Key Points
Question
Does postoperative use of scheduled intravenous acetaminophen (paracetamol), combined with intravenous propofol or dexmedetomidine, reduce the risk of postoperative delirium among older patients undergoing cardiac surgery?
Findings
In this randomized clinical trial that included 120 patients undergoing cardiac surgery, scheduled intravenous acetaminophen administered postoperatively for 48 hours, combined with intravenous propofol or dexmedetomidine as a sedative, significantly reduced in-hospital delirium compared with placebo (10% vs 28%, respectively).
Meaning
In older patients undergoing cardiac surgery, postoperative use of scheduled intravenous acetaminophen, combined with intravenous propofol or dexmedetomidine, may be considered to reduce the incidence of postoperative delirium, although additional research is needed.
Abstract
Importance
Postoperative delirium is common following cardiac surgery and may be affected by choice of analgesic and sedative.
Objective
To evaluate the effect of postoperative intravenous (IV) acetaminophen (paracetamol) vs placebo combined with IV propofol vs dexmedetomidine on postoperative delirium among older patients undergoing cardiac surgery.
Design, Setting, and Participants
Randomized, placebo-controlled, factorial clinical trial among 120 patients aged 60 years or older undergoing on-pump coronary artery bypass graft (CABG) surgery or combined CABG/valve surgeries at a US center. Enrollment was September 2015 to April 2018, with follow-up ending in April 2019.
Interventions
Patients were randomized to 1 of 4 groups receiving postoperative analgesia with IV acetaminophen or placebo every 6 hours for 48 hours and postoperative sedation with dexmedetomidine or propofol starting at chest closure and continued for up to 6 hours (acetaminophen and dexmedetomidine: n = 29; placebo and dexmedetomidine: n = 30; acetaminophen and propofol: n = 31; placebo and propofol: n = 30).
Main Outcomes and Measures
The primary outcome was incidence of postoperative in-hospital delirium by the Confusion Assessment Method. Secondary outcomes included delirium duration, cognitive decline, breakthrough analgesia within the first 48 hours, and ICU and hospital length of stay.
Results
Among 121 patients randomized (median age, 69 years; 19 women [15.8%]), 120 completed the trial. Patients treated with IV acetaminophen had a significant reduction in delirium (10% vs 28% placebo; difference, −18% [95% CI, −32% to −5%]; P = .01; HR, 2.8 [95% CI, 1.1-7.8]). Patients receiving dexmedetomidine vs propofol had no significant difference in delirium (17% vs 21%; difference, −4% [95% CI, −18% to 10%]; P = .54; HR, 0.8 [95% CI, 0.4-1.9]). There were significant differences favoring acetaminophen vs placebo for 3 prespecified secondary outcomes: delirium duration (median, 1 vs 2 days; difference, −1 [95% CI, −2 to 0]), ICU length of stay (median, 29.5 vs 46.7 hours; difference, −16.7 [95% CI, −20.3 to −0.8]), and breakthrough analgesia (median, 10 082.5 vs 12 609.0 µg morphine equivalents; difference, −2530 [95% CI, −5064 to −22]). For dexmedetomidine vs propofol, only breakthrough analgesia was significantly different (median, 10 110.0 vs 12 612.5 µg; difference, −2567 [95% CI, −5094 to −26]; P = .03). Fourteen patients in both the placebo-dexmedetomidine and acetaminophen-propofol groups (46% and 45%) and 7 in the acetaminophen-dexmedetomidine and placebo-propofol groups (24% and 23%) had hypotension.
Conclusions and Relevance
Among older patients undergoing cardiac surgery, postoperative scheduled IV acetaminophen, combined with IV propofol or dexmedetomidine, reduced in-hospital delirium vs placebo. Additional research, including comparison of IV vs oral acetaminophen and other potentially opioid-sparing analgesics, on the incidence of postoperative delirium is warranted.
Trial Registration
ClinicalTrials.gov Identifier: NCT02546765
This randomized clinical trial compares the effects of postoperative intravenous acetaminophen vs placebo, combined with intravenous propofol vs dexmedetomidine, on postoperative in-hospital delirium among older patients undergoing cardiac surgery.
Introduction
Delirium, characterized by an acute onset and fluctuating course of inattention and either disorganized thinking or an altered level of consciousness, is reported in 50% of cardiac surgical patients1 and is associated with increased length of intensive care unit (ICU) stay, morbidity, mortality, and long-term cognitive decline.2,3 Risk factors such as preexisting cognitive dysfunction, postoperative pain, use of opioids and sedatives, and surgical inflammation have been associated with delirium.2,4 Untreated pain from sternotomy, tube thoracostomy, and leg incision sites can induce delirium,5 but opioids may also increase this risk.6 Perioperative sedation and opioid-based analgesic regimens are potential risk factors for delirium that may be addressed with appropriate interventions.7
Nonsteroidal anti-inflammatory drugs and acetaminophen (paracetamol) are commonly used as adjuvant analgesics. Since nonsteroidal anti-inflammatory drugs are avoided after cardiac surgery because of bleeding and kidney injury risk, acetaminophen may be particularly useful in this setting. Intravenous (IV) acetaminophen administration may be advantageous compared with oral or rectal routes because of variability in bioavailability. In some settings, IV acetaminophen has been shown to reduce inflammation and may confer central analgesic properties8 and decrease opioid consumption in both opioid-naive and exposed patients.9 Despite these properties, IV acetaminophen has not been studied in the context of delirium prevention. Dexmedetomidine, a selective α2 receptor agonist, may have opioid-sparing effects10 with anti-inflammatory properties11; however, studies evaluating dexmedetomidine for prevention of delirium following cardiac surgery have shown mixed results.12,13,14
This study aimed to investigate the effect of IV acetaminophen vs placebo combined with IV dexmedetomidine or propofol on the incidence of postoperative delirium. It was hypothesized that postoperative IV acetaminophen for 48 hours as an adjuvant analgesic and dexmedetomidine as a sedative would reduce the incidence of in-hospital delirium following cardiac surgery.
Methods
Study Design
This randomized factorial trial was conducted at Beth Israel Deaconess Medical Center in Boston, Massachusetts, from September 2015 to April 2018. Institutional review board approval was obtained from the Committee on Clinical Investigations and all patients provided written informed consent. The study protocol has been previously published15 and is available in eAppendix 1 in Supplement 1.
Study Participants
Patients aged 60 years or older undergoing coronary artery bypass graft surgery with or without aortic and/or mitral valve replacement requiring cardiopulmonary bypass were eligible for trial inclusion. Patients with a preoperative left ventricular ejection fraction of less than 30%, preexisting cognitive impairment, Alzheimer disease, Parkinson disease, medications for cognitive decline, history of recent seizures, serum creatinine levels above 2 mg/dL, liver dysfunction, recent history of alcohol misuse, English-language limitations, and hypersensitivity to study medications and patients undergoing emergent surgery were excluded. Participants who did not speak English were excluded because of their inability to complete the cognitive assessments, which have been extensively validated in English.
