Key Points
Question
Is the presence of high levels of coronary artery calcification in the setting of very high levels of physical activity, for example, as typically practiced by masters marathon runners, associated with increased mortality?
Findings
In this observational study of 21 758 men with varying levels of physical activity, the presence of elevated levels of coronary artery calcification (≥100 Agatston units) was more prevalent among highly active men. However, no increase in all-cause or cardiovascular disease mortality was evident in this group when compared with men who were less active.
Meaning
In highly active individuals with elevated levels of coronary artery calcification, it appears that there is no evidence to suggest increased mortality risk from high levels of physical activity.
This observational study assesses the association of high levels of physical activity, prevalent coronary artery calcification, and subsequent mortality risk among patients from a preventive medicine clinic with varying levels of physical activity.
Abstract
Importance
Few data are available to guide clinical recommendations for individuals with high levels of physical activity in the presence of clinically significant coronary artery calcification (CAC).
Objective
To assess the association among high levels of physical activity, prevalent CAC, and subsequent mortality risk.
Design, Setting, and Participants
The Cooper Center Longitudinal Study is a prospective observational study of patients from the Cooper Clinic, a preventive medicine facility. The present study included participants seen from January 13, 1998, through December 30, 2013, with mortality follow-up through December 31, 2014. A total of 21 758 generally healthy men without prevalent cardiovascular disease (CVD) were included if they reported their physical activity level and underwent CAC scanning. Data were analyzed from September 26, 2017, through May 2, 2018.
Exposures
Self-reported physical activity was categorized into at least 3000 (n = 1561), 1500 to 2999 (n = 3750), and less than 1500 (n = 16 447) metabolic equivalent of task (MET)–minutes/week (min/wk). The CAC scores were categorized into at least 100 (n = 5314) and less than 100 (n = 16 444) Agatston units (AU).
Main Outcomes and Measures
All-cause and CVD mortality collected from the National Death Index Plus.
Results
Among the 21 758 male participants, baseline mean (SD) age was 51.7 (8.4) years. Men with at least 3000 MET-min/wk were more likely to have prevalent CAC of at least 100 AU (relative risk, 1.11; 95% CI, 1.03-1.20) compared with those accumulating less physical activity. In the group with physical activity of at least 3000 MET-min/wk and CAC of at least 100 AU, mean (SD) CAC level was 807 (1120) AU. After a mean (SD) follow-up of 10.4 (4.3) years, 759 all-cause and 180 CVD deaths occurred, including 40 all-cause and 10 CVD deaths among those with physical activity of at least 3000 MET-min/wk. Men with CAC of less than 100 AU and physical activity of at least 3000 MET-min/wk were about half as likely to die compared with men with less than 1500 MET-min/wk (hazard ratio [HR], 0.52; 95% CI, 0.29-0.91). In the group with CAC of at least 100 AU, men with at least 3000 MET-min/wk did not have a significant increase in all-cause mortality (HR, 0.77; 95% CI, 0.52-1.15) when compared with men with physical activity of less than 1500 MET-min/wk. In the least active men, those with CAC of at least 100 AU were twice as likely to die of CVD compared with those with CAC of less than 100 AU (HR, 1.93; 95% CI, 1.34-2.78).
Conclusions and Relevance
This study suggests there is evidence that high levels of physical activity (≥3000 MET-min/wk) are associated with prevalent CAC but are not associated with increased all-cause or CVD mortality after a decade of follow-up, even in the presence of clinically significant CAC levels.
Introduction
The health benefits of regular physical activity are well known, including decreased all-cause mortality, fatal and nonfatal cardiovascular disease (CVD) events, and sudden cardiac death.1 However, the adverse effects of high levels of endurance activity (well beyond current physical activity guidelines for health promotion)2 on the development of subclinical coronary artery atherosclerosis have been the focus of recent publications. In a study evaluating 152 masters athletes and 92 controls with low atherosclerotic risk profiles, a small percentage of male athletes (12 of 106 [11.3%]) had coronary artery calcification (CAC) of at least 300 Agatston units (AU), whereas no male controls had similar CAC levels.3 Whether these data are sufficiently robust to support the conclusion that “coronary plaques are more abundant in athletes”3(p126) is controversial.4 Another study evaluating 284 active men5 showed that those with the highest volume of physical activity (>2000 metabolic equivalent of task [MET]–minutes/week [min/wk]) had a higher prevalence of CAC. In these studies,3,4,5 the dominant plaque morphologic feature (calcified, noncalcified, or mixed) in the most active group was more likely to be calcified plaques, suggesting that these plaques might be more stable and less prone to rupture. These and similar observational studies6,7,8,9,10,11 with small numbers of highly select individuals have demonstrated conflicting results related to subclinical atherosclerosis prevalence. Importantly, primary clinical outcomes are unavailable for these studies, making their clinical implications uncertain.6,7,8,9,10,11
Few published reports present mortality outcomes in individuals with high levels of endurance activity in the presence of clinically significant CAC and thus, few data are available to guide clinical recommendations.6,7,12 If endurance athletes with higher amounts of CAC demonstrate increased mortality, then consideration should be given to reducing physical activity levels closer to those of the guidelines. Conversely, if the presence of CAC in athletes is not associated with increased mortality, then reassurance regarding high levels of physical activity would be more appropriate.
The objectives of this work were 2-fold: first, to assess the cross-sectional association of prevalent CAC with high levels of physical activity in a large population of generally healthy men, and second, to evaluate whether high levels of physical activity were associated with increased mortality in those with CAC because whether the mild increase in CAC seen in endurance athletes translates to greater mortality remains unknown. Ultimately, the overarching goal of these analyses is to provide clarity for health care professionals and patients regarding the risk of high levels of physical activity in the presence of subclinical atherosclerosis.
Methods
Study Population
The Cooper Clinic, Dallas, Texas, is a preventive medicine practice begun in 1970 that focuses on lifestyle modification for optimal health. This model has motivated endurance athletes and those with considerable routine moderate to vigorous physical activity to seek care at the clinic. In general, the patient population is white and educated and has access to medical care. The Cooper Center Longitudinal Study (CCLS) is a prospective study initiated to evaluate the association between cardiorespiratory fitness (CRF), physical activity, and health. Data collected at the Cooper Clinic and captured in the CCLS database are not based on a systematic research protocol but rather on clinical practices and patient-specific physician recommendations. Clinic patients sign informed consent for the use of their deidentified clinical data for research. The study is approved annually by the institutional review board of The Cooper Institute.
