Key Points
Question
After successful initial nonoperative treatment of periappendicular abscess, is interval appendectomy necessary, or can patients be treated using follow-up examinations with magnetic resonance imaging?
Findings
This randomized clinical trial of 60 patients had to be prematurely terminated owing to ethical concerns after an interim analysis revealed a high incidence of neoplasms, resulting in an underpowered trial unable to draw firm conclusions on the primary end point of treatment success at 1 year after the intervention. The neoplasm rate of the whole study population was 20%; the rate in patients older than 40 years was 29%.
Meaning
The neoplasm rate after periappendicular abscess in this small study population was high; if this rate is validated by future studies, it would argue for routine interval appendectomy in this context.
This randomized clinical trial assesses the safest procedures after initial successful nonoperative treatment of periappendicular abscess by comparing treatment success and morbidity in patients receiving interval appendectomy with patients receiving nonsurgical follow-up with magnetic resonance imaging.
Abstract
Importance
The step after conservative treatment of periappendicular abscess arouses controversy, ranging from recommendations to abandon interval appendectomy based on low recurrence rates of the precipitating diagnosis to performing routine interval appendectomy owing to novel findings of increased neoplasm risk at interval appendectomy. To our knowledge, there are no randomized clinical trials with sufficient patient numbers comparing these treatments.
Objective
To compare interval appendectomy and follow-up with magnetic resonance imaging after initial successful nonoperative treatment of periappendicular abscess.
Design, Setting, and Participants
The Peri–Appendicitis Acuta randomized clinical trial was a multicenter, noninferiority trial conducted in 5 hospitals in Finland. All patients between age 18 and 60 years with periappendicular abscess diagnosed by computed tomography and successful initial nonoperative treatment from January 2013 to April 2016 were included. Data analysis occurred from April 2016 to September 2017.
Interventions
Patients were randomized either to interval appendectomy or follow-up with magnetic resonance imaging; all patients underwent colonoscopy.
Main Outcomes and Measures
The primary end point was treatment success, defined as an absence of postoperative morbidity in the appendectomy group and appendicitis recurrence in the follow-up group. Secondary predefined end points included neoplasm incidence, inflammatory bowel disease, length of hospital stay, and days of sick leave.
Results
A total of 60 patients were included (36 men [60%]; median [interquartile range] age: interval appendectomy group, 49 [18-60] years; follow-up group, 47 [22-61] years). An interim analysis in April 2016 showed a high rate of neoplasm (10 of 60 [17%]), with all neoplasms in patients older than 40 years. The trial was prematurely terminated owing to ethical concerns. Two more neoplasms were diagnosed after study termination, resulting in an overall neoplasm incidence of 20% (12 of 60). On study termination, the overall morbidity rate of interval appendectomy was 10% (3 of 30), and 10 of the patients in the follow-up group (33%) had undergone appendectomy.
Conclusions and Relevance
The neoplasm rate after periappendicular abscess in this small study population was high, especially in patients older than 40 years. If this considerable rate of neoplasms after periappendicular abscess is validated by future studies, it would argue for routine interval appendectomy in this setting.
Trial Registration
ClinicalTrials.gov identifier: NCT03013686
Introduction
Complicated and uncomplicated cases of appendicitis follow different epidemiological patterns, which suggest that there are different pathophysiological processes behind these 2 different forms of appendicitis.1,2 In 3% to 10% of patients, complicated acute appendicitis involves the formation of a closed, circumscribed periappendicular abscess at presentation.3,4 The clinically established practice of antibiotic therapy and drainage, if necessary, has been shown to be safe and effective, allowing the acute inflammatory process to subside in more than 90% of cases without surgery.3,5
The need of subsequent interval appendectomy in complicated acute appendicitis presenting with a periappendicular abscess has recently been questioned, with appendicitis recurrence risk varying between 5% to 26%.3,6,7,8,9 Most of the recurrences happen within 6 months, and after the first year, the risk further decreases.3,7,8,9 Early appendectomy in the acute phase has been advocated for in adult patients because it is associated with fewer readmissions and additional interventions compared with nonoperative treatment,10 but in a pediatric population, no differences between these 2 strategies was found.11 Both early and delayed approaches to appendectomy offer the advantage of a definitive histopathological diagnosis. The reported risk of an underlying malignant neoplasm in acute appendicitis is very low, varying between 0.7% and 3%.3,9,12,13 However, recent studies have reported alarming appendiceal neoplasm rates detected during interval appendectomy in patients with previous periappendicular abscess, especially in patients older than 40 years.13,14,15,16
According to 2 systematic reviews and meta-analysis,3,5 initial nonoperative management is superior, with decreased complication and reoperation rates compared with emergency appendectomy. However, there is still major controversy regarding the necessity of an interval appendectomy after successful nonoperative treatment of periappendicular abscess.3,5 To our knowledge, there is only 1 published randomized clinical trial comparing nonsurgical follow-up with interval appendectomy, with a small number of patients (N = 60) and an additional third intervention group of patients who received delayed appendectomy during the initial hospitalization phase of the study.17
The aim of this randomized clinical trial, Peri–Appendicitis Acuta (PeriAPPAC), was to test the hypothesis that an interval appendectomy is unnecessary after initial successful nonoperative treatment of a periappendicular abscess, by comparing routine interval appendectomy to follow-up with magnetic resonance imaging (MRI) at 3 months after the initial treatment.
