Key Points
Question
Is routine screening and treatment for asymptomatic bacteriuria in patients undergoing orthopedic, cardiac, or vascular surgical procedures warranted?
Findings
In this national cohort study of 68 265 US veterans, preoperative asymptomatic bacteriuria was associated with higher rates of postoperative urine cultures with bacteriuria among patients who underwent cardiac, orthopedic, and vascular surgical procedures and with 30-day surgical-site infection in patients who had a cardiac surgical procedure. However, active antimicrobial therapy with activity against the uropathogen was not associated with improvement in any measurable postoperative clinical outcome.
Meaning
Findings from this study provide evidence against screening or treating preoperative asymptomatic bacteriuria.
Abstract
Importance
Limited data suggest that screening for asymptomatic bacteriuria (ASB) prior to nonurologic procedures is not useful. However, high-quality evidence to support consensus recommendations and influence clinical practice is lacking.
Objective
To characterize the association between detection and treatment of preoperative ASB and postoperative outcomes.
Design, Setting, and Participants
This retrospective cohort study involved patients, predominantly male veterans, who underwent surgical procedures in 109 US facilities within the US Department of Veterans Affairs health care system from October 1, 2008, to September 30, 2013. Participants included patients (n = 68 265) who had cardiac, orthopedic, or vascular surgical procedures. Each received a planned clinician review of complete medical records for antimicrobial prophylaxis as well as 30-day surgical-site infection (SSI) and urinary tract infection (UTI) outcomes, and each had a preoperative urine culture result available within the 30 days prior to the procedure. Data analysis was performed from December 2016 to August 2018.
Main Outcome and Measures
The primary outcome was the association between preoperative ASB and postoperative SSI. The secondary outcomes included postoperative UTI and the association between antimicrobial therapy for ASB and postoperative infectious outcomes.
Results
In total, 68 265 patients (65 664 [96.2%] were men and 2601 [3.8%] were women, with a mean [SD] age of 64.6 [9.2] years) were identified, and 17 611 (25.8%) were eligible for inclusion in the primary analysis. Preoperative urine cultures were performed in 17 749 (26.0%) patients, and the results were positive in 755 (4.3%), of which 617 (81.7%) were classified as ASB. With adjustments for age, American Society of Anesthesiologists class, smoking status, race/ethnicity, sex, and diabetes status, patients with or without ASB had similar odds of SSI (2.4% vs 1.6%; adjusted odds ratio [aOR], 1.58; 95% CI, 0.93-2.70; P = .08). Receipt of antimicrobial therapy with activity against the ASB organism was not associated with a reduced SSI risk (aOR, 1.01; 95% CI, 0.28-3.65; P = .99). Urinary tract infection occurred in 14 (3.3%) of 423 patients with ASB and 196 (1.5%) of 12 913 patients without ASB (aOR, 1.42; 95% CI, 0.80-2.49; P = .22). Treatment or prophylaxis for the ASB organism similarly was not associated with reduced odds of postoperative UTI (aOR 0.68; 95% CI, 0.20-2.30; P = .54). The ASB organisms matched a postoperative wound culture in 2 cases, both Staphylococcus aureus.
Conclusions and Relevance
The findings of this study suggest that receipt of antimicrobial therapy with activity against ASB organisms identified in preoperative urine cultures was not associated with reductions in the risk for postoperative infections, including UTI and SSI; such findings suggest there is evidence for discontinuing the practice of screening and treatment for preoperative ASB.
This study evaluates the association between the presence of asymptomatic bacteriuria before a surgical procedure and the risk of developing infections after the procedure among adults who undergo nonurologic operations.
Introduction
Asymptomatic bacteriuria (ASB) is associated with postoperative adverse events, including increases in surgical-site infection (SSI) and urinary tract infection (UTI), after nonurologic procedures.1,2 However, whether preoperative screening of urine cultures with antimicrobial therapy directed toward colonizing bacterial organisms improves clinical outcomes remains controversial.3 The 2018 update to the ASB guidelines by the Infectious Diseases Society of America recommends against this practice but without supporting high-quality evidence.4 Concern for bacterial translocation from the bladder with resultant contamination of the surgical site is high, particularly during procedures in which foreign material is implanted, such as orthopedic total joint replacement and cardiac valve replacement. In part because of the lack of concrete evidence supporting or refuting screening with directed treatment, clinical practice patterns vary widely, with some centers obtaining preoperative urine cultures as part of the standard of care.5,6,7
The associations between UTI and prosthetic joint infection after total joint replacement procedures were first described in the 1970s.1,8,9,10,11,12 More recently, a large observational study reported a 3-fold rise in prosthetic joint infections among patients with ASB.1 Of importance, Sousa et al1 also found that the SSIs were usually not caused by the organism identified in the preoperative urine cultures; the discordance between the uropathogen and the SSI pathogen suggests that ASB is a risk marker for SSI but is not part of the causal pathway.1 This premise is further supported by several small studies that found antimicrobial therapy directed toward the uropathogen in the preoperative period does not improve postoperative outcomes.1,13,14,15
Mayne et al16 highlighted the challenges of definitively answering whether screening for and treatment of ASB can positively affect postoperative clinical outcomes. They estimated that “a trial comparing screening and treatment of ASB with no treatment would require at least 50,000 patients in each arm to detect a difference in infection risk of 0.15% and is, therefore, in practice, impossible. Bigger and better observational research is still possible, however, and should be a priority.”16(p1) Thus, we sought to use a large, multicenter, national cohort to measure the association between ASB and key postoperative infectious outcomes, including SSI and UTI, and to determine if antimicrobial therapy directed against the colonizing organism was associated with reduced rates of infection after major cardiac, orthopedic, and vascular surgical procedures. A secondary aim was to evaluate if the colonizing organism matched the infecting organism in cases of SSI and UTI.
