered non–human subjects research by the institutional review board at Vanderbilt University Medical Center, Nashville, Tennessee, which waived the need for approval as well as patient informed consent. Reasons for condition-specific admissions were determined using the All-Patient Refined Diagnosis Related Groups (APR-DRGs) (version 32.0) classification scheme.4 Low frequency APR-DRGs (ie, APR-DRGs with <10 patients per year per hospital or APR-DRGs reported from <30 hospitals) were excluded. To ensure that patients within an APR-DRG had similar severity and complexity, discharges with high APR-DRG severity-of-illness levels (level 3 or 4), complex chronic conditions,5 intensive care unit services, or death were also excluded. To assess the association between index hospitalization LOS and readmissions, an ecological analysis was performed in which (1) the mean LOS (in bed-days) and associated 15-day and 30-day readmission rates for each APR-DRG were calculated; (2) the association between hospital-level adjusted mean LOS and hospital-level adjusted readmission rates using a linear regression model were estimated to identify which reasons for the index hospital admission had a statistically significant inverse association between LOS and readmission; and (3) the number of additional hospital bed-days and costs (estimated from charges using each hospital’s cost to charge ratio) required to prevent a single readmission were estimated. Statistical analyses were performed using SAS, version 9.4 (SAS Institute Inc), with a 2-sided P value less than .05 for significance.
Results
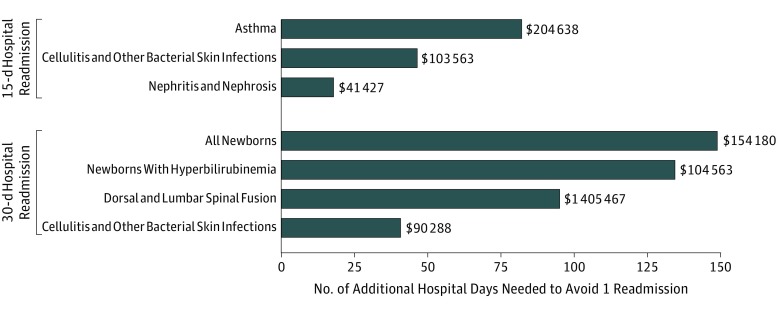
There were 956 507 pediatric hospitalizations included. Of 314 possible reasons for admission, only 6 distinct APR-DRGs for the index hospitalization (1.9%) had higher readmission rates with shorter hospital LOS. Of these 6 APR-DRGs, asthma, cellulitis and other bacterial skin infections, and nephritis and nephrosis had decreased 15-day readmissions and dorsal and lumbar spinal fusion (for scoliosis), cellulitis and other bacterial skin infections, all normal newborns, and the subset of newborns with hyperbilirubinemia had decreased 30-day readmissions (Table). To prevent a single readmission, the estimated number of additional hospital bed-days ranged from 18 days (for nephritis and nephrosis; 15-day readmission) to 148 days (for newborns; 30-day readmission). Accompanying costs for these additional hospital bed-days ranged from $41 000 (for nephritis and nephrosis) to $1.4 million (for dorsal and lumbar spinal fusion) (Figure). Among newborns, a longer hospital LOS for those with hyperbilirubinemia was associated with reduced readmissions; however, 134 additional hospital bed-days and $104 000 were required to prevent 1 readmission.
Table. LOS for Index Hospitalizations and Readmission Rates Among US Children.
| Reason for Index Hospitalization | No. of Children | Hospital Discharge Volume, Median (IQR)a | Index Hospitalization LOS, Median (IQR)b | Readmission Rate, Median (IQR), %b | Association Between LOS and Hospital Readmission | |
|---|---|---|---|---|---|---|
| β Coefficientc | P Value | |||||
| 15-d Unplanned Hospital Readmission | ||||||
| Asthma | 53 503 | 979 (604-1334) | 1.3 (1.2-1.4) | 1.6 (1.0-2.1) | −1.22 | .03 |
| Cellulitis and other bacterial skin infections | 24 992 | 468 (333-660) | 1.7 (1.5-1.8) | 2.3 (1.6-3.1) | −2.15 | .03 |
| Nephritis and nephrosis | 4107 | 80 (48-104) | 1.9 (1.6-2.2) | 9.3 (5.0-13.4) | −5.69 | .02 |
| 30-d Unplanned Hospital Readmission | ||||||
| Dorsal and lumbar spinal fusion | 3596 | 90 (34-128) | 3.5 (3.2-4.2) | 1.4 (0.1-2.8) | −1.06 | .03 |
| Cellulitis and other bacterial skin infections | 24 992 | 468 (333-660) | 1.6 (1.5-1.8) | 3.1 (2.1-4.3) | −2.47 | .03 |
| All newborns | 82 354 | 297 (182-640) | 2.0 (1.7-2.4) | 1.8 (0.1-3.0) | −0.67 | .04 |
| With hyperbilirubinemia | 22 999 | 200 (122-424) | 1.9 (1.6-2.5) | 3.2 (2.0-4.0) | −0.75 | .05 |
Abbreviations: APR-DRG, All-Patient Refined Diagnosis Related Group; IQR, interquartile range; LOS, length of stay.