Methods
Design and Ethics
This multicenter noninferiority randomized clinical trial was designed to test the hypothesis that an interval appendectomy is not necessary after initial successful treatment of periappendicular abscess. The trial was conducted in 5 Finnish hospitals (in Turku, Oulu, and Kuopio, and Tampere University Hospitals and Seinäjoki Central Hospital).
The study was approved by the Ethical Committee of Turku University Hospital district and conducted in accordance with the Declaration of Helsinki. All participating patients gave written informed consent. Amendments to the protocol could only be initiated by the coordinating center and the primary investigator. No independent data monitoring committee was established and no interim analysis was stated at study initiation. The interim analysis performed in April 2016 was prompted by clinical suspicion of increased tumor risk in the study population.
Participants
Patients between 18 and 60 years of age who were admitted to the emergency department with a computed tomography (CT) or MRI examination and diagnosed with periappendicular abscess were evaluated for study enrollment after completion of initial nonoperative treatment with antibiotic therapy and abscess drainage, if needed. The exclusion criteria included suspicion of tumor on diagnostic CT or MRI imaging, unsuccessful initial nonoperative treatment, an age younger than 18 years or older than 60 years, pregnancy or lactation, contraindications to CT imaging (eg, allergy to contrast media or iodine, renal insufficiency, or metformin medication), inability to give informed consent, a severe systemic illness, or a previous episode of acute appendicitis treated conservatively with antibiotics.
Randomization
A biostatistician (S.H.) created a computer-generated randomization list separately for each participating center. The randomization was performed in a 1:1 allocation ratio. A research assistant sealed the randomization group into numbered opaque envelopes, and neither the biostatistician nor the research assistant was involved in patient care. After confirmation of patient eligibility and signed informed consent, the research surgeon opened an envelope in numerical order to randomize the patient either to interval appendectomy or to follow-up examinations with MRI.
Interventions
Both interventions were scheduled at approximately 3 months after randomization. Prior to both interventions, a colonoscopy was performed for all patients to rule out a cecal tumor.
Interval Appendectomy
Patients randomized to operative treatment were scheduled to undergo a laparoscopic appendectomy. Conversion to open appendectomy was performed if necessary. Standard antibiotic prophylaxis of 1.5 g of cefuroxime and 500 mg of metronidazole was administered intravenously 30 minutes before incision. All of the removed appendixes underwent histopathological examination.
Follow-up With MRI Imaging
Patients randomized to follow-up examinations underwent an abdominal MRI according to the imaging protocol of the participating hospital. In the case of suspected recurrence or persistent symptoms, the patients were scheduled for either emergency or elective appendectomy, depending on the patient’s clinical condition.
Data Collection
Patient outcomes (initial nonoperative treatment including antibiotic therapy and possible drainage, C-reactive protein levels, leukocyte counts, length of hospital stay, and days of sick leave) were assessed during the initial hospital stay. The parameters for treatment interventions were collected either at the time of the appendectomy or after MRI. Follow-up data (complications, abdominal symptoms, and appendicitis recurrence) was collected by telephone interview at 1 week after the interval appendectomy procedure in the relevant group and at 2 months and 1 year after the intervention in both groups. For patients who could not be reached for follow-up, a search of hospital records in each research hospital district was conducted to retrieve information about a possible appendectomy procedure by patients in the MRI follow-up group or any other subsequent hospital visits by patients in either study group.
Primary and Secondary Outcomes
The primary end point was treatment success evaluated at 1 year after the intervention. In the interval appendectomy group, treatment success was defined as both successful appendectomy and uncomplicated recovery (as defined by an overall absence of postoperative morbidity) and in the follow-up group as an absence of recurrent acute appendicitis during the follow-up period. The predefined secondary end points included possible appendiceal or colonic tumors, possible inflammatory bowel disease diagnosis (eg, ulcerative colitis, Crohn disease), the hospital length of stay, and days of sick leave.
Sample Size
The sample size calculation for the trial was based on the primary outcome, assuming that all patients randomized to the surgical group would undergo a successful interval appendectomy procedure. For computations, the success rate for surgery was assumed to be 99%. The findings of prior studies indicate recurrence rates of acute appendicitis of 5% to 20% for follow-up, resulting in anticipated success rate of approximately 85% in the follow-up group. Because the noninferiority element of this trial was evaluated using the lower limit of 95% CI for treatment efficacy, we used a 75% success rate in the follow-up group as a marginal value and a 24% (95% CI, 99%-75%) noninferiority margin in the sample size calculations. We estimated that a total of 110 patients (55 patients per group) would yield a power of 0.90 (1-β) to establish whether follow-up was noninferior to surgery, with a significance level α of .05. With an assumption of an approximate 10% drop-out rate, our aim was to enroll 122 patients. Sample size calculations were performed using the Power procedure in SAS Systems for Windows version 9.3 (SAS Institute Inc).