For this study, individuals with an evaluation including history of physical activity and CAC scanning were identified as the base cohort (28 880 men seen from January 13, 1998, through December 30, 2013, with follow-up completed on December 31, 2014). Exclusion criteria for the primary cohort included being younger than 40 years or older than 80 years (n = 2828), follow-up of less than 1 year from scan visit (n = 3144), preexisting myocardial infarction (n = 316) or stroke (n = 112); missing body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) or measurements of blood pressure, glucose levels, triglyceride levels, and high density lipoprotein (HDL) cholesterol levels (n = 704); or a BMI of less than 18.5 (n = 18). These exclusions resulted in a final sample of 21 758 men. A subcohort of 18 564 men underwent treadmill exercise testing to determine CRF for corroboration with self-reported physical activity.
Women were excluded from the primary assessment owing to insufficient number of deaths, which is the primary outcome of interest. Of note, 9501 women remained after the exclusion criteria were applied. In this cohort, only 5 all-cause and 3 CVD deaths occurred in the highly active group of women (≥3000 MET-min/wk). However, because this question is important in men and women, the characteristics, CAC prevalence, and mortality tables for women are included as eTables 1 to 3 and the eFigure in the Supplement.
Clinical Status
The baseline examination included a thorough history questionnaire with medical and physical activity questions confirmed by the clinic physician. Prescription medications, including statins, were captured from the physician report. Dietary history was not routinely obtained and, hence, not considered in this analysis. Weight in kilograms and height in meters were measured using a standard clinical scale and stadiometer. Body mass index was then calculated and reported using the measured weight and height.2 Seated resting blood pressure was acquired using a mercury sphygmomanometer following a standard protocol and reported in millimeters of mercury. After a 12-hour fast, venous blood samples were collected and the Cooper Clinic laboratory assayed blood chemistry analytes according to standard procedures and reported in appropriate units.
Cardiorespiratory fitness was objectively measured based on maximal time on an exercise treadmill test using the modified Balke protocol as previously described.13,14 Treadmill time using this protocol is known to be highly correlated with measured maximal oxygen uptake in men (r = 0.92).15 Maximal MET levels (1 MET = 3.5 mL/O2 × kg−1 × min−1) were estimated from the final treadmill speed and grade.16
Physical Activity
The detailed, self-reported physical activity questionnaire was reviewed with the patient for accuracy. Patients are asked to define their participation in the following activities, including number of sessions per week (frequency) and mean duration of each workout during the preceding 3 months: walking, jogging or running, treadmill, bicycling, stationary cycle, swimming, aerobic dance or floor exercise, and vigorous activity. Frequency and duration were converted to minutes of activity per week, weighted by multiplying by an estimated MET value using the Compendium of Physical Activity values for intensity assessment17 and summed across all activities to total physical activity in MET-min/wk. This process provides a volume of weekly physical activity for each individual. No specific question defined whether these exercisers are in fact competitive athletes (eg, regular marathon runners). However, an activity level greater than 3000 MET-min/wk is substantially above the guidelines and corresponds to more than 5 hour/week of vigorous exercise, or approximately 48 kilometer/week at a pace 10 minutes per 1.6 kilometer.
Physical activity levels were categorized into the following 3 groups: at least 3000 or more, 1500 to 2999, and less than 1500 MET-min/wk. The Physical Activity Guidelines2 identify the need for at least 150 minutes/week (min/wk), or 500 MET-min/wk, of moderate to vigorous physical activity for health and at least 300 min/wk, or 1000 MET-min/wk, for enhanced health and performance benefits. To focus the evaluation on high activity volumes, at least 3000 MET-min/wk was considered the highest activity category. The remainder were divided as 1500 to 2999 MET-min/wk and less than 1500 MET-min/wk. The latter was selected as the lower threshold based on the distribution of physical activity in this sample (75.6% were at the level of <1500 MET-min/wk) and to ensure substantial volume of activity in the groups above that threshold (ie, >150 min/wk of vigorous physical activity at an intensity of 10 MET).
Coronary Artery Calcification
Coronary artery calcification as assessed by electron beam tomography scan using the C-150XP or C-300 system (GE Imatron) from 1998 through 2007. Three-millimeter thick slices were obtained with 2-mm table increments during a breath-holding protocol. The methods for determining the Agatston calcium score have been reported.18 Coronary artery calcification quantification in this cohort is highly reproducible and free of bias.19 From 2008 to 2013, a 64-section scanner (Lightspeed VCT; GE Healthcare) was used. For the primary analysis, CAC was characterized dichotomously as less than 100 AU vs at least 100 AU to create lower- and higher-risk categories.20 In addition, CAC of 0 vs CAC of greater than 0 and CAC of less than 400 and CAC of at least 400 were evaluated.
Mortality
Mortal events, including the specific cause of death, were ascertained through 2014 using National Death Index Plus. Cardiovascular death was classified with International Classification of Diseases, 9th Revision, (deaths through 1999), codes 390 to 449, or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (deaths after 1999), codes I00 to I99. Follow-up times of participants who were still living at the end of 2014 were right censored.
Statistical Analysis
Data were analyzed from September 26, 2017, through May 2, 2018. Baseline characteristics were summarized by physical activity (<1500, 1500-2999, or ≥3000 MET-min/wk) and CAC (<100 or ≥100 AU) categories. Follow-up time and numbers of all-cause and CVD deaths were summarized in the same categories. Relative risk of CAC of at least 100 AU for physical activity of less than 1500 and 1500 to 2999 vs at least 3000 MET-min/wk adjusted for age, smoking, BMI, glucose level, cholesterol level, and resting systolic blood pressure was estimated using Poisson regression with robust error variance.21 Maximum likelihood was used to estimate hazard ratios (HRs) for all-cause and CVD mortality from Gompertz mortality models, assuming event rates exponentially increasing with age. Mortality model fit was confirmed by testing the Cox-Snell residuals against a censored exponential distribution. The proportional hazards assumptions were tested using Fisher z transformation of the correlation between the Schoenfeld residuals and the rank-ordered event times. Cubic regression splines were used to fit mortality models with continuous physical activity effects. Post hoc power was calculated from exemplary data generated by applying the fitted mortality models to the actual data. The sample had at least 80% power to detect all-cause mortality HRs of greater than 1.60 for physical activity of at least 3000 vs less than 1500 MET-min/wk separately in those with CAC of less than 100 or at least 100 AU. The corresponding minimum detectable CVD mortality HRs were 2.50 and 2.00. All analyses were programmed in SAS/STAT software (version 9.4; SAS Institute Inc).