Randomization and Blinding
Patients were allocated using computer-generated block randomization of size 8 with the help of a research pharmacy to either acetaminophen or placebo as an adjunct analgesic and to either dexmedetomidine or propofol as a sedative. This resulted in 4 combinations (1:1:1:1) of analgesics and sedatives, namely, acetaminophen and dexmedetomidine, acetaminophen and propofol, dexmedetomidine and placebo, or propofol and placebo. To achieve blinding to analgesia group among patients, care teams, and research staff assessing outcomes, 1 g of IV acetaminophen and placebo (0.9% saline) were distributed in equal-volume IV bags. Given the distinct appearance of propofol, there was no blinding to sedation group.
Study Interventions
Acetaminophen or placebo was administered within 1 hour of ICU admission and thereafter every 6 hours for 8 doses. Both groups received opioids and other analgesics according to standard care practices during these 48 hours; however, administering acetaminophen in any form outside the blinded study medication during this time was not allowed. Propofol or dexmedetomidine started during chest closure was continued for up to 6 hours postoperatively or until extubation, whichever occurred first. A fast-tracking pathway according to standard care practices was used in the ICU to enable early weaning, extubation, spirometry, early mobilization, and subsequent discharge from the ICU (eAppendix 2 in Supplement 1). The dexmedetomidine group received an IV bolus dose of 0.5 to 1 µg/kg during chest closure, followed by a maintenance infusion of 0.1 to 1.4 µg/kg per hour (eAppendix 2). The IV propofol group received a maintenance dose of 20 to 100 µg/kg per minute.
Study Outcomes
The primary outcome was the incidence of postoperative in-hospital delirium at any time during a patient’s hospital stay. Delirium was measured daily until discharge with the Confusion Assessment Method (CAM) or CAM-ICU for intubated patients. The CAM is a standardized tool used for identification of delirium through a diagnostic algorithm based on 4 cardinal features of delirium, namely acute onset and fluctuating course, inattention, disorganized thinking, and altered level of consciousness. Secondary outcomes included duration of delirium, postoperative cognition at discharge, 48-hour breakthrough analgesic requirements, and ICU and hospital lengths of stay. Additional postoperative analgesic requirements were measured as the amount of opioid (IV morphine or hydromorphone) and oral analgesics required for pain control. This was calculated as the sum of (fentanyl dose × 100) + (hydromorphone dose × 4) + morphine dose + (oxycodone dose × 1.5).16 For context, a morphine equivalent dose of 90 morphine equivalents a day would correspond to 90 mg of hydrocodone or roughly 60 mg of oxycodone. Hospital length of stay was defined as the number of days admitted in the hospital following surgery and ICU length of stay was defined as the number of hours admitted in the ICU prior to transfer to the general floor. Postoperative cognitive decline was assessed as a secondary outcome using the Montreal Cognitive Assessment (MoCA) (range, 0 [worst] to 30 [best]; minimally clinically important difference [MCID], 2 points)17 at baseline and discharge. Daily cognitive assessments were performed each day using a standard questionnaire comprising the Delirium Symptom Interview, a standard cognitive assessment consisting of tests of attention, orientation, and memory, and the CAM or CAM-ICU. Nonverbal (intubated) patients were administered the CAM-ICU, which includes both brief cognitive testing and the CAM algorithm to determine the presence or absence of delirium. Assessments were administered by study team members masked to treatment assignment and specifically trained in recognition and assessment of delirium and cognition. Post hoc analyses included delirium severity (CAM severity [CAM-S] score; range, 0 [best/no delirium] to 19 [worst]; MCID, 2 points),18 median time to ICU discharge among patients with and without delirium, and postoperative pain. All reported pain scores (11-point scale from 0 [no pain] to 10 [worst pain]; MCID, 2 points)19 were obtained from study participants by nursing staff blinded to the analgesic assignment and were entered into the medical record. The median and highest (worst) of these pain scores were recorded for analysis for each patient on each postoperative day.
The study protocol provides the schedules of enrollment, interventions, and assessments used in the trial.15 Additional details of the study protocol are documented in eAppendix 1 in Supplement 1. Results of the postdischarge follow-up and biomarker analyses are not included in this article.
Adverse Event Assessments
Hypotension was predefined as a systolic blood pressure less than 90 mm Hg for 5 minutes or more. Bradycardia was defined as any heart rate less than 40/min. Adverse event data were collected from patients’ medical records daily for a maximum of 10 days. In a post hoc analysis, the difference between groups in the lowest documented blood pressures was assessed.
Sample Size
A sample size of 58 patients was needed for each group, acetaminophen and placebo, to detect a 50% reduction in delirium incidence from a baseline delirium incidence of 50% using 2-sided α = .05 and 80% power. The expected effect size in the primary outcome was based on a pilot study conducted at Beth Israel Deaconess Medical Center.20 Previous studies have shown that reductions in the incidence of delirium exceeding at least one-third of the baseline rate are considered clinically meaningful; therefore, this study would be powered to detect a clinically meaningful difference.21 A sample size of 120 patients who received the intervention was targeted to account for potential patient withdrawals. At the time of conception, this study was also interested in the effect of sedation type on the incidence of in-hospital delirium. Hence, the inclusion of this second factor was preplanned. It was therefore included in the factorial design to allow for generation of hypotheses with sedation techniques; however, the trial was powered only to detect differences between those who did and did not receive acetaminophen.
Statistical Analysis
Research Electronic Data Capture (REDCap) was used for data collection and included information on analgesics and sedatives, opioid dosage during the first 48 hours postoperatively, pain scores, patient delirium and cognition assessment data, adverse events, and demographic data. The primary analysis included all patients who were randomized and received at least 1 dose of the study medication. Patients who withdrew after receiving a study medication were still included in the analysis. Daily assessments of delirium were completed until the time of withdrawal. Data were abstracted from the medical record to assess secondary end points in patients who withdrew. Data are presented as means and standard deviations, medians and interquartile ranges (IQRs), or frequencies and proportions depending on variable type and distribution. Changes between groups are further presented as differences and 95% confidence intervals. The Shapiro-Wilk test was used to assess normality. Continuous data were assessed between groups using a parametric t test, Wilcoxon rank sum test, or Kruskal-Wallis test as appropriate. Differences in categorical variables, including the primary outcome (in-hospital delirium), were assessed with a χ2 test (or a 2-tailed Fisher exact test when cell counts were small). Missing data were uncommon in the data set (<6%); therefore, no imputation was performed. Interrater reliability assessments of delirium, reported as percent agreement, κ, and weighted κ, were performed both for presence of delirium and for key features including acute change, inattention, disorganized thinking, and altered level of consciousness.