Methods
Prior to data collection and analysis, all study procedures, including waiver of informed consent, were approved by the VA Boston Healthcare System Institutional Review Board. Data analysis was performed from December 2016 to August 2018.
Cohort Development
This study included all patients who underwent major cardiac (bypass or valve replacement), orthopedic knee and hip total joint replacement (eg, implant procedures), or vascular surgical procedures in 109 US facilities within the US Department of Veterans Affairs (VA) health care system from October 1, 2008, to September 30, 2013. A trained clinician performed a prospectively planned clinical record review for antimicrobial prophylaxis regimen (under the Reporting, Analytics, Performance, Improvement, and Deployment [RAPID] program) and for 30-day National Healthcare Safety Network–defined SSI and UTI postoperative outcomes (under the VA Surgical Quality Improvement Program [VASQIP]), and these patients underwent a urine culture during the 30-day preoperative period. The VASQIP assesses approximately 70% of surgical procedures within the VA system on the basis of a validated methodology for case review selection.17
Deep and organ/space SSI outcome was available for all surgical procedures during the study period. Per the planned VASQIP methodology, superficial SSI was assessed from 2012 to 2013 for cardiac surgical procedures and in all study years for the noncardiac procedures. Postoperative UTI was not assessed for patients who had cardiac surgical procedures.
Definitions
The decision for preoperative urine culture screening was directed by facility and/or surgeon practice. Urine culture results were defined as positive if they had 105 or more colony-forming units of any bacterial organism isolated. All other urine culture results were classified as negative. The clinical records of all patients with a positive urine culture result were manually reviewed by an infectious diseases physician on our team (J.G.S.) using a standardized data collection form to assess for lower UTI symptoms (ie, dysuria, frequency, urgency, and new hematuria) and for systemic symptoms (eg, fever or systemic inflammatory response syndrome [SIRS] and confusion or mental status changes). Patients with any symptom were classified as symptomatic UTI, and patients without any documented clinical symptoms were classified as having ASB.4 The classification of ASB or UTI was adjudicated by a second infectious diseases physician on our team (J.M.S.), and the robustness of this classification was assessed through a sensitivity analysis.
Antimicrobial regimens ordered anytime between the ASB culture date and the surgical procedure date were classified as active or inactive for the ASB organism on the basis of organism type and antimicrobial resistance profile. For cultures with more than 1 organism, antimicrobial therapy was considered inactive unless all organisms were susceptible to the regimen.
Outcomes
The 30-day SSI and UTI outcomes were measured by VASQIP according to the SSI and UTI surveillance definitions from the National Healthcare Safety Network. To expand the window to capture 90-day outcomes for cardiac and orthopedic implants, the wound culture results collected up to 90 days after the surgical procedure date were extracted electronically, as were the 90-day postoperative Clostridium difficile results and 30-day urine culture results. A wound culture result was classified as positive if any organism was grown in a culture obtained from a topography that was potentially associated with the surgical site. Cultures obtained for surveillance, cultures from foreign bodies such as central lines, and cultures from distant body sites were excluded.
Power and Sample Size
The sample size of the cohort was determined by the number of surgical procedures manually reviewed and provided by VASQIP. The expected incidence of patients with SSI without ASB was estimated at 2%, based on estimates used in the previous literature.1,18 Using this estimate, this study had greater than 80% power to identify a 2-fold higher rate of SSI among patients with ASB compared with those without ASB. Using an estimated SSI risk of 2% in patients treated for ASB, we had 72% power (1-tail test) to find a 3-fold increased risk of SSI among 132 patients who were not treated for ASB compared with 485 patients who received active treatment.