Results
Descriptive characteristics are presented in Table 1 by physical activity and CAC level categories. In this sample of 21 758 men, the mean (SD) age at baseline examination was 51.7 (8.4) years, and most did not use tobacco (86.0%) or a statin medication (82.8%). Men in the most highly active category (>3000 MET-min/wk) were slightly older, were less likely to smoke, had lower BMI and blood glucose and triglyceride levels, and had higher HDL cholesterol levels. The mean physical activity volume in the most highly active group was slightly more than 4600 MET-min/wk, which is equivalent to running 6 miles/day at a pace of 10 minutes per mile (9.6 kilometers/day at a pace of 10 minutes per 1.6 kilometers). This exercise volume is consistent with the weekly distances proposed for and practiced by many masters marathon runners.22 The lifetime activity in years increased with increasing physical activity category. Coronary artery calcification score, lesion number, and total volume demonstrated no significant trend across physical activity groups within groups with CAC of at least 100 and less than 100 AU.
Table 1. Baseline Characteristics of 21 758 Generally Healthy Men by Physical Activity Level and CAC Categoriesa.
| Characteristic | Physical Activity Category, MET-min/wk | All Men (N = 21 758) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CAC <100 AU | CAC ≥100 AU | ||||||||
| <1500 (n = 12 413) | 1500-2999 (n = 2902) | ≥3000 (n = 1129) | P Value for Trend | <1500 (n = 4034) | 1500-2999 (n = 848) | ≥3000 (n = 432) | P Value for Trend | ||
| Age, mean (SD), y | 49.5 (7.1) | 49.2 (7.0) | 50.0 (7.2) | .97 | 58.7 (8.5) | 57.9 (8.2) | 58.9 (8.5) | .10 | 51.7 (8.4) |
| White, No. (%) | 11 196 (90.2) | 2616 (90.1) | 1021 (90.4) | .07 | 3681 (91.2) | 775 (91.4) | 390 (90.3) | .07 | 19 679 (90.4) |
| Current smoker, No. (%) | 1874 (15.1) | 306 (10.5) | 136 (12.0) | <.001 | 583 (14.5) | 98 (11.6) | 47 (10.9) | <.001 | 3044 (14.0) |
| Statin use, No. (%) | 1590 (12.8) | 302 (10.4) | 131 (11.6) | <.001 | 1346 (33.4) | 287 (33.8) | 114 (26.4) | .046 | 3770 (17.3) |
| BMI, mean (SD) | 28.1 (4.2) | 27.2 (3.5) | 27.1 (3.6) | <.001 | 28.7 (4.4) | 27.5 (3.8) | 27.1 (3.7) | <.001 | 28.0 (4.1) |
| Systolic blood pressure, mean (SD), mm Hg | 123.4 (13.3) | 122.7 (13.0) | 123.2 (13.3) | .01 | 129.5 (16.1) | 128.4 (15.0) | 129.8 (16.3) | .49 | 124.8 (14.2) |
| Glucose level, mean (SD), mg/dL | 99.8 (19.1) | 97.3 (14.1) | 98.0 (30.3) | <.001 | 104.9 (23.4) | 102.3 (19.7) | 100.5 (21.7) | <.001 | 100.4 (20.3) |
| Cholesterol level, mean (SD), mg/dL | 199.3 (36.6) | 196.4 (35.2) | 195.2 (34.5) | <.001 | 195.5 (40.7) | 193.1 (36.2) | 195.6 (39.0) | .55 | 197.7 (37.2) |
| LDL cholesterol level, mean (SD), mg/dL | 123.9 (32.1) | 121.2 (30.8) | 119.7 (30.6) | <.001 | 119.1 (35.4) | 117.4 (32.5) | 119.3 (35.0) | .53 | 122.1 (32.6) |
| HDL cholesterol level, mean (SD), mg/dL | 48.1 (12.2) | 51.8 (13.2) | 53.4 (13.7) | <.001 | 48.2 (12.9) | 52.1 (13.9) | 52.7 (13.7) | <.001 | 49.1 (12.8) |
| Triglyceride level, mean (SD), mg/dL | 140.2 (103.1) | 119.3 (87.1) | 113.2 (79.5) | <.001 | 146.0 (117.4) | 120.9 (81.0) | 119.4 (76.9) | <.001 | 135.9 (102.2) |
| Calcium level, mean (SD), mg/dL | 9.2 (0.4) | 9.2 (0.4) | 9.2 (0.4) | .046 | 9.2 (0.4) | 9.2 (0.4) | 9.2 (0.4) | .04 | 9.2 (0.4) |
| Framingham Risk Score, mean (SD), % | 8.7 (5.4) | 7.4 (4.7) | 7.6 (4.8) | <.001 | 13.5 (8.0) | 11.5 (6.9) | 12.3 (7.4) | <.001 | 9.5 (6.3) |
| Physical activity level, mean (SD), MET-min/wk | 473.8 (469.2) | 2077.9 (416.7) | 4618.2 (2431.5) | <.001 | 430.7 (470.2) | 2087.1 (422.4) | 4646.9 (2187.9) | <.001 | 1040.6 (1399.6) |