The primary analysis focused on the relationship between the primary outcome, in-hospital delirium, and acetaminophen use. Given the factorial design of the study, an analysis was performed to determine whether an interaction was observed between groups. In this analysis, a regression model was created with in-hospital delirium as the outcome variable, including an interaction term between the sedative and analgesic groups. Prespecified secondary analyses were performed for outcomes in the factorial design, with 4 groups representing each of the acetaminophen and sedative combinations as well as for the relationship between sedative groups comparing patients who received dexmedetomidine with those who received propofol. No adjustment was performed for multiple testing; therefore, all results for secondary analyses should be interpreted as exploratory.
In post hoc analyses, Kaplan-Meier curves and a Cox proportional hazards model were used to compare time to experiencing delirium after confirming that the proportional hazards assumption was met. To test whether the proportional hazards were met, a time-varying covariate with group was included in the model (P = .56). Given the factorial design, this approach was replicated in models for all 4 factorial groups as well as for the pairwise comparisons (dexmedetomidine vs propofol and acetaminophen vs placebo) to ensure that this assumption was valid. No violations of this assumption were detected; therefore, no time-varying covariates were retained in the final model. Repeated-measures analyses including generalized estimating equations with robust variance were used to assess for differences in the median and worst daily pain scores between groups using mixed-model regression. SAS version 9.4 (SAS Institute Inc) was used for all analyses, with 2-sided P<.05 considered statistically significant. Full details of the statistical analysis plan are available in eAppendix 1 in Supplement 1.
Results
Study Population
A total of 140 patients provided informed consent and were enrolled, of whom 121 were randomized and a total of 120 received the study intervention and were subsequently analyzed (Figure 1). Patients were excluded from the study if they had an active history of drug or alcohol use disorder (96/268 [36%]), serum creatinine higher than 2 mg/dL (58/268 [22%]), preoperative left ventricular ejection fraction less than 30% (50/268 [19%]), liver dysfunction (28/268 [10%]), lack of English-language proficiency (22/268 [8%]), preexisting cognitive impairment (17/268 [6%]), seizures in the last 3 months (9/268 [3%]), emergent procedure (7/268 [3%]), hypersensitivity to study drugs or procedures (8/268 [3%]), Alzheimer disease (3/268 [1%]), prophylactic medications for cognitive decline (2/268 [0.7%]), or isolated aortic surgery (1/268 [0.4%]). Overall, the majority of enrolled participants were male (101/120 [84%]), were white (111/120 [93%]), and had a median age of 69 (IQR, 63-76) years. Isolated coronary artery bypass grafting was the most frequent cardiac procedure (79/120 [66%]), followed by coronary artery bypass grafting with an aortic valve replacement (32/120 [27%]). The baseline characteristics of the 4 factorial groups were similar (Table 1). Baseline functional status was similar among groups, with the majority of participants living independently and having a high school degree or higher (110/120 and 113/120, respectively) (eTable 1 in Supplement 2).
Figure 1. Participant Flow in the DEXACET Randomized Clinical Trial.
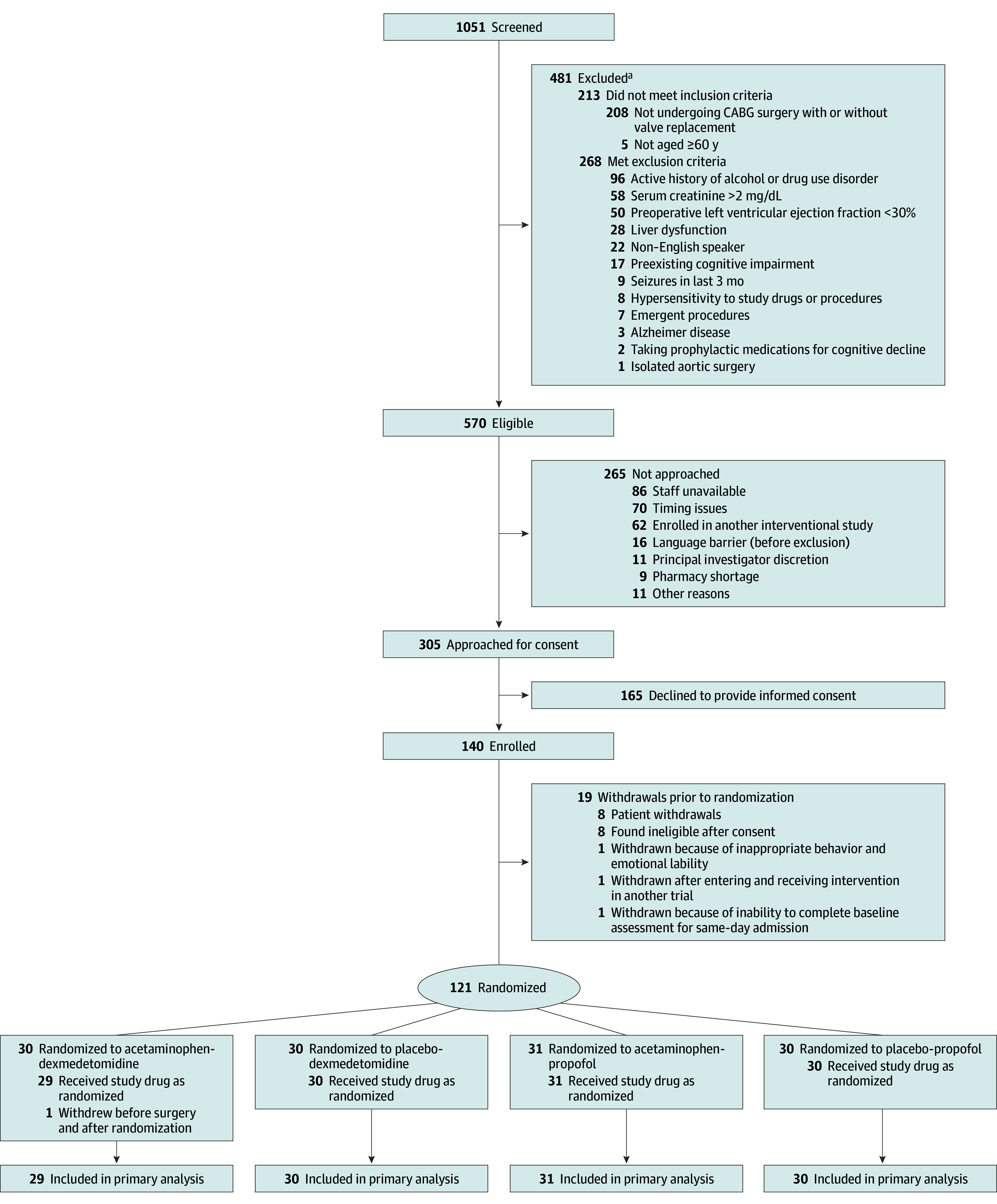
CABG indicates coronary artery bypass graft. To convert creatinine values to micromoles per liter, multiply by 88.4.
aNumbers of participants who did not meet inclusion or exclusion criteria are nonexclusive.