Statistical Methods
Summary measurements were presented as means with SD or as median with interquartile ranges (IQRs; 25th and 75th percentiles). The t test (continuous variables) and the Pearson χ2 test or Fisher exact test (categorical variables) were used for between-group comparisons. Two-tailed P values less than .05 were considered statistically significant. All analyses were performed according to intention- to-treat principle. We used SPSS for Windows version 24.0 (IBM) for analyses. The full trial protocol and statistical analysis plan can be found in the eMethods in Supplement 1.
Results
During the follow-up period, a clinical suspicion of increased tumor risk in the study population prompted an interim analysis not originally included in the study plan. This was performed in April 2016. At the interim analysis, there were 60 randomized patients (49.2% of the original target of 122 patients), and the trial was prematurely terminated owing to ethical concerns based on high tumor incidence.
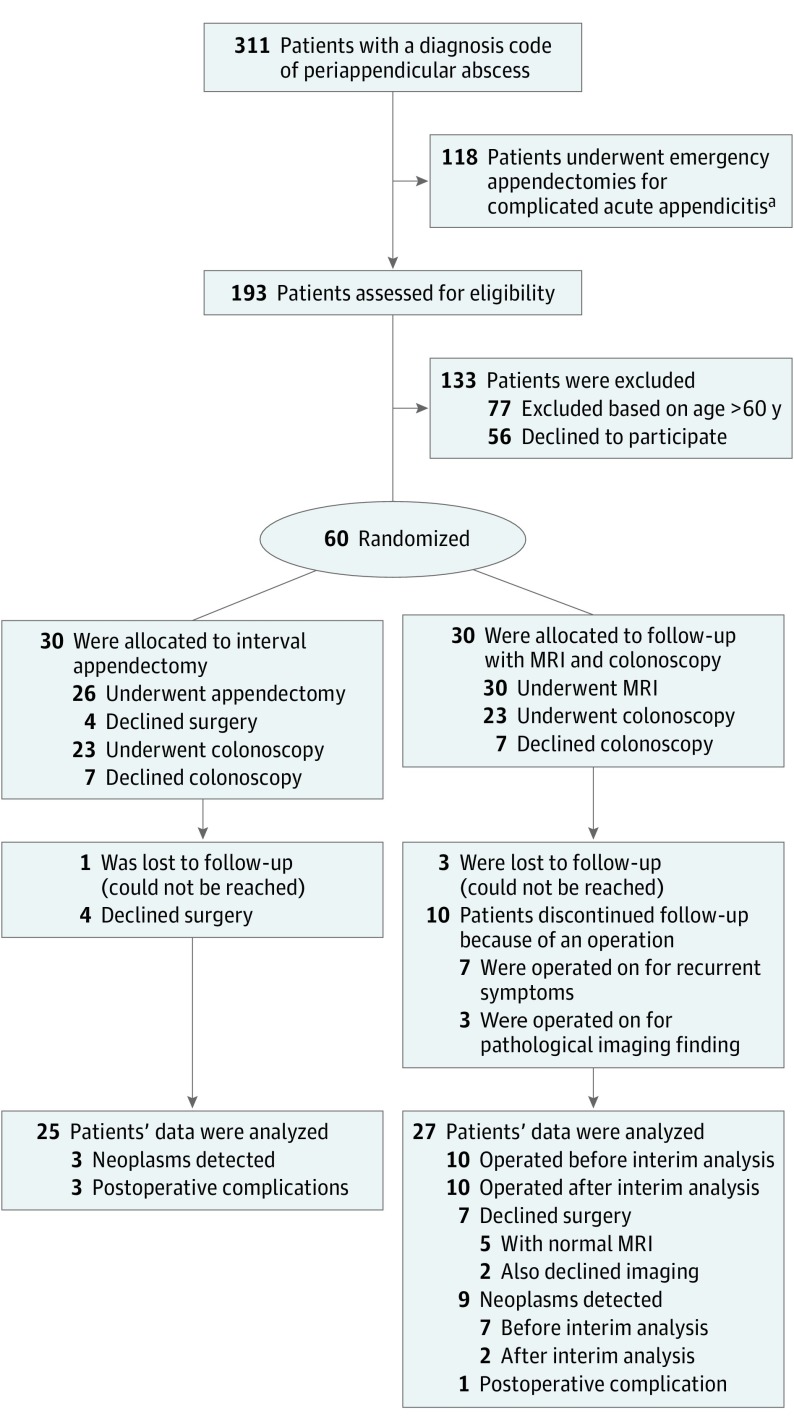
These 60 patients, each of whom had a CT-confirmed periappendicular abscess and a successful initial nonoperative treatment, were randomized from January 2013 until February 2016, with 30 patients in each treatment group. The trial flowchart is presented in the Figure. According to hospital discharge registry diagnosis codes, a total of 396 patients were treated at the participating hospitals for a periappendicular abscess during the study period, and 311 of these patients (78.5%) were evaluated for study enrollment. However, 118 of 311 patients (37.9%) underwent an emergency operation owing to actually being diagnosed with perforated appendicitis with minor fluid collection on imaging or a clinical diagnosis of complicated acute appendicitis without preoperative imaging. (In other words, in these patients, the emergency department diagnosis of periappendicular abscess was inaccurate.) There were altogether 193 patients with CT-diagnosed periappendicular abscess assessed for eligibility.
