Key Points
Question
Does management of unprotected left main coronary artery stenoses in contemporary clinical practice reflect that reported in clinical trials?
Findings
In this analysis of National Cardiovascular Data Registry CathPCI Registry data including 3.3 million patients, unprotected left main percutaneous coronary intervention (PCI) represented less than 1% of all PCI in clinical practice and was characterized by low operator and institutional volumes, older and more comorbid patients than trial populations, and a higher frequency of adverse events.
Meaning
Trials of unprotected left main PCI do not reflect contemporary practice, although it is possible that case selection and procedural inexperience influence the observed discrepancies; further study is needed to determine if case selection refinement and increasing experience may improve outcomes.
This analysis of National Cardiovascular Data Registry CathPCI Registry data compares the current use and outcomes of unprotected left main percutaneous coronary intervention with results reported in clinical trials.
Abstract
Importance
Recent data support percutaneous revascularization as an alternative to coronary artery bypass grafting in unprotected left main (ULM) coronary lesions. However, the relevance of these trials to current practice is unclear, as patterns and outcomes of ULM percutaneous coronary intervention (PCI) in contemporary US clinical practice are not well studied.
Objective
To define the current practice of ULM PCI and its outcomes and compare these with findings reported in clinical trials.
Design, Setting, and Participants
This cross-sectional multicenter analysis included data collected from 1662 institutions participating in the National Cardiovascular Data Registry (NCDR) CathPCI Registry between April 2009 and July 2016. Data were collected from 33 128 patients undergoing ULM PCI and 3 309 034 patients undergoing all other PCI. Data were analyzed from June 2017 to May 2018.
Main Outcomes and Measures
Patient and procedural characteristics and their temporal trends were compared between ULM PCI and all other PCI. In-hospital major adverse clinical events (ie, death, myocardial infarction, stroke, and emergent coronary artery bypass grafting) were compared using hierarchical logistic regression. Characteristics and outcomes were also compared against clinical trial cohorts.
Results
Of the 3 342 162 included patients, 2 223 570 (66.5%) were male, and the mean (SD) age was 64.2 (12.1) years. Unprotected left main PCI represented 1.0% (33 128 of 3 342 162) of all procedures, modestly increasing from 0.7% to 1.3% over time. The mean (SD) annualized ULM PCI volume was 0.5 (1.5) procedures for operators and 3.2 (6.1) procedures for facilities, with only 1808 of 10 971 operators (16.5%) and 892 of 1662 facilities (53.7%) performing an average of 1 or more ULM PCI annually. After adjustment, major adverse clinical events occurred more frequently with ULM PCI compared with all other PCI (odds ratio, 1.46; 95% CI, 1.39-1.53). Compared with clinical trial populations, patients in the CathPCI Registry were older with more comorbid conditions, and adverse events were more frequent.
Conclusions and Relevance
Use of ULM PCI has increased over time, but overall use remains low. These findings suggest that ULM PCI occurs infrequently in the United States and in an older and more comorbid population than that seen in clinical trials.
Introduction
Left main coronary artery stenosis has traditionally been considered a surgical disease, with clinical practice guidelines recommending coronary artery bypass grafting (CABG) as the preferred treatment.1,2 At the same time, revascularization via percutaneous coronary intervention (PCI) of unprotected left main (ULM) coronary artery stenosis has remained necessary for patients at prohibitive or high risk for surgical intervention,3 representing a small but clinically important population.4 Subsequent data implied that with improvements in technology and procedural techniques, the efficacy of PCI for left main coronary artery revascularization may approach that seen with surgery.5,6,7 Accordingly, randomized clinical trials have been conducted to address this hypothesis. While producing conflicting results, the recent publications of the Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization (EXCEL) trial8 and the Coronary Artery Bypass Grafting Versus Drug Eluting Stent Percutaneous Coronary Angioplasty in the Treatment of Unprotected Left Main Stenosis (NOBLE) trial9 portend a possible paradigm shift in the management of obstructive left main lesions. Despite these developments, to our knowledge, there has not been an assessment of the contemporary practice of ULM PCI in the United States in nearly a decade.4,10 While the results of the EXCEL and NOBLE trials8,9 may have significant implications for coronary revascularization, their applicability to current practice is unclear.
Accordingly, we studied the patient and procedural characteristics associated with ULM PCI in the National Cardiovascular Data Registry (NCDR) CathPCI Registry as well as the clinical outcomes of patients undergoing ULM PCI compared with patients undergoing PCI to other coronary segments as well as with findings reported in recent clinical trials. Understanding current practice for ULM PCI will aid clinicians as they seek to incorporate data from clinical trials into their practices.
Methods
Cohort
The cohort was derived from the NCDR CathPCI Registry, which collects data on patients undergoing PCI at more than 1600 institutions and accounts for greater than 90% of PCI-capable hospitals in the United States.11,12 Registry data elements were prospectively defined (http://cvquality.acc.org/ncdr-home). In the CathPCI Registry, each procedure is linked to both the operator and the institution. Data are entered at each institution using a standardized interface and exported to a central repository, where they undergo regular auditing to ensure optimal data integrity.13 Institutional review board approval was waived for this analysis, as data were derived from a national quality registry. Informed consent was not obtained, as data were deidentified.
We identified all PCI procedures performed at an institution participating in the NCDR CathPCI Registry from April 2009 to July 2016 (CathPCI version 4.0 and later). Procedures were excluded if patients had a history of CABG (providing protection to the left main coronary artery via left-sided bypass grafts) or if they presented for PCI with cardiogenic shock or cardiac arrest, as these procedures and patients would likely not be representative of most PCI in practice. Interventions to chronic total occlusion of the left main coronary artery were excluded for similar reasons. Finally, patients undergoing balloon angioplasty alone (ie, without stenting) were excluded, as these cases could represent interventions to temporize patients for CABG.