Statistical Analysis
Logistic regression analysis models adjusted for age, American Society of Anesthesiologists (ASA) physical status class, smoking status, race/ethnicity, sex, and diabetes status and then stratified by type of surgical procedure were used to measure the association between preoperative ASB and postoperative SSI, UTI, positive urine culture, and positive wound culture results. Race/ethnicity was classified as reported in the electronic medical records and included for purposes of describing the population. Among patients with ASB, we assessed the association between receipt of active antimicrobial therapy and/or active surgical prophylaxis and postoperative infectious outcomes. We used 2-tailed t test for continuous variables and χ2 for categorical variables, with P = .05 as the threshold for significance. All analyses were done in SAS, version 9.4 (SAS Institute).
A sensitivity analysis was performed to determine if expanding the control group (no ASB) to include patients without urine culture results changed the findings. Definition of the exposure group (ASB) remained the same. A second sensitivity analysis was performed to determine if expanding the exposure group to include all patients with a positive urine culture result regardless of the presence of symptoms changed the results. All other definitions remained the same.
Results
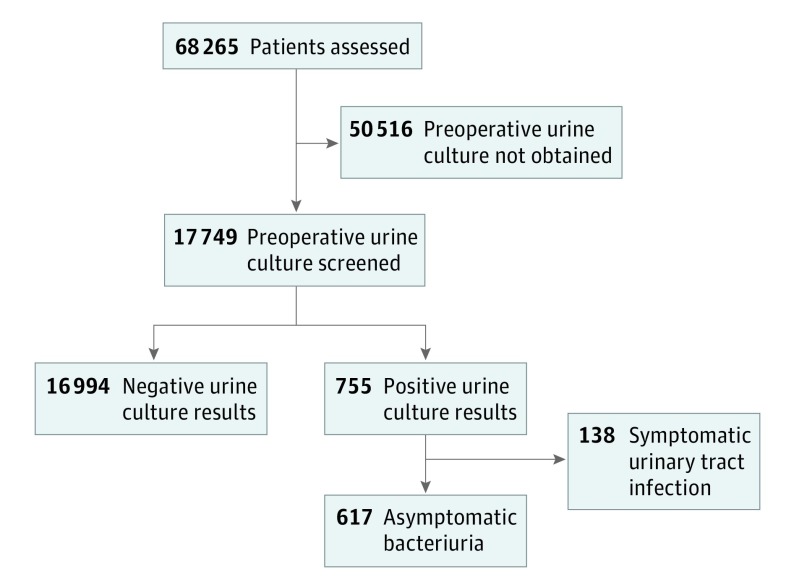
In total, 68 265 patients (65 664 [96.2%] were men and 2601 [3.8%] were women, with a mean [SD] age of 64.6 [9.2] years) who underwent cardiac, orthopedic, and vascular surgical procedures with manually validated SSI outcomes and antimicrobial prophylaxis regimens were identified. Of these patients, 17 749 (26.0%) had a urine culture and 17 611 (25.8%) were eligible for inclusion in the primary analysis (Figure 1).
Figure 1. Diagram of Eligible and Included Patients.
Among the 17 749 urine cultures performed, 755 (4.3%) had a positive result, of which 617 (81.7%) were designated as preoperative ASB. The proportion of preoperative urine cultures varied by surgical type, including 4324 (20%) obtained prior to cardiac surgical procedures, 12 399 (32%) prior to orthopedic surgical procedures, and 1027 (12.5%) prior to vascular surgical procedures. Urine cultures were performed within a median (interquartile range [IQR]) of 10 (4-18) days prior to the surgical procedure date. The mean age, sex, race/ethnicity, diabetes status, and smoking status were similar among the 50 516 patients without a preoperative urine culture compared with the 17 749 with a preoperative urine culture. Patients with ASB were older (mean [SD] age, 69.6 [10.4] years), less likely to be male (539 [87.4%]), and more likely to have diabetes (183 [29.7%]) compared with patients without ASB (Table 1).
Table 1. Demographics of Surgical Patients Stratified by Preoperative Urine Culture Results.
| Characteristic | No. (%) | ||||
|---|---|---|---|---|---|
| Preoperative Culture Screening | Total | ||||
| Not Performed | Negative Result | Positive Result | |||
| ASB | Symptomatic | ||||
| All patients | 50 516 | 16 994 | 617 | 138 | 68 265 |
| Male sex | 48 825 (96.7) | 16 173 (95.2) | 539 (87.4) | 127 (92.0%) | 65 664 (96.2) |
| Age, mean (SD), y | 64.5 (9.1) | 64.8 (9.4) | 69.6 (10.4) | 71.5 (10.0) | 64.6 (9.2) |
| Diabetes | 14 237 (28.2) | 4227 (24.9) | 183 (29.7) | 44 (31.9) | 18 691 (27.4) |
| Current smoker | 15 206 (30.1) | 4325 (25.5) | 150 (24.3) | 34 (24.6) | 19 715 (28.9) |
| Surgical cohort | |||||
| Cardiac | 17 076 (33.8) | 4081 (24.0) | 194 (31.4) | 48 (34.8) | 21 399 (31.3) |
| Orthopedic | 26 281 (52.0) | 11 949 (70.3) | 376 (60.9) | 74 (53.6) | 38 680 (56.7) |
| Vascular | 7159 (14.2) | 964 (5.7) | 47 (7.6) | 16 (11.6) | 8186 (12.0) |
| Race/ethnicitya | |||||
| White | 39 651 (78.5) | 13 565 (79.8) | 486 (78.8) | 104 (75.4) | 53 809 (78.8) |
| Black | 6783 (13.4) | 2117 (12.5) | 79 (12.8) | 22 (15.9) | 9001 (13.2) |
| Other | 4082 (8.1) | 1312 (7.7) | 52 (8.4) | 12 (8.7) | 5438 (8.0) |
| Ethnicitya | |||||
| Hispanic | 2307 (4.6) | 878 (5.2) | 33 (5.3) | 6 (4.3) | 3224 (4.7) |
Abbreviation: ASB, asymptomatic bacteriuria.