| Physical activity, mean (SD), min/wk | 104.0 (115.8) | 334.4 (179.2) | 712.8 (447.8) | <.001 | 105.2 (157.6) | 353.8 (136.2) | 766.5 (415.0) | <.001 | 189.4 (247.5) |
| Lifetime physical activity, mean (SD), y | 18.1 (13.3) | 22.8 (13.6) | 25.5 (13.6) | <.001 | 20.1 (15.2) | 26.0 (15.1) | 30.2 (16.3) | <.001 | 20.5 (14.2) |
| CAC score, mean (SD), AU | 11.3 (22.7) | 10.3 (21.5) | 11.5 (22.2) | .42 | 736.1 (975.9) | 680.9 (865.2) | 806.7 (1119.9) | .92 | 187.4 (572.1) |
| Calcification volume score, mean (SD) | 11.0 (28.7) | 10.2 (18.2) | 11.5 (18.6) | .32 | 442.9 (539.8) | 410.4 (488.1) | 474.0 (592.4) | .91 | 128.3 (572.1) |
| No. of calcification lesions, mean (SD) | 1.1 (2.1) | 1.0 (1.7) | 1.2 (2.7) | .41 | 12.5 (12.8) | 11.8 (9.8) | 12.1 (8.6) | .33 | 4.2 (8.2) |
| Cardiorespiratory fitness, mean (SD), MET | 11.0 (1.9) | 12.4 (2.0) | 12.9 (2.3) | <.001 | 10.1 (2.0) | 11.4 (2.1) | 11.8 (2.2) | <.001 | 11.2 (2.1) |
| V̇o2max, mean (SD), mL/kg/min | 38.6 (6.8) | 43.3 (7.0) | 45.1 (8.0) | <.001 | 35.4 (6.9) | 40.1 (7.4) | 41.3 (7.8) | <.001 | 39.2 (7.4) |
| V̇o2max ≥50 mL/kg/min, No. (%) | 571 (5.3) | 439 (16.9) | 246 (24.7) | <.001 | 68 (2.2) | 65 (9.2) | 48 (13.4) | <.001 | 1437 (7.7) |
| Maximum heart rate, mean (SD), bpm | 174.8 (13.4) | 174.6 (12.6) | 173.7 (12.5) | .02 | 165.0 (14.9) | 166.7 (13.7) | 165.9 (14.5) | .005 | 172.6 (14.1) |
| Heart rate recovery at 1 min, mean (SD), bpm | 23.1 (7.5) | 24.9 (7.9) | 25.4 (7.9) | <.001 | 21.8 (8.2) | 22.7 (8.4) | 24.4 (8.9) | <.001 | 23.2 (7.8) |
Abbreviations: AU, Agatston units; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); bpm, beats per minute; CAC, coronary artery calcification; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MET, metabolic equivalent of task; V̇o2max, maximum oxygen consumption.
SI conversion factors: To convert calcium to millimoles per liter, multiply by 0.25; cholesterol to millimoles per liter, multiply by 0.0259; glucose to millimoles per liter, multiply by 0.0555; triglycerides to millimoles per liter, multiply by 0.0113.
Sample sizes were reduced where a specific observation was missing with resulting minimum sample sizes for statin use (n = 20 239), LDL cholesterol level (n = 21 461), calcium level (n = 14 437), lifetime physical activity (n = 13 802), calcification volume (n = 19 411), number of calcifications (n = 19 480), cardiorespiratory fitness (n = 18 564), V̇o2max (n = 18 564), maximum heart rate (n = 18 564), and heart rate recovery (n = 18 564).
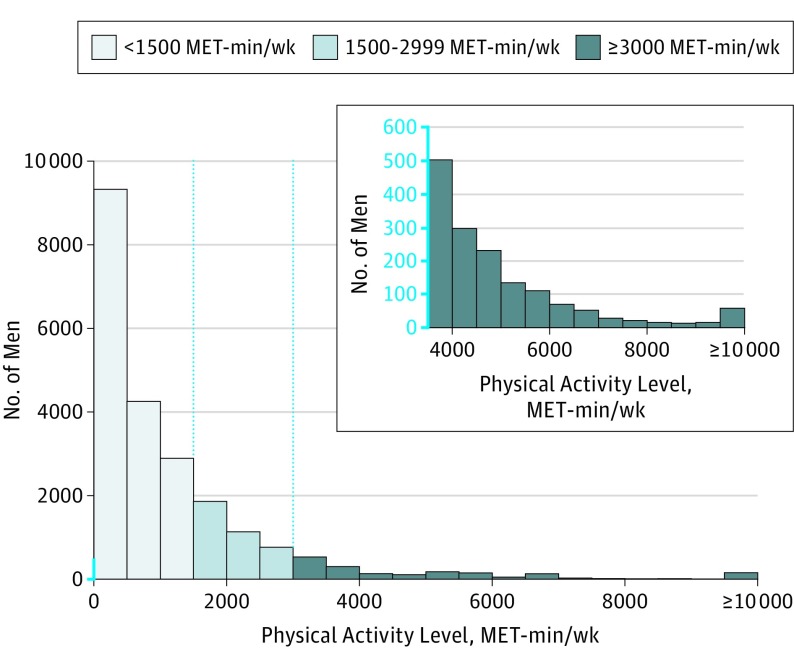
Figure 1 shows the sample distribution of physical activity categories in MET-min/wk, with a high-resolution distribution of the most active group. eTable 4 in the Supplement shows the distribution of activities in MET-min/wk by CAC and physical activity levels. Of note, the highest activity levels are not limited to running or any single activity. A subgroup analysis of those with an additional physical activity assessment within 5 years of baseline found 61.3% of those with physical activity of at least 3000 MET-min/wk at baseline had confirmation of ongoing high levels of physical activity of at least 1500 MET-min/wk. In 18 564 men with CRF measurement (Table 1), the most highly active group were more fit (mean [SD] METs, 12.9 [2.3] or 44.1 [8.1] mL−1 × kg−1 × min−1) and more likely to have an estimated maximal oxygen consumption of at least 50 mL−1 × kg−1 × min−1 than the less active groups.
Figure 1. Distribution of Individuals Across Physical Activity in the Study Population.
Physical activity levels are expressed as metabolic equivalent of task (MET)–minutes/week in 21 758 generally healthy men. The inset represents a magnified presentation of the most highly active individuals (≥3000 MET-min/wk).