Covariates of Interest
Baseline patient demographic, clinical, and procedural characteristics were collected from the CathPCI Registry and compared between patients undergoing ULM PCI and patients undergoing all other PCI. Temporal trends of these characteristics were compared in 2-year increments. Data were chosen based on characteristics and comorbidities associated with PCI outcomes and included age, sex, race/ethnicity, insurance payer, tobacco use, comorbid medical conditions, and characteristics of their presentation for PCI. Procedural risk for mortality was estimated using the CathPCI risk model.14 Procedural data included access site; use of mechanical circulatory support (MCS), stratified into any kind of MCS, use of intra-aortic balloon pump (IABP), or use of non-IABP MCS; timing of MCS initiation; procedural medications, including glycoprotein IIb/IIIa use and anticoagulant choice; and lesion and intervention characteristics, including use of atherectomy, stent type, and bifurcation status. Operator and facility data were also collected from the CathPCI database. Trial data from the EXCEL and NOBLE trials were abstracted directly from the published reports.8,9
Outcomes
In-hospital outcomes were collected from the CathPCI Registry. The primary outcome was in-hospital major adverse clinical events (MACE), which was a composite of death, myocardial infarction (MI), stroke, or emergent CABG. These outcomes were also assessed individually. Emergent CABG was defined as emergent or salvage or with an indication of PCI failure or PCI complication. Outcomes from the EXCEL and NOBLE trials were as published.8,9
Statistical Analysis
We compared patient, procedural, operator, and facility characteristics for patients undergoing ULM PCI and all other PCI, using t tests for continuous variables and χ2 or Fisher exact tests for categorical variables. Similar methods were used to compare characteristics of ULM PCI in the CathPCI Registry with that characteristics in the EXCEL and NOBLE trials.8,9 Patient, procedural, operator, and facility characteristics were also compared for ULM PCI over time, using 1-way analysis of variance tests for continuous variables and χ2 or Fisher exact tests for categorical variables. Multivariable regression was used to assess characteristics associated with adverse outcomes in patients undergoing PCI, including left main vs all other PCI. Secondary analyses used hierarchical logistic regression to assess the association of annual PCI volumes with ULM PCI outcomes by tertiles of operator and institutional PCI volume as well as the association of MCS use with ULM PCI outcomes by tertiles of institutional-level use of MCS. All inferences used a type I error rate of .05, and all P values were 2-tailed. Statistical analyses were performed using R version 3.2.2 (The R Foundation).
Results
Cohort
From April 2009 to July 2016, 4 715 818 patients underwent PCI at institutions participating in the NCDR CathPCI Registry. Of these, 844 471 patients were excluded for a history of CABG, 94 302 for cardiogenic shock, 51 272 for cardiac arrest, 130 815 for intervention to chronic total occlusions, and 253 426 for undergoing balloon angioplasty without stenting. The final cohort consisted of 3 342 162 patients who underwent PCI, of which 33 128 (1.0%) underwent ULM PCI (eFigure 1 in the Supplement).
Demographic, Clinical, Procedural, and Institutional Characteristics
Compared with patients undergoing all other PCI, patients undergoing ULM PCI were older (mean [SD] age, 71.8 [12.4] vs 64.1 [12.1] years) and had a higher burden of medical comorbidities, including history of heart failure (27.7% [9176] vs 10.0% [330 845]), cerebrovascular disease (21.6% [7153] vs 10.6% [351 821]), peripheral arterial disease (21.8% [7224] vs 9.7% [320 828]), diabetes (40.4% [13 368] vs 35.0% [1 158 940]), chronic lung disease (24.5% [8106] vs 14.3% [472 291]), and end-stage renal disease requiring dialysis (5.6% [1849] vs 2.3% [74 870]) (Table 1). Compared with those undergoing all other PCI, patients undergoing ULM PCI presented more commonly with unstable angina or non-ST elevation MI and with more frequent urgent procedural status. These differences were reflected in the NCDR CathPCI predicted risk of in-hospital mortality (ULM PCI: 2.3%; all other PCI: 0.8%; P < .001).
Table 1. Patient Demographic and Clinical Characteristics.
| Characteristic | No. (%) | P Value | ||
|---|---|---|---|---|
| Total (N = 3 342 162) | ULM PCI (n = 33 128) | All Other PCI (n = 3 309 034) | ||
| Demographic Characteristics | ||||
| Age, mean (SD), y | 64.2 (12.1) | 71.8 (12.4) | 64.1 (12.1) | <.001 |
| Male | 2 223 570 (66.5) | 19 875 (60.0) | 2 203 695 (66.6) | <.001 |
| Race | <.001 | |||
| White | 2 898 809 (86.7) | 28 595 (86.3) | 2 870 214 (86.7) | |
| African American | 294 311 (8.8) | 2413 (7.3) | 291 898 (8.8) | |
| Asian | 89 073 (0.6) | 1278 (3.9) | 87 795 (2.7) | |
| Other | 28 018 (0.8) | 401 (1.2) | 27 617 (0.8) | |
| Hispanic ethnicity | 190 753 (5.7) | 1859 (5.6) | 188 894 (5.7) | .47 |
| Insurance payor | <.001 | |||
| None | 228 461 (6.8) | 939 (2.8) | 227 522 (6.9) | |
| Private | 2 154 816 (64.5) | 20 945 (63.2) | 2 133 871 (64.5) | |
| Medicare | 1 623 926 (48.6) | 23 113 (69.8) | 1 600 813 (48.4) | |