Figure. Flowchart of Trial Participants.
aIndicates that the 118 patients in whom a diagnosis of periappendicular abcess was inaccurate. MRI indicates magnetic resonance imaging.
The patient baseline characteristics are presented in Table 1. Of the 60 enrolled patients (31.1% of the 193 assessed), 36 were men (60%). The median (IQR) age for the interval appendectomy group was 49 (18-60) years; for the follow-up group, it was 47 (22-61) years.
Table 1. Baseline Characteristics of the Trial Patients.
| Characteristic | Median (Range) | P Value | |
|---|---|---|---|
| Interval Appendectomy (n = 30) | Follow-up With Magnetic Resonance Imaging and Colonoscopy (n = 30) | ||
| Sex, No. (%) | |||
| Male | 16 (53.3) | 20 (66.7) | .43 |
| Female | 14 (46.7) | 10 (33.3) | |
| Age, y | 49 (18-60) | 47 (22-61) | .81 |
| Duration of symptoms, d | 7 (2-21) | 7 (2-9) | .07 |
| C-reactive protein, mg/L | 145 (30-271) | 166 (55-361) | .09 |
| White blood cell count per μL | 11 700 (6100-20 400) | 14 100 (8800-24 400) | .02 |
| Size of abscess, cm | 5.0 (2.0-9.0) | 5.1 (2.0-11.0) | .57 |
| Drainage of abscess, No. (%) | |||
| Yes | 6 (20.0) | 7 (23.3) | >.99 |
| No | 24 (80.0) | 23 (76.7) | |
| Duration of antibiotic treatment, d | 11.5 (4-23) | 12.0 (7-26) | .50 |
SI conversion factors: To convert C-reactive protein to nmol/L, multiply by 9.524; to convert white blood cells to number ×109/L, multiply by 0.001.
Primary End Points
At interim analysis, the treatment efficacy in the interval appendectomy group based on the sample size calculation definition was 26 of 30 patients (87%) because 4 asymptomatic patients declined to undergo interval appendectomy as planned. According to the primary end point definition for treatment success in the interval appendectomy group and taking into account the postoperative morbidity, the treatment success was 23 of 30 (77%) because 3 patients (10%) had postoperative complications. The treatment efficacy in the follow-up group was 77% because 7 of the 30 patients in the follow-up group (23%) experienced recurrent symptoms. The difference between the treatment groups concerning treatment success was 0% (95% CI, −21% to 21%).
In the interval appendectomy group, 23 of the 30 patients (77%) were operated on laparoscopically, with 3 conversions to laparotomy owing to technical difficulties, and all but 1 procedure (an ileocecal resection) were appendectomies. Four asymptomatic patients declined surgery, including 2 after colonoscopy, but the other 2 patients also declined colonoscopy and none of these 4 asymptomatic patients underwent follow-up imaging at 1-year follow-up. If they remain asymptomatic, these patients are scheduled to undergo the follow-up examination scheduled for patients in the follow-up group (at 3, 5, and 10 years). Altogether, 23 patients in the interval appendectomy group underwent colonoscopy, and colon adenomas outside the cecum were detected in 3 patients (including 2 low-grade dysplasias and 1 high-grade dysplasia). Complications associated with interval appendectomy consisted of 1 superficial wound infection, 1 incisional hernia, and 1 deep surgical site infection requiring radiological drainage. The patient with the deep infection also had right-sided hydronephrosis, which subsided without intervention. The patient with the incisional hernia is currently awaiting a hernioplasty procedure.
In the follow-up group, 10 patients (33%) had undergone appendectomy at the interim analysis. Seven patients (23%) were operated on for recurrent appendicitis. Five patients underwent an emergency operation, and 2 patients underwent elective appendectomy. In 4 of 5 (80%) of these emergency appendectomies, histopathological examinations revealed both acute appendicitis and a neoplasm; in the other patient, it revealed acute appendicitis. The 2 patients with elective appendectomies had reactive changes and subacute appendicitis on histopathological examination.