Six percent of patients had missing race data, and 3% had missing ethnicity data.
Association Between ASB and SSI
In total, 283 SSI (1.6%) were identified in the 30-day postoperative period among the 17 611 patients who had preoperative urine cultures in the absence of UTI symptoms. Among the 617 patients with ASB, 15 (2.4%) had an SSI compared with 268 (1.6%) of the 16 994 patients without ASB. After adjusting for age, ASA class, smoking status, race/ethnicity, sex, and diabetes status, no statistically significant difference in rates of SSI was identified in patients with or without ASB (adjusted odds ratio [aOR], 1.58; 95% CI, 0.93-2.70; P = .08) (Table 2). Adjusting for facility at the Veterans Integrated Service Networks level did not change the risk for SSI (aOR, 1.67; 95% CI, 0.95-2.90). The lack of association persisted when the analysis was stratified by surgical type, except for cardiac surgical procedures in which a 3-fold increase in the SSI rate was observed among preoperative patients with ASB compared with preoperative patients without ASB (6 of 194 [3.1%] vs 41 of 4081 [1.0%]; aOR, 3.06; 95% CI, 1.27-7.30) (Table 2).
Table 2. Frequency and Adjusted Risk of 30-Day Postoperative Outcomes in Patients With ASB or Without ASB, Stratified by Surgical Typea.
| Cohort | No./Total No. (%) | aOR (95% CI) | P Value | |
|---|---|---|---|---|
| Preoperative ASB Not Identified (n = 16 994) | Preoperative ASB Identified (n = 617) | |||
| Whole cohort | ||||
| SSI | 268/16 994 (1.6) | 15/617 (2.4) | 1.58 (0.93-2.70) | .08 |
| UTI | 196/12 913 (1.5) | 14/423 (3.3) | 1.42 (0.80-2.49) | .22 |
| Positive wound culture resultb | 497/16 994 (2.9) | 23/617 (3.7) | 1.20 (0.78-1.85) | .39 |
| Positive urine culture result | 616/16 994 (3.6) | 83/617 (13.5) | 2.87 (2.28-3.70) | <.001 |
| Cardiac procedure | ||||
| SSI | 41/4081 (1.0) | 6/194 (3.1) | 3.06 (1.27-7.30) | .01 |
| UTI | NA | NA | NA | NA |
| Positive wound culture resultb | 149/4081 (3.7) | 9/194 (4.6) | 1.22 (0.61-2.45) | .57 |
| Positive urine culture result | 195/4081 (4.8) | 31/194 (16) | 3.11 (2.04-4.74) | <.001 |
| Orthopedic procedure | ||||
| SSI | 154/11949 (1.3) | 5/376 (1.3) | 1.19 (0.48-2.96) | .69 |
| UTI | 164/11949 (1.4) | 14/376 (3.7) | 1.71 (0.97-3.04) | .06 |
| Positive wound culture resultb | 226/11949 (1.9) | 6/376 (1.6) | 0.86 (0.37-1.96) | .72 |
| Positive urine culture result | 364/11949 (3.0) | 46/376 (12.2) | 2.79 (1.98-3.93) | <.001 |
| Vascular procedure | ||||
| SSI | 73/964 (7.6) | 4/47 (8.5) | 1.10 (0.37-3.23) | .85 |
| UTI | 32/964 (3.3) | 0/47 (0) | NA | .98 |
| Positive wound culture resultb | 122/964 (12.7) | 8/47 (17.0) | 1.36 (0.61-3.04) | .44 |
| Positive urine culture result | 57/964 (5.9) | 6/47 (12.8) | 2.10 (0.84-5.25) | .11 |
Abbreviations: aOR, adjusted odds ratio; ASB, asymptomatic bacteriuria; NA, not applicable; SSI, surgical-site infection; UTI, urinary tract infection.
Covariates included diabetes status, smoking status, American Society of Anesthesiologists score higher than 2, sex, and age.
Wound cultures were abstracted up to 90 days after surgical procedure.