| Medicaid | 343 952 (10.3) | 3930 (11.9) | 340 022 (10.3) | |
| Military | 97 397 (2.9) | 1100 (3.3) | 96 297 (2.9) | |
| Other | 59 060 (1.8) | 502 (1.4) | 58 558 (1.8) | |
| History | ||||
| Current tobacco use | 963 078 (28.8) | 6447 (19.5) | 956 631 (28.9) | <.001 |
| Hypertension | 2 677 875 (80.1) | 28 497 (86.0) | 2 649 378 (80.1) | <.001 |
| Dyslipidemia | 2 523 393 (75.6) | 26 847 (81.2) | 2 496 546 (75.5) | <.001 |
| Family history of CAD | 766 160 (22.9) | 5318 (16.1) | 760 842 (23.0) | <.001 |
| Prior MI | 822 618 (24.6) | 11 262 (34.0) | 811 356 (24.5) | <.001 |
| Prior heart failure | 340 021 (10.2) | 9176 (27.7) | 330 845 (10.0) | <.001 |
| Prior PCI | 1 181 763 (35.4) | 12 402 (37.4) | 1 169 361 (35.3) | <.001 |
| ESRD on dialysis | 76 719 (2.3) | 1849 (5.6) | 74 870 (2.3) | <.001 |
| GFR, mean (SD) | 73.1 (17.6) | 73.1 (17.6) | 73.1 (17.5) | <.001 |
| Cerebrovascular disease | 358 974 (10.7) | 7153 (21.6) | 351 821 (10.6) | <.001 |
| Peripheral arterial disease | 328 052 (9.8) | 7224 (21.8) | 320 828 (9.7) | <.001 |
| Chronic lung disease | 480 397 (14.4) | 8106 (24.5) | 472 291 (14.3) | <.001 |
| Diabetes | 1 172 308 (35.1) | 13 368 (40.4) | 1 158 940 (35.0) | <.001 |
| Presentation Characteristics | ||||
| PCI status | <.001 | |||
| Elective | 1 291 227 (38.6) | 11 495 (34.7) | 1 279 732 (38.7) | |
| Urgent | 1 432 072 (42.9) | 18 091 (54.6) | 1 413 981 (42.7) | |
| Emergent | 615 190 (18.4) | 3265 (9.9) | 611 925 (18.5) | |
| Salvage | 2487 (0.1) | 263 (0.8) | 2224 (0.1) | |
| CAD presentation | <.001 | |||
| No symptoms | 225 269 (6.7) | 3274 (9.9) | 221 995 (6.7) | |
| Unlikely ischemic | 78 680 (2.4) | 860 (2.6) | 77 820 (2.4) | |
| Stable angina | 476 713 (14.3) | 4419 (13.3) | 472 294 (14.3) | |
| Unstable angina | 1 265 483 (37.9) | 13 881 (41.9) | 1 251 602 (37.8) | |
| Non-STEMI | 725 678 (21.7) | 8364 (25.3) | 717 314 (21.7) | |
| STEMI | 569 498 (17.0) | 2321 (7.0) | 567 177 (17.1) | |
| CCS class (2 wk) | <.001 | |||
| 0 | 338 201 (10.1) | 4509 (13.6) | 333 692 (10.1) | |
| 1 | 131 133 (3.9) | 912 (2.8) | 130 221 (3.9) | |
| 2 | 490 974 (14.7) | 3734 (11.3) | 487 240 (14.8) | |
| 3 | 1 170 340 (35.1) | 11 557 (34.9) | 1 158 783 (35.1) | |
| 4 | 1 204 445 (36.1) | 12 357 (37.4) | 1 192 088 (36.1) | |
| Antianginal medications (2 wk) | 2 304 937 (69.0) | 26 667 (80.5) | 2 278 270 (68.9) | <.001 |
| Heart failure medications (2 wk) | 325 063 (9.7) | 9816 (29.6) | 315 247 (9.5) | <.001 |
| Cardiomyopathy | 313 623 (9.4) | 7855 (23.7) | 305 768 (9.2) | <.001 |
| CathPCI Registry Procedural risk, mean (SD), % | 0.8 (2.6) | 2.3 (7.7) | 0.8 (2.5) | <.001 |
Abbreviations: CAD, coronary artery disease; CCS, Canadian Cardiovascular Society; ESRD, end-stage renal disease; GFR, glomerular filtration rate; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction; ULM, unprotected left main.
Unprotected left main PCI was performed via femoral access more frequently than other PCI (86.2% [28 535] vs 77.9% [2 577 738]; P < .001) and with significantly more use of MCS (24.7% [8169] vs 1.3% [43 928]; P < .001). Intra-aortic balloon pump counterpulsation represented slightly greater than half of MCS used for ULM PCI (55.6% [4538 of 8169]), while IABP use represented most of MCS used for all other PCI (83.1% [36 513 of 43 928]). Atherectomy was used more commonly in ULM PCI (9.3% [3087] vs 1.4% [46 705]; P < .001), with most being rotational. Drug-eluting stents were used in most interventions for both ULM PCI and all other PCI (Table 2). Of 33 128 patients undergoing ULM PCI, 24 520 left main coronary artery lesions (74.0%) were considered class C, with 14 947 lesions (45.1%) involving a bifurcation. Of these bifurcation lesions, 6053 (40.5%) were treated with a 2-stent strategy. Multivessel PCI was performed in 15 635 ULM interventions (47.2%), as opposed to 727 907 (22.0%) of all other PCI (P < .001). The mean (SD) number of stents used was 2.2 (1.3), and the mean (SD) lesion length was 51.8 (54.7) millimeters.
Table 2. Procedural and Institutional Characteristics.
| Characteristic | No. (%) | P Value | ||
|---|---|---|---|---|
| Total (N = 3 342 162) | ULM PCI (n = 33 128) | All Other PCI (n = 3 309 034) | ||
| Procedural Characteristics | ||||
| Arterial access site | <.001 | |||
| Femoral | 2 606 273 (78.0) | 28 535 (86.2) | 2 577 738 (77.9) | |
| Brachial | 8529 (0.3) | 180 (0.5) | 8349 (0.3) | |
| Radial | 724 499 (21.7) | 4323 (13.1) | 720 176 (21.8) | |
| Other | 1778 (0.1) | 81 (0.2) | 1697 (0.1) | |
| MCS | 52 097 (1.6) | 8169 (24.7) | 43 928 (1.3) | <.001 |
| Before PCI | 7278 (0.2) | 1722 (5.2) | 5556 (0.2) | <.001 |
| During or after PCI | 36 554 (1.1) | 3442 (10.4) | 33 112 (1.0) | <.001 |
| IABP | 41 051 (1.2) | 4538 (13.7) | 36 513 (1.1) | <.001 |
| Before PCI | 4459 (0.1) | 1095 (3.3) | 3364 (0.1) | <.001 |
| During or after PCI | 26 825 (0.8) | 68 (0.2) | 26 757 (0.8) | <.001 |
| Other MCS | 12 630 (0.4) | 4023 (12.1) | 8607 (0.3) | <.001 |
| Before PCI | 2894 (0.1) | 648 (2.0) | 2246 (0.1) | <.001 |
| During or after PCI | 9729 (0.3) | 3374 (10.2) | 6355 (0.2) | <.001 |
| Contrast volume, mean (SD), mL | 185.1 (83.6) | 216.9 (114.1) | 184.8 (83.1) | <.001 |
| Fluoroscopy time, mean (SD), min | 13.5 (10.4) | 23.0 (16.4) | 13.4 (10.3) | <.001 |