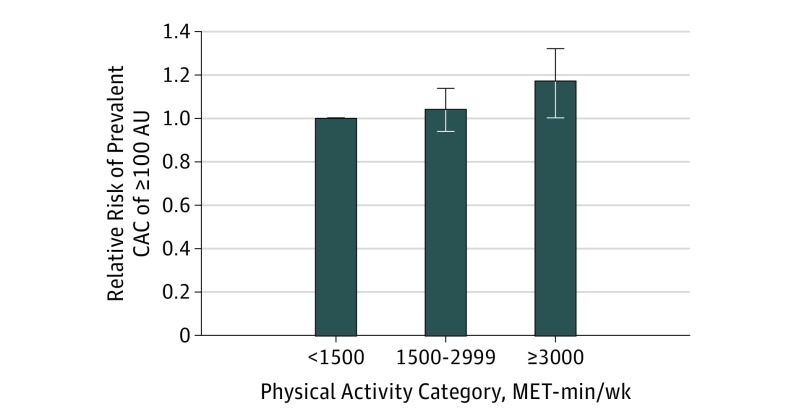
Figure 2 summarizes the relative risk of prevalent CAC by physical activity group. Men with at least 3000 MET-min/wk were more likely to have prevalent CAC of at least 100 AU (relative risk, 1.11; 95% CI, 1.03-1.20) compared with those accumulating lesser amounts of physical activity. The number of all-cause and CVD deaths and associated incidence rates are described in Table 2. During a mean (SD) follow-up of 10.4 (4.3) years, 759 men died, including 180 CVD deaths. Among those with physical activity of at least 3000 MET-min/wk, 40 all-cause and 10 CVD deaths occurred.
Figure 2. Relative Risk of Prevalent Coronary Artery Calcification (CAC).
Data are stratified by physical activity category in metabolic equivalent of task (MET)–minutes/week in 21 758 generally healthy men. The model was adjusted for age, body mass index, levels of glucose and cholesterol, systolic blood pressure, and smoking status. The error bars represent the 95% CIs. AU indicates Agatston units. P = .006 for trend.
Table 2. All-Cause and Cardiovascular Disease Mortality in 21 758 Generally Healthy Men by Physical Activity Category and CAC Category.
| Outcome | Physical Activity Category, MET-min/wk | All Men (N = 21 758) | |||||
|---|---|---|---|---|---|---|---|
| CAC <100 AU | CAC ≥100 AU | ||||||
| <1500 (n = 12 413) | 1500-2999 (n = 2902) | ≥3000 (n = 1129) | <1500 (n = 4034) | 1500-2999 (n = 848) | ≥3000 (n = 432) | ||
| Mean (SD) follow-up time, y | 10.5 (4.3) | 9.8 (4.3) | 9.6 (4.4) | 10.8 (4.3) | 10.5 (4.2) | 10.2 (4.3) | 10.4 (4.3) |
| Total follow-up, y | 130 060.6 | 28 491.3 | 10 782.9 | 43 544.1 | 8912.4 | 4424.0 | 226 215.3 |
| All-cause deaths | |||||||
| No. of deaths | 282 | 42 | 14 | 343 | 52 | 26 | 759 |
| Incidence per 1000 person-years | 2.2 | 1.5 | 1.3 | 7.9 | 5.8 | 5.9 | 3.4 |
| CVD deaths | |||||||
| No. of deaths | 50 | 7 | 2 | 102 | 11 | 8 | 180 |
| Incidence per 1000 person-years | 0.4 | 0.2 | 0.2 | 2.3 | 1.2 | 1.8 | 0.8 |
Abbreviations: AU, Agatston units; CAC, coronary artery calcification; CVD, cardiovascular disease; MET, metabolic equivalent of task.
Age- and multivariate-adjusted analyses revealed 1 statistically significant association among physical activity, CAC, and all-cause mortality (Table 3). In men with CAC of less than 100 AU, those who accumulated at least 3000 MET-min/wk were about half as likely to die compared with men with less than 1500 MET-min/wk (HR, 0.52; 95% CI, 0.29-0.91). In the group with CAC of at least 100 AU, men who accumulated at least 3000 MET-min/wk did not have an increase in all-cause mortality (HR, 0.77; 95% CI, 0.52-1.15) when compared with men with less than 1500 MET-min/wk. When evaluating the association among high physical activity, CAC, and mortality with other CAC cut points, a similar outcome was seen (eTable 5 and 6 in the Supplement), including a statistically significant decrease in all-cause mortality in the highest physical activity group with CAC of at least 1.00 AU (HR, 0.63; 95% CI, 0.44-0.92). Of note, increasing physical activity was not associated with a statistically significant increase in mortality, and no evidence suggested that physical activity hazards for all-cause mortality varied by category of CAC for physical activity of 1500 to less than 3000 MET-min/wk (HR for <1.00 AU, 0.78 [95% CI, 0.56-1.07] vs HR for ≥1.00 AU, 0.87 [95% CI, 0.65-1.17]) and for physical activity of at least 3000 MET-min/wk (HR for <1.00 AU, 0.52 [95% CI, 0.29-0.91] vs HR for ≥1.00 AU, 0.77 [95% CI, 0.52-1.15]; P = .47 for interaction). Similar observations were observed for CVD mortality by category of CAC (physical activity of 1500 to <3000 MET-min/wk: HR for <1.00 AU, 0.66 [95% CI, 0.29-1.51] vs HR for ≥1.00 AU, 0.66 [95% CI, 0.36-1.23]; physical activity of ≥3000 MET-min/wk: HR for <1.00 AU, 0.39 [95% CI, 0.08-1.79] vs HR for ≥1.00 AU, 0.80 [95% CI, 0.39-1.64]; P = .70 for interaction) (see Table 3 for details). Finally, a subgroup analysis was performed with those individuals (n = 20 239) who had medications reported in the study data to evaluate the potential association with statins. Again, HR of less than 1.00 was seen in the high physical activity group after adjusting for statin use (eTable 7 in the Supplement).