Association Between ASB and UTI
The VASQIP assessment captured 210 UTIs after 13 336 orthopedic and vascular procedures (1.6%). Fourteen (3.3%) of 423 patients with ASB had a UTI, compared with 196 (1.5%) of 12 913 patients without ASB (aOR, 1.42; 95% CI, 0.80-2.49; P = .22 (Table 2).
Sensitivity Analyses
In sensitivity analyses, in which the control group was expanded from 16 994 with a known negative urine culture result to also include the 50 516 patients without a urine culture result, minimal differences were observed in the risk of SSI or UTI compared with the more restrictive control group. The risk of SSI among the 67 510 patients without ASB identification was 2.1%, compared with 2.4% in patients with ASB (aOR, 1.17; 95% CI, 0.70-1.96; P = .55). Risk of UTI was 1.5% in 697 patients of the 46 353 expanded control group without ASB, compared with 3.3% in the ASB group (aOR, 1.46; 95% CI, 0.85-2.52; P = .17). Stratification across surgical types also demonstrated minimal changes in the OR when using the expanded control group definition. In a second sensitivity analysis that included all patients with positive urine culture results in the exposure group (including the 132 patients deemed to have symptoms consistent with possible UTI), the outcome of SSI also was not changed, compared with the more restrictive exposure group.
Association Between ASB and Other Postoperative Outcomes
Positive wound culture results from a potentially relevant body site were identified during the 90-day period after 520 surgical procedures. No statistically significant differences in the odds of positive wound culture results among patients with or without ASB were identified among the whole cohort or in the analysis stratified by surgical type.
During the 30-day postoperative period, 699 positive urine culture results (3.9%) were identified. The rate of positive postoperative urine culture results was higher among patients with ASB compared with patients without preoperative ASB (83 of 617 [13.5%] vs 616 of 16 994 [3.6%]; aOR, 2.87; 95% CI, 2.28-3.70; P < .001). The analysis stratified by surgical type had similar findings (Table 2).
We identified 128 cases of C difficile in the 90-day postoperative period. Five (0.8%) of 617 patients with ASB had C difficile compared with 123 (0.7%) of 16 994 patients without ASB (aOR, 0.82; 95% CI, 0.34-2.03; P = .67). Because all of the patients in the cohort received preoperative antimicrobial therapy (surgical prophylaxis at a minimum), stratification of C difficile rates according to antimicrobial exposure was not possible. Incidence of postoperative C difficile infection was similar across all surgical specialties.
Preoperative and Postoperative Microbiologic Results
The 617 preoperative ASB urine cultures included 249 (40.4%) Escherichia coli infection, 89 (14.4%) Klebsiella pneumoniae, 26 (4.2%) Pseudomonas aeruginosa, and 99 (16.0%) other gram-negative findings. Enterococci were the most common gram-positive organisms (94 of 617 [15.2%]), and 18 (2.9%) were Staphylococcus aureus. Among the ASB patients, 23 (3.7%) had a positive postoperative wound culture result. In 2 cases (0.3%), the ASB organism matched the organism in the postoperative wound culture result. In both cases, the organism was S aureus.
Among the 83 patients with a positive postoperative urine culture result, 41 (49.4%) had the same organism identified in the preoperative and postoperative urine culture results. Thirty-seven (90.2%) of the 41 organisms were gram-negative bacteria, and 24 (58.5%) were E coli.
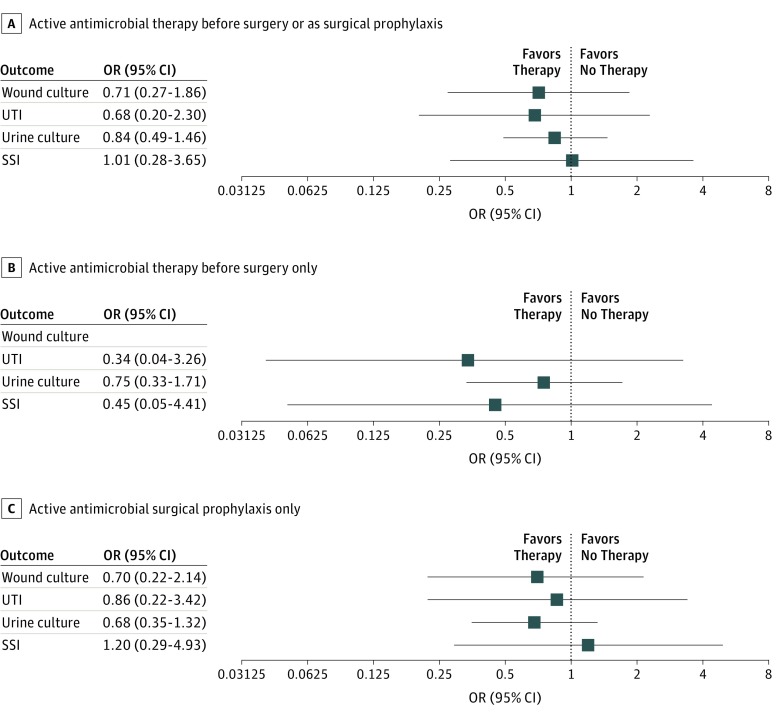
Association of ASB Treatment With Postoperative Outcomes
Among the 617 patients with ASB, 342 (55.4%) received antimicrobial therapy prior to the surgical procedure; the antimicrobial therapy was active against the ASB pathogen in 288 cases (46.7%). In patients who did not receive active therapy prior to the surgical procedure, 197 (31.9%) received a surgical prophylaxis regimen with activity against the uropathogen, resulting in a total of 485 patients (78.6%) who received antimicrobial therapy with activity against the ASB pathogen either before the surgical procedure or as a surgical prophylaxis. The remaining 132 patients with ASB (21.4%) received no active antimicrobial therapy for their ASB organism, either as a preoperative therapy or as a surgical prophylaxis (Figure 2).