Table 1. Baseline Characteristics of Study Participants by Treatment Group.
| Characteristics | Acetaminophen-Dexmedetomidine (n = 29) | Placebo-Dexmedetomidine (n = 30) | Acetaminophen-Propofol (n = 31) | Placebo-Propofol (n = 30) |
|---|---|---|---|---|
| Demographics | ||||
| Sex, No. (%) | ||||
| Male | 26 (89.7) | 25 (83.3) | 24 (77.4) | 26 (86.7) |
| Female | 3 (10.3) | 5 (16.7) | 7 (22.6) | 4 (13.3) |
| Age, median (IQR), y | 64 (63-72) | 69 (63-74) | 70 (66-75) | 71 (64-79) |
| Patient-reported race, No. (%)a | ||||
| White | 26 (89.7) | 28 (93.3) | 29 (93.6) | 28 (93.3) |
| Black/African American | 2 (6.9) | 1 (3.3) | 1 (3.2) | 1 (3.3) |
| Asian | 0 | 0 | 1 (3.2) | 0 |
| Multiracial | 0 | 0 | 0 | 1 (3.3) |
| Other | 0 | 1 (3.3) | 0 | 0 |
| Unknown/not specified | 1 (3.5) | 0 | 0 | 0 |
| Hispanic or Latino, No. (%) | 1 (3.5) | 1 (3.3) | 0 | 2 (6.7) |
| Weight, median (IQR), kg | 89.1 (80.4-102.0) |
87.6 (82.0-102.0) |
84.1 (79.0-93.2) |
90.0 (75.8-107.0) |
| Height, median (IQR), cm | 173.0 (167.6-180.3) |
172.7 (167.6-178.0) |
170.2 (167.6-173.3) |
175.1 (167.6-180.0) |
| Body mass index, median (IQR)b | 29.7 (26.6-32.3) |
29.4 (27.0-32.0) |
28.5 (26.6-32.3) |
29.2 (25.9-34.3) |
| Surgical characteristics | ||||
| Procedure, No. (%) | ||||
| Isolated CABG surgery | 19 (65.5) | 18 (60.0) | 19 (61.3) | 23 (76.7) |
| CABG surgery + mitral valve replacement | 1 (3.5) | 0 | 1 (3.2) | 0 |
| CABG surgery + aortic valve replacement | 8 (27.6) | 8 (26.7) | 10 (32.3) | 6 (20.0) |
| Otherc | 1 (3.5) | 4 (13.3) | 1 (3.2) | 1 (3.3) |
| No. of arteries affected, median (IQR) | 3 (2-4) | 3 (2-3) | 3 (2-3) | 3 (2-3) |
| Preoperative statin use, No. (%) | 24 (82.8) | 25 (83.3) | 29 (93.6) | 27 (90.0) |
| Cross-clamp time, median (IQR), min | 67 (58-84) | 73 (60-93) | 78 (66-87) | 64 (54-96) |
Abbreviations: CABG, coronary artery bypass graft; IQR, interquartile range.
Race was documented using patient-reported values from predetermined fixed categories.
Calculated as weight in kilograms divided by height in meters squared.
Other includes CABG surgery plus maze procedure, CABG surgery plus ascending aorta replacement, and CABG surgery plus pulmonary vein isolation with or without valve replacement.
Study Drug Administration
Two patients in the dexmedetomidine group received propofol and 2 patients in the propofol group received dexmedetomidine in the first 6 hours. Five participants (2 in the placebo group and 3 in the acetaminophen group) missed 1 dose and 1 placebo participant received 1 additional dose of placebo. Four participants randomized to acetaminophen and 1 participant randomized to placebo received additional IV, oral, or rectal acetaminophen during the study period. Despite these results, all analyses were performed using data from all randomized patients who received at least 1 of the 4 study medications.
In-Hospital Delirium
When conducting the analysis of the factorial groups, no significant interaction was observed between the sedation and analgesic groups (P = .62). Results of the main effects were therefore analyzed and are presented separately. Patients assigned to acetaminophen had a significantly lower incidence of in-hospital delirium, the primary outcome, compared with patients assigned to placebo (10% vs 28%; difference, −18%; 95% CI, −32% to −5%; P = .01) (Table 2). In contrast, no significant difference was observed in the incidence of delirium (17% vs 21%; difference, −4%; 95% CI, −18% to 10%; hazard ratio, 0.8; 95% CI, 0.4-1.9; P = .54) between those who did and did not receive dexmedetomidine. Agreement was 100% and κ and weighted κ were 1.00 for all CAM variables collected.
Table 2. Primary and Secondary Outcomes.
| Outcomes | Analgesic | Sedative | ||||||
|---|---|---|---|---|---|---|---|---|
| Acetaminophen (n = 60) | Placebo (n = 60) | Difference (95% CI) | P Value | Dexmedetomidine (n = 59) | Propofol (n = 61) | Difference (95% CI) | P Value | |
| Delirium | ||||||||
| In-hospital delirium (primary outcome), No. (%) | 6 (10.00) | 17 (28.33) | −18.3% (−32.0% to −4.6%) | .01 | 10 (16.95) | 13 (21.31) | −4% (−18% to 10%) | .54 |
| Days with delirium, median (IQR) | 1.0 (1.0 to 1.0) | 2.0 (1.0 to 3.0) | −1 (−2 to 0) | .03 | 1.0 (1.0 to 2.0) | 2.0 (1.0 to 3.0) | −1 (−2 to 0) | .31 |
| Worst delirium severity, median (IQR)a | 9.0 (7.0 to 11.0) | 8.0 (6.0 to 11.0) | 1.0 (−2.0 to 3.0) | .81 | 6.5 (6.0 to 11.0) | 9.0 (8.0 to 11.0) | −2.5 (−3.0 to 2.0) | .39 |
| MoCA scoreb | ||||||||
| Baseline, median (IQR) | 24.0 (22.0 to 26.0) |
23.5 (20.4 to 26.0) |
0.5 (−1 to 2) |
.39 | 24.0 (21.0 to 26.0) |
24.0 (21.0 to 26.0) |
0 (−1 to 1) |
.84 |
| Discharge, median (IQR) | 24.0 (21.0 to 26.0) |
24.0 (20.0 to 26.0) |
0 (−1 to 2) |
.29 | 24.0 (21.0 to 25.0) |
24.0 (21.0 to 26.0) |
0 (−2 to 1) |
.55 |
| Change from baseline, median (IQR) | 0.0 (−2.0 to 1.0) |
−0.4 (−2.0 to 1.0) |
0.4 (−1.0 to 1.0) |
.82 | 0.0 (−1.6 to 1.0) |
−0.9 (−2.0 to 1.2) |
0.9 (−1.0 to 1.0) |
.82 |
| Time-related outcomes | ||||||||
| Hospital length of stay, median (IQR), d | 8.0 (6.0 to 9.5) | 8.5 (6.0 to 11.0) | −0.5 (−2 to 0) | .13 | 8.0 (6.0 to 10.0) | 8.0 (6.0 to 11.0) | 0 (−1 to 1) | .71 |
| ICU length of stay, median (IQR), h | 29.46 (25.07 to 49.43) |
46.17 (27.83 to 81.44) |
−16.7 (−20.3 to −0.8) |
.02 | 31.98 (27.42 to 54.27) |
29.70 (25.65 to 56.55) |
2.3 (−3.2 to 5.0) |
.66 |
| 48-h Postoperative medication administration | ||||||||
| Total morphine equivalent administered, median (IQR), µgc | 10 082.5 (7524.0 to 15 090.0) |
12 609.0 (10 076.0 to 20 141.5) |
−2530 (−5064 to −22) |
.03 | 10 110.0 (5113.0 to 15 075.0) |
12 612.5 (10 052.5 to 20 067.5) |
−2567 (−5094 to 26) |
.03 |
Abbreviations: ICU, intensive care unit; IQR, interquartile range; MoCA, Montreal Cognitive Assessment.