Table 3. Hazards for All-Cause and CVD Mortality in 21 758 Generally Healthy Men by CAC and Physical Activity Category.
| Physical Activity Category, MET-min/wk | CAC Category, HR (95% CI) | |||
|---|---|---|---|---|
| <100 AU | ≥100 AU | |||
| Age-Adjusted | Fully Adjusteda | Age-Adjusted | Fully Adjusteda | |
| All-cause mortality | ||||
| <1500 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1500-2999 | 0.73 (0.53-1.01) | 0.78 (0.56-1.07) | 0.82 (0.62-1.10) | 0.87 (0.65-1.17) |
| ≥3000 | 0.55 (0.32-0.94) | 0.52 (0.29-0.91) | 0.72 (0.49-1.08) | 0.77 (0.52-1.15) |
| CVD mortality | ||||
| <1500 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 1500-2999 | 0.69 (0.31-1.52) | 0.66 (0.29-1.51) | 0.58 (0.31-1.09) | 0.66 (0.36-1.23) |
| ≥3000 | 0.45 (0.11-1.83) | 0.39 (0.08-1.79) | 0.75 (0.36-1.54) | 0.80 (0.39-1.64) |
Abbreviations: AU, Agatston units; CAC, coronary artery calcification; CVD, cardiovascular disease; HR, hazard ratio; MET, metabolic equivalent of task.
Adjusted for age, body mass index, glucose level, cholesterol level, systolic blood pressure, and smoking.
Discussion
In this large cohort of men with more than a decade of follow-up, adjusted risk of CAC of at least 100 AU was 11% greater among individuals with very high levels of physical activity compared to those with lower levels. More importantly, no evident association existed between very high levels of physical activity and increased mortality among individuals with and without clinically relevant levels of subclinical atherosclerosis. Indeed, in virtually every analysis, at any cut point of CAC or when considered continuously, individuals with the highest levels of physical activity had lower mortality than those with the lowest activity levels. These results do not support the contention that high-volume endurance activity, with a mean of more than 1 hour of activity per day, increases the risk of all-cause or CVD mortality, regardless of CAC level. The sample size (n = 21 758) and the mean follow-up (10.4 years) are substantially larger than those of other similar studies. Despite this large sample and prolonged follow-up, the number of mortal events in the highest-activity group was remarkably low.
A robust literature describes substantial all-cause and CVD mortality benefits from routine physical activity and CRF.1,23,24,25 However, more recent literature has raised concern that this mortality benefit diminishes with increasing volumes of physical activity. In the Copenhagen City Heart Study,26 individuals reporting 1.0 to 2.4 hours/week of jogging had 71% reduced mortality compared with nonjoggers, but strenuous joggers appeared to have higher mortality (HR, 1.97; 95% CI, 0.48-8.14). Only 2 deaths, however, occurred among the strenuous joggers, and the cause of death was not identified. Conversely, in a meta-analysis of 10 studies evaluating 42 807 elite or professional athletes,27 the elite athletes lived longer and had reduced CVD and cancer mortality (standardized mortality ratio, 0.67; 95% CI, 0.55-0.81) compared with the general population. These studies and others7,28,29 demonstrate mortality benefit in a wide variety of populations in terms of size, participant athleticism, and availability of descriptive information to allow adjustment for competing risks for mortality. Thus, a paucity of evidence suggests that high levels of long-term aerobic activity increase mortality.
Recent studies have raised the possibility that these levels of exercise may increase subclinical atherosclerosis.3,4,5 Most related literature has shown a lack of association between high levels of physical activity and coronary atherosclerosis, but again, these studies include small groups of athletes.9,10,11,30 Two recent studies3,5 have suggested that extreme levels of physical activity, including marathon running, are associated with increased CAC. However, data evaluating high-volume activity athletes with known CAC and long-term clinical outcomes are scarce. Once CAC is discovered, a great clinical concern is whether continued high levels of activity accelerate the transition to clinical disease, including nonfatal and fatal CVD events. In the present study, although highly active men had slightly greater risk of CAC of at least 100 AU, a corresponding greater mortality was not seen.
Several studies have evaluated the joint effects of CAC and physical activity or CRF, a marker of habitual physical activity, on health outcomes.1 A large (N = 10 690) study12 assessed regular physical activity with a low resolution scale from 0 to 10 (0 indicates never; 10, all the time) and demonstrated all-cause mortality was higher with lower activity and higher CAC. With respect to CRF, in a study of 25 972 middle-aged Korean individuals with CAC and CRF measurements who were followed up for 5.5 years,31 those with more than 10-MET CRF (vs lower CRF) had an attenuated association of high CAC with all-cause mortality. Recently, Radford et al32 evaluated more than 8000 healthy men and found that for any baseline age and CAC level, higher CRF was associated with lower annual total CVD incidence. Although these studies evaluated large numbers of individuals, they did not focus on the high levels of physical activity associated with endurance athletes for whom the question of training-induced coronary calcification has been raised. Indeed, the key question addressed in the present study was whether the presence of high CAC associated with high levels of exercise training as typically practiced by masters marathon runners is associated with greater mortality. For this question, the answer is clearly no.
Strengths and Limitations
Strengths of this study include the large sample (21 758 men), long mean duration of follow-up (10.4 years), and the availability of self-reported and measured risk factor information for risk estimation and multivariate analyses. The overall risk profile would suggest that sufficient risk exists within the population for the outcomes of interest to occur. Although physical activity is self-reported, the extensive questionnaire allows solid definition of total physical activity volume. An ample subcohort also underwent treadmill exercise testing for CRF assessment and demonstrated a strong association between reported high levels of activity and high CRF, supporting the cogency of self-reported activity levels.
Limitations in this study include the homogeneity of the population that is predominantly white, well educated, and with access to health care. Although limiting generalizability, this homogeneity removes unmeasured confounders and emphasizes the exposures of interest, including physical activity and CAC. The cross-sectional nature of the analysis between physical activity and CAC limits our ability to make a direct casual inference, but results are suggestive of the physical activity and CAC association previously described. The selected covariates were based on the Framingham Cardiovascular Risk equation33 and represent consistently available variables. Although data regarding baseline statin use are available, information on the length of use or the chronic lipid control level is not. Further, multiple visits were not analyzed owing to the limited mortal events in those with more than 1 visit and, hence, lack information on whether CAC discovery might have led to lifestyle and/or treatment modification. Thus, the patients’ rationale for their high levels of activity is unknown (eg, influence of risk status or existing medical problems).