Figure 2. Forest Plots of the Adjusted Risk for Each Selected Outcome in Patients With Preoperative Asymptomatic Bacteriuria (ASB) .
Patients who received active antimicrobial therapy (ie, agent with in vitro activity against all pathogens in the ASB urine culture, and not necessarily an intent to treat the ASB pathogen) before surgery or as a surgical prophylaxis (n = 485; A), active antimicrobial therapy before surgery but not as a prophylaxis (n = 92; B), and active antimicrobial therapy as a surgical prophylaxis but not before surgery (n = 197; C). Each group was compared with those who did not receive active antimicrobial therapy against the ASB organisms before surgery or as a surgical prophylaxis (n = 132). OR indicates odds ratio; SSI, surgical site infection; UTI, urinary tract infection.
The incidence of SSI was slightly higher in patients who received either active therapy or prophylaxis (2.5%), compared with those who did not receive active therapy or prophylaxis (2.3%), but was not statistically different (aOR, 1.01; 95% CI, 0.28-3.65; P = .99) (Figure 2). Treatment or prophylaxis for the ASB organism similarly did not reduce the odds of postoperative UTI (aOR 0.68; 95% CI, 0.20-2.30; P = .54) (Figure 2A). The incidence of postoperative urine and wound cultures with positive results also did not differ statistically significantly by receipt of active antimicrobial therapy (Figure 2).
In the cardiac surgical procedure subgroup, SSI occurred more frequently (5 of 152 [3.3%]) in patients treated with active antimicrobial therapy or surgical prophylaxis compared with patients who did not receive any active therapy or prophylaxis (1 of 42 [2.4%]). However, this difference was not statistically significant (aOR, 1.71; 95% CI, 0.17-16.34).
Discussion
In this large cohort of veterans, preoperative ASB was associated with higher rates of positive postoperative urine culture results among patients who underwent cardiac, orthopedic, and vascular surgical procedures and was associated with 30-day SSI in patients who had cardiac surgical procedures. Of importance, active antimicrobial therapy directed toward the asymptomatic uropathogen was not associated with improvement in any measurable postoperative clinical outcome; the rates of manually determined SSI, UTI, and positive wound and urine culture results were the same in patients who were treated and in those who were untreated. These data, therefore, suggest that there is no clinical utility to preoperative screening of urine cultures for cardiac, orthopedic, and vascular surgical procedures. Furthermore, if urine cultures are obtained, there is no value in, and therefore no role for, providing treatment or expanded prophylaxis to sterilize the urine in the perioperative period. These data are strengthened by our ability to match organism, antimicrobial resistance profile, and antimicrobial receipt to demonstrate that active treatment was not associated with improvement in clinical outcomes.
Much of the published medical literature focuses on positive interventions. However, identifying interventions that do not improve clinical care but only escalate health care costs is equally important. The Choosing Wisely campaign highlights the importance of not treating ASB in most circumstances, given the concerns about the harms of antimicrobial use, such as adverse drug events, emergence of antimicrobial resistance, and increases in C difficile infection, without any demonstrated value.19 However, in the setting of new hardware, surgeons often feel compelled to provide targeted therapy for any colonizing organism given a desire to prevent highly morbid postoperative infections, such as prosthetic joint infections.3,18,20 These findings are underscored by multiple investigations demonstrating that when urine culture results are positive, clinicians prescribe targeted therapy to treat the colonizing uropathogen21; the higher the colony count, the stronger the inclination to treat.22 An orthopedic study found that discontinuing routine urine culture screening led to reductions in antimicrobial prescriptions without increases in postoperative prosthetic joint infections.23
This study provides strong evidence that the practice of screening for asymptomatic bacteriuria with directed antimicrobial therapy should be de-implemented given the lack of advantages, potential for antimicrobial-associated harm, and unnecessary medical costs. Furthermore, the risk of SSI did not change when we expanded the exposure group to include patients with symptoms potentially consistent with UTI or when we expanded the control group to include patients who did not have urine cultures (which counted them as not having ASB). Thus, the findings are robust and are reliable in settings with practice variations in urine culture screening and documentation of symptoms.