| Lesion Characteristics | ||||
| Class C lesion | 1 855 009 (55.7) | 24 520 (74.0) | 1 830 489 (55.5) | <.001 |
| LMCA bifurcation | NA | 14 947 (45.1) | NA | NA |
| 1 Stent | NA | 8871 (26.8) | NA | NA |
| >1 Stent | NA | 6053 (18.3) | NA | NA |
| Missing | NA | 23 (0.1) | NA | NA |
| Lesion treated previously | 310 066 (9.3) | 2909 (8.8) | 307 157 (9.3) | <.001 |
| Restenosis | 263 664 (7.9) | 2464 (7.4) | 261 200 (7.9) | .001 |
| Stent thrombosis | 42 790 (1.3) | 231 (0.7) | 42 559 (1.3) | <.001 |
| Lesion length, mean (SD), mm | 30.1 (27.8) | 51.8 (54.7) | 29.9 (27.3) | <.001 |
| No. of lesions treated, mean (SD) | 1.4 (0.6) | 2.0 (1.1) | 1.3 (0.6) | <.001 |
| Multivessel PCI | 743 542 (22.2) | 15 635 (47.2) | 727 907 (22.0) | <.001 |
| PCI Characteristics | ||||
| Atherectomy | <.001 | |||
| Laser | 4734 (0.1) | 135 (0.4) | 4599 (0.1) | |
| Orbital | 6353 (0.2) | 303 (0.9) | 6050 (0.2) | |
| Rotational | 38 705 (1.2) | 2649 (8.0) | 36 056 (1.1) | |
| Thrombectomy | ||||
| Aspiration | 136 864 (4.1) | 530 (1.6) | 136 334 (4.1) | <.001 |
| Mechanical | 14 041 (0.4) | 117 (0.4) | 13 924 (0.4) | .06 |
| Cutting or scoring balloon | 133 315 (4.0) | 3409 (10.3) | 129 906 (3.9) | <.001 |
| No. of stents, mean (SD) | 1.5 (0.8) | 2.2 (1.3) | 1.5 (0.8) | <.001 |
| BMS | 619 169 (18.5) | 4831 (14.6) | 614 338 (18.6) | <.001 |
| DES | 2 756 071 (82.5) | 29 226 (88.2) | 2 726 845 (82.4) | <.001 |
| Stent type | <.001 | |||
| Cobalt chromium EES | 1 264 395 (45.9) | 12 662 (43.3) | 1 251 733 (45.9) | |
| Platinum chromium EES | 581 530 (21.1) | 7059 (24.2) | 574 471 (21.1) | |
| ZES | 602 324 (21.9) | 5636 (19.3) | 596 688 (21.9) | |
| PES | 168 608 (6.1) | 1207 (4.1) | 167 401 (6.1) | |
| SES | 61 284 (2.2) | 427 (1.5) | 60 857 (2.2) | |
| Bioabsorbable DES | 519 (0.0) | 0 | 519 (0.0) | |
| Other DES | 515 (0.0) | 6 (0.0) | 509 (0.0) | |
| >1 DES type | 76 896 (2.8) | 2229 (7.6) | 74 667 (2.7) | |
| Operator annual PCI volume, mean (SD) | 102.6 (68.5) | 128.4 (91.0) | 102.3 (68.2) | <.001 |
| Institutional Characteristics | ||||
| Institutional location | <.001 | |||
| Rural | 437 460 (13.1) | 2882 (8.7) | 434 578 (13.1) | |
| Suburban | 1 029 765 (30.8) | 8319 (25.1) | 1 021 446 (30.9) | |
| Urban | 1 874 937 (56.1) | 21 927 (66.2) | 1 853 010 (56.0) | |
| Institutional designation | <.001 | |||
| Government | 36 827 (1.1) | 320 (0.7) | 36 507 (1.1) | |
| Private/community | 2 901 604 (86.8) | 25 645 (77.4) | 2 875 959 (86.9) | |
| University | 403 731 (12.1) | 7163 (21.6) | 396 568 (12.0) | |
| Teaching institution | 1 624 038 (48.6) | 20 634 (62.3) | 1 603 404 (48.5) | <.001 |
| Institutional census division | <.001 | |||
| E North Central | 620 265 (18.6) | 5524 (16.7) | 614 741 (18.6) | |
| E South Central | 283 289 (8.5) | 1817 (5.5) | 281 472 (8.5) | |
| Middle Atlantic | 400 730 (12.0) | 3842 (11.6) | 396 888 (12.0) | |
| Mountain | 164 696 (4.9) | 1494 (4.5) | 163 202 (4.9) | |
| New England | 138 721 (4.2) | 1552 (4.7) | 137 169 (4.1) | |
| Pacific | 366 298 (11.0) | 5804 (17.5) | 360 494 (10.9) | |
| South Atlantic | 767 927 (23.0) | 6420 (19.4) | 761 507 (23.0) | |
| W North Central | 282 283 (8.4) | 3785 (11.4) | 278 498 (8.4) | |
| W South Central | 317 887 (9.5) | 2890 (8.7) | 314 997 (9.5) | |
| Institutional annual PCI volume, mean (SD) | 600.3 (404.6) | 693.9 (429.8) | 599.3 (404.3) | <.001 |
| On-site surgical back-up | 2 883 567 (86.3) | 30 763 (92.9) | 2 852 804 (86.2) | <.001 |
Abbreviations: BMS, bare-metal stent; DES, drug-eluting stent; EES, everolimus-eluting stent; IABP, intra-aortic balloon pump; LMCA, left main coronary artery; MCS, mechanical circulatory support; NA, not applicable; PCI, percutaneous coronary intervention; PES, paclitaxel-eluting stent; SES, sirolimus-eluting stent; ULM, unprotected left main; ZES, zotarolimus-eluting stent.
Annual PCI volume was higher among ULM PCI operators (mean [SD] procedures, 128.4 [91.0] vs 102.3 [68.2]; P < .001) and institutions performing ULM PCI (mean [SD] procedures, 693.9 [429.8] vs 599.3 [404.3]; P < .001) compared with operators and institutions performing all other PCI. Unprotected left main PCI was performed most frequently at institutions in urban settings and with private or community designations. Unprotected left main PCI was performed most frequently in the South Atlantic and Pacific census divisions. On-site surgical backup was present more frequently among institutions performing ULM PCI (92.9% [30 763] vs 86.2% [2 852 804]; P < .001).
Temporal Trends in ULM PCI
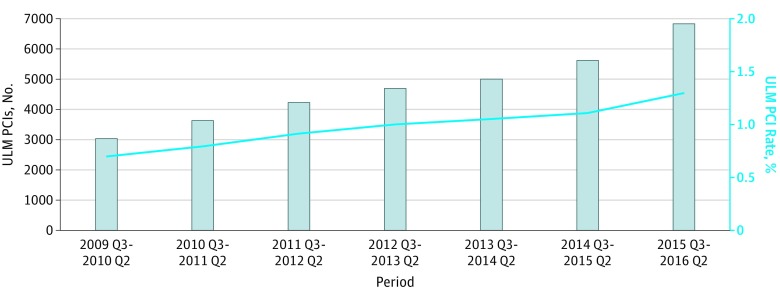
Unprotected left main PCI use has increased over time, from 3054 procedures between quarter 3 of 2009 and quarter 2 of 2010 (0.7% of all PCIs performed) to a peak of 6829 procedures between quarter 3 of 2015 and quarter 2 of 2016 (1.3% of all PCIs performed) (Figure 1). Age and sex were similar across the study period between patients undergoing ULM PCI and patients undergoing all other PCI. However, rates of medical comorbidities increased significantly in those undergoing ULM PCI. Estimated risk of inpatient mortality increased over time, from 2.2% to 2.5% (P = .02) (eTable 1 in the Supplement).
Figure 1. Temporal Trends in Unprotected Left Main (ULM) Percutaneous Coronary Intervention (PCI).