Total hospital discharge volume of index hospital admissions for each APR-DRG shown.
Index hospitalization LOS and readmission rates were risk adjusted by the case-mix index (mean relative weight) for each APR-DRG.6
The β coefficient was the slope of the regression line for readmission rate vs adjusted LOS by hospital.
Figure. Aggregate Number of Additional Bed-Days Needed Across Index Hospitalizations to Avoid 1 Pediatric Hospital Readmission Among US Children.
After generating the model associating hospital-level adjusted mean length of stay (LOS) with adjusted readmission rate for each All Patient Refined Diagnosis Related Group (APR-DRG), β coefficients from the regression equation were used to estimate the number of additional bed-days needed to avoid 1 pediatric hospital readmission. The β coefficient provided an estimate for the change in the readmission rate for a 1-day increase in mean LOS. Thus, the change in the number of readmissions was estimated as follows: (No. of Observed Readmissions) − (Observed Readmission Rate + β) × No. of Cases. Then the number of days needed to avoid 1 readmission was estimated as follows: (No. of Additional Days)/(Change in the No. of Readmissions), where the number of additional days was equal to the number of cases because 1 day was added to the LOS of each case. Additional costs associated with additional hospital bed-days were determined by multiplying the number of days needed to avoid 1 readmission by the median cost per day for the APR-DRG. For example, for asthma, 81.8 additional days were required to prevent 1 readmission, with a cost per day of $2502 (or $204 638 for 81.8 additional bed-days).
Discussion
These findings do not suggest a robust association between index hospitalization LOS and hospital readmission among children. Few specific reasons for the index hospitalization admission had an inverse association between LOS and readmission. For those diagnoses, the number of additional hospital bed-days and costs needed to avoid 1 readmission may neither be reasonable nor cost-effective to pursue. Because the study findings are most applicable to children’s hospitals, future studies should assess the association between hospital LOS and readmission in other types of hospitals. In children’s hospitals, the majority of children may already be staying in the hospital for the appropriate amount of time. As a result, efforts to avoid readmissions should focus on other aspects of hospital discharge care.
References
- 1.Berry JG, Blaine K, Rogers J, et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955-962. doi: 10.1001/jamapediatrics.2014.891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sud M, Yu B, Wijeysundera HC, et al. Associations between short or long length of stay and 30-day readmission and mortality in hospitalized patients with heart failure. JACC Heart Fail. 2017;5(8):578-588. doi: 10.1016/j.jchf.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 3.Morse RB, Hall M, Fieldston ES, et al. Children’s hospitals with shorter lengths of stay do not have higher readmission rates. J Pediatr. 2013;163(4):1034-8.e1. doi: 10.1016/j.jpeds.2013.03.083 [DOI] [PubMed] [Google Scholar]
- 4.Averill RF, Goldfield NI, Muldoon J, Steinbeck BA, Grant TM. A closer look at All-Patient Refined DRGs. J AHIMA. 2002;73(1):46-50. [PubMed] [Google Scholar]
- 5.Feinstein JA, Russell S, DeWitt PE, Feudtner C, Dai D, Bennett TD. R Package for pediatric complex chronic condition classification. JAMA Pediatr. 2018;172(6):596-598. doi: 10.1001/jamapediatrics.2018.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richardson T, Rodean J, Harris JM, et al. Development of Hospitalization Resource Intensity Scores for Kids (H-RISK) and comparison across pediatric populations. J Hosp Med. 2018;13(9):602-608. [DOI] [PubMed] [Google Scholar]