Three of 10 patients with appendectomy at interim analysis were operated for tumor suspicion at follow-up imaging. On histopathological examination, 1 of these patients had chronic appendicitis and 1 had a sessile serrated adenoma. The third patient unintentionally underwent a CT instead of MRI at follow-up, and she was diagnosed with a cecal tumor with metastases in both lungs. Her primary CT at periappendicular abscess diagnosis were retrospectively evaluated, and the pulmonary metastases in the right lung were already visible in the CT taken during the first hospital stay 3 months earlier, indicating disseminated disease already at the study enrollment. The cecal tumor was not visible in the primary CT scan owing to the periappendicular abscess. This patient underwent a palliative right hemicolectomy after initial chemotherapy; in addition to the cecal adenocarcinoma, a sessile serrated appendiceal adenoma was diagnosed on histopathological examination. In the follow-up group, a total of 23 patients underwent a colonoscopy, and hyperplastic polyps were detected in 1 patient. Characteristics of all the patients in the follow-up group who had been operated on are presented in detail in Table 2.
Table 2. Operative Interventions in the Group Receiving Follow-up Treatment and Magnetic Resonance Imaging.
| Patient Sex/Age, y | Reason for Intervention | Intervention | Time to Intervention, d | Histological Findings |
|---|---|---|---|---|
| M/59 | Recurrent acute symptoms | Emergency operation | 183 | Acute appendicitis |
| M/59 | Recurrent acute symptoms | Emergency operation | 329 | Periappendicular abscess and adenocarcinoma |
| M/46 | Recurrent acute symptoms | Interval appendectomy after conservative treatment | 303 | Reactive changes |
| M/47 | Recurrent acute symptoms | Interval appendectomy after conservative treatment | 258 | Subacute appendicitis |
| M/59 | Recurrent acute symptoms | Emergency operation | 18 | Periappendicular abscess and LAMN |
| M/61 | Recurrent acute symptoms | Emergency operation | 330 | Appendicitis and mucinous cystadenoma of the appendix |
| M/55 | Recurrent acute symptoms | Emergency operation | 189 | Appendicitis and goblet cell carcinoid tumor |
| F/58 | Tumor suspicion on follow-up MRI | Elective operation | 199 | Sessile serrated adenoma |
| F/53 | Metastasized tumor on follow-up MRI | Palliative operation after oncologic treatment | 332 | Cecal adenocarcinoma and sessile serrated adenoma of the appendix |
| F/53 | Tumor suspicion on follow-up MRI | Elective operation | 96 | Chronic appendicitis |
Abbreviations: LAMN, low-grade appendiceal mucinous neoplasm; MRI, magnetic resonance imaging.
Secondary End Points
At interim analysis, the incidence of neoplasms in the whole study population was 17% (10 of 60) and the neoplasm rate in patients older than 40 years was 24% (10 of 41). All neoplasms were diagnosed in patients older than 40 years, with a median age of 53 years (range, 40-61 years). At study termination, all the patients randomized to the follow-up group were reevaluated, and laparoscopic appendectomy was recommended to all, with a special emphasis on patients older than 40 years. Of the 20 patients in the follow-up group, 3 were lost to follow-up, leaving 17 patients for reevaluation. Ten of these 17 patients (59%) underwent surgery, resulting in a total of 20 patients in the follow-up group (67%) undergoing surgery. In these procedures, 2 more neoplasms (low-grade appendiceal mucinous neoplasms [LAMNs]) were diagnosed; these 2 patients have been asymptomatic at the follow-up examination. The characteristics of the patients operated on in the follow-up group after interim analysis are shown in Table 3.
Table 3. Operative Interventions in the Group Receiving Follow-up Treatment and Magnetic Resonance Imaging After Interim Analysis.
| Patient Sex/Age, y | Time to Appendectomy, mo | Histological Findings |
|---|---|---|
| M/37 | 45 | Normal |
| M/38 | 35 | Acute appendicitis |
| M/43 | 18 | Fibrosis |
| M/39 | 10 | Fibrosis |
| M/46 | 10 | Chronic inflammation |
| M/56 | 12 | Normal |
| M/61 | 16 | LAMN |
| M/26 | 15 | Normal |
| F/56 | 11 | Normal |
| F/42 | 5 | LAMN |
Abbreviation: LAMN, low-grade appendiceal mucinous neoplasm.
After study termination and reevaluation of the follow-up group, the overall incidence of neoplasms in the study population was 12 of 60 (20%), and the rate of neoplasms in patients older than 40 years of age was 12 of 41 (29%). The characteristics of the all patients with neoplasms are shown in detail in Table 4. The rate of neoplasms in all patients who were operated on was 12 of 46 (26%). In patients older than 40 years who were operated on, the rate was 12 of 34 (35%), because all neoplasms were diagnosed in patients older than 40 years.