Use of ULM PCI over time in aggregate and as a proportion of all other PCI. Q indicates quarter.
Use of radial access increased from 4.7% (315 of 6696) from 2009 to 2011 to 20.3% (1383 of 6829) from 2015 to 2016 (P < .001). Between these periods, use of MCS increased modestly (22.6% [1511] to 29.2% [1995]; P < .001), but use of IABP declined (15.8% [1055] to 11.8% [806]; P < .001) and use of other MCS increased (7.9% [529] to 18.8% [1281]; P < .001). Rates of atherectomy increased over the study period from 6.9% (465) to 9.4% (641) (P < .001); atherectomy was mainly rotational but with an increasing proportion of orbital atherectomy (0% to 22.5% [144 of 641] of all atherectomy; P < .001) (eTable 2 in the Supplement).
Composite rates of in-hospital death, MI, stroke, or emergent CABG decreased over time (2009-2011, 9.3% [620 of 6696]; 2015-2016, 7.8% [532 of 6829]; P = .01). Individual rates of MI also decreased over time (2009-2011, 4.5% [303]; 2015-2016, 2.5% [169]; P < .001), while rates of death, stroke, and emergent CABG did not differ significantly (eTable 3 in the Supplement).
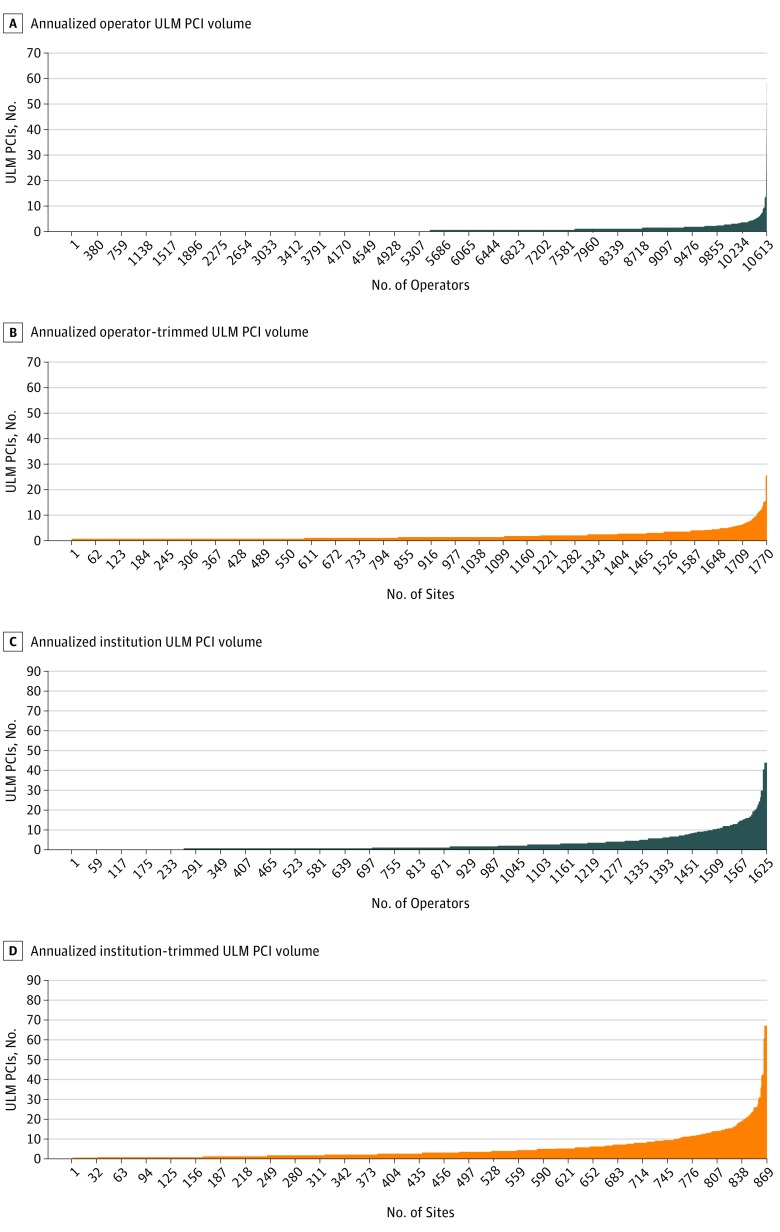
Variation in Performance of ULM PCI
The mean (SD) annualized volume of ULM PCI across operators in the CathPCI Registry was 0.5 (1.5) procedures, with only 1808 operators (16.7%) averaging 1 or more ULM PCI annually (Figure 2A). Discounting all operators averaging less than 1 ULM PCI annually over the study period, the trimmed operator mean (SD) annual volume was 2.5 (2.8) ULM PCI per year (Figure 2B). Among operators performing any left main PCI, the median annualized ULM PCI volume was 1.75 ULM PCI per year. The mean (SD) annualized volume of ULM PCI across institutions participating in the CathPCI Registry was 3.2 (6.1) procedures, with 892 institutions (53.7%) averaging 1 or more ULM PCI annually (Figure 2C). Discounting all institutions averaging less than 1 ULM PCI annually over the study period, the trimmed institutional mean (SD) annual volume was 5.7 (7.4) ULM PCI per year (Figure 2D). Among institutions performing at least 1 ULM PCI annually, the median annualized volume was 3.31 ULM PCI per year.
Figure 2. Variation in Use of Unprotected Left Main (ULM) Percutaneous Coronary Intervention (PCI) Across Operators and Institutions.
A, Variation in annualized volume of ULM PCI across operators. B, Variation in annualized volume of ULM PCI across operators averaging at least 1 ULM PCI per year. C, Variation in annualized volume of ULM PCI across institutions. D, Variation in annualized volume of ULM PCI across institutions averaging at least 1 ULM PCI per year.
Outcomes
Patients undergoing ULM PCI had a significantly higher rate of MACE compared with all other PCI (9.0% [2993] vs 2.6% [86 940]; P < .001). Unprotected left main PCI also had higher frequency of each individual outcome, including death (5.0% [1643] vs 0.6% [21 344]), MI (3.9% [1285] vs 1.8% [60 015]), stroke (0.5% [176] vs 0.2% [6304]), and emergent CABG (0.7% [224] vs 0.1% [3219]) (Table 3). After covariate adjustment, the odds of MACE were significantly increased with ULM PCI compared with all other PCI (odds ratio [OR], 1.46; 95% CI, 1.39-1.53) (eFigure 2 in the Supplement).