The ability to directly compare the preoperative uropathogen with the organism grown in postoperative wound cultures strengthens the argument against screening and prophylaxis. An important finding is that in no cases did the ASB organism match the organism found in a prosthetic joint infection. Only twice did the preoperative ASB organism match the postoperative pathogen; in both cases, the infecting organism was S aureus and the surgical type was cardiac.
The role that urinary colonization with S aureus plays in the future development of postoperative infections is unknown, and our data are not able to definitively answer how these cases should be managed clinically. In this large cohort that included more than 17 000 urine cultures, we identified only 2 matches. As skin organisms, staphylococcal species are the most common cause of SSI. Thus, the match in these 2 cases may have occurred simply by chance. However, the positive urine culture result may also be a possible risk marker for a high burden of staphylococcal colonization and high risk for future S aureus infection, but the urinary colonization may not itself be in the causal pathway. Because we only identified 2 matches, we did not have statistical power to measure the implications of antimicrobial prophylaxis for patients specifically colonized with S aureus. However, in cases in which methicillin-resistant strains are cultured, it may be prudent to manage patients with S aureus in their urine as colonized and to administer appropriate surgical prophylaxis and decolonization.
Limitations
This study has several limitations. First, it is limited by its observational and retrospective nature as well as the rarity of the events evaluated. In this cohort comprising more than 17 000 clean surgical procedures with an integrated electronic medical record that optimized the capture of exposure and outcome data, only 617 cases of ASB occurred. Thus, given the infrequency of ASB, study designs that can establish causality, such as randomized clinical trials, are not feasible. Previous studies that attempted to answer how ASB treatment affected postoperative outcomes hinted that treatment of ASB before orthopedic total joint replacement procedures was not associated with improvement in postoperative outcomes; however, these studies included only a single center and had limited statistical power because of their small sample size.7 The one randomized clinical trial that compared ASB treatment with no treatment included 46 cases of ASB in the active and control arms combined; thus, that trial did not have statistical power to measure the association between treatment and postoperative outcomes.13 Although, to our knowledge, this study substantially expands on current evidence, it only had the power to detect a 3-fold difference in outcomes between the treatment and no treatment groups; thus, some patients possibly gained some advantages that were not detected in this analysis. However, the harms of antimicrobial treatment, such as increases in C difficile infections, acute kidney injury, allergic reactions, and other adverse events, likely exceed any value, which would not have been detected in a cohort this large. Second, the study population was primarily male, and we were not able to control for variables such as immunocompromise, which could affect generalizability. Third, the ability to adjust by surgeon-level data was also limited.
Conclusions
The routine screening of preoperative urine cultures prior to major cardiac, orthopedic, and vascular surgical procedures rarely identified ASB in the predominantly male population of this study. When present, ASB was associated with high rates of positive urine culture results during the postoperative period. However, active antimicrobial therapy was not associated with a reduced incidence of postoperative SSIs or UTIs, indicating that ASB is a marker for host risk of colonization but not in the causal pathway of infections. To our knowledge, this study is the largest and most robust investigation into urine culture screening to date. It provides strong evidence that preoperative screening may not be valuable and should be discontinued as routine clinical practice.
References
- 1.Sousa R, Muñoz-Mahamud E, Quayle J, et al. Is asymptomatic bacteriuria a risk factor for prosthetic joint infection? Clin Infect Dis. 2014;59(1):41-47. doi: 10.1093/cid/ciu235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ollivere BJ, Ellahee N, Logan K, Miller-Jones JC, Allen PW. Asymptomatic urinary tract colonisation predisposes to superficial wound infection in elective orthopaedic surgery. Int Orthop. 2009;33(3):847-850. doi: 10.1007/s00264-008-0573-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailin S, Noiseux N, Pottinger JM, et al. Screening patients undergoing total hip or knee arthroplasty with perioperative urinalysis and the effect of a practice change on antimicrobial use. Infect Control Hosp Epidemiol. 2017;38(3):281-286. doi: 10.1017/ice.2016.272 [DOI] [PubMed] [Google Scholar]