Table 4. Neoplasms Found in the Study Population.
| Patient Sex/Age, y | Reason for Intervention | Time to Intervention, d | Intervention | Histological Findings | Time to Secondary Intervention, d | Secondary Intervention |
|---|---|---|---|---|---|---|
| F/56 | Allocated intervention | 90 | Appendectomy | LAMN and pseudomyxoma peritonei | 156 | Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy |
| M/47 | Allocated intervention | 120 | Appendectomy | LAMN | NA | Surveillance |
| M/59 | Allocated intervention | 134 | Appendectomy | Sessile serrated adenoma | NA | Surveillance |
| M/59 | Recurrent symptoms | 329 | Ileocecal resection | Adenocarcinoma of the appendix | 378 | Right hemicolectomy |
| M/59 | Recurrent symptoms | 18 | Appendectomy | LAMN | 98 | Ileocecal resection |
| M/61 | Recurrent symptoms | 330 | Appendectomy | Mucinous cystadenoma | NA | Surveillance |
| M/55 | Recurrent symptoms | 189 | Appendectomy | Goblet cell carcinoid | 252 | Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy |
| F/58 | MRI tumor suspicion | 199 | Appendectomy | Sessile serrated adenoma | NA | Surveillance |
| F/53 | CT tumor suspicion | 171 | Chemotherapy | Cecal adenocarcinoma and sessile serrated appendiceal adenoma | 332 | Right hemicolectomy (palliative) |
| M/61 | Recommended | 429 | Appendectomy | LAMN | NA | Surveillance |
| F/41 | Recommended | 142 | Appendectomy | LAMN | NA | Surveillance |
Abbreviations: CT, computed tomography; LAMN, low-grade appendiceal mucinous neoplasm; MRI, magnetic resonance imaging; NA, not applicable.
Five asymptomatic patients with normal abdominal MRI results who had been in the follow-up group, including 2 older than 40 years, refused appendectomy, even though the risk of neoplasm was thoroughly explained. Four of 5 patients (80%) underwent a follow-up colonoscopy with normal findings, but the fifth, a 22-year-old patient, also refused the colonoscopy. Two asymptomatic patients (both younger than 40 years) refused any further interventions, including MRI examinations.
In the patients operated on after the interim analysis, there was 1 infection of a superficial wound treated with antibiotics. The overall morbidity rate in all appendectomies performed (26 in the interval appendectomy group and 20 in the follow-up group) was 4 of 46 (9%). There was no intervention-associated mortality. In addition, no patients were diagnosed with inflammatory bowel disease. The median (range) hospital length of stay for initial treatment of periappendicular abscess was 3 days (1-17) days. After initial treatment, the median (range) hospital stay for patients for the 17 patients undergoing surgery who were in the group that had received interval appendectomy procedures was 1 (1-8) days and that of group that had received follow-up was 1 (1-6) days.
Discussion
The hypothesis of this Peri-APPAC randomized trial was that an interval appendectomy is not necessary after initial successful nonoperative treatment of a periappendicular abscess. However, during trial enrollment, the high incidence of appendiceal tumors in the study population alarmed the researchers, prompting an interim analysis to be performed in April 2016, and the trial was ceased on February 14, 2016, to complete this analysis. Based on the results, including a 17% rate of appendiceal tumors in the study population, the trial was prematurely terminated based on ethical concerns. All the patients in the follow-up group were reevaluated, and surgery was offered and recommended to these patients. After this assessment and additional appendectomies, 2 more tumors were diagnosed, resulting in a rate of neoplasms of 20% in the whole study group. All cases were diagnosed in patients older than 40 years, and the neoplasm rate in this age group was 29%.
Based on the premature termination of this trial, we failed to reach the intended sample size, which left our study underpowered to draw conclusions on the initial primary end point. However, the predefined secondary end point of appendiceal tumor rate strongly overrides the primary end point in clinical significance and ethical surgical practice. Based on high appendiceal tumor rate in patients older than 40 years, the study hypothesis of avoiding interval appendectomy in this patient group should be approached with extreme caution. The rate of appendiceal neoplasm in patients older than 40 years should be further evaluated in prospective patient cohorts undergoing interval appendectomy because interval appendectomy is generally well tolerated and obliterates the risk of missing a possible tumor.