Table 3. In-Hospital Outcomes.
| Outcome | No. (%) | P Value | ||
|---|---|---|---|---|
| Total (N = 3 342 162) | ULM PCI (n = 33 128) | All Other PCI (n = 3 309 034) | ||
| Death, MI, stroke, or emergent CABG | 89 933 (2.7) | 2993 (9.0) | 86 940 (2.6) | <.001 |
| Death | 22 987 (0.7) | 1643 (5.0) | 21 344 (0.6) | <.001 |
| MI (biomarker positive) | 61 300 (1.8) | 1285 (3.9) | 60 015 (1.8) | <.001 |
| Stroke | 6480 (0.2) | 176 (0.5) | 6304 (0.2) | <.001 |
| Emergent CABG | 3443 (0.1) | 224 (0.7) | 3219 (0.1) | <.001 |
Abbreviations: CABG, coronary artery bypass grafting; MI, myocardial infarction; PCI, percutaneous coronary intervention; ULM, unprotected left main.
Secondary Analyses
Annual PCI Volume
When stratified by tertiles of institutional annual PCI volumes, lower rates of MACE occurred after ULM PCI at institutions and among operators in the highest tertile of PCI volume compared with the first and second tertiles (eTable 4 in the Supplement). After adjustment, higher tertiles of annual PCI volume were associated with improved outcomes at the institutional level (tertile 2 vs tertile 1: OR, 0.90; 95% CI, 0.80-1.01; tertile 3 vs tertile 1: OR, 0.84; 95% CI, 0.74-0.96) and operator level (tertile 2 vs tertile 1: OR, 0.94; 95% CI, 0.91-0.97; tertile 3 vs tertile 1: OR, 0.90; 95% CI, 0.87-0.93).
Mechanical Circulatory Support
When stratified by tertiles of institutional use of MCS, increased rates of MACE were observed with increased use of IABP counterpulsation in the highest tertile compared with the first and second tertiles (eTable 4 in the Supplement). After multivariable adjustment, higher tertiles of IABP use during ULM PCI remained associated with increased MACE (tertile 2 vs tertile 1: OR, 1.11; 95% CI, 1.004-1.22; tertile 3 vs tertile 1: OR, 1.17; 95% CI, 1.07-1.30), while there was no difference in MACE across institutional tertiles of non-IABP MCS use (tertile 2 vs tertile 1: OR, 0.95; 95% CI, 0.85-1.06; tertile 3 vs tertile 1: OR, 1.07; 95% CI, 0.96-1.20).
Comparison With Clinical Trials
Compared with recent trials,8,9 patients undergoing ULM PCI at CathPCI Registry institutions were significantly older and had more medical comorbidities (eTable 5 in the Supplement). Mortality and stroke occurred more frequently among patients in the CathPCI Registry compared with participants of the EXCEL and NOBLE trials,8,9 while rates of inpatient MI were similar. While SYNTAX scores are not available for patients in this study, other markers of anatomic complexity, such as lesion length and number of stents, were similar to those in EXCEL trial.8 Left main bifurcation lesions were less frequent among patients undergoing ULM PCI (45.1% [14 947 of 33 128]) compared with patients in the EXCEL trial (80.5% [763 of 948]) and the NOBLE trial (85.8% [508 of 592]) (P < .001), but 2-stent strategies were used more frequently for these lesions in patients undergoing ULM PCI than in the NOBLE trial (40.5% [6053 of 14 947] vs 36.8% [187 of 508]; P < .001).9 Intravascular imaging was used less frequently among patients undergoing ULM PCI (39.8% [4557 of 11 437]) than patients in the EXCEL trial (76.2% [722 of 948]) and the NOBLE trial (74.9% [430 of 574]) (P < .001), while MCS use was nearly 5-fold higher in patients undergoing ULM PCI compared with patients in the EXCEL trial (24.7% [8169 of 33 128] vs 5.6% [53 of 948]; P < .001).
Discussion
We describe contemporary practice of ULM PCI in the United States, as represented in the NCDR CathPCI Registry. While use of ULM PCI has numerically doubled over time from 2009 to 2016, it remains a small proportion of all PCI, modestly increasing from 0.7% to 1.3% over the study period. Patients undergoing ULM PCI were older, had more comorbid conditions than patients undergoing all other PCI, and demonstrated high rates of mortality, MI, stroke, and emergent CABG. These patients, their characteristics, and outcomes stand in contrast with those reported by clinical trials evaluating ULM PCI, demonstrating key differences between contemporary clinical practice and trial populations. Finally, we observed remarkably low operator and institutional volumes, with, on average, less than 1 annual ULM PCI for operators and only 3 ULM PCI for institutions.
Our findings document a slow uptake of ULM PCI performance in the United States despite emerging data suggesting ULM PCI as a reasonable alternative to CABG. The 5-year follow-up of the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) trial15 suggested similar outcomes for left main coronary artery PCI vs CABG with intermediate or low SYNTAX scores, and after the emergence of additional supporting data,16 both US and international guidelines shifted recommendations to include either percutaneous or surgical revascularization for ULM stenoses in the absence of complex anatomic features.1,17 The recent publications of the EXCEL and NOBLE trials8,9 offered further insights. The EXCEL trial suggested equivalence in outcomes for CABG and PCI in the treatment of ULM stenoses,8 while the NOBLE trial suggested better outcomes with CABG.9 These divergent findings have been attributed to differences in patient populations and trial designs, particularly with respect to the primary end point definitions.18,19 Professional guidelines continue to recommend consideration of both ULM PCI and surgical revascularization for treatment of left main stenoses, incorporating patient and anatomic complexity into decision making.
However, in contrast to clinical trials, the present analysis demonstrates significantly worse outcomes for a contemporary cohort undergoing ULM PCI in the United States as well as major differences in demographic, clinical, and procedural characteristics. Much of this demonstrated difference in outcomes is likely attributable to patient and procedural factors, with age and burden of comorbidities greater among patients in the CathPCI Registry than those reported in clinical trials, and procedural distinctions, such as the use of intravascular imaging. The difference in patient populations is further highlighted by the nearly 5-fold increase in use of MCS among patients in the CathPCI Registry compared with in clinical trials. With a higher burden of comorbidities among patients undergoing ULM PCI, it is possible that there is significant selection bias in management strategies wherein more clinically complex patients may undergo percutaneous rather than surgical revascularization in clinical practice.20 Additionally, these findings suggest that PCI is an infrequently used management strategy for ULM stenoses. The estimated prevalence of left main disease found during diagnostic angiography is 6% in published series.21,22 With more than 1 million coronary angiograms performed annually in the United States,23 the annual number of patients undergoing ULM PCI is quite low in comparison to the extrapolated incidence of ULM stenoses. Therefore, most patients with ULM stenoses are likely managed with strategies other than PCI in contemporary practice. Despite limited use of PCI for ULM stenoses, this analysis found 1662 institutions performing at least 1 ULM PCI during the study period, while randomized clinical trials were limited to a small number of high-volume centers (126 centers in the EXCEL trial8 and 36 centers in the NOBLE trial9). Furthermore, there is significant variability in the frequency of ULM PCI performance across registry operators and institutions. Taken together, these findings suggest that ULM PCI is performed in older patients with high degrees of morbidity, performed with significant variability in operator and institutional procedural experience, and represents a minority of the management of left main stenosis. This raises the possibility that operator and institutional inexperience may play a role in addition to patient and procedural features in the observed difference in outcomes.