Post hoc outcome. Worst delirium severity was based on the highest postoperative Confusion Assessment Method severity score, in which patients are assigned values from 0 (best) to 19 (worst).
The MoCA is scored on a scale from 0 (worst) to 30 (best). A MoCA score of 24 is equivalent to a Mini–Mental State Examination score of about 27 or 28. Depending on education and peak intellectual attainment, such a score could be consistent with either being cognitively normal or having very early mild cognitive impairment. Such a person would be capable of living independently in the community and managing most or all of their affairs.
Total morphine equivalent is calculated as the sum of (fentanyl dose × 100) + (hydromorphone dose × 4) + morphine dose + (oxycodone dose × 1.5).
Comparison of Acetaminophen vs Placebo
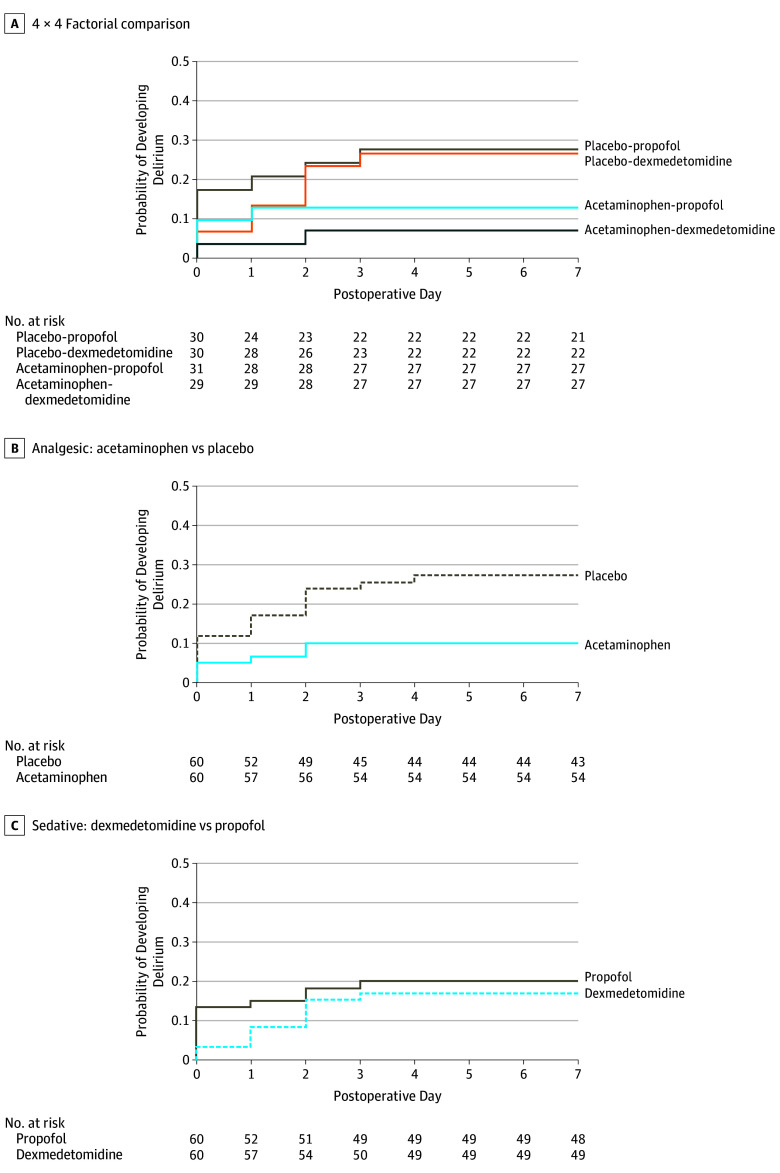
Patients who received acetaminophen experienced a shorter duration of delirium compared with placebo (median, 1 vs 2 days; difference, −1 day; 95% CI, −2 to 0 days; P = .03) (Table 2). Postoperative cognition, as assessed via the median discharge MoCA score, was not significantly different between the 2 groups (median, 24.0 vs 24.0 points; difference, 0 points; 95% CI, −1.0 to 2.0 points; P = .29). Intensive care unit length of stay was significantly different in patients who received acetaminophen (29.5 vs 46.2 hours; difference, −16.7 hours; 95% CI, −20.3 to −0.8 hours; P = .02). There was no significant difference in the median hospital stay between those who did and did not receive acetaminophen (median, 8.0 vs 8.5 days; difference, −0.5 days; 95% CI, −2 to 0 days; P = .13). The acetaminophen groups received a lower opioid dose in the first 48 hours postoperatively compared with the placebo groups (median, 10 082.5 vs 12 609.0 µg; difference, −2530 µg; 95% CI, −5064 to −22 µg; P = .03) (eFigure 1 in Supplement 2). Total doses of each sedative administered are shown in eFigure 2 in Supplement 2. Although pain scores were reduced over time in post hoc analyses, no statistically significant difference was observed between those who did and did not receive acetaminophen for either worst (P = .44) or median (P = .21) pain scores (Figure 2). In post hoc analyses, the worst delirium severity (CAM-S) score was not significantly different between those who did and did not receive acetaminophen (median, 9.0 vs 8.0 points; difference, 1.0 point; 95% CI, −2.0 to 3.0 points; P = .81); however, time to delirium onset was significantly different between those in the acetaminophen and placebo groups (hazard ratio, 2.8; 95% CI, 1.1-7.8) (Figure 3). Furthermore, in a post hoc analysis of ICU length of stay, the median time to ICU discharge was significantly higher in patients who experienced delirium as opposed to those who did not (median, 52.4 [IQR, 29.7-123.6] hours vs 29.2 [IQR, 25.7-51.7] hours, respectively; P = .01).