In this large cohort with long duration of follow-up and a focus on the tail of a distribution, statistical power is limited. Of the 759 deaths, only 40 are among those with high physical activity levels. Power to detect all-cause mortality HRs to 1.60 for high vs low physical activity levels falls below 80% among those with CAC of at least 100 AU as well as less than 100 AU. Power to detect CVD mortality HRs to 2.00 among those with CAC of at least 100 AU and to 2.50 among those with CAC of less than 100 AU falls below 80%. Consequently, and although all our evidence suggests diminished risk at high levels of physical activity, we are unable to rule out risk ratios to these limits.
Conclusions
The present study, with, what is to our knowledge, the best available mortality data in a large population with CAC and quantification of physical activity, advances our understanding of the association of high levels of physical activity, clinically relevant CAC, and mortality. An 11% increase occurred in the adjusted prevalence of CAC of at least 100 AU in the most highly active group, most of whom had a CAC of less than 100 AU. In the presence of CAC and high levels of physical activity, however, the risk of all-cause and CVD mortality was less (compared with lower levels of physical activity) and thus appears to provide evidence against the hypothesis that high levels of activity increase the risk of all-cause or CVD mortality. Our findings should reassure patients and their health care professionals that it appears these highly active individuals can safely continue their exercise programs.
eTable 1. Baseline Characteristics of 9501 Generally Healthy Women by Physical Activity Level and Coronary Artery Calcification Categories
eFigure. Relative Risk of Prevalent Coronary Artery Calcification (≥100 Agatston Units) by Physical Activity Category in 9501 Generally Healthy Women
eTable 2. Total Number of All-Cause and Cardiovascular Disease Mortality in 9501 Generally Healthy Women by Physical Activity Category and Coronary Artery Calcification Category
eTable 3. Mean Physical Activity Reported by 9501 Generally Healthy Women by Physical Activity Category and Coronary Artery Calcification Category
eTable 4. Mean Physical Activity Reported by 21 758 Generally Healthy Men by Physical Activity Category and Coronary Artery Calcification Category
eTable 5. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 21 758 Generally Healthy Men by Coronary Artery Calcification (0 vs ≥1 AU) and Physical Activity Category
eTable 6. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 21 758 Generally Healthy Men by Coronary Artery Calcification (<400 vs ≥400 AU) and Physical Activity Category
eTable 7. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 20 239 Generally Healthy Men by Coronary Artery Calcification (<100 vs ≥100 AU) and Physical Activity Category With Reported Medication Use to Allow Adjustment for Statin Use (n = 3770)
References
- 1.DeFina LF, Haskell WL, Willis BL, et al. Physical activity versus cardiorespiratory fitness: two (partly) distinct components of cardiovascular health? Prog Cardiovasc Dis. 2015;57(4):324-329. doi: 10.1016/j.pcad.2014.09.008 [DOI] [PubMed] [Google Scholar]
- 2.Committee PAGA. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: Dept of Health and Human Services; 2008. [Google Scholar]
- 3.Merghani A, Maestrini V, Rosmini S, et al. Prevalence of subclinical coronary artery disease in masters endurance athletes with a low atherosclerotic risk profile. Circulation. 2017;136(2):126-137. doi: 10.1161/CIRCULATIONAHA.116.026964 [DOI] [PubMed] [Google Scholar]
- 4.Baggish AL, Levine BD. Coronary artery calcification among endurance athletes: “Hearts of Stone”. Circulation. 2017;136(2):149-151. doi: 10.1161/CIRCULATIONAHA.117.028750 [DOI] [PubMed] [Google Scholar]
- 5.Aengevaeren VL, Mosterd A, Braber TL, et al. Relationship between lifelong exercise volume and coronary atherosclerosis in athletes. Circulation. 2017;136(2):138-148. doi: 10.1161/CIRCULATIONAHA.117.027834 [DOI] [PubMed] [Google Scholar]
- 6.Möhlenkamp S, Lehmann N, Breuckmann F, et al. ; Marathon Study Investigators; Heinz Nixdorf Recall Study Investigators . Running: the risk of coronary events: prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J. 2008;29(15):1903-1910. doi: 10.1093/eurheartj/ehn163 [DOI] [PubMed] [Google Scholar]
- 7.Möhlenkamp S, Leineweber K, Lehmann N, et al. Coronary atherosclerosis burden, but not transient troponin elevation, predicts long-term outcome in recreational marathon runners. Basic Res Cardiol. 2014;109(1):391. doi: 10.1007/s00395-013-0391-8 [DOI] [PubMed] [Google Scholar]
- 8.Braber TL, Mosterd A, Prakken NH, et al. Occult coronary artery disease in middle-aged sportsmen with a low cardiovascular risk score: the Measuring Athlete’s Risk of Cardiovascular Events (MARC) study. Eur J Prev Cardiol. 2016;23(15):1677-1684. doi: 10.1177/2047487316651825 [DOI] [PubMed] [Google Scholar]
- 9.Popovic M, Puchner S, Endler G, Foraschik C, Minar E, Bucek RA. The effects of endurance and recreational exercise on subclinical evidence of atherosclerosis in young adults. Am J Med Sci. 2010;339(4):332-336. doi: 10.1097/MAJ.0b013e3181cefbb9 [DOI] [PubMed] [Google Scholar]
- 10.Roberts WO, Schwartz RS, Kraus SM, et al. Long-term marathon running is associated with low coronary plaque formation in women. Med Sci Sports Exerc. 2017;49(4):641-645. doi: 10.1249/MSS.0000000000001154 [DOI] [PubMed] [Google Scholar]
- 11.Pressler A, Suchy C, Friedrichs T, et al. Running multiple marathons is not a risk factor for premature subclinical vascular impairment. Eur J Prev Cardiol. 2017;24(12):1328-1335. doi: 10.1177/2047487317713326 [DOI] [PubMed] [Google Scholar]
- 12.Arnson Y, Rozanski A, Gransar H, et al. Impact of exercise on the relationship between CAC scores and all-cause mortality. JACC Cardiovasc Imaging. 2017;10(12):1461-1468. doi: 10.1016/j.jcmg.2016.12.030 [DOI] [PubMed] [Google Scholar]