Neoplasm rates associated to acute appendicitis are very low, varying between 0.7% to 1.7% in large series of appendectomies, including patients with uncomplicated and complicated acute appendicitis.12,18 Increasing evidence from randomized clinical trials suggests that most patients with uncomplicated acute appendicitis can be treated safely with antibiotics with low tumor rates, avoiding unnecessary surgery and resulting in decreased morbidity and cost savings.19,20,21 The essential factor is to acknowledge the 2 different forms to acute appendicitis; the differential diagnosis between complicated and uncomplicated acute appendicitis is of vital clinical importance. Appendicitis is a similar condition with acute diverticulitis, which can also be graded as uncomplicated and complicated, with an increased risk of colon cancer up to 11.4% in patients with acute diverticulitis and an abscess on CT scan.22
There are contradictory results regarding the rate of appendiceal tumors in patients with complicated acute appendicitis, and this may be based on the varying definitions of complicated appendicitis. According to a systematic review,3,19 the rate of malignant tumors in patients who were diagnosed with acute appendicitis and an inflammatory appendiceal mass (1.1%) was similar to the rates of tumor in patients with uncomplicated acute appendicitis cases (1.5%). In a recent systematic review of retrospective cohort studies involving 13 244 patients with acute appendicitis, the overall appendiceal tumor rate was 1% after appendectomy, but in patients presenting with appendiceal inflammatory mass, the neoplasm rate varied from 10% to 29%.13 Alarming rates of appendiceal neoplasms at interval appendectomy procedures after initial conservative treatment of periappendicular abscess or phlegmon have also been reported in retrospective patient case series.14,15,16,23
The proportion of mucinous neoplasms (LAMN or mucinous adenocarcinoma) varied between 20% and 100% in the analyzed retrospective studies.13 This is in accordance with the current trial because 42% of all neoplasms in this study were LAMNs. All tumors associated with periappendicular abscess always present with tumor perforation, creating an extraluminal abscess that carries an inevitable risk of peritoneal dissemination. This is strongly contradictory to promoting operative treatment of periappendicular abscess in the acute phase of the disease10 because this would transform a restricted tumor perforation to an unlimited peritoneal spreading, countering the principles of the oncologic approach to cancer surgery. Specifically, the perforation of LAMN might predispose to the development of pseudomyxoma peritonei.24,25,26 In a report of 22 patients with a LAMN detected incidentally in an appendectomy, the rate of pseudomyxoma peritonei was 23%24; in 80% of the patients with peritoneal dissemination, CT results were negative and occult peritoneal disease was identified only by laparoscopic examination.24 In this study population, 2 cases of appendiceal malignant conditions were diagnosed only after recurrent symptoms at the time of appendectomy, despite these patients undergoing both MRI and colonoscopy examinations. This is in line with the previous results24 and further supports the need for interval appendectomy, regardless of normal imaging findings and the absence of symptoms.
The strong elements of this study include the randomized multicenter nature, the CT scan–confirmed diagnosis and the follow-up imaging with MRI. The premature termination of the study can also be evaluated as a strength; the secondary end point of an alarmingly high appendiceal neoplasm rate associated with periappendicular abscess is of vital clinical importance.
Based on the study findings, we believe that appendectomy in the acute phase should be approached with caution, at least in patients older than 40 years, and interval appendectomy should be resourced with adequate expertise to determine the correct surgical procedure required to avoid unnecessary secondary interventions. In addition, possible future trials that include a follow-up arm after periappendicular abscess should consider excluding patients older than 40 years based on the high risk for appendiceal neoplasm in this study group. However, follow-up after periappendicular abscess may still be worth exploring for asymptomatic patients who are younger than 40 years.
Limitations
This study has several limitations. The major limitation is the small number of patients, which was the result of premature termination of the study after interim analysis based on clinical suspicion. In addition, no interim analysis was originally planned, which was a weakness in the trial protocol. Because the enrollment fell far from the sample size calculation, this ethically inevitable premature termination resulted in an underpowered trial and thus inconclusiveness of the trial hypothesis and primary end point.
Other limitations include the recruitment period, which was longer than anticipated, and the suboptimal recording of the data on the excluded patients; all potentially eligible patients were not evaluated for the study. These limitations were based on the acute care surgery setting of the multicenter trial, which had busy acute care surgery wards and recruitment by senior research surgeons with limited time availability.
Another limitation is the lack of standardization of the follow-up MRI protocols between the study hospitals. However, this most likely had very limited effect because these imaging protocols in Finnish tertiary hospitals are very similar.
Conclusions
In conclusion, the overall rate of neoplasms after a periappendicular abscess in this study was high. Until further information is available from future studies, we suggest careful evaluation of interval appendectomy, at least in patients older than 40 years. If this high rate of neoplasms after periappendicular abscess is validated by future studies, it would argue for routine interval appendectomy in this context.
eMethods. Study Protocol and Statistical Analysis Plan.
Data Sharing Statement.