Figure 2. Post Hoc Pain Scores Stratified by Study Group.

Median and worst daily pain scores are reported on a scale from 0 (best) to 10 (worst). Top and bottom of boxes indicate interquartile ranges; center lines indicate medians. Tukey error bars are shown, which extend to the farthest points that are not outliers. Outliers (black circles) were defined as values greater than 1.5 times the interquartile range.
Figure 3. Post Hoc Kaplan-Meier Analysis for Time to Delirium.
Patients in the acetaminophen-dexmedetomidine, placebo-dexmedetomidine, acetaminophen-propofol, and placebo-propofol groups were assessed for delirium on a median of 4 (interquartile range [IQR], 4-4) days, 4 (IQR, 4-5) days, 4 (IQR, 4-5) days, and 4 (IQR, 4-5) days, respectively.
Comparison of Dexmedetomidine vs Propofol
When stratified by sedation group, duration of delirium, compared between those who did and did not receive dexmedetomidine, was not statistically significantly different (median, 1.0 vs 2.0 days; difference, −1 day; 95% CI, −2 to 0 days; P = .31) (Table 2). The median MoCA score at discharge was not statistically different between those who did and did not receive dexmedetomidine (median, 24.0 vs 24.0 points; difference, 0.9 points; 95% CI, −1.0 to 1.0 points; P = .55). Median lengths of stay in both the ICU (median, 32.0 vs 29.7 hours; difference, 2.3 hours; 95% CI, −3.2 to 5.0 hours; P = .66) and the hospital (median, 8.0 vs 8.0 days; difference, 0 days; 95% CI, −1 to 1 day; P = .71) were not significantly different between the dexmedetomidine and propofol groups. Patients who received propofol had larger total morphine equivalent doses given in the first 48 hours postoperatively compared with patients who received dexmedetomidine (median, 10 110.0 vs 12 612.5 µg; difference, −2567 µg; 95% CI, −5094 to −26 µg; P = .03). In post hoc analyses, worst and median pain scores were not statistically different between sedative groups (P = .39 and P = .13, respectively) (Figure 2). In post hoc analyses, the severity of delirium (median CAM-S score, 6.5 vs 9.0 points; difference, −2.5 points; 95% CI, −3.0 to 2.0 points; P = .39) was not statistically different between groups.
Comparison of All 4 Randomization Groups
In a prespecified exploratory analysis of differences across all 4 groups, there was no statistically significant difference in the incidence of in-hospital delirium (P = .07) (Table 3). Specifically, in a logistic regression model including all 4 groups with placebo-propofol as the reference category, the acetaminophen-propofol group and the placebo-dexmedetomidine group showed no statistically significant difference in the odds of developing in-hospital delirium (odds ratios, 0.35 [95% CI, 0.09-1.28] and 0.85 [95% CI, 0.28-2.61], respectively). However, a statistically significant difference was observed in the acetaminophen-dexmedetomidine group (odds ratio, 0.17; 95% CI, 0.03-0.87). These and other results for secondary end points showed effect sizes consistent with those observed in the primary analysis.
Table 3. Secondary Outcomes Stratified by Factorial Groupa.
| Outcomes | Acetaminophen-Dexmedetomidine (n = 29) | Placebo-Dexmedetomidine (n = 30) | Acetaminophen-Propofol (n = 31) | Propofol-Placebo (n = 30) | P Value |
|---|---|---|---|---|---|
| Delirium | |||||
| In-hospital delirium, No. (%) | 2 (6.9) | 8 (26.7) | 4 (12.9) | 9 (30.0) | .07 |
| Days with delirium, median (IQR) | 1 (1 to 1) | 1 (1 to 3) | 1 (1 to 1) | 3 (2 to 3) | .047 |
| Worst delirium severity, median (IQR)b | 10 (9 to 11) | 6 (6 to 9) | 8 (6 to 10) | 9 (8 to 11) | .35 |
| MoCA scorec | |||||
| Baseline, median (IQR) | 23 (22 to 26) | 24 (20 to 26) | 24 (22 to 26) | 23 (21 to 26) | .85 |
| Discharge, median (IQR) | 24 (21 to 25) | 24 (20 to 26) | 25 (22 to 27) | 24 (21 to 25) | .49 |
| Change from baseline, median (IQR) | 0.0 (−1.1 to 1.0) | 0.0 (−1.8 to 1.3) | 0.5 (−2.5 to 2.0) | −1.0 (−2.0 to 1.0) | .93 |
| Time-related outcomes | |||||
| Hospital length of stay, median (IQR), d | 8 (6 to 9) | 9 (7 to 11) | 8 (6 to 11) | 8 (6 to 11) | .37 |
| ICU length of stay, median (IQR), h | 28.8 (24.9 to 43.5) |
49.1 (29.0 to 92.9) |
30.3 (25.3 to 52.8) |
29.3 (25.7 to 74.3) |
.02 |
| 48-h Postoperative medication administration | |||||
| Total morphine equivalent administered, median (IQR), µgd | 10 050 (5094 to 12 530) | 11 382 (10 032 to 18 840) | 12 611 (10 026 to 17 639) | 12 616 (10 116 to 22 590) | .02 |
Abbreviations: ICU, intensive care unit; IQR, interquartile range; MoCA, Montreal Cognitive Assessment.
Differences were assessed between groups using a χ2 test for categorical variables and a Kruskal-Wallis test for continuous variables.
Post hoc outcome. Worst delirium severity was based on the highest postoperative Confusion Assessment Method severity score, in which patients are assigned values from 0 (best) to 19 (worst).
The MoCA is scored on a scale from 0 (worst) to 30 (best).
Total morphine equivalent is calculated as the sum of (fentanyl dose × 100) + (hydromorphone dose × 4) + morphine dose + (oxycodone dose × 1.5).
Adverse Events
Clinical outcomes and adverse events were not significantly different when stratified by randomization group (eTable 2 in Supplement 2). Fourteen patients each in the placebo-dexmedetomidine and acetaminophen-propofol groups (46% and 45%, respectively) and 7 patients each in the acetaminophen-dexmedetomidine and placebo-propofol groups (24% and 23%, respectively) experienced at least 1 episode of hypotension postoperatively. One patient (3%) in the placebo-dexmedetomidine group and 1 patient (3%) in the acetaminophen-propofol group experienced postoperative bradycardia. In a post hoc analysis, although roughly one-third of patients met the prespecified threshold for hypotension (systolic blood pressure <90 mm Hg for >5 minutes), the median of their lowest documented systolic blood pressure measurements was 83 (IQR, 79-86) mm Hg, which did not differ by group (P = .74).