- 13.Willis BL, Morrow JR Jr, Jackson AW, Defina LF, Cooper KH. Secular change in cardiorespiratory fitness of men: Cooper Center Longitudinal Study. Med Sci Sports Exerc. 2011;43(11):2134-2139. doi: 10.1249/MSS.0b013e31821c00a7 [DOI] [PubMed] [Google Scholar]
- 14.Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. U S Armed Forces Med J. 1959;10(6):675-688. [PubMed] [Google Scholar]
- 15.Pollock ML, Bohannon RL, Cooper KH, et al. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92(1):39-46. doi: 10.1016/S0002-8703(76)80401-2 [DOI] [PubMed] [Google Scholar]
- 16.Pescatello LS, Arena R, Riebe D, Thompson PD. ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed Philadelphia, PA: Lippincott Williams & Wilkins; 2014. [DOI] [PubMed] [Google Scholar]
- 17.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575-1581. doi: 10.1249/MSS.0b013e31821ece12 [DOI] [PubMed] [Google Scholar]
- 18.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827-832. doi: 10.1016/0735-1097(90)90282-T [DOI] [PubMed] [Google Scholar]
- 19.Cheng YJ, Church TS, Kimball TE, et al. Comparison of coronary artery calcium detected by electron beam tomography in patients with to those without symptomatic coronary heart disease. Am J Cardiol. 2003;92(5):498-503. doi: 10.1016/S0002-9149(03)00714-8 [DOI] [PubMed] [Google Scholar]
- 20.Budoff MJ, Achenbach S, Blumenthal RS, et al. ; American Heart Association Committee on Cardiovascular Imaging and Intervention; American Heart Association Council on Cardiovascular Radiology and Intervention; American Heart Association Committee on Cardiac Imaging, Council on Clinical Cardiology . Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114(16):1761-1791. doi: 10.1161/CIRCULATIONAHA.106.178458 [DOI] [PubMed] [Google Scholar]
- 21.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 22.Masters Road Runnings Marathon. http://www.mastersathletics.net/index.php?id=489. Accessed June 13, 2018.
- 23.Blair SN, Kohl HW III, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262(17):2395-2401. doi: 10.1001/jama.1989.03430170057028 [DOI] [PubMed] [Google Scholar]
- 24.Lavie CJ, Lee DC, Sui X, et al. Effects of running on chronic diseases and cardiovascular and all-cause mortality. Mayo Clin Proc. 2015;90(11):1541-1552. doi: 10.1016/j.mayocp.2015.08.001 [DOI] [PubMed] [Google Scholar]
- 25.Lee DC, Brellenthin AG, Thompson PD, Sui X, Lee IM, Lavie CJ. Running as a key lifestyle medicine for longevity. Prog Cardiovasc Dis. 2017;60(1):45-55. doi: 10.1016/j.pcad.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 26.Schnohr P, O’Keefe JH, Marott JL, Lange P, Jensen GB. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol. 2015;65(5):411-419. doi: 10.1016/j.jacc.2014.11.023 [DOI] [PubMed] [Google Scholar]
- 27.Garatachea N, Santos-Lozano A, Sanchis-Gomar F, et al. Elite athletes live longer than the general population: a meta-analysis. Mayo Clin Proc. 2014;89(9):1195-1200. doi: 10.1016/j.mayocp.2014.06.004 [DOI] [PubMed] [Google Scholar]
- 28.Antero-Jacquemin J, Rey G, Marc A, et al. Mortality in female and male French Olympians: a 1948-2013 cohort study. Am J Sports Med. 2015;43(6):1505-1512. doi: 10.1177/0363546515574691 [DOI] [PubMed] [Google Scholar]
- 29.Levine BD. Can intensive exercise harm the heart? the benefits of competitive endurance training for cardiovascular structure and function. Circulation. 2014;130(12):987-991. doi: 10.1161/CIRCULATIONAHA.114.008142 [DOI] [PubMed] [Google Scholar]
- 30.Bittencourt CR, Izar MC, Schwerz VL, et al. Effects of high-intensity training of professional runners on myocardial hypertrophy and subclinical atherosclerosis. PLoS One. 2016;11(11):e0166009. doi: 10.1371/journal.pone.0166009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi SY, Sung J, Park HE, Han D, Chang HJ. Combined effects of exercise capacity and coronary atherosclerotic burden on all-cause mortality in asymptomatic Koreans. Atherosclerosis. 2016;251:396-403. doi: 10.1016/j.atherosclerosis.2016.05.042 [DOI] [PubMed] [Google Scholar]
- 32.Radford NB, DeFina LF, Leonard D, et al. Cardiorespiratory fitness, coronary artery calcium, and cardiovascular disease events in a cohort of generally healthy middle-age men: results from the Cooper Center Longitudinal Study. Circulation. 2018;137(18):1888-1895. doi: 10.1161/CIRCULATIONAHA.117.032708 [DOI] [PubMed] [Google Scholar]
- 33.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837-1847. doi: 10.1161/01.CIR.97.18.1837 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Baseline Characteristics of 9501 Generally Healthy Women by Physical Activity Level and Coronary Artery Calcification Categories
eFigure. Relative Risk of Prevalent Coronary Artery Calcification (≥100 Agatston Units) by Physical Activity Category in 9501 Generally Healthy Women
eTable 2. Total Number of All-Cause and Cardiovascular Disease Mortality in 9501 Generally Healthy Women by Physical Activity Category and Coronary Artery Calcification Category
eTable 3. Mean Physical Activity Reported by 9501 Generally Healthy Women by Physical Activity Category and Coronary Artery Calcification Category
eTable 4. Mean Physical Activity Reported by 21 758 Generally Healthy Men by Physical Activity Category and Coronary Artery Calcification Category
eTable 5. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 21 758 Generally Healthy Men by Coronary Artery Calcification (0 vs ≥1 AU) and Physical Activity Category
eTable 6. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 21 758 Generally Healthy Men by Coronary Artery Calcification (<400 vs ≥400 AU) and Physical Activity Category
eTable 7. Hazard Ratio for All-Cause and Cardiovascular Disease Mortality in 20 239 Generally Healthy Men by Coronary Artery Calcification (<100 vs ≥100 AU) and Physical Activity Category With Reported Medication Use to Allow Adjustment for Statin Use (n = 3770)