References
- 1.Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg. 2011;146(3):308-314. doi: 10.1001/archsurg.2011.2 [DOI] [PubMed] [Google Scholar]
- 2.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886-892. doi: 10.1097/01.sla.0000256391.05233.aa [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246(5):741-748. doi: 10.1097/SLA.0b013e31811f3f9f [DOI] [PubMed] [Google Scholar]
- 4.Meshikhes AW. Management of appendiceal mass: controversial issues revisited. J Gastrointest Surg. 2008;12(4):767-775. doi: 10.1007/s11605-007-0399-1 [DOI] [PubMed] [Google Scholar]
- 5.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010;147(6):818-829. doi: 10.1016/j.surg.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 6.Anderson JE, Bickler SW, Chang DC, Talamini MA. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. World J Surg. 2012;36(12):2787-2794. doi: 10.1007/s00268-012-1749-z [DOI] [PubMed] [Google Scholar]
- 7.Darwazeh G, Cunningham SC, Kowdley GC. A systematic review of perforated appendicitis and phlegmon: interval appendectomy or wait-and-see? Am Surg. 2016;82(1):11-15. [PubMed] [Google Scholar]
- 8.Kaminski A, Liu IL, Applebaum H, Lee SL, Haigh PI. Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg. 2005;140(9):897-901. doi: 10.1001/archsurg.140.9.897 [DOI] [PubMed] [Google Scholar]
- 9.Lai HW, Loong CC, Chiu JH, Chau GY, Wu CW, Lui WY. Interval appendectomy after conservative treatment of an appendiceal mass. World J Surg. 2006;30(3):352-357. doi: 10.1007/s00268-005-0128-4 [DOI] [PubMed] [Google Scholar]
- 10.Mentula P, Sammalkorpi H, Leppäniemi A. Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? a randomized controlled trial. Ann Surg. 2015;262(2):237-242. doi: 10.1097/SLA.0000000000001200 [DOI] [PubMed] [Google Scholar]
- 11.St Peter SD, Aguayo P, Fraser JD, et al. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010;45(1):236-240. doi: 10.1016/j.jpedsurg.2009.10.039 [DOI] [PubMed] [Google Scholar]
- 12.Charfi S, Sellami A, Affes A, Yaïch K, Mzali R, Boudawara TS. Histopathological findings in appendectomy specimens: a study of 24,697 cases. Int J Colorectal Dis. 2014;29(8):1009-1012. doi: 10.1007/s00384-014-1934-7 [DOI] [PubMed] [Google Scholar]
- 13.Teixeira FJR Jr, Couto Netto SDD, Akaishi EH, Utiyama EM, Menegozzo CAM, Rocha MC. Acute appendicitis, inflammatory appendiceal mass and the risk of a hidden malignant tumor: a systematic review of the literature. World J Emerg Surg. 2017;12:12. doi: 10.1186/s13017-017-0122-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carpenter SG, Chapital AB, Merritt MV, Johnson DJ. Increased risk of neoplasm in appendicitis treated with interval appendectomy: single-institution experience and literature review. Am Surg. 2012;78(3):339-343. [PubMed] [Google Scholar]
- 15.Furman MJ, Cahan M, Cohen P, Lambert LA. Increased risk of mucinous neoplasm of the appendix in adults undergoing interval appendectomy. JAMA Surg. 2013;148(8):703-706. doi: 10.1001/jamasurg.2013.1212 [DOI] [PubMed] [Google Scholar]
- 16.Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH. Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015;209(3):442-446. doi: 10.1016/j.amjsurg.2014.09.020 [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Jain S. Treatment of appendiceal mass: prospective, randomized clinical trial. Indian J Gastroenterol. 2004;23(5):165-167. [PubMed] [Google Scholar]
- 18.Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA. Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol. 2008;34(2):196-201. doi: 10.1016/j.ejso.2007.04.002 [DOI] [PubMed] [Google Scholar]
- 19.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348. doi: 10.1001/jama.2015.6154 [DOI] [PubMed] [Google Scholar]
- 20.Sippola S, Grönroos J, Tuominen R, et al. Economic evaluation of antibiotic therapy versus appendicectomy for the treatment of uncomplicated acute appendicitis from the APPAC randomized clinical trial. Br J Surg. 2017;104(10):1355-1361. doi: 10.1002/bjs.10575 [DOI] [PubMed] [Google Scholar]
- 21.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777):1573-1579. doi: 10.1016/S0140-6736(11)60410-8 [DOI] [PubMed] [Google Scholar]
- 22.Sallinen V, Mentula P, Leppäniemi A. Risk of colon cancer after computed tomography-diagnosed acute diverticulitis: is routine colonoscopy necessary? Surg Endosc. 2014;28(3):961-966. doi: 10.1007/s00464-013-3257-0 [DOI] [PubMed] [Google Scholar]
- 23.Lee WS, Choi ST, Lee JN, Kim KK, Park YH, Baek JH. A retrospective clinicopathological analysis of appendiceal tumors from 3,744 appendectomies: a single-institution study. Int J Colorectal Dis. 2011;26(5):617-621. doi: 10.1007/s00384-010-1124-1 [DOI] [PubMed] [Google Scholar]
- 24.Foster JM, Sleightholm RL, Wahlmeier S, Loggie B, Sharma P, Patel A. Early identification of DPAM in at-risk low-grade appendiceal mucinous neoplasm patients: a new approach to surveillance for peritoneal metastasis. World J Surg Oncol. 2016;14(1):243. doi: 10.1186/s12957-016-0996-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Honoré C, Caruso F, Dartigues P, et al. Strategies for preventing pseudomyxoma peritonei after resection of a mucinous neoplasm of the appendix. Anticancer Res. 2015;35(9):4943-4947. [PubMed] [Google Scholar]
- 26.Yantiss RK, Shia J, Klimstra DS, Hahn HP, Odze RD, Misdraji J. Prognostic significance of localized extra-appendiceal mucin deposition in appendiceal mucinous neoplasms. Am J Surg Pathol. 2009;33(2):248-255. doi: 10.1097/PAS.0b013e31817ec31e [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Study Protocol and Statistical Analysis Plan.
Data Sharing Statement.