There are several possibilities to explain the limited rates of ULM PCI in contemporary practice. One is likely the comfort and experience that referring physicians have with CABG. Its historical efficacy and operator and institutional experience may influence referring physicians to send patients with ULM stenosis for coronary artery bypass surgery despite data suggesting equivalent short-term and mid-term outcomes in patients with lower anatomic complexity. It is also possible that clinicians see that real-world outcomes for patients undergoing ULM PCI—many of whom are older, frail, and may be determined to be at prohibitive risk for surgery—compare unfavorably with patients undergoing both all other PCI as well as CABG, leaving practitioners hesitant to refer younger, healthier patients for ULM PCI and further propagating the demonstrated differences in case mix. Third, it is likely that high-risk patients and procedures, like the older and comorbid patients presenting with acute coronary syndromes in this registry population, would be less likely to be enrolled in clinical trials, underscoring another important difference when considering trial results in the context of clinical practice. Fourth, it is possible that through a combination of low overall use and diffusion of higher-risk cases across operators and centers, operators and institutions are less comfortable performing ULM PCI compared with operators involved in randomized trials. The observed rates of 3.2 ULM PCI per year for institutions and 0.5 ULM PCI per year for operators in clinical practice are fractions of the rates published in clinical trials, with an institutional average of 7.5 PCIs in the EXCEL trial,8 16.4 PCIs in the NOBLE trial,9 and more than 20 left main coronary interventions and more than 300 PCIs per year for operators included in the recently published Double Kissing and Double Crush Versus Provisional T Stenting Technique for the Treatment of Unprotected Distal Left Main True Bifurcation Lesions (DKCRUSH-V) trial.24 Additionally, the significantly increased use of MCS in the CathPCI Registry compared with clinical trials may reflect these contrasting levels of procedural inexperience as opposed to solely medical or anatomic factors. As published data support an association of increasing volumes with improved PCI outcomes, it is possible that a similar association exists between ULM PCI volume and outcomes.25,26 Our findings of an association of increasing operator and institutional PCI volumes with lower risks of MACE following ULM PCI would support this hypothesis. Thus, it is perhaps unsurprising and even judicious that ULM PCI remains infrequent, given limited operator experience and observed poor outcomes in a high-risk patient population. Concentrating ULM PCI performance to experienced centers and high-volume operators could potentially facilitate improved outcomes. Alternatively, broadening use of ULM PCI among lower-risk patients (more similar to those seen in clinical trials) may augment operator and institutional volumes to attain operator experience and comfort among patients more likely to have successful procedures.
Study Limitations
The findings of the present analysis should be interpreted while considering several limitations. First, as an observational analysis, residual confounding may be present and could bias findings. Demonstrated differences in demographic and clinical characteristics between patients undergoing ULM PCI vs not undergoing ULM PCI suggest selective use of ULM PCI in high-risk patients at participating CathPCI Registry institutions. These differences limit comparison with other published studies but underscore the restricted use of a viable treatment modality of ULM revascularization. Second, use of registry data requires assumptions that data are reported completely and accurately. While error in data collection or entry is possible, the NCDR CathPCI Registry undergoes periodic auditing to ensure optimal data integrity. Third, we were unable to ascertain longitudinal outcomes for patients undergoing ULM PCI, as postdischarge data are not available in the CathPCI Registry. Fourth, we were unable to compare treatment with ULM PCI with CABG or medical therapy. These groups are important for understanding the entirety of management of patients with ULM stenoses as well as clinical outcomes and factors associated with patient, operator, or institutional determination of treatment strategy and represent an opportunity for further study. Finally, the inability to calculate SYNTAX scores limited our ability to define the influence of anatomic complexity on outcomes and limited our ability to characterize compliance with past and current guideline recommendations.
Conclusions
Among patients treated at institutions participating in the CathPCI Registry, ULM PCI occurs infrequently and in an older and more comorbid population than those represented in clinical trials. While ULM PCI increased over the study period, operator and institutional volumes remained variable and limited, and outcomes were significantly worse than those seen in clinical trials. These findings suggest that randomized clinical trials demonstrating safety and efficacy of ULM PCI do not reflect contemporary clinical practice and suggest an opportunity to refine patient selection and increase operator and institutional experience as potential means to improving outcomes.
eTable 1. Demographic and clinical characteristics of patients undergoing ULM PCI over time.
eTable 2. Procedural characteristics of ULM PCI over time.
eTable 3. Clinical outcomes of patients undergoing ULM PCI over time.
eTable 4. Clinical outcomes of patients undergoing ULM PCI stratified by tertile of operator and institutional annual PCI volumes and by tertile of institutional use of mechanical circulatory support.
eTable 5. Baseline characteristics and outcomes in patients who underwent left main PCI in the NCDR, EXCEL trial, and NOBLE trial.
eFigure 1. Cohort creation.
eFigure 2. Factors associated with increased rates of major adverse cardiac events after multivariate adjustment.