Discussion
In this randomized trial, patients who received scheduled IV acetaminophen analgesia in the first 48 hours postoperatively demonstrated a decreased in-hospital incidence of delirium compared with placebo. Additionally, delirium duration, ICU length of stay, and opioid and/or opioid equivalent use in the immediate postoperative period were lower in participants randomized to receive acetaminophen. In sedation analyses, although opioid use was significantly lower in the dexmedetomidine groups compared with the propofol groups, there was no statistically significant difference in delirium or length of stay. To our knowledge, this study is the first to show a significant and meaningful reduction of delirium with use of IV acetaminophen in patients undergoing cardiac surgery.
Mamoun et al22 previously assessed use of IV acetaminophen every 6 hours for 24 hours following cardiac surgery, in which reduced pain intensity was demonstrated without a reduction in opioid consumption. The key differences between the study by Mamoun et al and the present study are intervention and opioid assessment duration (48 hours in this study), use of patient-controlled analgesia by Mamoun et al vs nurse-driven postoperative analgesia in the present study, and inclusion of patients aged 18 years or older by Mamoun et al vs older patients in this study. It is possible that age-related23 opioid-sparing effects could also partially explain the reduction in opioid consumption seen in this study. Several investigations have shown that IV acetaminophen may have better analgesic efficacy than oral acetaminophen and differing effects on opioid consumption.23,24,25,26 Reduced opioid consumption6 may partially explain the mechanism behind the reduction in the incidence of delirium seen in the present study.
The finding of a decreased ICU length of stay in patients receiving IV acetaminophen was similar to the results from a meta-analysis in which critically ill patients with delirium had a 1-day longer mean length of ICU stay than those without delirium.27 Furthermore, increased inspiratory lung capacity24 and better pain relief with patient satisfaction23 favor a shorter ICU stay, both of which could potentially be achieved more effectively with a successful opioid-sparing technique. These positive benefits need further exploration in larger clinical trials, both in the setting of enhanced recovery after cardiac surgery as well as in the face of the current opioid epidemic.
Although dexmedetomidine reduced opioid use in bariatric surgical patients,10,28,29 its role in reducing postoperative delirium following cardiac surgery has yielded contradictory results.12,13,30,31 In this study, although a decrease in opioid consumption in the first 48 hours postoperatively was observed, no statistically significant trend was observed in delirium incidence, severity, or duration. In addition, no interaction was found between dexmedetomidine and acetaminophen in reducing delirium incidence. Further studies in a larger cohort are needed to truly elucidate the effect of dexmedetomidine on aspects of delirium and cognition.
Limitations
This study has several limitations. First, although powered to detect a difference in postoperative delirium between those who did and did not receive acetaminophen, the sample size was relatively small and the incidence of delirium was lower in this study compared with the pilot study used to perform the power calculation. It is therefore possible that the large effect size observed may not be replicated in larger trials. It is also possible that group interactions could be limited by the sample size, specifically the interaction between IV acetaminophen and dexmedetomidine. Given the small sample size, inferences should be interpreted with caution. Second, anesthetic management was left to the discretion of treating anesthesiologists. This may have affected the outcome given the potential differing effects of anesthetic drugs on the development of postoperative delirium. However, practice variability in perioperative care was minimized with a protocolized cardiac surgical environment and preservation of randomization would be expected to minimize confounding from any anesthetic practice differences. Third, it was not possible to blind the sedative (propofol or dexmedetomidine) to the study team. However, the primary outcome was based on blinded, placebo-controlled exposure to IV acetaminophen. Fourth, it is possible that during daily delirium assessments, some periods of acute-onset inattention, disorganized thinking, or altered level of consciousness may have been missed, potentially leading to misclassification of these outcomes. Despite this, routine testing once per day is an accepted method of diagnosing delirium.32 Fifth, the postoperative analgesic regimen was nursing driven (standard of care) even though patient-controlled analgesia would have been ideal, although randomization and the triple-blind design would have mitigated this. Sixth, the limited sample size from a single center and restrictive inclusion may place some limitations on generalizability. Specifically, non–English-speaking participants were excluded because of their inability to complete the cognitive assessments. The resulting cohort was predominantly white and male. It is possible that the findings observed may not be generalizable to other institutions or to people of other racial and ethnic backgrounds. As this was a single-center study, the results should be replicated in a larger multicenter trial.
Conclusions
Among older patients undergoing cardiac surgery, postoperative scheduled IV acetaminophen, combined with IV propofol or dexmedetomidine, significantly reduced the incidence of in-hospital delirium compared with placebo. Additional research, including comparison of IV vs oral acetaminophen and other potentially opioid-sparing analgesics on the incidence of postoperative delirium, is warranted.
eAppendix 1. Study Protocol and Statistical Analysis Plan
eAppendix 2. Fast Track Protocol and Intravenous Drug Administration Guidelines
eFigure 1. Morphine Equivalents Stratified by Study Group
eFigure 2. Total Sedative Dose Stratified by Study Group
eTable 1. Baseline Function
eTable 2. Clinical Outcomes by Treatment Group
Data Sharing Statement
Section Editor: Derek C. Angus, MD, MPH, Associate Editor, JAMA (angusdc@upmc.edu).