- 4.Nicolle LE, Gupta K, Bradley S, et al. Clinical Practice Guideline for the management of asymptomatic bacteriuria: 2018 update by the Infectious Diseases Society of America. Paper presented at: IDWeek 2018; October 7, 2018; San Diego, CA. [Google Scholar]
- 5.de Lange MP, Sonker U, Kelder JC, de Vos R. Practice variation in treatment of suspected asymptomatic bacteriuria prior to cardiac surgery: are there differences in postoperative outcome? A retrospective cohort study. Interact Cardiovasc Thorac Surg. 2016;22(6):769-775. doi: 10.1093/icvts/ivw039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soltanzadeh M, Ebadi A. Is presence of bacteria in preoperative microscopic urinalysis of the patients scheduled for cardiac surgery a reason for cancellation of elective operation? Anesth Pain Med. 2013;2(4):174-177. doi: 10.5812/aapm.8667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayne AIW, Davies PSE, Simpson JM. Antibiotic treatment of asymptomatic bacteriuria prior to hip and knee arthroplasty; a systematic review of the literature. Surgeon. 2018;16(3):176-182. doi: 10.1016/j.surge.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 8.Maderazo EG, Judson S, Pasternak H. Late infections of total joint prostheses. A review and recommendations for prevention. Clin Orthop Relat Res. 1988;(229):131-142. [PubMed] [Google Scholar]
- 9.Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008;466(7):1710-1715. doi: 10.1007/s11999-008-0209-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodríguez D, Pigrau C, Euba G, et al. ; REIPI Group (Spanish Network for Research in Infectious Disease) . Acute haematogenous prosthetic joint infection: prospective evaluation of medical and surgical management. Clin Microbiol Infect. 2010;16(12):1789-1795. doi: 10.1111/j.1469-0691.2010.03157.x [DOI] [PubMed] [Google Scholar]
- 11.Kaandorp CJ, Dinant HJ, van de Laar MA, Moens HJ, Prins AP, Dijkmans BA. Incidence and sources of native and prosthetic joint infection: a community based prospective survey. Ann Rheum Dis. 1997;56(8):470-475. doi: 10.1136/ard.56.8.470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sousa R, Soriano A, Guyot A. Reply to Uçkay et al. Clin Infect Dis. 2014;59(10):1507-1508. doi: 10.1093/cid/ciu606 [DOI] [PubMed] [Google Scholar]
- 13.Cordero-Ampuero J, González-Fernández E, Martínez-Vélez D, Esteban J. Are antibiotics necessary in hip arthroplasty with asymptomatic bacteriuria? Seeding risk with/without treatment. Clin Orthop Relat Res. 2013;471(12):3822-3829. doi: 10.1007/s11999-013-2868-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bouvet C, Lübbeke A, Bandi C, et al. Is there any benefit in pre-operative urinary analysis before elective total joint replacement? Bone Joint J. 2014;96-B(3):390-394. doi: 10.1302/0301-620X.96B3.32620 [DOI] [PubMed] [Google Scholar]
- 15.Martínez-Vélez D, González-Fernández E, Esteban J, Cordero-Ampuero J. Prevalence of asymptomatic bacteriuria in knee arthroplasty patients and subsequent risk of prosthesis infection. Eur J Orthop Surg Traumatol. 2016;26(2):209-214. doi: 10.1007/s00590-015-1720-4 [DOI] [PubMed] [Google Scholar]
- 16.Mayne AI, Davies PS, Simpson JM. Screening for asymptomatic bacteriuria before total joint arthroplasty. BMJ. 2016;354:i3569. doi: 10.1136/bmj.i3569 [DOI] [PubMed] [Google Scholar]
- 17.Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5)(suppl):S19-S27. doi: 10.1016/j.amjsurg.2009.07.025 [DOI] [PubMed] [Google Scholar]
- 18.Branch-Elliman W, Ripollone JE, O’Brien WJ, et al. Risk of surgical site infection, acute kidney injury, and Clostridium difficile infection following antibiotic prophylaxis with vancomycin plus a beta-lactam versus either drug alone: A national propensity-score-adjusted retrospective cohort study. PLoS Med. 2017;14(7):e1002340. doi: 10.1371/journal.pmed.1002340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jung N, Lehmann C, Fätkenheuer G. The “Choosing Wisely”: initiative in infectious diseases. Infection. 2016;44(3):283-290. doi: 10.1007/s15010-015-0848-9 [DOI] [PubMed] [Google Scholar]
- 20.Finnigan TKP, Bhutta MA, Shepard GJ. Asymptomatic bacteriuria prior to arthoplasty: how do you treat yours? [abstract]. Orthop Proc. 2012;94-B(suppl XXIX):58. [Google Scholar]
- 21.Leis JA, Rebick GW, Daneman N, et al. Reducing antimicrobial therapy for asymptomatic bacteriuria among noncatheterized inpatients: a proof-of-concept study. Clin Infect Dis. 2014;58(7):980-983. doi: 10.1093/cid/ciu010 [DOI] [PubMed] [Google Scholar]
- 22.Drekonja DM, Gnadt C, Kuskowski MA, Johnson JR. Urine cultures among hospitalized veterans: casting too broad a net? Infect Control Hosp Epidemiol. 2014;35(5):574-576. doi: 10.1086/675829 [DOI] [PubMed] [Google Scholar]
- 23.Lamb MJ, Baillie L, Pajak D, et al. Elimination of Screening Urine Cultures Prior to Elective Joint Arthroplasty. Clin Infect Dis. 2017;64(6):806-809. [DOI] [PubMed] [Google Scholar]