References
- 1.Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64(18):1929-1949. doi: 10.1016/j.jacc.2014.07.017 [DOI] [PubMed] [Google Scholar]
- 2.Kolh P, Windecker S, Alfonso F, et al. ; European Society of Cardiology Committee for Practice Guidelines; EACTS Clinical Guidelines Committee; Task Force on Myocardial Revascularization of the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery; European Association of Percutaneous Cardiovascular Interventions . 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg. 2014;46(4):517-592. doi: 10.1093/ejcts/ezu366 [DOI] [PubMed] [Google Scholar]
- 3.McNulty EJ, Ng W, Spertus JA, et al. Surgical candidacy and selection biases in nonemergent left main stenting: implications for observational studies. JACC Cardiovasc Interv. 2011;4(9):1020-1027. doi: 10.1016/j.jcin.2011.06.010 [DOI] [PubMed] [Google Scholar]
- 4.Brennan JM, Dai D, Patel MR, et al. Characteristics and long-term outcomes of percutaneous revascularization of unprotected left main coronary artery stenosis in the United States: a report from the National Cardiovascular Data Registry, 2004 to 2008. J Am Coll Cardiol. 2012;59(7):648-654. doi: 10.1016/j.jacc.2011.10.883 [DOI] [PubMed] [Google Scholar]
- 5.Cavalcante R, Sotomi Y, Lee CW, et al. Outcomes after percutaneous coronary intervention or bypass surgery in patients with unprotected left main disease. J Am Coll Cardiol. 2016;68(10):999-1009. doi: 10.1016/j.jacc.2016.06.024 [DOI] [PubMed] [Google Scholar]
- 6.Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery trial. Circulation. 2014;129(23):2388-2394. doi: 10.1161/CIRCULATIONAHA.113.006689 [DOI] [PubMed] [Google Scholar]
- 7.Serruys PW, Morice MC, Kappetein AP, et al. ; SYNTAX Investigators . Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961-972. doi: 10.1056/NEJMoa0804626 [DOI] [PubMed] [Google Scholar]
- 8.Stone GW, Sabik JF, Serruys PW, et al. ; EXCEL Trial Investigators . Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375(23):2223-2235. doi: 10.1056/NEJMoa1610227 [DOI] [PubMed] [Google Scholar]
- 9.Mäkikallio T, Holm NR, Lindsay M, et al. ; NOBLE study investigators . Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016;388(10061):2743-2752. doi: 10.1016/S0140-6736(16)32052-9 [DOI] [PubMed] [Google Scholar]
- 10.Huang HW, Brent BN, Shaw RE. Trends in percutaneous versus surgical revascularization of unprotected left main coronary stenosis in the drug-eluting stent era: a report from the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Catheter Cardiovasc Interv. 2006;68(6):867-872. doi: 10.1002/ccd.20886 [DOI] [PubMed] [Google Scholar]
- 11.Brindis RG, Fitzgerald S, Anderson HV, Shaw RE, Weintraub WS, Williams JF. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR): building a national clinical data repository. J Am Coll Cardiol. 2001;37(8):2240-2245. doi: 10.1016/S0735-1097(01)01372-9 [DOI] [PubMed] [Google Scholar]
- 12.Moussa I, Hermann A, Messenger JC, et al. The NCDR CathPCI Registry: a US national perspective on care and outcomes for percutaneous coronary intervention. Heart. 2013;99(5):297-303. doi: 10.1136/heartjnl-2012-303379 [DOI] [PubMed] [Google Scholar]
- 13.Messenger JC, Ho KK, Young CH, et al. ; NCDR Science and Quality Oversight Committee Data Quality Workgroup . The National Cardiovascular Data Registry (NCDR) data quality brief: the NCDR Data Quality Program in 2012. J Am Coll Cardiol. 2012;60(16):1484-1488. doi: 10.1016/j.jacc.2012.07.020 [DOI] [PubMed] [Google Scholar]
- 14.Peterson ED, Dai D, DeLong ER, et al. ; NCDR Registry Participants . Contemporary mortality risk prediction for percutaneous coronary intervention: results from 588,398 procedures in the National Cardiovascular Data Registry. J Am Coll Cardiol. 2010;55(18):1923-1932. doi: 10.1016/j.jacc.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629-638. doi: 10.1016/S0140-6736(13)60141-5 [DOI] [PubMed] [Google Scholar]
- 16.Athappan G, Patvardhan E, Tuzcu ME, Ellis S, Whitlow P, Kapadia SR. Left main coronary artery stenosis: a meta-analysis of drug-eluting stents versus coronary artery bypass grafting. JACC Cardiovasc Interv. 2013;6(12):1219-1230. doi: 10.1016/j.jcin.2013.07.008 [DOI] [PubMed] [Google Scholar]
- 17.Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 2015;10(9):1024-1094. doi: 10.4244/EIJY14M09_01 [DOI] [PubMed] [Google Scholar]
- 18.Fortier JH, Shaw RE, Glineur D, Grau JB. Percutaneous coronary intervention versus coronary artery bypass grafting: where are we after NOBLE and EXCEL? Curr Opin Cardiol. 2017;32(6):699-706. doi: 10.1097/HCO.0000000000000450 [DOI] [PubMed] [Google Scholar]
- 19.Holmes AA, Bangalore S. PCI or CABG for severe unprotected left main coronary artery disease: making sense of the NOBLE and EXCEL trials. J Thorac Dis. 2017;9(5):E451-E456. doi: 10.21037/jtd.2017.04.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatt DL. CABG the clear choice for patients with diabetes and multivessel disease. Lancet. 2018;391(10124):913-914. doi: 10.1016/S0140-6736(18)30424-0 [DOI] [PubMed] [Google Scholar]
- 21.Giannoglou GD, Antoniadis AP, Chatzizisis YS, Damvopoulou E, Parcharidis GE, Louridas GE. Prevalence of narrowing ≥50% of the left main coronary artery among 17,300 patients having coronary angiography. Am J Cardiol. 2006;98(9):1202-1205. doi: 10.1016/j.amjcard.2006.05.052 [DOI] [PubMed] [Google Scholar]
- 22.Ragosta M, Dee S, Sarembock IJ, Lipson LC, Gimple LW, Powers ER. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv. 2006;68(3):357-362. doi: 10.1002/ccd.20709 [DOI] [PubMed] [Google Scholar]
- 23.Riley RF, Don CW, Powell W, Maynard C, Dean LS. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes. 2011;4(2):193-197. doi: 10.1161/CIRCOUTCOMES.110.958744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen SL, Zhang JJ, Han Y, et al. Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V randomized trial. J Am Coll Cardiol. 2017;70(21):2605-2617. doi: 10.1016/j.jacc.2017.09.1066 [DOI] [PubMed] [Google Scholar]
- 25.Strom JB, Wimmer NJ, Wasfy JH, Kennedy K, Yeh RW. Association between operator procedure volume and patient outcomes in percutaneous coronary intervention: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2014;7(4):560-566. doi: 10.1161/CIRCOUTCOMES.114.000884 [DOI] [PubMed] [Google Scholar]
- 26.Fanaroff AC, Zakroysky P, Dai D, et al. Outcomes of PCI in relation to procedural characteristics and operator volumes in the United States. J Am Coll Cardiol. 2017;69(24):2913-2924. doi: 10.1016/j.jacc.2017.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Demographic and clinical characteristics of patients undergoing ULM PCI over time.
eTable 2. Procedural characteristics of ULM PCI over time.
eTable 3. Clinical outcomes of patients undergoing ULM PCI over time.
eTable 4. Clinical outcomes of patients undergoing ULM PCI stratified by tertile of operator and institutional annual PCI volumes and by tertile of institutional use of mechanical circulatory support.
eTable 5. Baseline characteristics and outcomes in patients who underwent left main PCI in the NCDR, EXCEL trial, and NOBLE trial.
eFigure 1. Cohort creation.
eFigure 2. Factors associated with increased rates of major adverse cardiac events after multivariate adjustment.