References
- 1.Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112(5):1202-1211. doi: 10.1213/ANE.0b013e3182147f6d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-922. doi: 10.1016/S0140-6736(13)60688-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1):30-39. doi: 10.1056/NEJMoa1112923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown CH. Delirium in the cardiac surgical ICU. Curr Opin Anaesthesiol. 2014;27(2):117-122. doi: 10.1097/ACO.0000000000000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrison RS, Magaziner J, Gilbert M, et al. Relationship between pain and opioid analgesics on the development of delirium following hip fracture. J Gerontol A Biol Sci Med Sci. 2003;58(1):76-81. doi: 10.1093/gerona/58.1.M76 [DOI] [PubMed] [Google Scholar]
- 6.Gallagher R. Opioid-induced neurotoxicity. Can Fam Physician. 2007;53(3):426-427. [PMC free article] [PubMed] [Google Scholar]
- 7.Santos FS, Velasco IT, Fráguas R Jr. Risk factors for delirium in the elderly after coronary artery bypass graft surgery. Int Psychogeriatr. 2004;16(2):175-193. doi: 10.1017/S1041610204000365 [DOI] [PubMed] [Google Scholar]
- 8.Graham GG, Scott KF. Mechanism of action of paracetamol. Am J Ther. 2005;12(1):46-55. doi: 10.1097/00045391-200501000-00008 [DOI] [PubMed] [Google Scholar]
- 9.O’Neal JB. The utility of intravenous acetaminophen in the perioperative period. Front Public Health. 2013;1:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song J, Ji Q, Sun Q, Gao T, Liu K, Li L. The opioid-sparing effect of intraoperative dexmedetomidine infusion after craniotomy. J Neurosurg Anesthesiol. 2016;28(1):14-20. doi: 10.1097/ANA.0000000000000190 [DOI] [PubMed] [Google Scholar]
- 11.Li B, Li Y, Tian S, et al. Anti-inflammatory effects of perioperative dexmedetomidine administered as an adjunct to general anesthesia: a meta-analysis. Sci Rep. 2015;5:12342. doi: 10.1038/srep12342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X, Yang J, Nie XL, et al. Impact of dexmedetomidine on the incidence of delirium in elderly patients after cardiac surgery: a randomized controlled trial. PLoS One. 2017;12(2):e0170757. doi: 10.1371/journal.pone.0170757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deiner S, Luo X, Lin HM, et al. ; Dexlirium Writing Group . Intraoperative infusion of dexmedetomidine for prevention of postoperative delirium and cognitive dysfunction in elderly patients undergoing major elective noncardiac surgery: a randomized clinical trial. JAMA Surg. 2017;152(8):e171505. doi: 10.1001/jamasurg.2017.1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Su X, Meng ZT, Wu XH, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10054):1893-1902. doi: 10.1016/S0140-6736(16)30580-3 [DOI] [PubMed] [Google Scholar]
- 15.Shankar P, Mueller A, Packiasabapathy S, et al. Dexmedetomidine and intravenous acetaminophen for the prevention of postoperative delirium following cardiac surgery (DEXACET trial): protocol for a prospective randomized controlled trial. Trials. 2018;19(1):326. doi: 10.1186/s13063-018-2718-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alcántara Montero A, Sánchez Carnerero CI, Ibor Vidal PJ, Alonso Verdugo A. CDC guidelines for prescribing opioids for chronic pain [in Spanish]. Semergen. 2017;43(4):e53-e54. [DOI] [PubMed] [Google Scholar]
- 17.Wong GKC, Mak JSY, Wong A, et al. Minimum clinically important difference of Montreal Cognitive Assessment in aneurysmal subarachnoid hemorrhage patients. J Clin Neurosci. 2017;46:41-44. doi: 10.1016/j.jocn.2017.08.039 [DOI] [PubMed] [Google Scholar]
- 18.Vasunilashorn SM, Fong TG, Albuquerque A, et al. Delirium severity post-surgery and its relationship with long-term cognitive decline in a cohort of patients without dementia. J Alzheimers Dis. 2018;61(1):347-358. doi: 10.3233/JAD-170288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Myles PS, Myles DB, Galagher W, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. 2017;118(3):424-429. doi: 10.1093/bja/aew466 [DOI] [PubMed] [Google Scholar]
- 20.Susheela AT, Packiasabapathy S, Gasangwa DV, et al. The use of dexmedetomidine and intravenous acetaminophen for the prevention of postoperative delirium in cardiac surgery patients over 60 years of age: a pilot study. F1000Res. 2017;6:1842. doi: 10.12688/f1000research.12552.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340(9):669-676. doi: 10.1056/NEJM199903043400901 [DOI] [PubMed] [Google Scholar]
- 22.Mamoun NF, Lin P, Zimmerman NM, et al. Intravenous acetaminophen analgesia after cardiac surgery: a randomized, blinded, controlled superiority trial. J Thorac Cardiovasc Surg. 2016;152(3):881-889.e1. doi: 10.1016/j.jtcvs.2016.04.078 [DOI] [PubMed] [Google Scholar]
- 23.Jelacic S, Bollag L, Bowdle A, Rivat C, Cain KC, Richebe P. Intravenous acetaminophen as an adjunct analgesic in cardiac surgery reduces opioid consumption but not opioid-related adverse effects: a randomized controlled trial. J Cardiothorac Vasc Anesth. 2016;30(4):997-1004. doi: 10.1053/j.jvca.2016.02.010 [DOI] [PubMed] [Google Scholar]
- 24.Eremenko AA, Kuslieva EV. Analgesic and opioid-sparing effects of intravenous paracetamol in the early period after aortocoronary bypass surgery [in Russian]. Anesteziol Reanimatol. 2008;(5):11-14. [PubMed] [Google Scholar]
- 25.Pettersson PH, Jakobsson J, Owall A. Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. J Cardiothorac Vasc Anesth. 2005;19(3):306-309. doi: 10.1053/j.jvca.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 26.Macario A, Royal MA. A literature review of randomized clinical trials of intravenous acetaminophen (paracetamol) for acute postoperative pain. Pain Pract. 2011;11(3):290-296. doi: 10.1111/j.1533-2500.2010.00426.x [DOI] [PubMed] [Google Scholar]
- 27.Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ. 2015;350:h2538. doi: 10.1136/bmj.h2538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vaughns JD, Martin C, Nelson J, Nadler E, Quezado ZM. Dexmedetomidine as an adjuvant for perioperative pain management in adolescents undergoing bariatric surgery: an observational cohort study. J Pediatr Surg. 2017;52(11):1787-1790. doi: 10.1016/j.jpedsurg.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 29.Tufanogullari B, White PF, Peixoto MP, et al. Dexmedetomidine infusion during laparoscopic bariatric surgery: the effect on recovery outcome variables. Anesth Analg. 2008;106(6):1741-1748. doi: 10.1213/ane.0b013e318172c47c [DOI] [PubMed] [Google Scholar]
- 30.Djaiani G, Silverton N, Fedorko L, et al. Dexmedetomidine versus propofol sedation reduces delirium after cardiac surgery: a randomized controlled trial. Anesthesiology. 2016;124(2):362-368. doi: 10.1097/ALN.0000000000000951 [DOI] [PubMed] [Google Scholar]
- 31.Dasta JF, Jacobi J, Sesti AM, McLaughlin TP. Addition of dexmedetomidine to standard sedation regimens after cardiac surgery: an outcomes analysis. Pharmacotherapy. 2006;26(6):798-805. doi: 10.1592/phco.26.6.798 [DOI] [PubMed] [Google Scholar]
- 32.Evered L, Silbert B, Knopman DS, et al. ; Nomenclature Consensus Working Group . Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery—2018. Br J Anaesth. 2018;121(5):1005-1012. doi: 10.1016/j.bja.2017.11.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Study Protocol and Statistical Analysis Plan
eAppendix 2. Fast Track Protocol and Intravenous Drug Administration Guidelines
eFigure 1. Morphine Equivalents Stratified by Study Group
eFigure 2. Total Sedative Dose Stratified by Study Group
eTable 1. Baseline Function
eTable 2. Clinical Outcomes by Treatment Group
Data Sharing Statement